Anemia of prematurity
Anemia of prematurity means that a baby born early (prematurely) does not have enough red blood cells. Red blood cells carry oxygen to the body. Preterm infants with birth weight <1.0 kg (commonly designated as extremely low birth weight or ELBW, infants) have completed ≤29 weeks of gestation, and nearly all will need red blood cell (RBC) transfusions during the first weeks of life. Every week in the United States, approximately 10,000 infants are born prematurely (ie, <37 weeks of gestation), with 600 (6%) of these preterm infants being extremely low birth weight 1. Approximately 90% of extremely low birth weight neonates will receive at least one red blood cell transfusion 2.
All babies have some anemia (decrease in hemoglobin concentration) when they are born. In healthy term infants, the nadir hemoglobin value rarely falls below 10 g/dL at an age of 10 to 12 weeks 3. This is normal and is called “physiological anemia of infancy”. For the term infant, a physiologic and usually asymptomatic anemia is observed 8-12 weeks after birth. But in premature babies, the number of red blood cells may decrease faster and go lower than in full-term babies. This may happen because:
- A premature baby may not make enough red blood cells.
- A premature baby may need tests that require blood samples. It may be hard for the baby to produce enough red blood cells to make up for the blood that’s taken out and used in the tests.
- A baby’s red blood cells don’t live as long as an older child’s red blood cells.
Anemia of prematurity is an exaggerated, pathologic response of the preterm infant to this transition. Anemia of prematurity is a normocytic, normochromic, hyporegenerative anemia characterized by a low serum erythropoietin (EPO) level, often despite a remarkably reduced hemoglobin concentration 4. Nutritional deficiencies of iron, vitamin E, vitamin B-12, and folate may exaggerate the degree of anemia, as may blood loss and/or a reduced red cell life span.
The anemia of prematurity is caused by untimely birth occurring before placental iron transport and fetal erythropoiesis are complete, by phlebotomy blood losses taken for laboratory testing, by low plasma levels of erythropoietin due to both diminished production and accelerated catabolism, by rapid body growth and need for commensurate increase in red cell volume/mass, and by disorders causing red blood cell losses due to bleeding and/or hemolysis 3.
The risk of anemia of prematurity is inversely related to gestational maturity and birthweight 4. As many as half of infants of less than 32 weeks gestation develop anemia of prematurity. Anemia of prematurity is not typically a significant issue for infants born beyond 32 weeks’ gestation.
Race and sex have no influence on the incidence of anemia of prematurity.
Testosterone is believed to be at least partially responsible for a slightly higher hemoglobin level in male infants at birth, but this effect is of no significance with regard to risk of anemia of prematurity. The nadir of the hemoglobin level is typically observed 4-10 weeks after birth in the tiniest infants, with hemoglobin levels of 8-10 g/dL if birthweight was 1200-1400 grams, or 6-9 g/dL at birth weights of less than 1200 grams and to approximately 7 g/dL in infants with birth weights <1 kg 4.
Anemia of prematurity is usually not serious. Anemia of prematurity spontaneously resolves in many premature infants within 3-6 months of birth 4. In others, however, medical intervention is required, because the low oxygen levels in a premature infant can make other problems worse, such as heart and lung problems. Most infants with birth weight <1.0 kg are given multiple red blood cell (RBC) transfusions within the first few weeks of life 3.
Red blood cell transfusions are the mainstay of therapy for anemia of prematurity with recombinant human erythropoietin (EPO) largely unused because it fails to substantially diminish red blood cell transfusion needs despite exerting substantial erythropoietic effects on neonatal marrow.
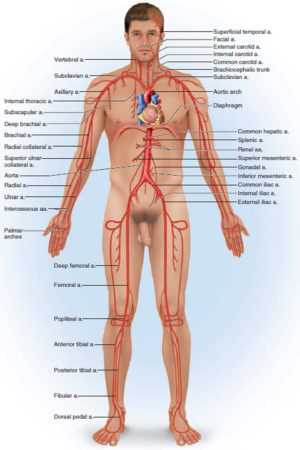
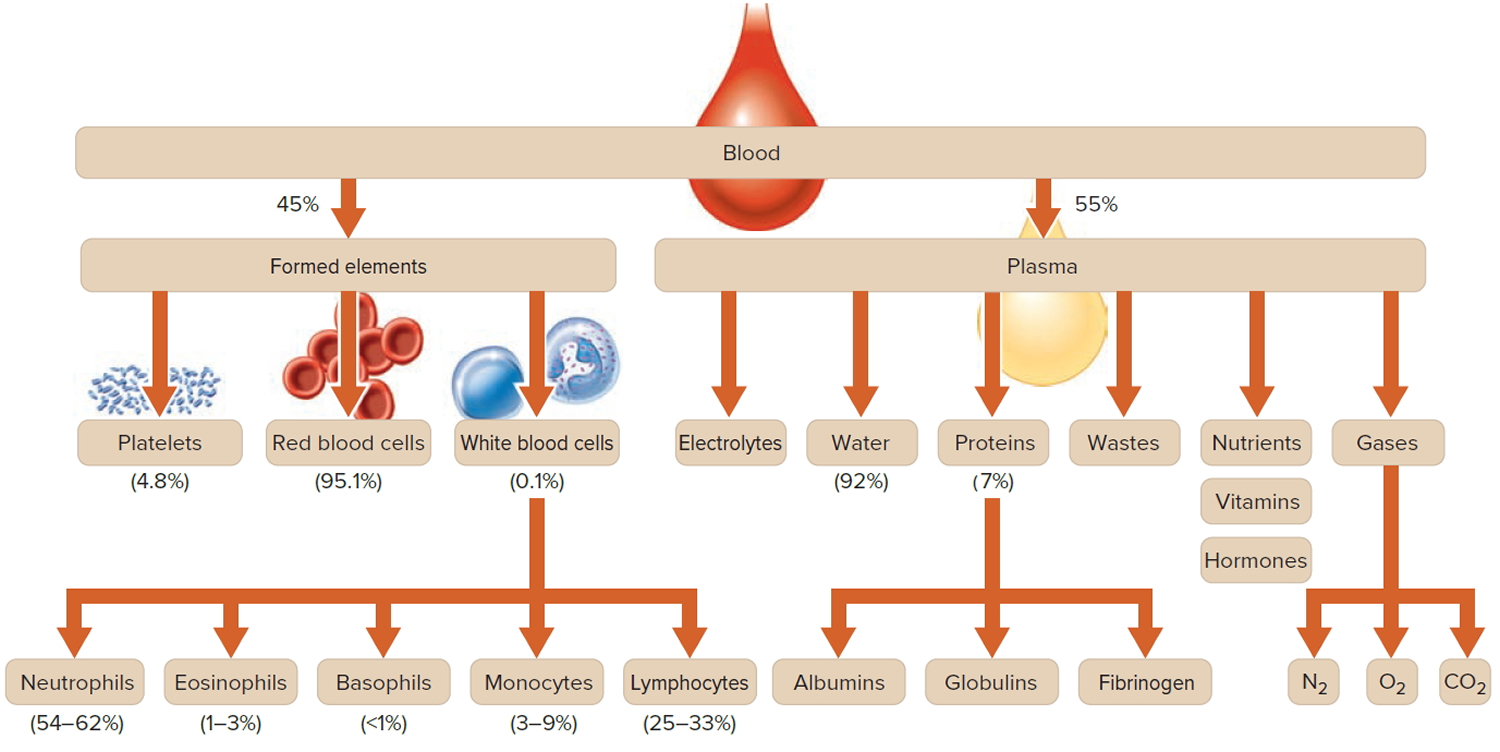
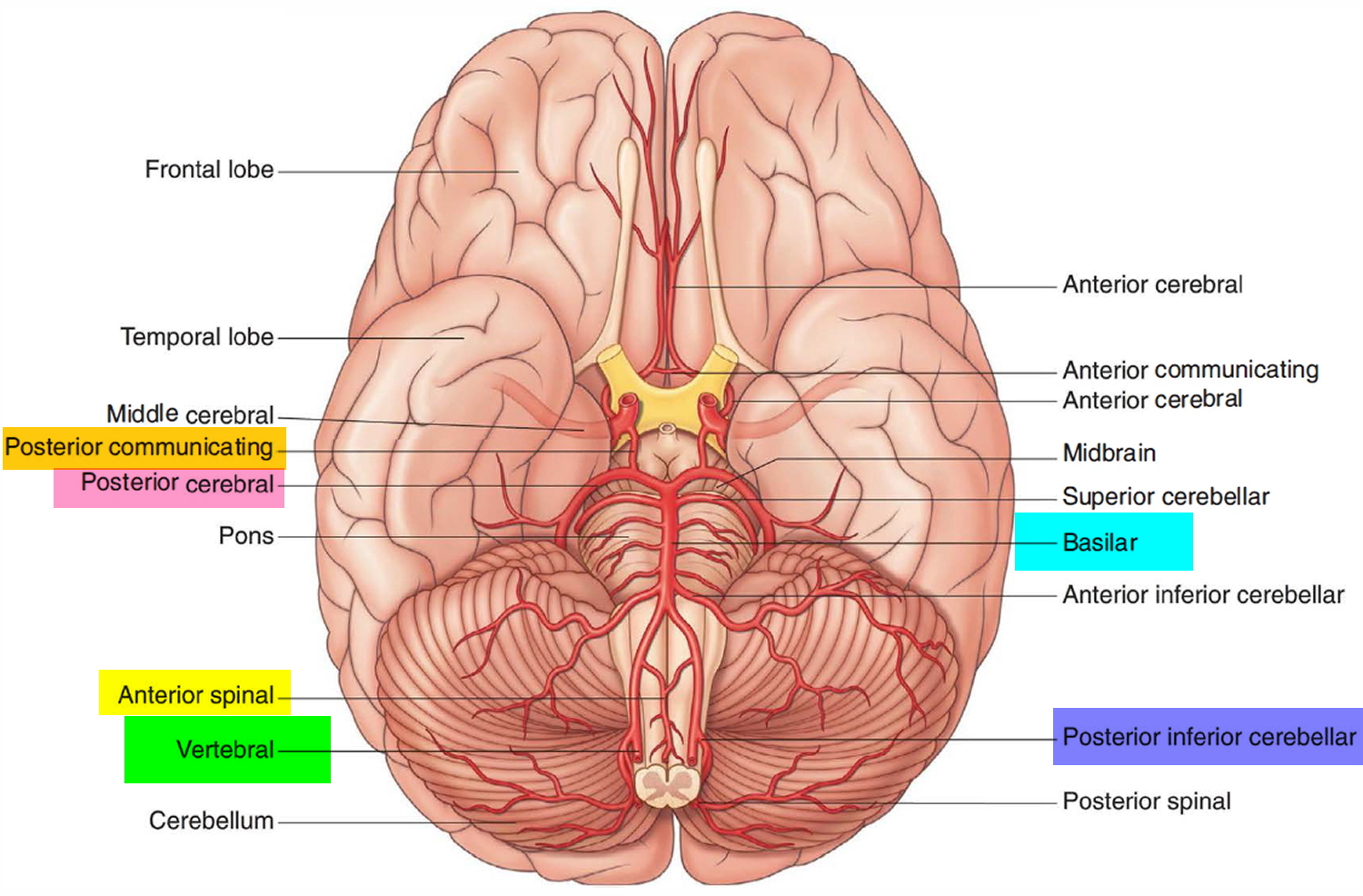
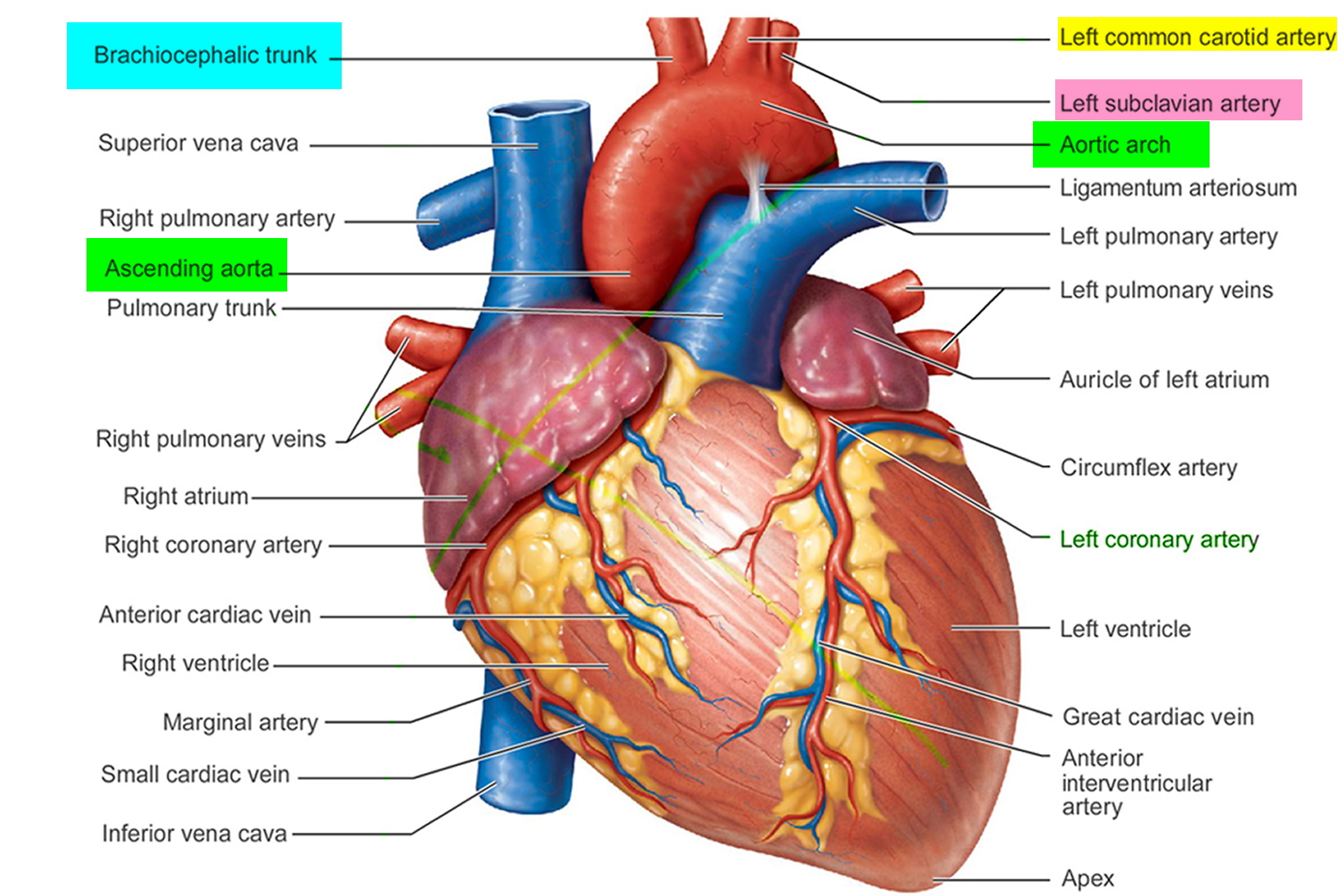
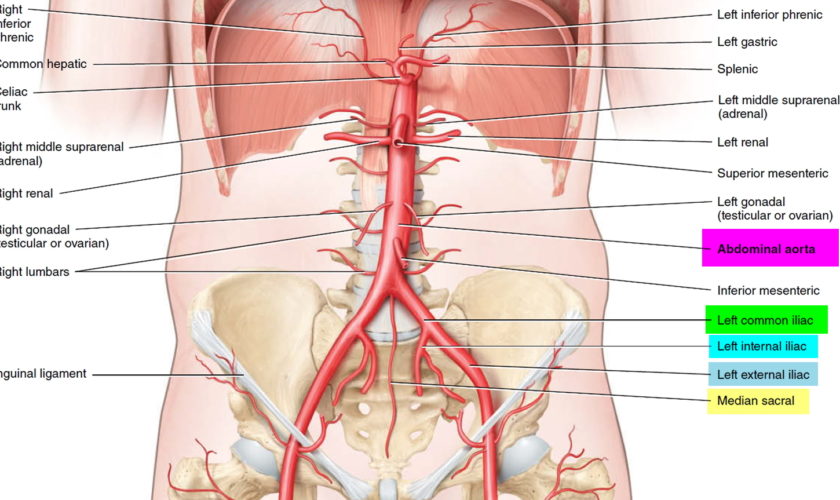
Figure 1. Blood composition
Footnote: Blood consists of a liquid portion called plasma and a solid portion (the formed elements) that includes red blood cells, white blood cells, and platelets. When blood components are separated by centrifugation, the white blood cells and platelets form a thin layer, called the “buffy coat,” between the plasma and the red blood cells, which accounts for about 1% of the total blood volume. Blood cells and platelets can be seen under a light microscope when a blood sample is smeared onto a glass slide.
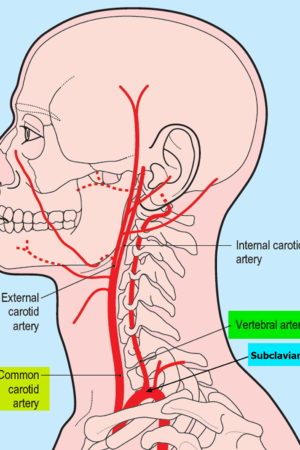
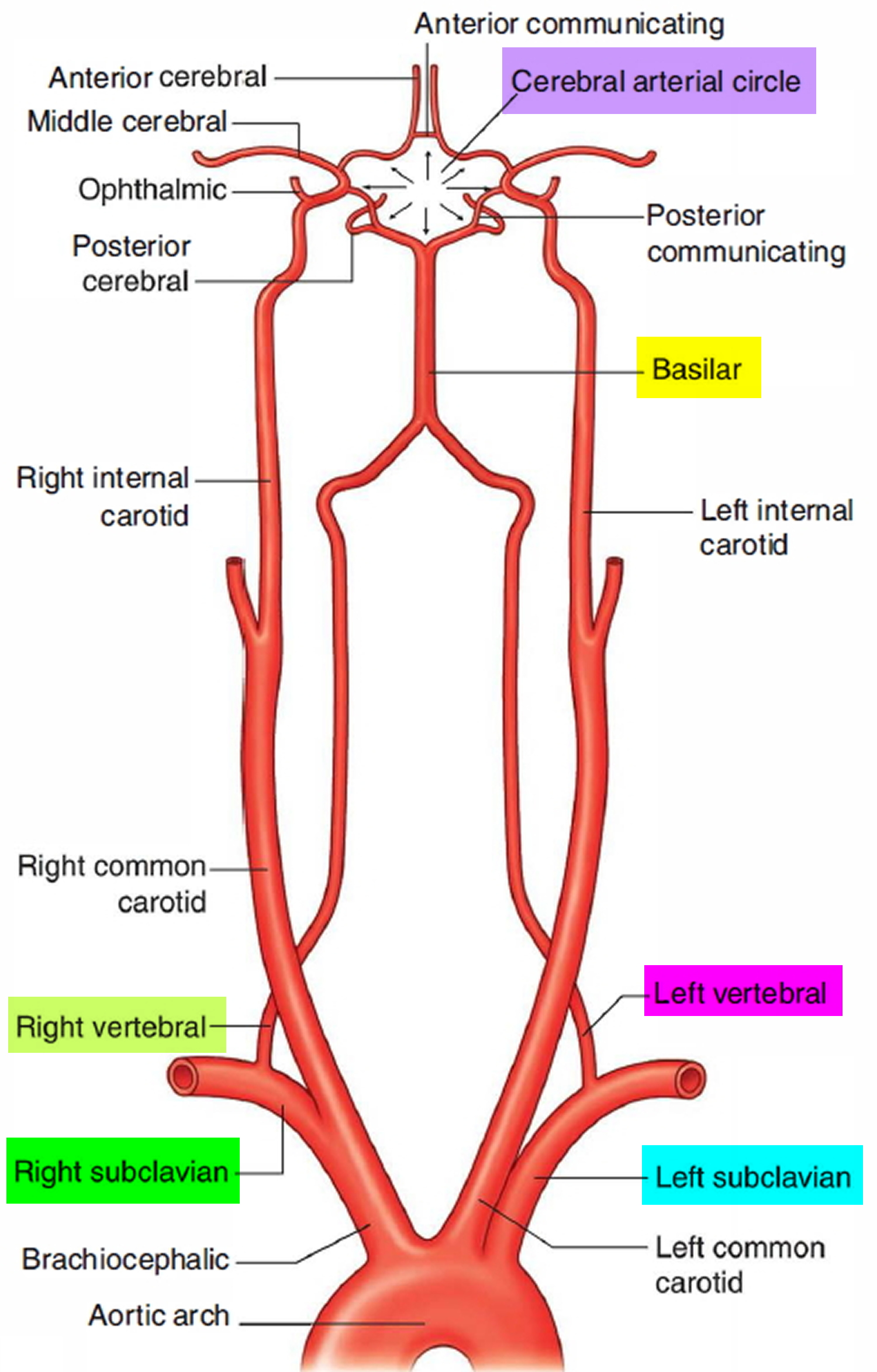
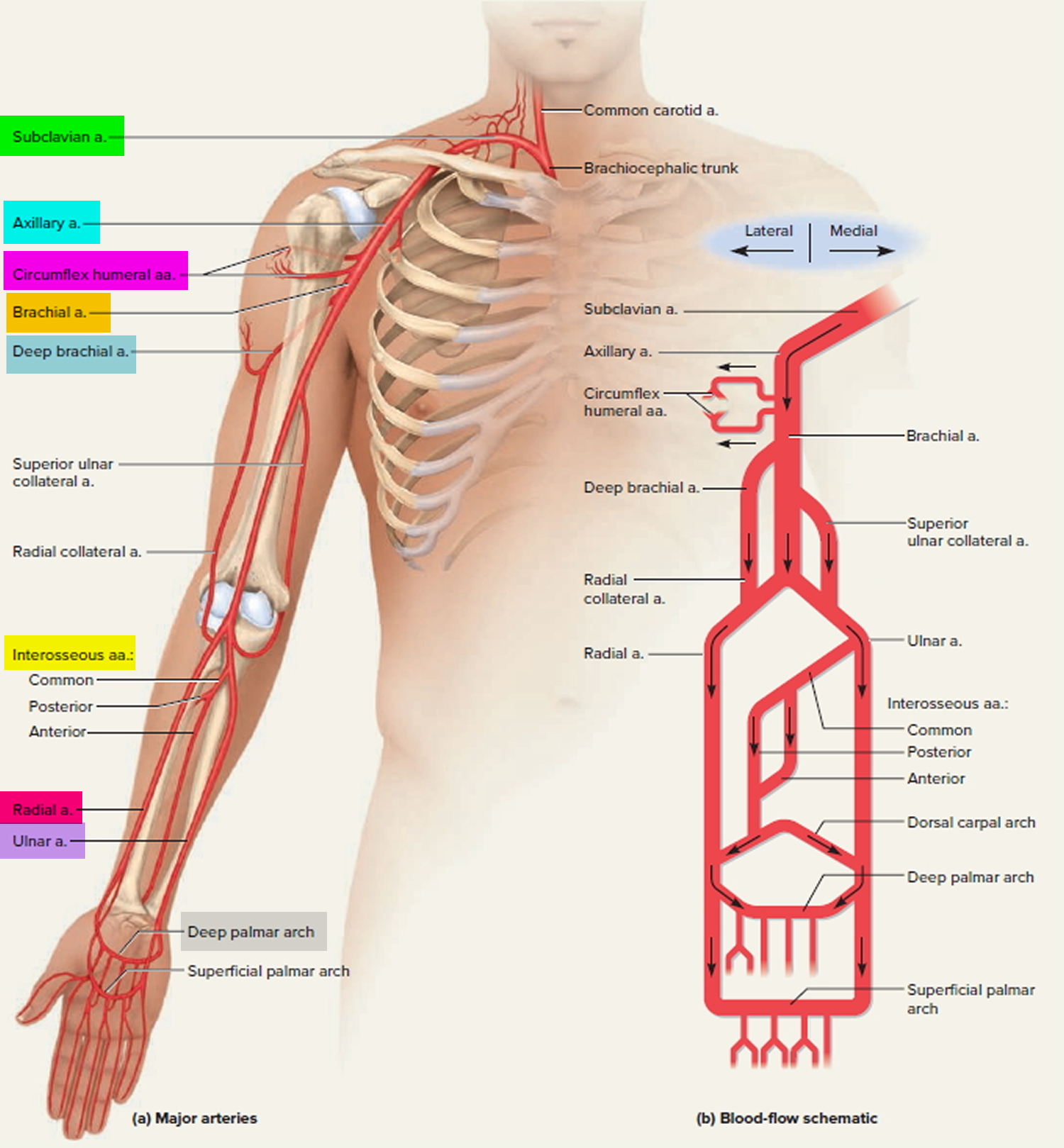
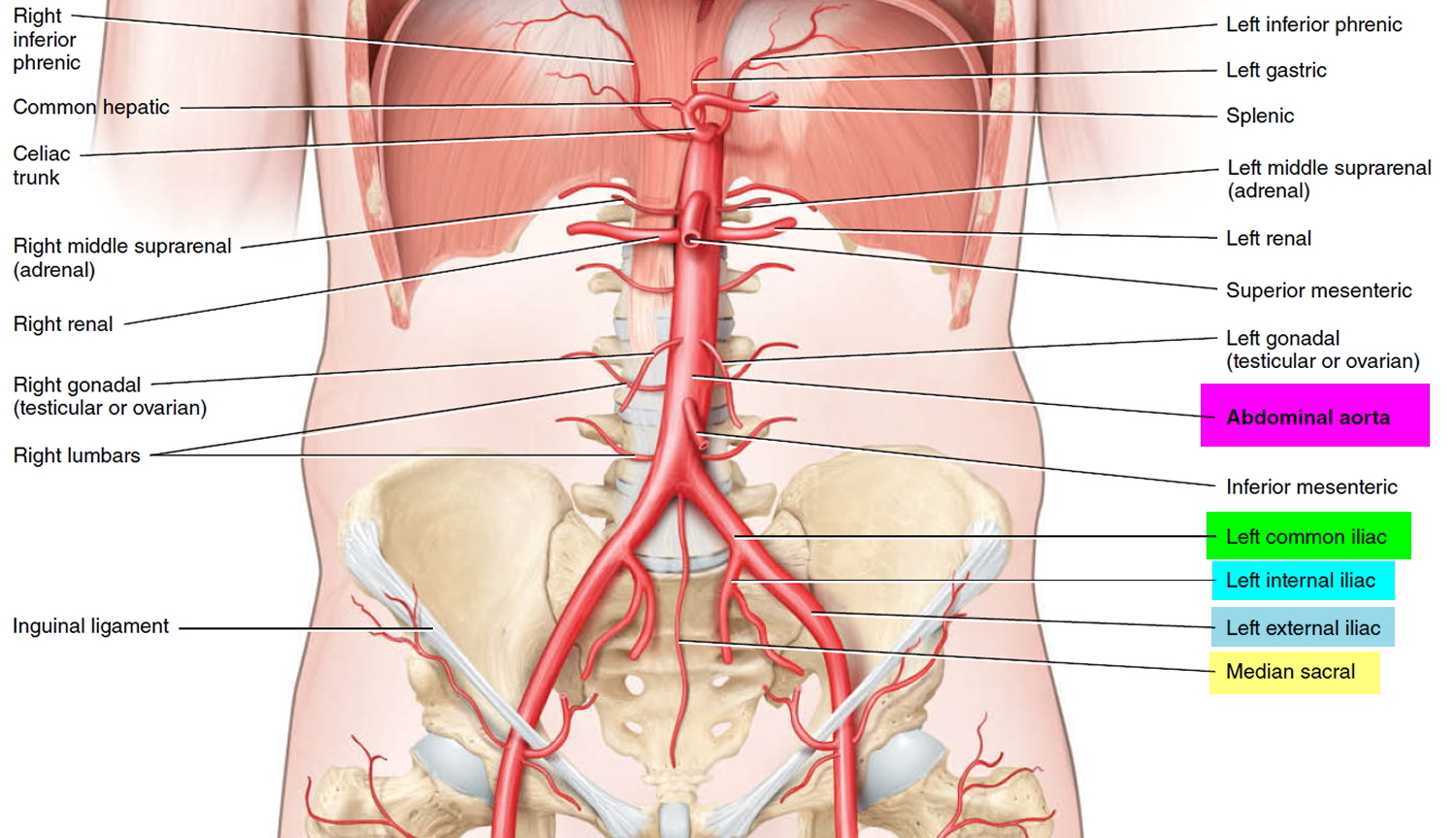
Figure 2. Red blood cells (normal red blood cells)
Anemia of prematurity causes
The three basic mechanisms for the development of anemia of prematurity include:
- Inadequate red blood cell production,
- Shortened red blood cell life span,
- Blood loss.
Taken together, the premature infant is at risk for the development of anemia of prematurity because of limited red blood cell synthesis during rapid growth, a diminished red blood cell life span, and an increased loss of red blood cells.
Inadequate red blood cell production
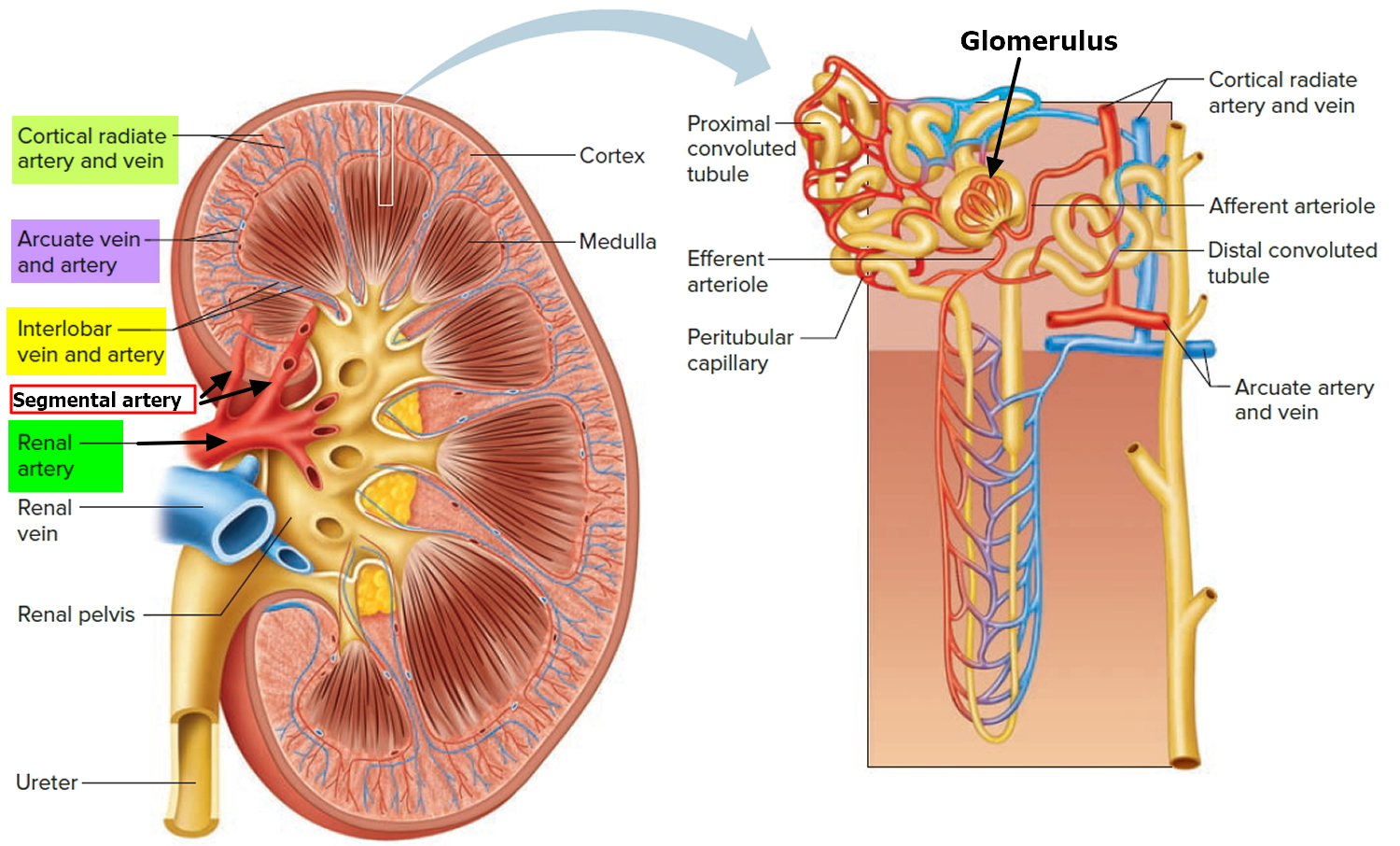
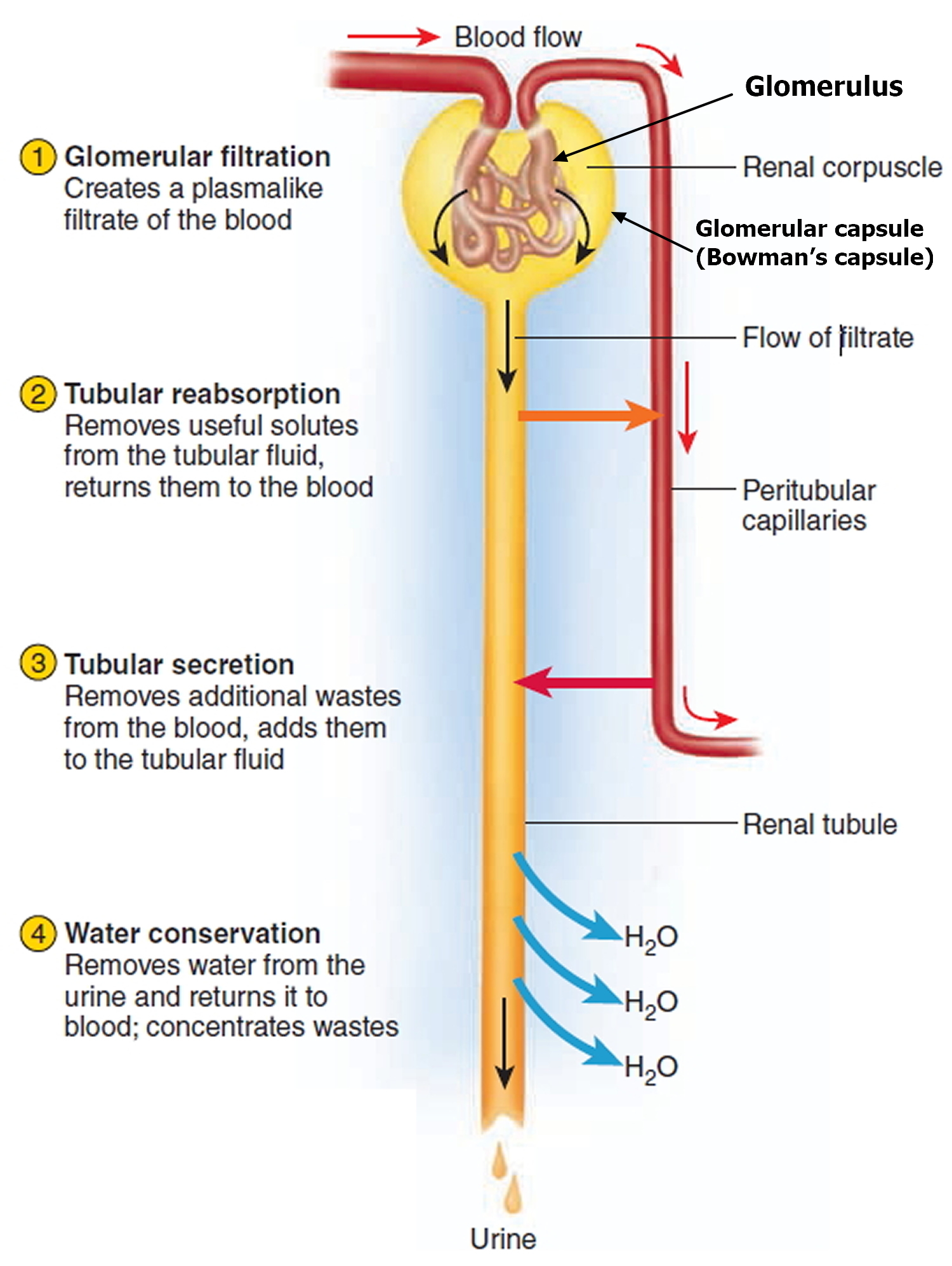
The first mechanism of anemia is inadequate red blood cell production for the growing premature infant. The location of erythropoietin (EPO) and red blood cell production changes during gestation. Erythropoietin (EPO) synthesis initially occurs in the fetal liver but gradually shifts toward the kidney as gestation advances. By the end of gestation, however, the liver remains the major source of erythropoietin (EPO).
Fetal erythrocytes are produced in the yolk sac during the first few weeks of embryogenesis. The fetal liver becomes more important as gestation advances and, by the end of the first trimester, has become the primary site of erythropoiesis. Bone marrow then begins to take on a more active role in producing erythrocytes. By about 32 weeks’ gestation, the burden of erythrocyte production in the fetus is shared evenly by liver and bone marrow. By 40 weeks’ gestation, the marrow is the sole erythroid organ. Premature delivery does not accelerate the ontogeny of these processes.
Although erythropoietin (EPO) is not the only erythropoietic growth factor in the fetus, it is the most important. Erythropoietin (EPO) is synthesized in response to anemia and consequent relative tissue hypoxia. The degree of anemia and hypoxia required to stimulate erythropoietin (EPO) production is far greater for the fetal liver than for the fetal kidney. Erythropoietin (EPO) production may not be stimulated until a hemoglobin concentration of 6-7 g/dL is reached. As a result, new red blood cell production in the extremely premature infant, whose liver remains the major site of erythropoietin (EPO) production, is blunted despite what may be marked anemia. In addition, erythropoietin (EPO), whether endogenously produced or exogenously administered, has a larger volume of distribution and is more rapidly eliminated by neonates, resulting in a curtailed time for bone marrow stimulation.
Erythroid progenitors in premature infants are quite responsive to erythropoietin (EPO), but the response may be blunted if iron or other substrate or co-factor stores are insufficient. Another potential problem is that while the infant may respond appropriately to increased erythropoietin (EPO) concentrations with increased reticulocyte counts, rapid growth may prevent the appropriate increase in hemoglobin concentration.
Shortened red blood cell life span or hemolysis
Also important in the development of anemia of prematurity is that the average life span of a neonatal red blood cell is only one half to two thirds that of an adult red blood cell. Cells of the most immature infants may survive only 35-50 days. The shortened red blood cell life span of the neonate is a result of multiple factors, including diminished levels of intracellular adenosine triphosphate (ATP), carnitine, and enzyme activity; increased susceptibility to lipid peroxidation; and increased susceptibility of the cell membrane to fragmentation.
Blood loss
Finally, blood loss may contribute to the development of anemia of prematurity. If the neonate is held above the placenta for a time after delivery, fetal-placental transfer of blood may occur. Conversely, delayed cord clamping may lessen the degree of anemia of prematurity 5, although a study by Elimian et al 6 did not find this to be true. More commonly, because of the need to closely monitor the tiny infant, frequent samples of blood are removed for various tests. These losses are often 5-10% of the total blood volume.
Anemia of prematurity differential diagnoses
Conditions to consider in the differential diagnosis of anemia of prematurity are those which diminish red cell production, increase red cell destruction, or cause blood loss.
- Acute Anemia
- Birth Trauma
- Chronic Anemia
- Head Trauma
- Hemolytic Disease of the Newborn
- Parvovirus B19 Infection
- Intraventricular Hemorrhage in the Preterm Infant
Conditions that diminish red blood cell synthesis are as follows:
- Bone marrow infiltration
- Bone marrow depression (eg, pancytopenia, drugs)
- Diamond-Blackfan anemia
- Substrate deficiencies (eg, iron, vitamin E, folic acid)
- Congenital fetal infections (eg, cytomegalovirus, parvovirus, syphilis)
Conditions that cause hemolysis are as follows:
- Congenital fetal infections (eg, cytomegalovirus, parvovirus, syphilis)
- Acute systemic infections (leading to disseminated intravascular coagulation)
- Abnormal red blood cells (spherocytosis, elliptocytosis)
- Nonspherocytic hemolytic anemias (eg, G6PD deficiency, kinase and isomerase deficiencies)
- Hemolytic disease of the newborn (Rh, ABO, other major blood-group incompatibilities between mother and fetus)
Conditions that reduce blood volume are as follows:
- Twin-to-twin transfusion syndrome (donor twin)
- Iatrogenic (eg, excessive blood sampling)
- Hemorrhage (eg, gastrointestinal, central nervous system, subcutaneous tissues)
Anemia of prematurity symptoms
Many clinical findings have been attributed to anemia of prematurity, but they are neither specific nor diagnostic. These symptoms may include the following:
- Poor weight gain despite adequate caloric intake
- Cardiorespiratory symptoms such as tachycardia, tachypnea, and flow murmurs
- Decreased activity, lethargy, and difficulty with oral feeding
- Pallor
- Increase in apneic and bradycardic episodes, and worsened periodic breathing
- Metabolic acidemia – Increased lactic acid secondary to increased cellular anaerobic metabolism in relatively hypoxic tissues
Anemia of prematurity diagnosis
The following are useful laboratory studies:
- Complete blood count (CBC) – White blood cell (WBC) and platelet values are normal in anemia of prematurity. Low hemoglobin values, below 10 g/dL, are found. They may descend to a nadir of 6-7 g/dL. Lowest levels are generally observed in the smallest infants. Red blood cell indices are normal (eg, normochromic, normocytic) for age.
- Reticulocyte count – The reticulocyte count is low when the degree of anemia is considered, as a result of the low levels of erythropoietin (EPO). Conversely, an elevated reticulocyte count is not consistent with the diagnosis of anemia of prematurity.
- Peripheral blood smear – Red blood cell morphology should be normal. Red blood cell precursors may appear to be more prominent.
- Maternal and infant blood typing; direct antibody test (Coombs) – The direct Coombs test result may be coincidentally positive. Despite this, it is important to ensure an immune-mediated hemolytic process related to maternal-fetal blood group incompatibility (hemolytic disease of the newborn) is not present.
- Serum bilirubin – An elevated serum bilirubin level should suggest other possible explanations for the anemia. These would include hemolytic entities, such as G-6-PD deficiency or other kinase/isomerase/enzyme deficiencies, or more common causes such as infection or hemolytic disease of the newborn.
- Lactic acid – Elevated lactic acid levels have been suggested by some to be useful as an aid to determine the need for transfusion.
Anemia of prematurity treatment
Medical treatment options are blood transfusion(s), recombinant erythropoietin (EPO) treatment, and observation.
Observation may be the best course of action for infants who are asymptomatic, not acutely ill, and are receiving adequate nutrition. Adequate amounts of vitamin E, vitamin B-12, folate, and iron are important to blunt the expected decline in hemoglobin levels in the premature infant. Periodic measurements of the hematocrit level in infants with anemia of prematurity are necessary after hospital discharge. Once a steady increase in the hematocrit level has been established, only routine checks are required.
Packed red blood cell transfusions
Packed red blood cell transfusions are the mainstay of therapy for anemia of prematurity. The frequency of blood transfusion varies with gestational age, degree of illness, and, interestingly, the hospital evaluated. Unfortunately, there is considerable disagreement about the indication, timing, and efficacy of packed red blood cell transfusion.
Guidelines for transfusing red blood cells to preterm neonates are controversial, and practices vary greatly 7. This lack of a universal approach stems from limited knowledge of the cellular and molecular biology of erythropoiesis during the perinatal period, an incomplete understanding of infant physiological/adaptive responses to anemia, and contrary/controversial transfusion practice guidelines as based on results of randomized clinical trials and expert opinions. Generally, red blood cell transfusions are given to maintain a level of blood hemoglobin or hematocrit believed to be optimal for each neonate’s clinical condition. Guidelines for red blood cell transfusions, judged to be reasonable by most neonatologists to treat the anaemia of prematurity, are listed by Table 1. These guidelines are very general, and it is important that terms such as “severe” and “symptomatic” be defined to fit local transfusion practices/policies. Importantly, guidelines are not mandates for red blood cell transfusions that must be followed; they simply suggest situations when an red blood cell transfusion would be judged to be reasonable/acceptable.
The decision to give a transfusion should not be made lightly, because significant infectious, hematologic, immunologic, and metabolic complications are possible. Late-onset necrotizing enterocolitis has been reported in stable-growing premature infants electively transfused for anemia of prematurity 8. Transfusions also transiently decrease erythropoiesis and EPO levels. There is also agreement that the number of transfusions, as well as the number of donor exposures, should be reduced as much as possible.
Clinical trials designed to determine the efficacy of blood transfusions in relieving symptoms ascribed to anemia of prematurity have produced conflicting results 9. Improved growth has been an inconsistent finding. While some studies have demonstrated a decrease in apneic episodes after blood transfusion, others have found similar results with simple crystalloid volume expansion.
Subjective improvement in activity, decreased lethargy, and improved feeding have been described in some studies. Blood transfusions have been documented to decrease lactic acid levels in otherwise healthy preterm infants who are anemic. Blood transfusions have reduced tachycardia in anemic infants who are transfused.
Some medical professionals have suggested using lactate levels as an aid in determining the need for transfusion.
Table 1. Allogeneic red blood cell transfusions for the anemia of prematurity
Transfuse to maintain the blood hematocrit per each clinical situation:
- > 40% (35 to 45% *) for severe cardiopulmonary disease
- > 30% for moderate cardiopulmonary disease
- > 30% for major surgery
- >25% (20 to 25% *) for symptomatic anemia
- > 20% for asymptomatic anemia
*Reflects practices that vary among neonatologists. Thus, any value within range is acceptable for local practices.
Reducing the number of transfusions
Studies from individual centers have documented a marked decrease in the administration of packed red blood cell transfusions in the past decades, even before the use of EPO became more frequent. This decrease in transfusions is almost certainly multifactorial in origin. Adoption of standardized transfusion protocols that take various factors into account, including hemoglobin levels, degree of cardiorespiratory disease, and traditional signs and symptoms of pathologic anemia, are acknowledged as an important factor in this reduction. A restricted transfusion protocol may decrease the number of transfusions while also decreasing the hematocrit at discharge 10.
A 2011 study 11 evaluated 41 preterm infants with birth weights of 500-1300 g who were enrolled in a clinical trial that compared high and low hematocrit thresholds for transfusion. A rise in systemic oxygen transport and a decrease in lactic acid after transfusion was noted in both groups; however, oxygen consumption did not change significantly in either group. In the low hematocrit group only, cardiac output and fractional oxygen extraction fell after transfusion, which shows that these infants had increased their cardiac output to maintain adequate tissue oxygen delivery in response to anemia. The results demonstrate that infants with low hematocrit thresholds may benefit from transfusion, while transfusion in those with high hematocrit thresholds may provide no acute physiological benefit 11.
The Premature Infant in Need of Transfusion study 12 showed that transfusing infants to maintain higher hemoglobin level (8.5-13.5 g/dL) conferred no benefit in terms of mortality, severe morbidity, or apnea intervention compared with infants transfused to maintain a low hemoglobin levels (7.5-11.5 g/dL).
These findings differ from the Iowa study, which found less parenchymal brain hemorrhage, periventricular leukomalacia, and apnea in infants whose transfusion criteria was not restricted and whose hemoglobin level was higher. Clearly, no universally accepted guidelines for transfusion in infants with anemia of prematurity are available at this time, and clinicians must determine their individual standardized transfusion practices.
Anemia of prematurity guidelines
No universally accepted guidelines for transfusion in infants with anemia of prematurity are available at this time, and clinicians must determine their individual standardized transfusion practices.
As an example, note the Children’s Hospital of Wisconsin Transfusion Committee guidelines for consideration:
- An infant with a hemoglobin (Hb) level of less than 8 g/dL may be transfused at the discretion of the attending physician
- A stable infant with a hemoglobin level of 8-10 g/dL without clinical symptoms or other exceptions listed below may be transfused
- An infant with a hemoglobin level of 11-13 g/dL without a supplemental oxygen or continuous positive airway pressure (CPAP) requirement, apnea/bradycardia, significant tachycardia or tachypnea, or other exceptions listed below should not be transfused
- An infant with a hemoglobin level of more than 13 g/dL without an oxygen requirement of more than 40% by hood, CPAP, or ventilator; hypotension that requires pressor medication; major surgery; or other exceptions listed below should not be transfused
- An infant with a hemoglobin level of more than 15 g/dL without cyanotic heart disease, extracorporeal membrane oxygenation (ECMO) therapy, regional oxygen saturations less than 50%, or hypotension that requires pressor medications should not be transfused
- An infant with a history of massive blood loss may be transfused at the discretion of the attending physician
It is of obvious importance to discuss with the family their child’s need for transfusion and to obtain consent before the transfusion. It is also important to discuss with parents the normal course of anemia, the criteria for and risks associated with transfusions, and the advantages and disadvantages of erythropoietin (EPO) administration. Also necessary is consideration of the family’s religious beliefs regarding transfusions.
Reducing the number of donor exposures
Reducing the number of donor exposures is also important. Preservatives and additive systems allow blood to be stored safely for as long as 35-42 days. This can be accomplished by using packed red blood cells stored in preservatives (eg, citrate-phosphate-dextrose-adenine [CPDA-1]) and additive systems (eg, Adsol). Infants may be assigned a specific unit of blood, which may suffice for treatment during their entire hospitalization and thus limit exposure to the single donor of that unit. Concerns that stored blood might increase serum potassium levels are unfounded if the transfused volume is low.
Complications
Potential complications of transfusion include the following:
- Infection (eg, hepatitis, cytomegalovirus [CMV], human immunodeficiency virus [HIV], syphilis)
- Fluid overload and electrolyte imbalances
- Exposure to plasticizers
- Hemolysis
- Posttransfusion graft versus host disease
An important tool in reducing at least one of these transfusion risks is to use all available screening techniques for infection. The risk of cytomegalovirus (CMV) transmission can be dramatically reduced by use of CMV-safe blood. This can be accomplished by using CMV serology–negative cells, along with blood processed through leukocyte-reduction filters or inverted spin technique. These methods also reduce other WBC-associated infectious agents (eg, Epstein-Barr virus, retroviruses, Yersinia enterocolitica) by yielding a leukocyte-poor suspension of packed red blood cells. The American Red Cross now provides exclusively leukocyte-reduced blood to hospitals in the United States.
Recombinant Erythropoietin treatment
Multiple investigations have established that premature infants respond to exogenously administered recombinant human EPO and supplemental iron with a brisk reticulocytosis. Subcutaneous administration of EPO may be preferred, as intravenous administration has increased urinary losses. Although EPO cannot prevent early transfusions, modest decreases in the frequency of late packed red blood cell transfusions have been documented. Additional iron supplementation is necessary during exogenous EPO treatment.
Trials have evaluated the impact of EPO treatment in populations of the most immature neonates. These studies likewise have demonstrated that infants with very low birth weight (VLBW) are capable of responding to EPO with a reticulocytosis.
Studies and a Cochrane Neonatal Systemic review suggest an association between exogenous EPO administration and retinopathy of prematurity 13.
Yasmeen et al 14 studied 60 preterm low birth weight infants and concluded that short-term recombinant human erythropoietin with iron and folic acid was effective in preventing anemia of prematurity.
EPO with iron does not adversely affect growth or developmental outcomes, but the impact on the number of transfusions a premature infant receives ranges from nonexistent to small.
At this time, no agreement regarding the safety, timing, dosing, route, or duration of therapy has been established. In short, the cost-benefit ratio for EPO has yet to be clearly established, and this medication is not universally accepted as a standard therapy for an infant with anemia of prematurity.
Anemia of prematurity prognosis
Spontaneous recovery of mild anemia of prematurity may occur 3-6 months after birth. In more severe, symptomatic cases, medical intervention may be required.
- Martin JA, Hamilton BE, Sutton PD, et al. Births: final data for 2008 national Vital Statistics Reports. Centers for Disease Control and Prevention. 2009;57:7.[↩]
- Maier RJ, Sonntag J, Walka MM, et al. Changing practices of red blood cell transfusions in infants with birth weights less than 1000 g. J Pediatr. 2000;136:220–224.[↩]
- Strauss RG. Anaemia of prematurity: pathophysiology and treatment. Blood Rev. 2010;24(6):221-225. doi:10.1016/j.blre.2010.08.001 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2981681[↩][↩][↩]
- Anemia of Prematurity. https://emedicine.medscape.com/article/978238-overview[↩][↩][↩][↩]
- Ultee CA, van der Deure J, Swart J, Lasham C, van Baar AL. Delayed cord clamping in preterm infants delivered at 34 36 weeks’ gestation: a randomised controlled trial. Arch Dis Child Fetal Neonatal Ed. 2008 Jan. 93(1):F20-3.[↩]
- Elimian A, Goodman J, Escobedo M, Nightingale L, Knudtson E, Williams M. Immediate compared with delayed cord clamping in the preterm neonate: a randomized controlled trial. Obstet Gynecol. 2014 Dec. 124 (6):1075-9.[↩]
- dos Santos AMN, Guinsburg R, Procianoy RS, dos SR, Sadeck L, Netto AA, Rugolo LM, et al. Variability on red blood cell transfusion practices among Brazilian neonatal intensive care units. Transfusion. 2010;50:150–159.[↩]
- Singh R, Shah BL, Frantz ID 3rd. Necrotizing enterocolitis and the role of anemia of prematurity. Semin Perinatol. 2012 Aug. 36(4):277-82.[↩]
- Bell EF, Nahmias C, Sinclair JC, Zipursky A. Changes in circulating red cell volume during the first 6 weeks of life in very-low-birth-weight infants. Pediatr Res. 2014 Jan. 75 (1-1):81-4.[↩]
- Bell EF, Strauss RG, Widness JA, et al. Randomized trial of liberal versus restrictive guidelines for red blood cell transfusion in preterm infants. Pediatrics. 2005 Jun. 115(6):1685-91.[↩]
- Fredrickson LK, Bell EF, Cress GA, et al. Acute physiological effects of packed red blood cell transfusion in preterm infants with different degrees of anaemia. Arch Dis Child Fetal Neonatal Ed. 2011 Jul. 96(4):F249-53.[↩][↩]
- Kirpalani H, Whyte RK, Andersen C, et al. The Premature Infants in Need of Transfusion (PINT) study: a randomized, controlled trial of a restrictive (low) versus liberal (high) transfusion threshold for extremely low birth weight infants. J Pediatr. 2006 Sep. 149(3):301-307.[↩]
- Suk KK, Dunbar JA, Liu A, et al. Human recombinant erythropoietin and the incidence of retinopathy of prematurity: a multiple regression model. J AAPOS. 2008 Jun. 12(3):233-8.[↩]
- Yasmeen BH, Chowdhury MA, Hoque MM, Hossain MM, Jahan R, Akhtar S. Effect of short-term recombinant human erythropoietin therapy in the prevention of anemia of prematurity in very low birth weight neonates. Bangladesh Med Res Counc Bull. 2012 Dec. 38(3):119-23.[↩]