What is calcium phosphate
Calcium phosphate is the calcium salt of phosphoric acid with widely used applications. Calcium phosphate is used to prevent and to treat calcium deficiencies. Calcium phosphate is typically available as an over the counter supplement or as an added ingredient in some toothpastes 1. Calcium phosphate (mono-, di-, and tribasic) is used as a multiple purpose food substance in food for human consumption is generally recognized as safe (GRAS) by the U.S. Food and Drug Administration (FDA) when used in accordance with good manufacturing practice 2. Calcium phosphates (E 341) [monocalcium phosphate (E 341i), dicalcium phosphate (E 341ii), tricalcium phosphate (E 341iii)] are used as food additive as raising agent, stabilizer, dough strengthener, anti-caking agent, texturizer, flour treating agent and acidity regulator. Calcium phosphate agent can also be used as a countermeasure for exposure to strontium and radium radionuclides. Upon oral uptake, calcium phosphate competes for and blocks the absorption of radium (Ra-226) and strontium (Sr-90) in the gastrointestinal (GI) tract 3. Various calcium phosphate minerals are used in the production of phosphoric acid and fertilizers.
Calcium phosphates are insoluble in water and constitute the following series: calcium phosphate (monobasic) which is used as acidulant and mineral supplement; calcium phosphate (dibasic) is used as dietary supplement in doses of 1 g orally; calcium phosphate (tribasic) is used as gastric antacid in doses of 1 g orally; and bone phosphate. Metabolically they behave as sources of calcium and phosphate ions.
Calcium and phosphate are multivalent cations that are important for many biologic and cellular functions. The kidneys play a central role in the homeostasis of calcium and phosphate ions 4. Gastrointestinal absorption is balanced by renal excretion. When body stores of these ions decline significantly, gastrointestinal absorption, bone resorption, and renal tubular reabsorption increase to normalize their levels. Renal regulation of these ions occurs through glomerular filtration and tubular reabsorption and/or secretion and is therefore an important determinant of plasma ion concentration. Under physiologic conditions, the whole body balance of calcium and phosphate is maintained by fine adjustments of urinary excretion to equal the net intake.
Calcium homeostasis
The total amount of calcium in the human body ranges from 1000 to 1200 g 4. Approximately 99% of body calcium resides in the skeleton; the other 1% is present in the extracellular and intracellular spaces 4. Although >99% of the total body calcium is located in bone, calcium is a critical cation in both the extracellular and intracellular spaces. Approximately 1% of the calcium in the skeleton is freely exchangeable with calcium in the extracellular fluid compartment. Serum calcium concentration is held in a very narrow range in both spaces. Calcium serves a vital role in nerve impulse transmission, muscular contraction, blood coagulation, hormone secretion, and intercellular adhesion 5. Calcium can also bind to other minerals (such as phosphate) and aid in their removal from the body.
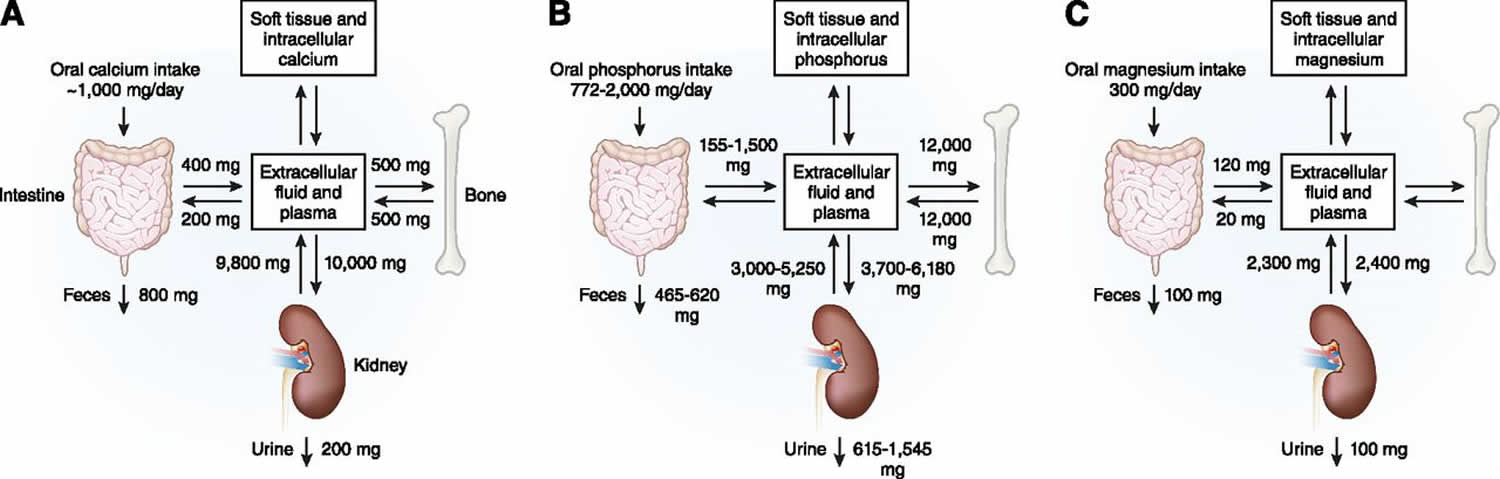
Figure 1. Calcium and phosphate homeostasis maintained by physiological processes
Footnote: Calcium (A), phosphate (B), and magnesium (C) balance is a complex process involving bone, intestinal absorption of dietary calcium, phosphate, and magnesium, and renal excretion of calcium, phosphate, and magnesium.
[Source 4 ]Gastrointestinal absorption of calcium
Calcium balance is tightly regulated by the concerted action of calcium absorption in the intestine, reabsorption in the kidney, and exchange from bone, which are all under the control of the calciotropic hormones that are released upon a demand for calcium (Figure 1 A above). In healthy adults, approximately 800–1000 mg of calcium should be ingested daily. This amount will vary depending on the amount of dairy product consumed. When 1 g of calcium is ingested in the diet, approximately 800 mg is excreted in the feces and 200 mg in the urine. Approximately 400 mg of the usual 1000 mg dietary calcium intake is absorbed by the intestine, and calcium loss by way of intestinal secretions is approximately 200 mg/d. Therefore, a net absorption of calcium is approximately 200 mg/d (20%) 6. Although serum calcium levels can be maintained in the normal range by bone resorption, dietary intake is the only source by which the body can replenish stores of calcium in bone. Calcium is absorbed almost exclusively within the duodenum, jejunum, and ileum. Each of these intestinal segments has a high absorptive capacity for calcium, with their relative calcium absorption being dependent on the length of each respective intestinal segment and the transit time of the food bolus 6.
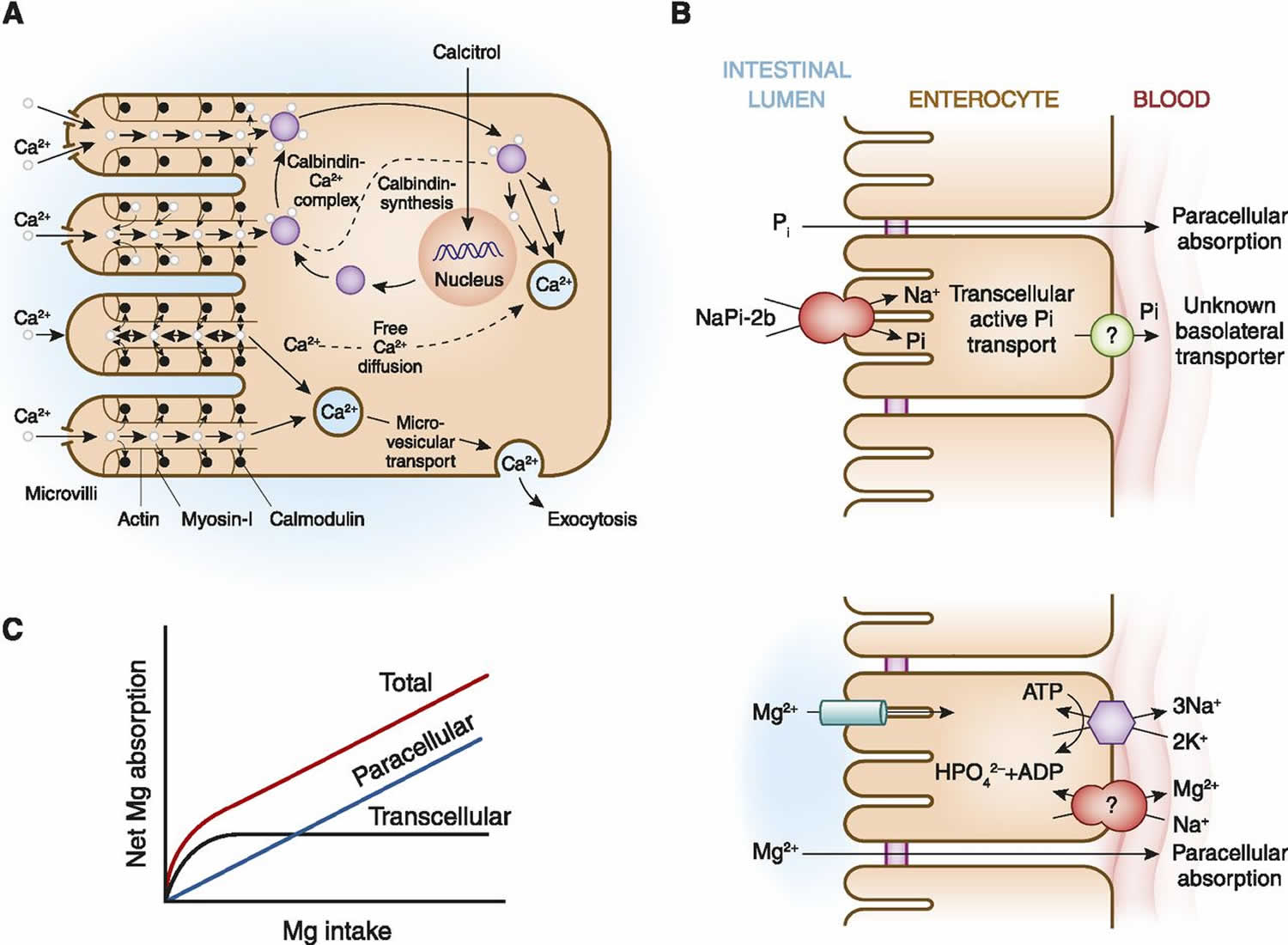
There are two routes for the absorption of calcium across the intestinal epithelium: the paracellular pathway (i.e., between the cells) and the transcellular route (i.e., through the cell) (Figure 2A). The paracellular pathway is passive, and it is the predominant route of calcium absorption when the lumen concentration of calcium is high. The paracellular route is indirectly influenced by calcitriol [1,25(OH)2D] because it is capable of altering the structure of intracellular tight junctions by activation of protein kinase C, making the tight junction more permeable to the movement of calcium. However, calcitriol (1,25(OH)2D) mainly controls the active absorption of calcium. Calcium moves down its concentration gradient through a calcium channel into the apical section of the microvillae. Because the luminal concentration of calcium is usually much higher than the intracellular concentration of calcium, a large concentration gradient favors the passive movement of calcium. Calcium is rapidly and reversibly bound to the calmodulin-actin-myosin I complex. Calcium moves to the basolateral area of the cell by way of microvesicular transport. As the calmodulin-actin-myosin I complex becomes saturated with calcium, the concentration gradient becomes less favorable, which slows down calcium absorption. Calcitriol (1,25(OH)2D) exerts influence on the intestinal epithelial cells to increase their synthesis of calbindin. Calcium binds to calbindin, thereby unloading the calcium-calmodulin complexes, which then remove calcium from the microvilli region. This decrease in calcium concentration again favors the movement of calcium into the microvilli. As the calbindin-calcium complex dissociates, the free intracellular calcium is actively extruded from the cell sodium-calcium (Na-Ca) exchanger 7.
Figure 2. Calcium and phosphate absorption
Footnote: (A) Proposed pathways for calcium (Ca) absorption across the intestinal epithelium. Two routes exist for the absorption of Ca across the intestinal epithelium: the paracellular pathway and the transcellular route. (B) Proposed pathways for phosphorus (Pi) absorption across the intestinal epithelium. NaPi2b mediates active transcellular transport of Pi. A paracellular pathway is also believed to exist. (C) Proposed pathways for magnesium (Mg) absorption across the intestinal epithelium. Apical absorption is mediated by the TRPM6/TRPM7 channel, whereas basolateral exit occurs by an magnesium (Mg) exchanger that is yet to be fully defined. A paracellular pathway is also believed to exist. TRPM (transient receptor potential melastatin).
[Source 4 ]Kidney regulation of calcium and phosphate balance
Total serum calcium consists of ionized, protein bound, and complexed fractions (approximately 48%, 46%, and 7%, respectively). The complexed calcium is bound to molecules such as phosphate and citrate. The ultrafilterable calcium equals the total of the ionized and complexed fractions. Normal total serum calcium is approximately 8.9–10.1 mg/dl (about 2.2–2.5 mmol/l). Calcium can be bound to albumin and globulins. For each 1.0-g/dl decrease in serum albumin, total serum calcium decreases by 0.8 mg/dl. For each 1.0-g/dl decrease in serum globulin fraction, total serum calcium decreases by 0.12 mg/dl. Acute alkalosis decreases the ionized calcium. Because both hydrogen ions and calcium are bound to serum albumin, in the presence of metabolic alkalosis, bound hydrogen ions dissociate from albumin, freeing up the albumin to bind with more calcium and thereby decreasing the freely ionized portion of the total serum calcium. For every 0.1 change in pH, ionized calcium changes by 0.12 mg/dl 8.
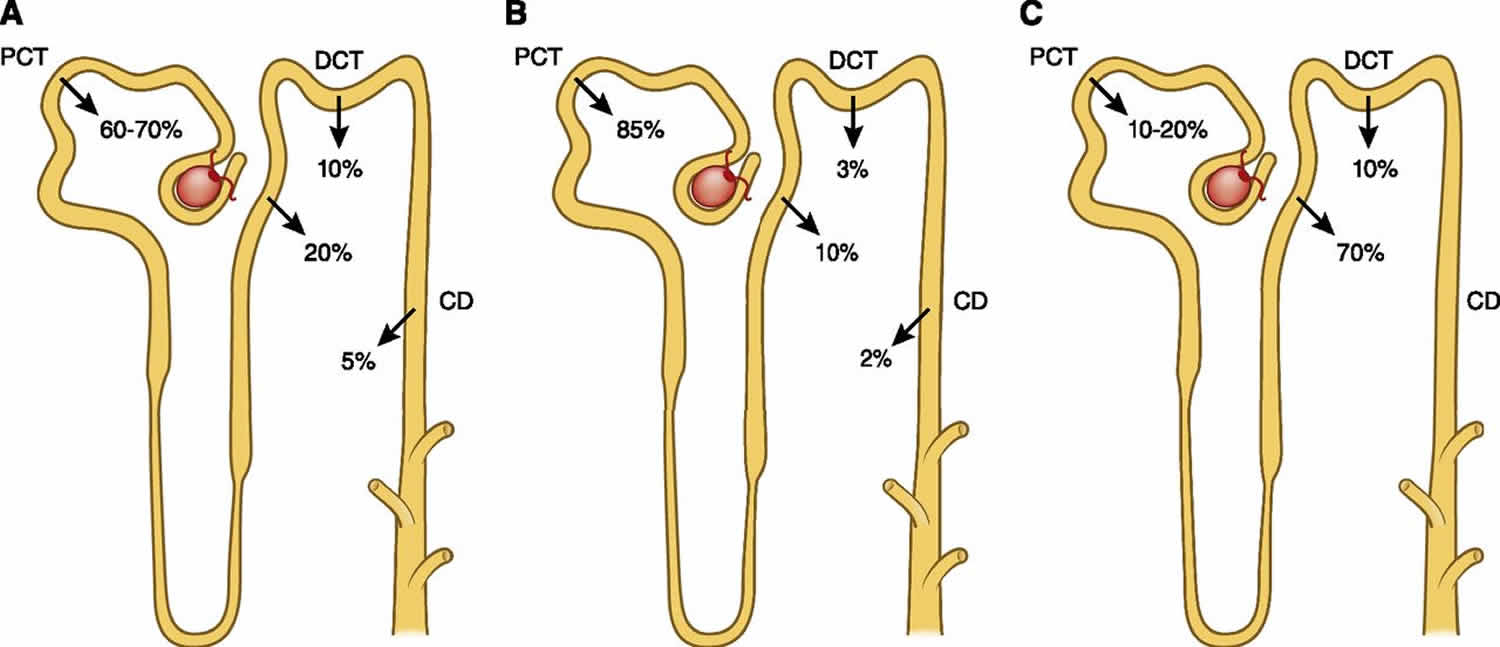
In humans who have a glomerular filtration rate (GFR) of 170 liters per 24 hours, roughly 10 g of calcium is filtered per day. The amount of calcium excreted in the urine usually ranges from 100 to 200 mg per 24 hours; hence, 98%–99% of the filtered load of calcium is reabsorbed by the renal tubules. Approximately 60%–70% of the filtered calcium is reabsorbed in the proximal convoluted tubule, 20% in the loop of Henle, 10% by the distal convoluted tubule, and 5% by the collecting duct. The terminal nephron, although responsible for the reabsorption of only 5%–10% of the filtered calcium load, is the major site for regulation of calcium excretion (Figure 3A) 5.
Figure 3. Kidney regulation of calcium and phosphate balance
Footnote: (A) Calcium is filtered at the glomerulus, with the ultrafilterable fraction of plasma calcium entering the proximal tubule. Within the proximal convoluted tubule and the proximal straight tubule, 60%–70% of the filtered calcium has been reabsorbed. No reabsorption of calcium occurs within the thin segment of the loop of Henle. The cortical segments of the loop of Henle reabsorb about 20% of the initially filtered load of calcium. Approximately 10% of the filtered calcium is reabsorbed in the distal convoluted tubule, with another 3%–10% of filtered calcium reabsorbed in the connecting tubule. (B) The majority (approximately 85%) of phosphate reabsorption occurs in the proximal convoluted tubule. Approximately 10% of Pi reabsorption occurs in the loop of Henle, 3% occurs in the distal convoluted tubule, and 2% in the collecting duct via unidentified pathways. (C) Approximately 10%–30% of the filtered magnesium is absorbed in the proximal tubule, 40%–70% of filtered magnesium is absorbed in the thick ascending limb, and the remaining 5%–10% of magnesium is reabsorbed in the distal convoluted tubule.
Abbreviations: CD = collecting duct; DCT = distal convoluted tubule; PCT = proximal convoluted tubule.
[Source 4 ]The reabsorption of calcium in the proximal convoluted tubule parallels that of sodium and water. Proximal tubular calcium reabsorption is thought to occur mainly by passive diffusion and solvent drag. This is based on the observation that the ratio of calcium in the proximal tubule fluid to that in the glomerular filtrate is 1:1.2. The passive paracellular pathways account for approximately 80% of calcium reabsorption in this segment of the nephron. A small but significant component of active calcium transport is observed in the proximal tubules. The active transport of calcium proceeds in a two-step process, with calcium entry from the tubular fluid across the apical membrane and exit though the basolateral membrane. This active transport is generally considered to constitute 10%–15% of total proximal tubule calcium reabsorption and it is mainly regulated by parathyroid hormone (PTH) and calcitonin 9.
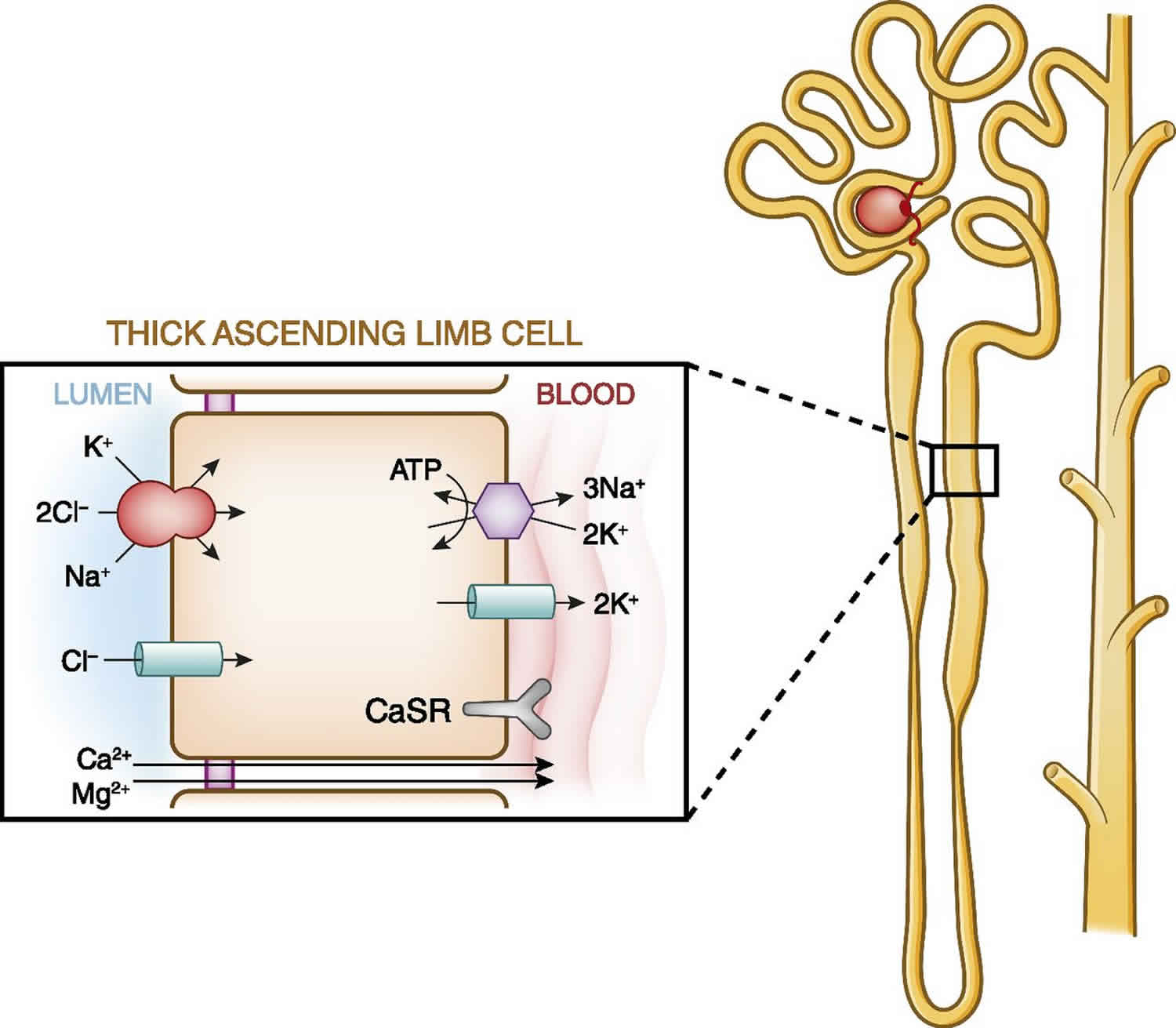
No reabsorption of calcium occurs within the thin segment of the loop of Henle (Figure 3A). In the thick ascending limb of the loop of Henle, 20% of the filtered calcium is reabsorbed largely by the cortical thick ascending limb, through both transcellular and paracellular routes. In the thick ascending limb, the bulk of calcium reabsorption proceeds through the paracellular pathway and is proportional to the transtubular electrochemical driving force. The apical Na+-K+-2Cl− cotransporter NKCC2 and the renal outer medullary potassium K+ (ROMK) channel generate the “driving force” for paracellular cation transport. Whereas NaCl reabsorption through NKCC2 is electroneutral (NKCC2 translocates one Na+ (sodium), one K+ (potasssium), and two Cl− (chloride) ions from the lumen into the cell), apical potassium represents the rate-limiting step of this process and potassium ions back-diffuse into the lumen through the renal outer medullary potassium K+ (ROMK) channels. Na+ and Cl− accumulated inside the cell are then transported into the bloodstream through basolateral Na+-K+-ATPase and Cl− channels, respectively. Overall, these processes yield a net cellular reabsorption of NaCl and the generation of a lumen-positive transepithelial potential difference, which drives nonselective calcium reabsorption through the paracellular route (Figure 4) 10. Calcium transport in the thick ascending limb of the loop of Henle is also influenced by the calcium-sensing receptor (CaSR) 9, which is localized in the basolateral membrane. How calcium-sensing receptor (CaSR) controls the calcium reabsorption in the thick ascending limb is now better understood. Using microdissected, in vitro microperfused rat cortical thick ascending limb, Loupy et al. 11 showed that an acute inhibition of the calcium-sensing receptor (CaSR) does not alter NaCl reabsorption or the transepithelial potential difference but increased the permeability to calcium of the paracellular pathway. The tight junction in the thick ascending limb expresses several claudins, including claudin-14, claudin-16, and claudin-19. A normal expression of claudin-16 and claudin-19 is required for a normal absorption of divalent cations in this tubular segment. Toka et al. 12 reported that the disruption of calcium-sensing receptor (CaSR) decreases the abundance of the claudin-14 mRNA and increases that of the claudin-16 mRNA. A treatment by cinacalcet increases the abundance of claudin-14 mRNA, and in cell culture models overexpression of claudin-14, decreases the paracellular permeability to calcium 12. Calciotropic hormones, such as parathyroid hormone (PTH) and calcitonin, stimulate active cellular calcium absorption in the cortical thick ascending limb 9.
Figure 4. Kidney regulation of calcium and magnesium balance
Footnote: Calcium absorption proceeds through both an active, transcellular pathway and by a passive paracellular pathway. Only transport pathways relevant to calcium absorption are shown. Basal absorption is passive and is driven by the ambient electrochemical gradient for calcium. The apical Na+-K+-2Cl− cotransporter and the renal outer medullary potassium K+ channel generate the “driving force” for paracellular cation transport. Calciotropic hormones, such as parathyroid hormone and calcitonin, stimulate active calcium absorption in cortical thick ascending limbs. Inhibition of Na-K-2Cl cotransport by loop diuretics or in Bartter’s syndrome decreases the transepithelial voltage, thus diminishing passive calcium absorption. In the model of magnesium absorption by thick ascending limb of Henle, 40%–70% of filtered magnesium is absorbed in the thick ascending limb by a paracellular pathway, mostly enhanced by lumen-positive transepithelial voltage. The apical Na-K-2Cl cotransporter mediates apical absorption of Na, K, and Cl. The apical renal outer medullary K channel mediates apical recycling of K back to the tubular lumen and generates lumen-positive voltage. Cl channel Kb mediates Cl exit through the basolateral membrane. Here Na,K-ATPase also mediates Na exit through the basolateral membrane and generates the Na gradient for Na absorption. The tight junction proteins claudin-16 and claudin-19 play a prominent role in magnesium absorption. The calcium-sensing receptor was also recently determined to regulate magnesium transport in this segment: upon stimulation, magnesium transport is decreased.
Abbreviations: Na+ = sodium ion; K+ = potassium ion; Cl− = chloride ion; CaSR = calcium-sensing receptor
[Source 4 ]Hormonal and other Factors Regulating Renal Calcium Handling
Parathyroid hormone (PTH)
Many physiologic, pharmacologic, and pathologic factors influence renal calcium absorption (Table 1). The most important regulator is parathyroid hormone (PTH), which stimulates calcium absorption. parathyroid hormone (PTH) is a polypeptide secreted from the parathyroid gland in response to a decrease in the plasma concentration of ionized calcium. Therefore, the major physiologic role of the parathyroid gland is to regulate calcium homeostasis. Parathyroid hormone (PTH) acts to increase the plasma concentration of calcium in three ways: (1) it stimulates bone resorption, (2) it enhances intestinal calcium and phosphate absorption by promoting the formation within the kidney of calcitriol (1,25(OH)2D), and (3) it augments active renal calcium absorption. These effects are reversed by small changes in the serum calcium concentration that lower parathyroid hormone (PTH) secretion.
Table 1. Factors that alter renal regulation of calcium
| Increase Calcium Absorption | Decrease Calcium Absorption |
| Hyperparathyroidism | Hypoparathyroidism |
| Calcitriol | Low calcitriol levels |
| Hypocalcemia | Hypercalcemia |
| Volume contraction | Extracellular fluid expansion |
| Metabolic alkalosis | Metabolic acidosis |
| Thiazides diuretics | Loop diuretics |
Daily phosphate homeostasis
At steady state, oral phosphorus intake is balanced by phosphate (Pi) excretion in the urine and feces (see Figure 1B above). Daily phosphorus intake varies between 700 and 2000 mg, depending on consumption of phosphorus-rich foods, such as dairy products. After absorption, phosphorus is transported across cell membranes as phosphate (31 mg/l elemental phosphorus=1 mmol/l phosphate). Phosphate in the plasma or extracellular fluid undergoes one of three fates: transport into cells, deposition in bone or soft tissue, or elimination predominantly by the kidneys. Within the body, the majority of phosphorus stores are in the bone. Although serum phosphate (Pi) levels constitute <1% of total body phosphorus stores, maintenance of serum Pi within a relatively narrow range (2.5–4.5 mg/dl in adulthood) is crucial for several important cellular processes, including energy metabolism, bone formation, signal transduction, or as a constituent of phospholipids and nucleic acids 13. Maintenance of serum phosphate within the normal range depends on a complex interplay between absorption of phosphate in the gut, exchange with bone stores, shifts between intracellular and intravascular compartments, and renal excretion.
Gastrointestinal absorption of phosphate
Although the kidneys are the major regulators of phosphate homeostasis, serum levels of phosphate are also altered by intestinal Pi absorption mediated by the type IIb NaPi cotransporters Npt2b (see Figure 2B above) 14. Npt2b is regulated by dietary phosphate intake as well as calcitriol [1,25(OH)2D]. In the rat, phosphate reabsorption is greatest in the duodenum and the jejunum, with very little occurring in the ileum. By contrast, in the mouse, Pi is absorbed along the entire intestine with the highest levels of phosphate reabsorption occurring in the ileum. The human pattern of intestinal phosphate reabsorption is thought to resemble that found in the rat.
Kidney regulation of phosphate balance
The kidney plays a key role in phosphate homeostasis. In normal adults, between 3700 and 6100 mg/d of phosphorus is filtered by the glomerulus (Figure 1B). Net renal excretion of phosphorus is between 600 and 1500 mg/d, which means that between 75% and 85% of the daily filtered load is reabsorbed by the renal tubules.
Maintenance of normal serum phosphorus levels is primarily achieved through a tightly regulated process of phosphate reabsorption from the glomerular filtrate. Within the nephron, approximately 85% of phosphate reabsorption occurs within the proximal tubule (Figure 3B). The remainder of the nephron plays a minor role in phosphate regulation and the transporters involved have yet to be identified 15.
Within the proximal tubule, phosphate transport from the ultrafiltrate across the proximal tubule epithelium is an energy-dependent process that requires sodium 16. The three renal sodium phosphate cotransporters, Npt2a, Npt2c, and PiT-2, are all positioned in the apical brush border membrane of renal proximal tubule cells and use the energy derived from the transport of sodium down its gradient to move inorganic phosphate from the luminal filtrate into the cell. The amount of phosphate reabsorbed from the filtrate is determined by the abundance of the cotransporters in the apical membrane of proximal tubule cells and not by any alterations in the rate or affinity of phosphate transport by post-transcriptional modifications 16. Thus, hormones or dietary factors that alter phosphate reabsorption in the kidney do so by changing the abundance of the sodium phosphate cotransporters in the apical membrane of renal proximal tubule cells. An increase in the brush border levels of the sodium phosphate cotransporters abundance results in increased phosphate absorption from the urine, whereas a decrease in cotransporter abundance leads to phosphaturia. Transport of phosphate from the renal proximal tubule to the peritubular capillaries occurs via an unknown basolateral transporter 17.
Renal control of phosphate reabsorption is regulated by a number of hormonal and metabolic factors (Table 2) that are discussed below in more detail. These factors change phosphate reabsorption from the ultrafiltrate by changing the abundance of the three sodium phosphate cotransporters in the brush border membrane of the proximal tubule. It should be noted that the time course of response to various stimulatory or inhibitory factors differs between the three cotransporters. In general, dietary or hormonal changes result in relatively rapid (minutes to hours) insertion or removal of Npt2a from the brush border membrane, whereas regulation of Npt2c and PiT-2 occurs more slowly (hours to days) 15.
Table 2. Factors that alter renal regulation of phosphate
| Increase Phosphate Absorption | Decrease Phosphate Absorption |
| Low-phosphate diet | Parathyroid hormone |
| 1,25-Vitamin D3 | Phosphatonins e.g., fibroblast growth factor-23 (FGF23) |
| Thyroid hormone | High-phosphate diet |
| Metabolic acidosis | |
| Potassium deficiency | |
| Glucocorticoids | |
| Dopamine | |
| Hypertension | |
| Estrogen |
Dietary factors regulating renal phosphate handling
In animals with normal renal function, ingestion of phosphorus-containing foods leads to removal of Npt2a, Npt2c, and PiT-2 from the proximal tubule brush border membrane, thereby decreasing phosphate reabsorption from the ultrafiltrate. By contrast, dietary phosphate restriction leads to insertion of the sodium phosphate cotransporters in the proximal tubule brush border membrane, increasing phosphate reabsorption.
Potassium deficiency leads to an increase in phosphate excretion in the urine despite a paradoxical increase in the abundance of Npt2a in the proximal tubule brush border membrane that should increase phosphate reabsorption. Potassium deficiency leads to changes in the brush border membrane lipid composition that are thought to inhibit Npt2a activity 18.
Hormonal and otherfactors regulating renal phosphate handling
Parathyroid hormone (PTH).
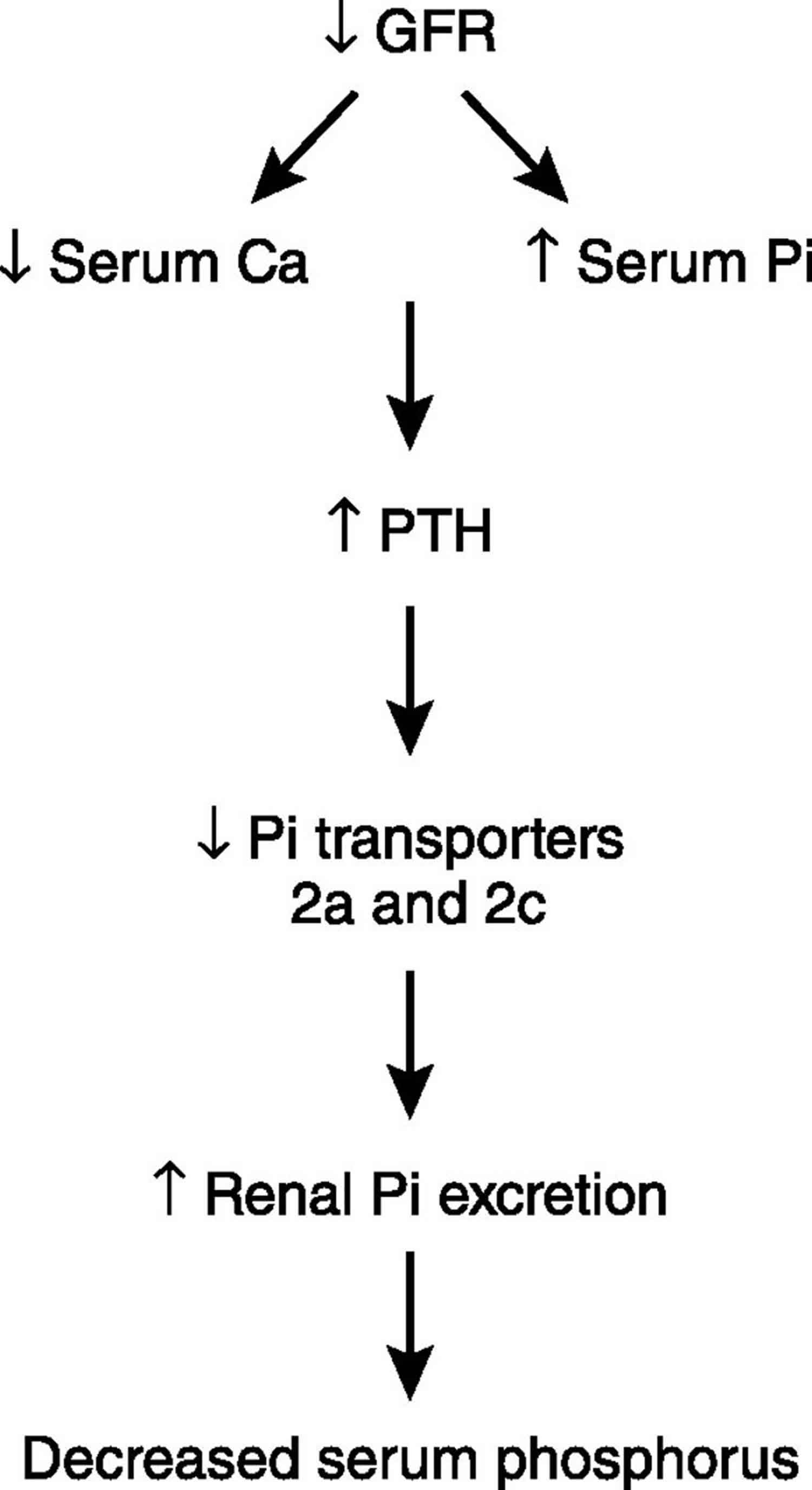
Parathyroid hormone (PTH) causes decreased renal reabsorption of phosphate and phosphaturia by decreasing the abundance of Npt2a, Npt2c, and PiT-2 in the renal proximal tubule brush border membrane (Figure 5). In response to parathyroid hormone (PTH), Npt2a is removed rapidly (within minutes), whereas the decrease in apical membrane abundance of Npt2c and PiT-2 takes hours 19. The sodium phosphate cotransporter response to parathyroid hormone (PTH) involves several kinases, including protein kinases A and C and mitogen-activated protein kinase extracellular signal-regulated kinase 1/2, as well as a myosin motor (myosin VI) 20.
Figure 5. Parathyroid hormone (PTH) controling phosphate homeostasis
Footnote: As glomerular filtration rate (GFR) falls, serum phosphorus levels increase, which stimulates release of parathyroid hormone (PTH) from the parathyroid glands. This in turn decreases the brush border abundance of Npt2a and Npt2c in the renal proximal tubule, leading to increased urinary excretion of phosphorus.
[Source 4 ]Fibroblast Growth Factor-23
Fibroblast growth factor-23 (FGF23) is produced in osteoblasts in response to increases in serum phosphate. To exert its physiologic effects on the proximal tubule, FGF23 requires the presence of a cofactor, Klotho, which is produced in the kidney and activates FGF receptor 1 21. Fibroblast growth factor-23 (FGF23) reduces the expression and activity of the sodium phosphate cotransporters in the renal proximal tubule and is also thought to decrease the activity of the intestinal sodium phosphate cotransporter. Fibroblast growth factor-23 (FGF23) also reduces serum levels of calcitriol by decreasing the renal expression of 1α-hydroxylase, which is the rate-limiting step in calcitriol synthesis, and increasing renal expression of 24-hydroxylase, which is required for calcitriol degradation 22. In addition, FGF23 suppresses parathyroid hormone (PTH) synthesis, although the parathyroid glands are believed to become resistant to FGF23 as kidney disease progresses.
Calcitriol
Calcitriol is believed to increase phosphate reabsorption in the proximal tubule 23 but the effects are confounded by the fact that changes in calcitriol (1,25(OH)2D) also alter plasma calcium and parathyroid hormone (PTH) levels.
Glucocorticoids
Increased glucocorticoid levels lead to decreased proximal tubule synthesis and abundance of Npt2a as well as changes in brush border membrane lipid composition, which is thought to modulate sodium phosphate cotransporter activity 24.
Estrogen
Estrogen causes phosphaturia by decreasing the abundance of Npt2a in the proximal tubule without altering Npt2c levels 25. Estrogen also increases fibroblast growth factor-23 (FGF23) synthesis 26.
Thyroid Hormone
Increased levels of thyroid hormone increase phosphate absorption by increasing proximal tubule transcription and expression of Npt2a 27. The Npt2a gene contains a thyroid response element and transcription of Npt2a mRNA is regulated by 3,5,3-tri-iodothyronine 28.
Dopamine
Dopamine leads to phosphaturia by inducing internalization of Npt2a from the proximal tubule brush border membrane. Dopamine-mediated internalization of Npt2a is dependent on a scaffolding protein (sodium-hydrogen exchanger regulatory factor 1) because dopamine does not induce phosphaturia in sodium-hydrogen exchanger regulatory factor 1 knockout mice 29.
Metabolic Acidosis
Metabolic acidosis stimulates phosphaturia, which helps remove acid from the blood because phosphate serves as a titratable acid 30. By contrast, metabolic alkalosis increases renal phosphate absorption 31. In mice, acidosis increases proximal tubule brush border membrane abundance of Npt2a and Npt2c, suggesting that phosphaturia results from inhibition of sodium phosphate cotransporter activity rather than changes in the levels of these proteins.
Hypertension
An acute increase in blood pressure leads to decreased renal phosphate reabsorption by inducing removal of Npt2a from the proximal tubule brush border membrane microvilli to subapical endosomes 32.
Calcium phosphate uses
Calcium phosphates are found in many living organisms, e.g., bone mineral and tooth enamel. In milk, it exists in a colloidal form in micelles bound to casein protein with magnesium, zinc, and citrate – collectively referred to as colloidal calcium phosphate 33. Calcium phosphate is typically available as an over the counter supplement, antacid, or as an added ingredient in some toothpastes 1. Calcium phosphate supplement is used to prevent and to treat calcium deficiencies. Calcium phosphate (mono-, di-, and tribasic) is also used as a multiple purpose food substance in food for human consumption is generally recognized as safe (GRAS) by the U.S. Food and Drug Administration (FDA) when used in accordance with good manufacturing practice 2. Calcium phosphates (E 341) [monocalcium phosphate (E 341i), dicalcium phosphate (E 341ii), tricalcium phosphate (E 341iii)] are used as food additive as raising agent, stabilizer, dough strengthener, anti-caking agent, texturizer, flour treating agent and acidity regulator. At the same time, calcium phosphate may serve complimentary as a nutrient source for calcium and potentially improve nutrient profile of processed foodstuffs.
Calcium phosphate agent can also be used as a countermeasure for exposure to strontium and radium radionuclides. Upon oral uptake, calcium phosphate competes for and blocks the absorption of radium (Ra-226) and strontium (Sr-90) in the gastrointestinal (GI) tract 3. Various calcium phosphate minerals are used in the production of phosphoric acid and fertilizers.
Is calcium phosphate bad for you?
Calcium phosphate supplement is contraindicated in patients with hypercalcemia, renal calculi, or hypophosphatemia.
Calcium phosphates are insoluble in water and constitute the following series: calcium phosphate (monobasic) which is used as acidulant and mineral supplement; calcium phosphate (dibasic) is used as dietary supplement in doses of 1 g orally; calcium phosphate (tribasic) is used as gastric antacid in doses of 1 g orally; and bone phosphate. Metabolically they behave as sources of calcium and phosphate ions 34. These compounds have been evaluated for acceptable daily intake by the Joint Food and Agriculture Organization of the United Nations (FAO)/World Health Organization (WHO) Expert Committee on Food Additives (JECFA) in 1961, 1963, 1964, 1965, 1969 and 1970 34.
Studies on 15 students, who drank 2000-4000 mg of phosphoric acid in fruit juices every day for 10 days, and on 2 males who received 3900 mg of phosphoric acid every day for 14 days, revealed no observable change in urine composition indicative of a disturbed metabolism 35.
Thomas 36 administered orthophosphates to some 37 renal calculi patients for periods of up to 8 years with usually favorable results. Two groups of anionic inhibitors of mineralization were found in the urine and the more potent of these was found to be present at a lower concentration in the urine of affected patients when compared with normal controls. Alkaline phosphate (K2HPO4) was found to cause increased concentrations of these mineralization inhibitors in urine (acidic and neutral phosphates increased only the less potent inhibitor).
In a study in which the daily basal diet of 4 men contained 450 mg calcium and 1400 mg phosphate, supplementation with 750 mg phosphorus as phosphoric acid for 1 week resulted in a slight decrease in urinary excretion of calcium. When the treatment was continued for 12 weeks, there was a further decrease in urinary calcium excretion 37. In another study, groups of 6 women previously on a basal diet containing 300 mg calcium and 800 mg phosphate, received a diet containing 1500 mg calcium and 1400 mg phosphate, or 1500 mg calcium and 800 mg phosphate. The high level of phosphate in the first diet resulted in decreased calcium utilization when compared to the second group 38.
The toxicity of calcium phosphate compounds is in part due to separate problems arising from the various cations and to the phosphate anions in general. They are primarily due to excess phosphate in the diet, and deficiencies in calcium and magnesium. Metabolically, the phosphate salts provide a source of the various cations and the phosphate ion. Of greatest concern is the toxicity arising from calcium, magnesium and phosphate imbalance in the diet. Phosphate salts were not mutagenic in a number of test systems. Teratogenic effects have not been observed in mammalian test systems.
Numerous animal studies have shown that excessive dietary phosphate causes an increase of plasma phosphate and a decrease in serum calcium. The resulting hypocalcaemia stimulates secretion of parathyroid hormone (PTH) which in turn increases the rate of bone resorption and decreases calcium excretion. These homeostatic adjustments to high dietary phosphate may result in bone loss and calcification of soft tissues in animals.
The dose levels of phosphate producing nephrocalcinosis were not consistent among the various rat feeding studies. However, the rat is exquisitely susceptible to calcification and hydronephrosis upon exposure to acids forming calcium chelates or complexes. The lowest dose levels that produce nephrocalcinosis overlap the higher dose levels failing to do so. However, this may be related to other dietary imbalances, such as the level of magnesium in the diet. There is still uncertainty on the optimal calcium-phosphate ratio and whether this ratio is of any dietary significance in man.
The lowest level of phosphate that produced nephrocalcinosis in the rat (1% phosphate in the diet) is used as the basis for the evaluation and, by extrapolation based on the daily food intake of 2800 calories, this gives a dose level of 6600 mg phosphate per day as the best estimate of the lowest level that might conceivably cause nephrocalcinosis in man.
The usual calculation for provision of a margin of safety is probably not suitable for food additives that are also nutrients. Ingested phosphates from natural sources should be considered together with that from food additives sources. Since phosphorus (as phosphates) is an essential nutrient and an unavoidable constituent of food, it is not feasible or appropriate to give a range of values from zero to a maximum.
Monophosphates have already been evaluated in the Seventh Report of the Joint FAO/WHO Expert Committee on Food Additives. The acceptable daily intake for man of phosphates as additives should be related to the total dietary phosphatesa and calcium intake.
- Estimate of acceptable daily phosphate intake for man (as total dietary phosphorous intake from both food and food additives) 0 – 30 mg/kg body weight per day 39.
- Estimate of maximum tolerable daily intake for man 70 mg/kg body weight per day. Note: The maximum tolerable daily intake is expressed as phosphorus and it applies to the sum of phosphates naturally present in food and the additives. It also applies to diets that are nutritionally adequate in respect of calcium. However, if the calcium intake were high, the intake of phosphate could be proportionately higher, and the reverse relationship would also apply.
Calcium phosphate supplement
Calcium phosphate is used to prevent and to treat calcium deficiencies. Each tablet provides 600 mg of elemental calcium. The recommended daily allowance (RDA) of calcium is 800 mg. The recommended daily allowance (RDA) for pregnant or breastfeeding women is 1,200 mg.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Before taking calcium phosphate supplement
To make sure you can safely take calcium phosphate, tell your doctor if you have any of these other conditions:
- a history of kidney stones; or
- a parathyroid gland disorder.
Talk to your doctor before taking calcium phosphate if you are pregnant.
Talk to your doctor before taking calcium phosphate if you are breast-feeding a baby.
How should I take calcium phosphate?
Use exactly as directed on the label, or as prescribed by your doctor. Do not use in larger or smaller amounts or for longer than recommended.
Calcium phosphate works best if you take it with food.
Take calcium phosphate with a full glass of water.
Store at room temperature away from moisture and heat.
Adult Dose for Hypocalcemia
- 1 to 2 tablets orally once a day.
Adult Dose for Osteomalacia
- 1 to 2 tablets orally once a day.
Adult Dose for Osteoporosis
- 1 to 2 tablets orally once a day.
Adult Dose for Pseudohypoparathyroidism
1 to 2 tablets orally once a day.
Adult Dose for Hypoparathyroidism
- 1 to 2 tablets orally once a day.
What happens if I miss a dose?
Take the missed dose as soon as you remember. Skip the missed dose if it is almost time for your next scheduled dose. Do not take extra medicine to make up the missed dose.
Renal Dose Adjustments
Patients with renal dysfunction have an increased risk of hypercalcemia. Periodically checking the serum calcium level, especially if signs or symptoms of hypercalcemia are detected, is recommended.
Dialysis
Calcium is removed by hemodialysis. To ensure a positive net calcium flux into the patient during dialysis, a dialysate calcium concentration of 3 to 3.5 mEq/L is usually required. Modest mid-dialysis hypercalcemia is not uncommon when this concentration is used.
Calcium is removed by peritoneal dialysis. The standard peritoneal dialysate contains 3.5 mEq/L of calcium (in 1.5% dextrose) to maintain a positive calcium balance and to prevent calcium losses. When higher concentrations of dextrose are used, the net calcium balance may be negative because of a greater convective removal of calcium during ultrafiltration, which counterbalances the diffusion of calcium from the dialysate to the patient.
Liver Dose Adjustments
- Data not available
What other drugs will affect calcium phosphate?
Calcium phosphate can make it harder for your body to absorb other medications you take by mouth. Tell your doctor if you are taking:
- digoxin (Lanoxin, Lanoxicaps);
- antacids or other calcium supplements;
- calcitriol (Rocaltrol) or vitamin D supplements; or
- doxycycline (Adoxa, Doryx, Oracea, Vibramycin), minocycline (Dynacin, Minocin, Solodyn, Vectrin), or tetracycline (Brodspec, Panmycin, Sumycin, Tetracap).
This list is not complete and other drugs may interact with calcium phosphate. Tell your doctor about all medications you use. This includes prescription, over-the-counter, vitamin, and herbal products. Do not start a new medication without telling your doctor.
Calcium phosphate side effects
Get emergency medical help if you have any of these signs of an allergic reaction while taking calcium phosphate tablets: hives; difficulty breathing; swelling of your face, lips, tongue, or throat.
Less serious side effects of calcium phosphate, tribasic may include:
- nausea or vomiting;
- decreased appetite;
- constipation;
- dry mouth or increased thirst; or
- increased urination.
Overdose symptoms may include nausea, vomiting, decreased appetite, constipation, confusion, delirium, stupor, and coma.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects.
Gastrointestinal
- Gastrointestinal side effects have included nausea in up to 9% of patients receiving calcium phosphate with vitamin D and fluoride.
Metabolic
Metabolic side effects have included hyperphosphatemia and hypercalciuria. Hypercalcemia has been reported with some calcium salts; however, it has not yet been associated with the use of calcium phosphate.
Metabolic changes associated with some calcium salts include hypercalcemia, although this has not yet been associated with the use of calcium phosphate.
Hyperphosphatemia can result from overuse.
Prolonged calcium administration of some calcium salts has rarely resulted in hypercalciuria. This may be more likely in patients with hypoparathyroidism who are receiving vitamin D.
Cardiovascular
Cardiovascular side effects have included a single case report of systemic tricalcium phosphate crystallosis involving the heart (myocarditis and pericarditis).
References- Calcium Phosphate. https://www.drugbank.ca/drugs/DB11348
- Food Additive Status List. https://www.fda.gov/Food/IngredientsPackagingLabeling/FoodAdditivesIngredients/ucm091048.htm
- Tricalcium phosphate. https://pubchem.ncbi.nlm.nih.gov/compound/24456
- Renal Control of Calcium, Phosphate, and Magnesium Homeostasis. Judith Blaine, Michel Chonchol, Moshe Levi. CJASN Jul 2015, 10 (7) 1257-1272; DOI: 10.2215/CJN.09750913
- Jacobson HR, Striker GE, Klahr S & Kumar R. Calcium metabolism. In: The Principles and Practice of Nephrology, edited by Jacobson HR, Striker GE, Klahr S, 2nd Ed., St. Louis, MO, Mosby-Year Book, 1995, pp 964–971
- Johnson JA, Kumar R. Renal and intestinal calcium transport: Roles of vitamin D and vitamin D-dependent calcium binding proteins. Semin Nephrol 14: 119–128, 1994
- Keller J, Schinke T. The role of the gastrointestinal tract in calcium homeostasis and bone remodeling. Osteoporos Int 24: 2737–2748, 2013
- Friedman PA, Gesek FA. Cellular calcium transport in renal epithelia: Measurement, mechanisms, and regulation. Physiol Rev 75: 429–471, 1995
- Felsenfeld A, Rodriguez M, Levine B. New insights in regulation of calcium homeostasis. Curr Opin Nephrol Hypertens 22: 371–376, 2013
- Riccardi D, Brown EM. Physiology and pathophysiology of the calcium-sensing receptor in the kidney. Am J Physiol Renal Physiol 298: F485–F499, 2010
- Loupy A, Ramakrishnan SK, Wootla B, Chambrey R, de la Faille R, Bourgeois S, Bruneval P, Mandet C, Christensen EI, Faure H, Cheval L, Laghmani K, Collet C, Eladari D, Dodd RH, Ruat M, Houillier P. PTH-independent regulation of blood calcium concentration by the calcium-sensing receptor. J Clin Invest 122: 3355–3367, 2012
- Toka HR, Al-Romaih K, Koshy JM, DiBartolo S 3rd., Kos CH, Quinn SJ, Curhan GC, Mount DB, Brown EM, Pollak MR. Deficiency of the calcium-sensing receptor in the kidney causes parathyroid hormone-independent hypocalciuria. J Am Soc Nephrol 23: 1879–1890, 2012
- Biber J, Hernando N, Forster I. Phosphate transporters and their function. Annu Rev Physiol 75: 535–550, 2013
- Marks J, Debnam ES, Unwin RJ. Phosphate homeostasis and the renal-gastrointestinal axis. Am J Physiol Renal Physiol 299: F285–F296, 2010
- Blaine J, Weinman EJ, Cunningham R. The regulation of renal phosphate transport. Adv Chronic Kidney Dis 18: 77–84, 2011
- Forster IC, Hernando N, Biber J, Murer H. Proximal tubular handling of phosphate: A molecular perspective. Kidney Int 70: 1548–1559, 2006
- Azzarolo AM, Ritchie G, Quamme GA. Some characteristics of sodium-independent phosphate transport across renal basolateral membranes. Biochim Biophys Acta 1064: 229–234, 1991
- Breusegem SY, Takahashi H, Giral-Arnal H, Wang X, Jiang T, Verlander JW, Wilson P, Miyazaki-Anzai S, Sutherland E, Caldas Y, Blaine JT, Segawa H, Miyamoto K, Barry NP, Levi M. Differential regulation of the renal sodium-phosphate cotransporters NaPi-IIa, NaPi-IIc, and PiT-2 in dietary potassium deficiency. Am J Physiol Renal Physiol 297: F350–F361, 2009
- Déliot N, Hernando N, Horst-Liu Z, Gisler SM, Capuano P, Wagner CA, Bacic D, O’Brien S, Biber J, Murer H. Parathyroid hormone treatment induces dissociation of type IIa Na+-P(i) cotransporter-Na+/H+ exchanger regulatory factor-1 complexes. Am J Physiol Cell Physiol 289: C159–C167, 2005
- Lederer ED, Khundmiri SJ, Weinman EJ. Role of NHERF-1 in regulation of the activity of Na-K ATPase and sodium-phosphate co-transport in epithelial cells. J Am Soc Nephrol 14: 1711–1719, 2003
- Berndt T, Kumar R. Phosphatonins and the regulation of phosphate homeostasis. Annu Rev Physiol 69: 341–359, 2007
- Hasegawa H, Nagano N, Urakawa I, Yamazaki Y, Iijima K, Fujita T, Yamashita T, Fukumoto S, Shimada T. Direct evidence for a causative role of FGF23 in the abnormal renal phosphate handling and vitamin D metabolism in rats with early-stage chronic kidney disease. Kidney Int 78: 975–980, 2010
- Kurnik BR, Hruska KA. Mechanism of stimulation of renal phosphate transport by 1,25-dihydroxycholecalciferol. Biochim Biophys Acta 817: 42–50, 1985
- Levi M, Shayman JA, Abe A, Gross SK, McCluer RH, Biber J, Murer H, Lötscher M, Cronin RE. Dexamethasone modulates rat renal brush border membrane phosphate transporter mRNA and protein abundance and glycosphingolipid composition. J Clin Invest 96: 207–216, 1995
- Faroqui S, Levi M, Soleimani M, Amlal H. Estrogen downregulates the proximal tubule type IIa sodium phosphate cotransporter causing phosphate wasting and hypophosphatemia. Kidney Int 73: 1141–1150, 2008
- Cannata-Andía JB, Carrillo-López N, Naves-Díaz M. Estrogens and bone disease in chronic kidney disease: Role of FGF23. Curr Opin Nephrol Hypertens 19: 354–358, 2010
- Alcalde AI, Sarasa M, Raldúa D, Aramayona J, Morales R, Biber J, Murer H, Levi M, Sorribas V. Role of thyroid hormone in regulation of renal phosphate transport in young and aged rats. Endocrinology 140: 1544–1551, 1999
- Ishiguro M, Yamamoto H, Masuda M, Kozai M, Takei Y, Tanaka S, Sato T, Segawa H, Taketani Y, Arai H, Miyamoto K, Takeda E. Thyroid hormones regulate phosphate homoeostasis through transcriptional control of the renal type IIa sodium-dependent phosphate co-transporter (Npt2a) gene. Biochem J 427: 161–169, 2010
- Weinman EJ, Biswas R, Steplock D, Douglass TS, Cunningham R, Shenolikar S. Sodium-hydrogen exchanger regulatory factor 1 (NHERF-1) transduces signals that mediate dopamine inhibition of sodium-phosphate co-transport in mouse kidney. J Biol Chem 285: 13454–13460, 2010
- Nowik M, Picard N, Stange G, Capuano P, Tenenhouse HS, Biber J, Murer H, Wagner CA. Renal phosphaturia during metabolic acidosis revisited: Molecular mechanisms for decreased renal phosphate reabsorption. Pflugers Arch 457: 539–549, 2008
- Biber J, Hernando N, Forster I, Murer H. Regulation of phosphate transport in proximal tubules. Pflugers Arch 458: 39–52, 2009
- Magyar CE, Zhang Y, Holstein-Rathlou NH, McDonough AA. Proximal tubule Na transporter responses are the same during acute and chronic hypertension. Am J Physiol Renal Physiol 279: F358–F369, 2000
- A. Y. Tamime, ed. (2006). Brined cheeses – The Society of Dairy Technology (SDT). Wiley-Blackwell. ISBN 978-1-4051-2460-7.
- PHOSPHORIC ACID AND PHOSPHATE SALTS. http://www.inchem.org/documents/jecfa/jecmono/v17je22.htm
- Lauersen, F. (1953) Uber gesundheitliche bedenken bei der Verwendung von Phosphonsaune und primarem Phosphat in Enfrischungsgetranken, Z. Lebensmitt-Untersuch., 96, 418-440
- Thomas, W. C. (1972) Effectiveness and mode of action of orthophosphates in patients with calcareous renal calculi. Trans. Am. Clin. Climatol. Assoc., 83, 113-124
- Malm, O. J. (1953) On phosphates and phosphoric acid as dietary factors in the calcium balance of man, Scand. J. Clin. Lab. Invest., 5, 75-84
- Leichsenring, J. M. et al., (1951) The effect of level of intake on calcium and phosphorus metabolism in college women, J. Nutr., 45, 407-418
- Furia, T.E. (ed.). CRC Handbook of Food Additives. 2nd ed. Cleveland: The Chemical Rubber Co., 1972., p. 641