What is a blighted ovum
A blighted ovum is an egg that is fertilized but doesn’t develop 1. A blighted ovum is a common problem and may cause up to 50% of miscarriages in the first 12 weeks. A blighted ovum, also called an anembryonic pregnancy or anembryonic gestation, occurs when the early embryo stops developing, is resorbed and leaves an empty gestational sac larger than 18 mm without evidence of embryonic tissues (yolk sac or embryo). In a blighted ovum, a gestational (embryo) sac forms and grows; however, the embryo does not develop. The reason why blighted ovum occurs is often unknown, but it may be due to chromosomal abnormalities in the fertilized egg.
A blighted ovum usually occurs early in pregnancy — between about week 8 and week 13 — sometimes before you even know you’re pregnant. However, you may be aware of your early pregnancy because of a positive pregnancy test or missed menstrual period. A pregnancy test may be positive because the early embryo secretes a pregnancy hormone — human chorionic gonadotropin (hCG) — until the embryo stops developing and fails to implant.
You may have symptoms of early pregnancy, such as breast tenderness, nausea and vomiting. But when the embryo stops growing and hormone levels decrease, pregnancy symptoms subside. At this point, minor abdominal cramping and light spotting or bleeding are possible. An ultrasound will show an empty gestational sac.
A blighted ovum eventually results in miscarriage. Some women choose to wait for the miscarriage to happen naturally, while others take medication to trigger the miscarriage. In some cases, a procedure called dilation and curettage (D&C) is used to remove the placental tissues.
Most women who’ve had a blighted ovum go on to have successful pregnancies. If you experience multiple consecutive miscarriages, talk with your doctor or other care provider to identify any underlying causes.
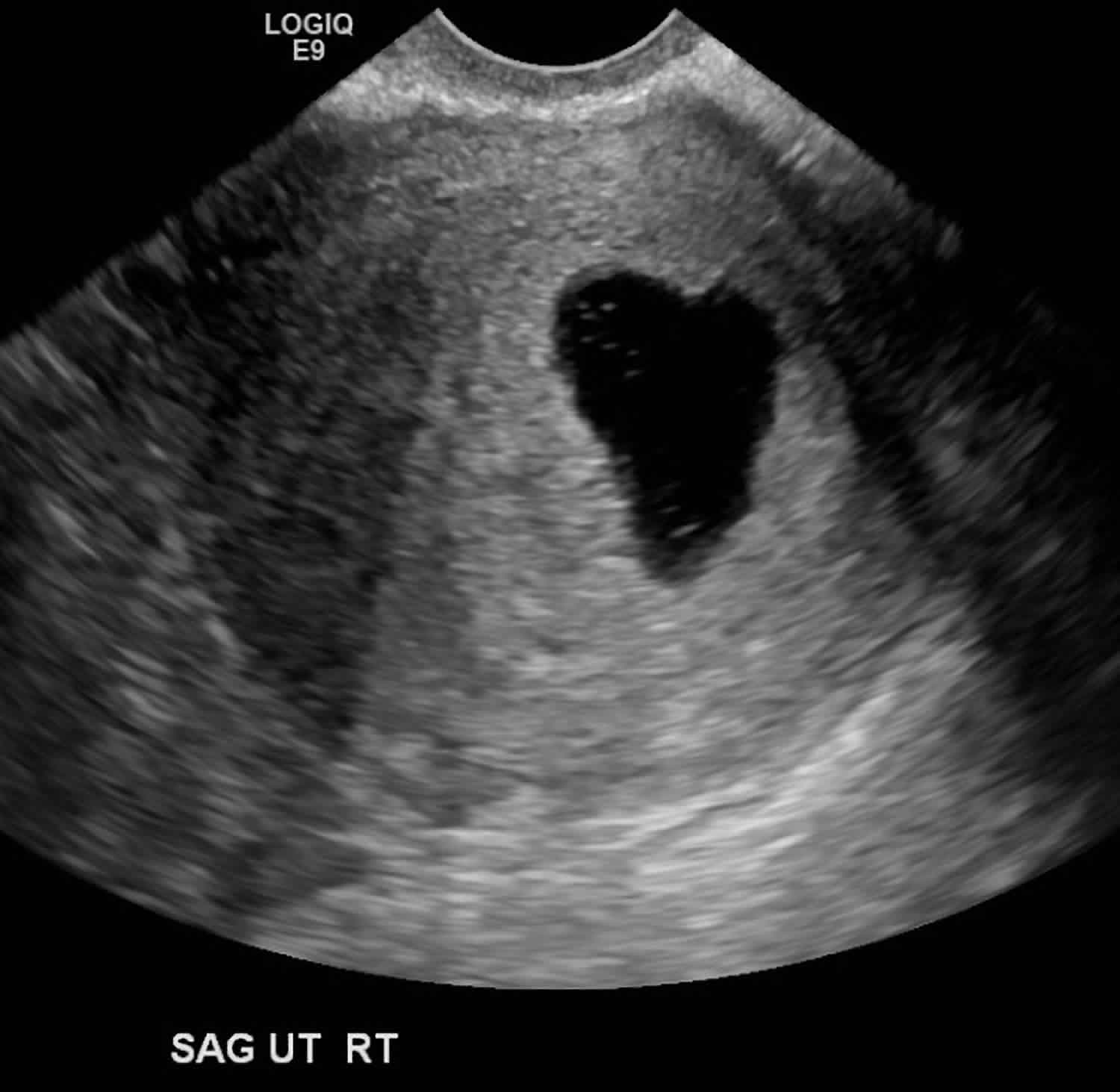
Figure 1. Blighted ovum ultrasound
Footnote: Female 25 years of age with beta hCG positive undergoing a scan for determination of gestational age. No fetal pole is present within this 25 mm intrauterine gestational sac. This is in keeping with blighted ovum or an anembryonic pregnancy. The irregular shape of the gestational sac is also regarded as a poor prognostic factor.
[Source 2]Call your doctor or seek immediate medical care if:
- You have severe vaginal bleeding.
- You are dizzy or light-headed, or you feel like you may faint.
- You have a fever.
- You have new or worse pain in your belly or pelvis.
- You have vaginal discharge that smells bad.
Watch closely for changes in your health, and be sure to contact your doctor if:
- You do not get better as expected.
How common is a blighted ovum?
A blighted ovum is the leading cause of miscarriage (50%) 1. In the first trimester, the names early pregnancy loss, miscarriage, or spontaneous abortion are all interchangeably used as there is no consensus in the literature. Early pregnancy loss is the spontaneous loss of a pregnancy before 13 weeks of gestation.
What is a miscarriage?
In the United Kingdom, miscarriage is the loss of an intrauterine pregnancy before 24 complete weeks of gestation. The World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) define miscarriage as the loss of a pregnancy before 20 weeks of gestation or the ejection or removal of an embryo or fetus that weighs 500 g or less. This definition is used in the United States; however, it may vary based on State laws.
Biochemical miscarriage is a loss that occurs after a positive urine pregnancy test (hCG) or a raised serum beta-hCG before ultrasound or histological verification.
Clinical miscarriage is when ultrasound examination or histologic evidence has confirmed the existence of an intrauterine pregnancy.
In general, clinical miscarriage is classified as early (before 12 weeks of pregnancy) and late (12 weeks to 20 weeks). In Europe, the late loss is defined as one that occurs between 12 and 22 weeks.
Miscarriage classified as sporadic and recurrent. Sporadic miscarriage is the more common than recurrent. Sporadic miscarriage is when 2 or 3 consecutive pregnancy losses occur.
According to the European Society of Human Reproduction and Embryology guidelines, recurrent miscarriage is defined as 3 or more consecutive pregnancy losses before 22 weeks of gestation.
Blighted ovum causes
The most common cause of blighted ovum is genetic. This is often due to chromosomal defects from a poor quality sperm or egg (too many or too few chromosomes in them). However, in India, in addition to a genetic cause, causes include infections (tuberculosis [TB]) or structural defects of the uterus.
Genetics
According to Buckett and Regan 1, trisomies are the major fetal chromosomal abnormality in sporadic cases of miscarriage (30% of all miscarriages) and 60% of chromosomally abnormal miscarriages (recurrent miscarriage). Trisomies with Monosomy X (15% to 25%) and triploidy (12% to 20%) account for over 90% of all chromosomal abnormalities found in sporadic cases of miscarriage 1.
Trisomies of all chromosomes have been found except for Chromosome 1 and Y. However, the frequency of these trisomies varies (Chromosome 16 and to a lesser extent 2, 13, 15, 18, 21, 22, accounts for the majority of trisomic abnormalities). According to a study by Edmonds in 1992, trisomy 16 was found to give rise to the most rudimentary embryonic growth with an empty sac, while other trisomies often resulted in early embryonic demise.
A 1992 study by Alberman implicated trisomies and monosomies for miscarriage at the modal peak of 9 weeks; whereas, triploidy pregnancy losses spanned 5 to 16 weeks of gestation.
Recurrent miscarriage due to blighted ovum
Recurrent miscarriage due to blighted ovum was significantly higher (68.5% versus 31.5%) in consanguineous marriages according to the study Chromosomal Study of Couples with the History of Recurrent Spontaneous Abortions with Diagnosed Blighted Ovum) by Shekoohi et al. 3 done in Iran.
Sperm DNA Fragmentation
There is a link between DNA damage in sperm and miscarriage. According to the research article by Larsen et al. in 2013 4, “a meta-analysis of 16 studies found a highly significant increase in miscarriage rate in couples where the male partner had elevated levels of sperm DNA damage compared to those where the male partner had low levels of sperm DNA damage.”
Nutrition/Body Mass Index (BMI) Status
According to the study done by Popovic et al. (2016) in Serbia, published in the European Review for Medical and Pharmacological Sciences, low levels of copper (Cu), prostaglandin E2, and anti-oxidative enzymes (except for superoxide dismutase) and significantly high levels of lipid peroxidation products in the plasma have been attributed to the cause of blighted ovum miscarriages.
According to Larsen et al. 4, there are many pregnancy-related complications associated with obesity, including miscarriage. “A meta-analysis from 2008 including primary studies on infertile populations showed significantly increased miscarriage rates in women with a body mass index (BMI) greater than or equal to 25 kg/m² were compared to women with a BMI less than 25 kg/m².”
“This tendency has also been demonstrated in women with recurrent marriage although it must be emphasized that a significantly increased risk of another miscarriage was demonstrated only in obese women; that is, BMI ≥30 kg/m².”
Infections
According to the WHO (1998) 1 in 5 women who have an unsafe abortion, suffer from reproductive tract infections and as a result, lead to infertility. According to the study done by Maharana in 2011, the occurrence of spontaneous abortion (defined as pregnancy loss without the application of any deliberate method to terminate it during early weeks of pregnancy) is 10% and induced abortion (often done using several dangerous procedures and under substandard clinical and sanitary conditions) is 3%.
In India, which includes 11 major states, the occurrence of induced abortion among women with reproductive tract infections is 2 times higher than those not affected by reproductive tract infections.
According to Patki and Chauhan (2015), the most common cause of blighted ovum/miscarriage in addition to genetics is infections (TB) and structural defects of the uterus.
Anomalies of the uterus
According to the study (New Insights into Mechanisms Behind Miscarriage) by Larsen et al., BMC Medicine 4 uterine malformations which can be congenital or acquired are the cause of recurrent miscarriage. Congenital includes arcuate, didelphic, bicornuate, and septate uteri.
Drugs and Vaccines
According to the SAGE Working Group On Dengue Vaccines and WHO Secretariat (March 17, 2016), an additional serious adverse event found by the investigator in the 28 days to 6 months post-CYD (dengue) injection was blighted ovum.
Other causes
Immunologic
Immunologic disorders in the mother such as NK Cell Dysfunction, autoantibodies, hereditary and acquired thrombophilia, among others) can lead to the maternal immunological rejection of the implanting embryo in the uterus resulting in miscarriage.
Hormonal
Low levels of progesterone can lead to miscarriage.
Endocrine disorders
Thyroid disorders (thyroid autoimmunity and thyroid dysfunction) and ovarian disorders (e.g., polycystic ovarian syndrome [PCOS]) are associated with infertility and pregnancy loss. According to Larsen et al. 4, “the prevalence of PCOS among women with Recurrent Miscarriage is estimated to be 8.3% to 10%.”
Alcohol consumption
Even modest amounts of alcohol increase miscarriage risk significantly. Moreover, study results suggested that the risk increased in a dose-related manner.
Risk factors for miscarriage
Various factors increase the risk of miscarriage, including:
- Age. Women older than age 35 have a higher risk of miscarriage than do younger women. At age 35, you have about a 20 percent risk. At age 40, the risk is about 40 percent. And at age 45, it’s about 80 percent.
- Previous miscarriages. Women who have had two or more consecutive miscarriages are at higher risk of miscarriage.
- Chronic conditions. Women who have a chronic condition, such as uncontrolled diabetes, have a higher risk of miscarriage.
- Uterine or cervical problems. Certain uterine abnormalities or weak cervical tissues (incompetent cervix) might increase the risk of miscarriage.
- Smoking, alcohol and illicit drugs. Women who smoke during pregnancy have a greater risk of miscarriage than do nonsmokers. Heavy alcohol use and illicit drug use also increase the risk of miscarriage.
- Weight. Being underweight or being overweight has been linked with an increased risk of miscarriage.
- Invasive prenatal tests. Some invasive prenatal genetic tests, such as chorionic villus sampling and amniocentesis, carry a slight risk of miscarriage.
Blighted ovum prevention
Often, there’s nothing you can do to prevent a miscarriage. Simply focus on taking good care of yourself and your baby:
- Seek regular prenatal care.
- Avoid known miscarriage risk factors — such as smoking, drinking alcohol and illicit drug use.
- Take a daily multivitamin.
- Limit your caffeine intake. A recent study found that drinking more than two caffeinated beverages a day appeared to be associated with a higher risk of miscarriage.
If you have a chronic condition, work with your health care team to keep it under control.
Blighted ovum signs and symptoms
You may be asymptomatic, presenting for an early pregnancy ultrasound. Alternatively, you may have symptoms of early pregnancy, such as breast tenderness, nausea and vomiting. But when the embryo stops growing and hormone levels decrease, pregnancy symptoms subside. At this point, minor abdominal cramping and light spotting or bleeding are possible. An ultrasound will show an empty gestational sac.
Due to falling hCG levels, the clinical signs of pregnancy tend to subside.
A blighted ovum eventually results in miscarriage. Some women choose to wait for the miscarriage to happen naturally, while others take medication to trigger the miscarriage. In some cases, a procedure called dilation and curettage (D&C) is used to remove the placental tissues.
Signs and symptoms of a miscarriage might include:
- Vaginal spotting or bleeding
- Pain or cramping in your abdomen or lower back
- Fluid or tissue passing from your vagina
If you have passed fetal tissue from your vagina, place it in a clean container and bring it to your health care provider’s office or the hospital for analysis.
Keep in mind that most women who experience vaginal spotting or bleeding in the first trimester go on to have successful pregnancies.
Misdiagnosed blighted ovum
A dangerous clinical situation could happen when the diagnosis of blighted ovum is missed. Heavy vaginal bleeding can lead to anemia. In an unpublished case report of a patient at 15 weeks from her last menstrual period, without any bleeding nor menstruation, the ultrasound examination showed a thick and dense endometrium. The surgical procedure led to a massive intraoperative bleed. It required intrauterine long gauze bandage positioning to stop the bleeding and a transfusion procedure to improve her hematocrit level 1.
Blighted ovum diagnosis
Your health care provider might do a variety of tests:
- Pelvic exam. Your health care provider might check to see if your cervix has begun to dilate.
- Ultrasound. During an ultrasound, your health care provider will check for a fetal heartbeat and determine if the embryo is developing normally. If a diagnosis can’t be made, you might need to have another ultrasound in about a week.
- Blood tests. Your health care provider might check the level of the pregnancy hormone, human chorionic gonadotropin (HCG), in your blood and compare it to previous measurements. If the pattern of changes in your HCG level is abnormal, it could indicate a problem. Your health care provider might check to see if you’re anemic — which could happen if you’ve experienced significant bleeding — and may also check your blood type.
- Tissue tests. If you have passed tissue, it can be sent to a lab to confirm that a miscarriage has occurred — and that your symptoms aren’t related to another cause.
- Chromosomal tests. If you’ve had two or more previous miscarriages, your health care provider may order blood tests for both you and your partner to determine if your chromosomes are a factor.
A blighted ovum (anembryonic pregnancy) may be diagnosed:
- when there is no embryo seen on endovaginal scanning in a gestational sac with mean sac diameter ≥25 mm 5
Or
- there is no embryo on follow-up endovaginal scan 6:
- ≥11 days after scan showing gestational sac with yolk sac, but no embryo, or
- ≥ 2 weeks after a scan showing gestational sac without yolk sac or embryo
Assessment of interval mean sac diameter growth has been shown to be insufficiently accurate in the diagnosis of anembryonic pregnancy, due to an overlap of gestational sac growth rates of viable and non-viable pregnancies.
Other ancillary features have been described, and may be considered poor prognostic factors, but do not contribute to the formal diagnosis of a failed pregnancy. These include:
- absent yolk sac when mean sac diameter >8 mm on transvaginal ultrasound
- poor decidual reaction: often <2 mm
- irregular gestational sac shape
- abnormally low sac position
Blighted ovum treatment
Treatment of blighted ovum:
- Expectant management: If you have no signs of infection, you might choose to let the miscarriage progress naturally. Usually this happens within a couple of weeks of determining that the embryo has died. Unfortunately, it might take up to three or four weeks. This can be an emotionally difficult time. If expulsion doesn’t happen on its own, medical or surgical treatment will be needed. If, after a diagnosis of certain pregnancy loss, you’d prefer to speed the process, medication can cause your body to expel the pregnancy tissue and placenta. The medication can be taken by mouth or by insertion in the vagina. Your health care provider might recommend inserting the medication vaginally to increase its effectiveness and minimize side effects such as nausea and diarrhea. For about 70 to 90 percent of women, this treatment works within 24 hours.
- Medical treatment consisting of misoprostol on an outpatient basis is another option. However, it may take several days for the body to expel all tissue and may have more bleeding and side effects. The recommended dose of misoprostol is per the International Federation of Gynecology and Obstetrics (FIGO), 2017 guidelines as published in the article by Morris et al. 7.
- Surgical Treatment: Another option is a minor surgical procedure called suction dilation and curettage (D&C). During this procedure, your health care provider dilates your cervix and removes tissue from the inside of your uterus. Complications are rare, but they might include damage to the connective tissue of your cervix or the uterine wall. Surgical treatment is needed if you have a miscarriage accompanied by heavy bleeding or signs of an infection.
How can you care for yourself at home?
- You will probably have vaginal bleeding, similar to a period, for up to a week. Use pads instead of tampons. You may use tampons during your next period, which should start in 3 to 6 weeks.
- Take an over-the-counter pain medicine, such as acetaminophen (Tylenol), ibuprofen (Advil, Motrin), or naproxen (Aleve) for cramps. Read and follow all instructions on the label. You may have cramps for several days after the miscarriage.
- Do not take two or more pain medicines at the same time unless the doctor told you to. Many pain medicines have acetaminophen, which is Tylenol. Too much acetaminophen (Tylenol) can be harmful.
- Your doctor may want you to collect tissue that you might pass. Use a clear container. Take it to your doctor’s office as soon as you can.
- Do not have sex until the bleeding stops.
- You may return to your normal activities if you feel well enough to do so. But you should avoid heavy exercise until the bleeding stops.
- If you plan to get pregnant again, check with your doctor. Most doctors suggest waiting until you have had at least one normal period before you try to get pregnant.
- If you do not want to get pregnant, ask your doctor about birth control. You can get pregnant again before your next period starts if you are not using birth control.
- You may be low in iron because of blood loss. Eat a balanced diet that is high in iron and vitamin C. Foods rich in iron include red meat, shellfish, eggs, beans, and leafy green vegetables. Talk to your doctor about whether you need to take iron pills or a multivitamin.
- The loss of a pregnancy can be very hard. You may wonder why it happened and blame yourself. Talking to family members, friends, a counselor, or your doctor may help you cope with your loss.
Physical recovery
In most cases, physical recovery from miscarriage takes only a few hours to a couple of days. In the meantime, call your health care provider if you experience heavy bleeding, fever or abdominal pain.
You may ovulate as soon as two weeks after a miscarriage. Expect your period to return within four to six weeks. You can start using any type of contraception immediately after a miscarriage. However, avoid having sex or putting anything in your vagina — such as a tampon — for two weeks after a miscarriage
Pregnancy after blighted ovum
It’s possible to become pregnant during the menstrual cycle immediately after a miscarriage. But if you and your partner decide to attempt another pregnancy, make sure you’re physically and emotionally ready. Ask your health care provider for guidance about when you might try to conceive.
Keep in mind that miscarriage is usually a one-time occurrence. Most women who miscarry go on to have a healthy pregnancy after miscarriage. Less than 5 percent of women have two consecutive miscarriages, and only 1 percent have three or more consecutive miscarriages.
If you experience multiple miscarriages, generally two or three in a row, consider testing to identify any underlying causes — such as uterine abnormalities, coagulation problems or chromosomal abnormalities. If the cause of your miscarriages can’t be identified, don’t lose hope. About 60 to 80 percent of women with unexplained repeated miscarriages go on to have healthy pregnancies.
Doctors most often recommend couples wait for 1 to 3 regular menstrual cycles before trying to conceive again after any miscarriage.
Recommendations of the common obstetric guidelines by American College of Obstetricians and Gynecologists and Royal College of Obstetricians and Gynaecologists (United Kingdom) on different topics were not comparable the majority of the time. In the United Kingdom, the Royal College of Obstetricians and Gynecologists (RCOG) as per the new guidelines, recommends that physicians monitor a growing gestational sac until it reaches at least 25 mm (this would be about 9 weeks into pregnancy) before diagnosing a blighted ovum. One can be misdiagnosed as having a blighted ovum if diagnosed at 8 weeks or sooner.
Many women who have a tilted uterus look 1 to 2 weeks behind and can be misdiagnosed as having a blighted ovum, so they should wait until at least 9 weeks (if no complications) when most women see the baby.
The expertise of different ultrasound technicians (positioning of the woman especially with a tilted uterus) on the same day can affect the ultrasound measurements. These measurements can be off 4 mm or 5 mm which can result in misdiagnosis.
References- Chaudhry K, Siccardi MA. Blighted Ovum (Anembryonic Pregnancy) [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499938
- Anembryonic pregnancy. https://radiopaedia.org/cases/anembryonic-pregnancy-1
- Shekoohi S, Mojarrad M, Raoofian R, Ahmadzadeh S, Mirzaie S, Hassanzadeh-Nazarabadi M. Chromosomal study of couples with the history of recurrent spontaneous abortions with diagnosed blightded ovum. Int J Mol Cell Med. 2013;2(4):164–168. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3927383
- New insights into mechanisms behind miscarriage. BMC Medicine 2013, 11:154 https://doi.org/10.1186/1741-7015-11-154
- Dogra V, Paspulati RM, Bhatt S. First trimester bleeding evaluation. Ultrasound Q. 2005;21 (2): 69-85.
- Doubilet PM, Benson CB, Bourne T et-al. Diagnostic criteria for nonviable pregnancy early in the first trimester. N. Engl. J. Med. 2013;369 (15): 1443-51. doi:10.1056/NEJMra1302417
- Morris, J. L., Winikoff, B. , Dabash, R. , Weeks, A. , Faundes, A. , Gemzell‐Danielsson, K. , Kapp, N. , Castleman, L. , Kim, C. , Ho, P. C. and Visser, G. H. (2017), FIGO’s updated recommendations for misoprostol used alone in gynecology and obstetrics. Int J Gynecol Obstet, 138: 363-366. doi:10.1002/ijgo.12181 https://obgyn.onlinelibrary.wiley.com/doi/pdf/10.1002/ijgo.12181