What causes brain lesions
Brain lesions have many different causes that range from traumatic brain injury or disease, such as a infection, autoimmune diseases, abscess, stroke, genetic disorders or tumors or cancers (primary brain cancer and metastatic cancer or brain metastases). A brain lesion may involve small to large areas of your brain, and the severity of the underlying condition may range from relatively minor to life-threatening.
A brain lesion is an abnormality seen on a brain-imaging test, such as magnetic resonance imaging (MRI) or computerized tomography (CT). On CT or MRI scans, brain lesions appear as dark or light spots that don’t look like normal brain tissue.
Usually, a brain lesion is an incidental finding unrelated to the condition or symptom that led to the imaging test in the first place.
A brain lesion may involve small to large areas of your brain, and the severity of the underlying condition may range from relatively minor to life-threatening.
If a brain lesion discovered during a brain-imaging test doesn’t appear to be from a benign or resolved condition, your doctor will likely seek more information from additional testing or consulting a specialist.
Your doctor may recommend that you see a neurologist for a specialized examination and, possibly, further tests. Even if a neurological work-up doesn’t result in a diagnosis, your doctor may recommend continued testing to reach a diagnosis or follow-up imaging tests at regular intervals to monitor the lesion.
Often, a brain lesion has a characteristic appearance that will help your doctor determine its cause. Sometimes the cause of the abnormal-appearing area cannot be diagnosed by the image alone, and additional or follow-up tests may be necessary.
Among the known possible causes of brain lesions are:
- Brain aneurysm (a bulge in an artery in your brain)
- Brain AVM (arteriovenous malformation) — an abnormal formation of brain blood vessels
- Brain tumor (both cancerous and noncancerous)
- Encephalitis (brain inflammation)
- Epilepsy
- Hydrocephalus
- Multiple sclerosis
- Stroke
- Traumatic brain injury
While brain trauma of any sort may result in a concussion as well as a brain lesion, concussions and brain lesions are not the same thing. Concussions more often occur without ever causing any changes on the CT or MRI and are diagnosed by symptoms rather than imaging tests.
If a brain lesion discovered during a brain-imaging test doesn’t appear to be from a benign or resolved condition, your doctor will likely seek more information from additional testing or consulting a specialist.
Your doctor may recommend that you see a neurologist for a specialized examination and, possibly, further tests. Even if a neurological work-up doesn’t result in a diagnosis, your doctor may recommend continued testing to reach a diagnosis or follow-up imaging tests at regular intervals to monitor the lesion.
MS brain lesions
Multiple sclerosis (MS) is a nervous system disease that affects your brain and spinal cord. Multiple sclerosis damages the myelin sheath, the material that surrounds and protects your nerve cells. This damage slows down or blocks messages between your brain and your body, leading to the symptoms of MS. They can include
- Visual disturbances
- Muscle weakness
- Trouble with coordination and balance
- Sensations such as numbness, prickling, or “pins and needles”
- Thinking and memory problems
No one knows what causes MS. It may be an autoimmune disease, which happens when your immune system attacks healthy cells in your body by mistake. Multiple sclerosis affects women more than men. It often begins between the ages of 20 and 40. Usually, the disease is mild, but some people lose the ability to write, speak, or walk.
There is no single test for MS. Doctors use a medical history, physical exam, neurological exam, MRI, and other tests to diagnose it. There is no cure for MS, but medicines may slow it down and help control symptoms. Physical and occupational therapy may also help.
Investigation
- CT may be performed because of focal neurology but is insensitive
- MRI is the investigation of choice and should be performed with contrast and include the spine
- preferred imaging modailty for diagnosis and follow up
- best visualized on a fluid-sensitive sequence, e.g. T2, FLAIR
- white matter lesions
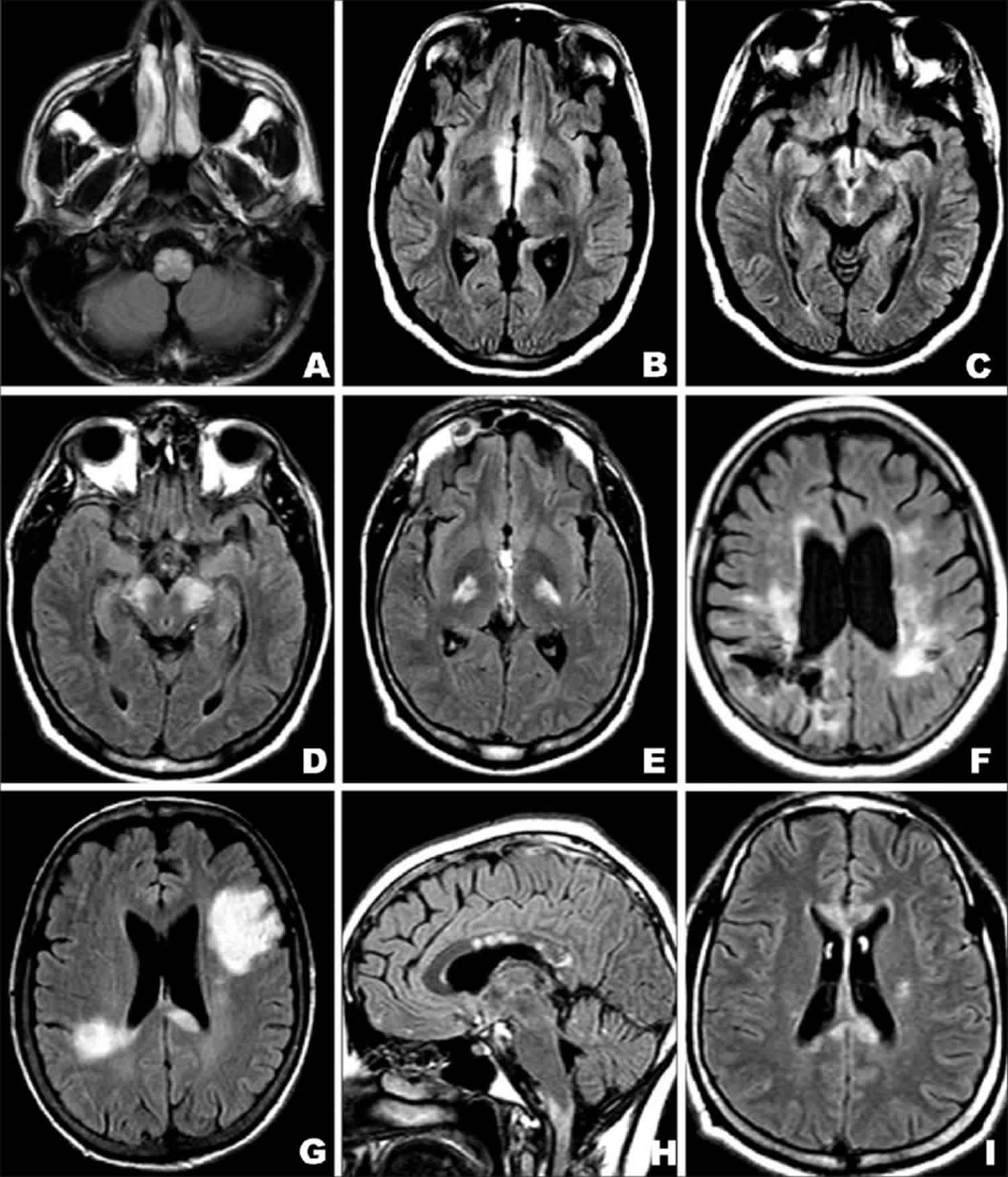
- characteristic periventricular, they tend to extend perpendicularly and on sagittal views are called “Dawson’s fingers” (Figure 1)
- lesions may occur throughout the CNS and be found in a variety of locations, e.g. juxtacortical, brainstem, cerebellum, or spinal cord (also part of the CNS)
- enhancement is a marker of activity and can be used to determine lesion load and disease progression
Dawson fingers are a radiographic feature of demyelination characterized by periventricular demyelinating plaques distributed along the axis of medullary veins, perpendicular to the body of the lateral ventricles and/or callosal junction. This is thought to reflect perivenular inflammation. They are a relatively specific sign for multiple sclerosis.
- T1: low signal in chronic lesions; otherwise usually isointense to white matter
- T2/FLAIR: linear or ovoid high signal
- T1C+ (Gd): enhancement can be seen with active lesions
Figure 1. MS brain lesions
Footnote: Multiple white matter plaques, some of them are perpendicular to the corpus callosum – so-called Dawson fingers – are typical of multiple sclerosis.
[Source 1 ]Figure 2. Brain metastases from melanoma
Footnote: 60 year old female who developed left-handed weakness which improved with corticosteroids. Neurological examination reveals left pronator drift and left sided arm and leg weakness. Right frontoparietal hyperdense intra-axial lesion that enhances in post contrast study. Small surrounding vasogenic edema. No significant mass effect.
[Source 2 ]Figure 3. Brain cancer
Footnote: 30 year with fainting episodes. The lesion in the left medial cranial fossa measures 30 x 40 x 35 mm, has broad contact with the cranial vault, but there is no reaction the adjacent bone and no meningeal enhancement. There is no evidence of cortex or CSF cleft between the lesion and deep white matter, confirming intra-axial site. There is no contrast enhancement. There is no diffusion restriction. Cerebral parenchymal signal intensity and architecture are elsewhere normal. There is no hydrocephalus. There is abnormal signal within the mass within the left globe, and the globe is of slightly smaller volume of the right, consistent with vitreous hemorrhage and/or retinal detachment. The tumor is almost certainly a diffuse astrocytoma IDH+ve and unlikely to have 1p19q deletion given prominent partial flair suppression. An outside possibility is a large DNET although this is much less likely.
[Source 3 ]Figure 4. Stroke
Footnote: Adult with two days after right hemiparesis and aphasia. . Typical appearances of an established middle cerebral artery territory infarct with pronounced restricted diffusion. MRI shows restricted diffusion in left MCA distribution in keeping with an acute infarct. Note the loss of normal grey white matter differentiation on T1 weighted images and the increased T2 signal and gyral swelling.
[Source 4 ]Figure 5. Traumatic brain injury
Footnote: 60 year male with tonic-clonic seizure with head injury. GCS 6. Bleeding from left ear and epistaxis. Multiple well defined hyperdensities in right frontal lobe, bilateral temporal lobes and left pareital lobe. Bilateral frontal subdural hyperdense hemorrhages. Left subdural collection of mixed density in keeping with acute on subacute subdural hemorrhage. Subarachnoid blood also present. Effacement of right lateral ventricle (adjacent to largest intraparenchymal bleed). Impression of frontal subfalcine displacement but other midline structures in normal position. Basal cisterns normal. Mixed transverse and longitudinal left temporal bone fracture involving mastoid and external auditory canal. Hyperdense fluid in mastoid air spaces, middle ear and external ear canal in keeping with blood. No involvement of venous sinuses or jugular system.
[Source 5 ]Brain lesions treatment
Treatment involves treating the underlying cause(s) of the brain lesion.
References- Multiple sclerosis. https://radiopaedia.org/cases/multiple-sclerosis-4
- Metastatic malignant melanoma. https://radiopaedia.org/cases/metastatic-malignant-melanoma
- Diffuse astrocytoma IDH-1 mutant. https://radiopaedia.org/cases/diffuse-astrocytoma-idh-1-mutant
- Left MCA Infarct. https://radiopaedia.org/cases/left-mca-infarct-2
- Multiple cerebral contusions and temporal bone fracture. https://radiopaedia.org/cases/multiple-cerebral-contusions-and-temporal-bone-fracture