What is the stomach
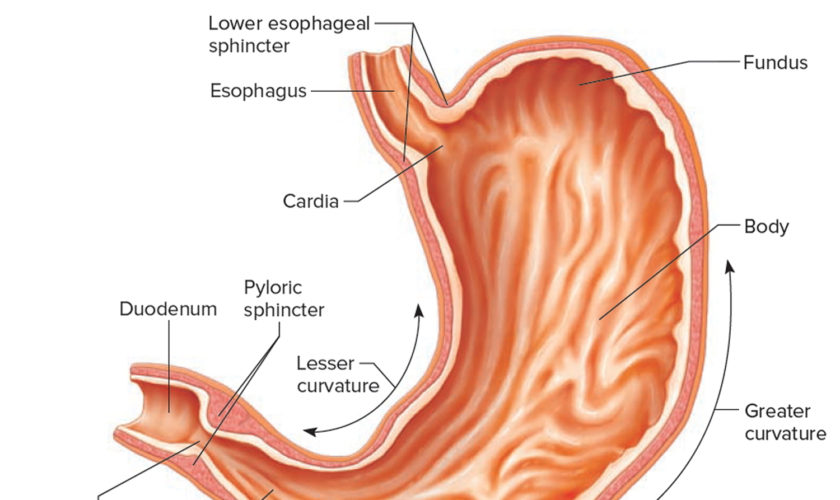
The stomach is a muscular J-shaped pouchlike hollow organ that hangs inferior to the diaphragm in the upper left portion of the abdominal cavity and has a capacity of about 1 liter or more (Figure 1) 1. The stomach’s shape and size vary from person to person, depending on things like people’s sex and build, but also on how much they eat.
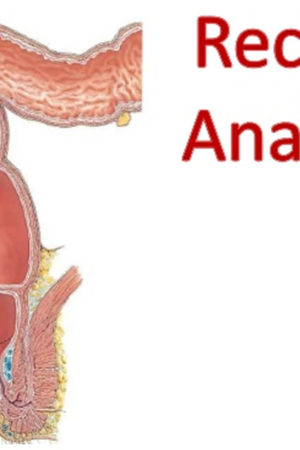
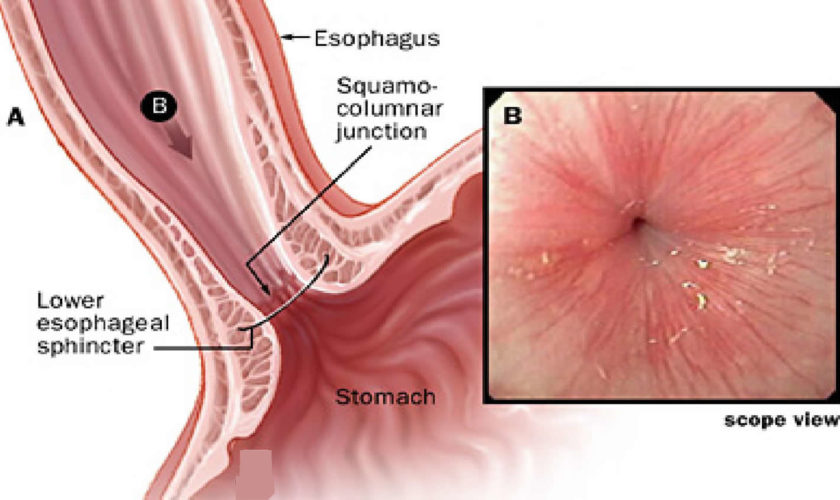
At the point where the esophagus leads into the stomach, the digestive tube is usually kept shut by muscles of the esophagus and diaphragm. When you swallow, these muscles relax and the lower end of the esophagus opens, allowing food to enter the stomach. If this mechanism does not work properly, acidic gastric juice might get into the esophagus, leading to heartburn or an inflammation (see Figure 2).
Thick folds (rugae) of mucosal and submucosal layers mark the stomach’s inner lining and disappear when the stomach wall is distended. The stomach receives food from the esophagus, mixes the food with gastric juice, initiates protein digestion, carries on limited absorption, and moves food into the small intestine.
Figure 1. Stomach
Figure 2. Gastroesophageal junction
Parts of the Stomach
The stomach has 5 parts (Figure 3):
The cardia is a small area near the esophageal opening.
The fundus, which balloons superior to the cardia, is a temporary storage area. It is usually filled with air that enters the stomach when you swallow.
The dilated body region, called the body (corpus), which is the main part of the stomach, lies between the fundus and pylorus. In the body of the stomach food is churned and broken into smaller pieces, mixed with acidic gastric juice and enzymes, and pre-digested.
The antrum – the lower portion (near the intestine), where the food is mixed with gastric juice
The pylorus is the distal portion and the last part of the stomach where it approaches the small intestine. The pyloric canal is a narrowing of the pylorus as it approaches the small intestine. At the end of the pyloric canal the muscular wall thickens, forming a powerful circular muscle, the pyloric sphincter. This muscle is a valve that controls gastric emptying.
The first 3 parts of the stomach (cardia, fundus, and body) are sometimes called the proximal stomach. Some cells in these parts of the stomach make acid and pepsin (a digestive enzyme), the parts of the gastric juice that help digest food. They also make a protein called intrinsic factor, which the body needs to absorb vitamin B12.
The lower 2 parts (antrum and pylorus) are called the distal stomach. The stomach has 2 curves, which form its inner and outer borders. They are called the lesser curvature and greater curvature, respectively.
Figure 3. Parts of the stomach
The stomach wall has 5 layers:
The stomach wall is made up of several layers of mucous membrane, connective tissue with blood vessels and nerves, and muscle fibers (see Figure 5).
- The innermost layer is the mucosa. This is where stomach acid and digestive enzymes are made. Most stomach cancers start in this layer.
- Next is a supporting layer called the submucosa.
- Outside of this is the muscularis propria, a thick layer of muscle that moves and mixes the stomach contents.
- The outer 2 layers, the subserosa and the outermost serosa, wrap the stomach.
The layers are important in determining the stage (extent) of the cancer and in helping to determine a person’s prognosis (outlook). As a cancer grows from the mucosa into deeper layers, the stage becomes more advanced and the prognosis is not as good.
The muscle layer alone has three different sub-layers. The muscles move the contents of the stomach around so vigorously that solid parts of the food are crushed and ground, and mixed into a smooth food pulp.
The inner mucous membrane (lining) has large folds that are visible to the naked eye. These folds run toward the exit of the stomach, providing “pathways” along which liquids can quickly flow through the stomach. If you look at the mucous membrane under a microscope, you can see lots of tiny glands. There are three different types of glands. These glands make digestive enzymes, hydrochloric acid, mucus and bicarbonate.
Gastric juice is made up of digestive enzymes, hydrochloric acid and other substances that are important for absorbing nutrients – about 3 to 4 liters of gastric juice are produced per day. The hydrochloric acid in the gastric juice breaks down the food and the digestive enzymes split up the proteins. The acidic gastric juice also kills bacteria. The mucus covers the stomach wall with a protective coating. Together with the bicarbonate, this ensures that the stomach wall itself is not damaged by the hydrochloric acid.
Figure 4. Stomach anatomy

Figure 5. Layers of the stomach
Stomach function
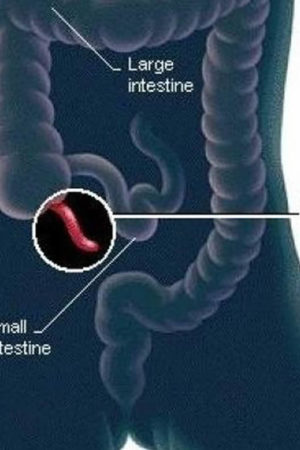
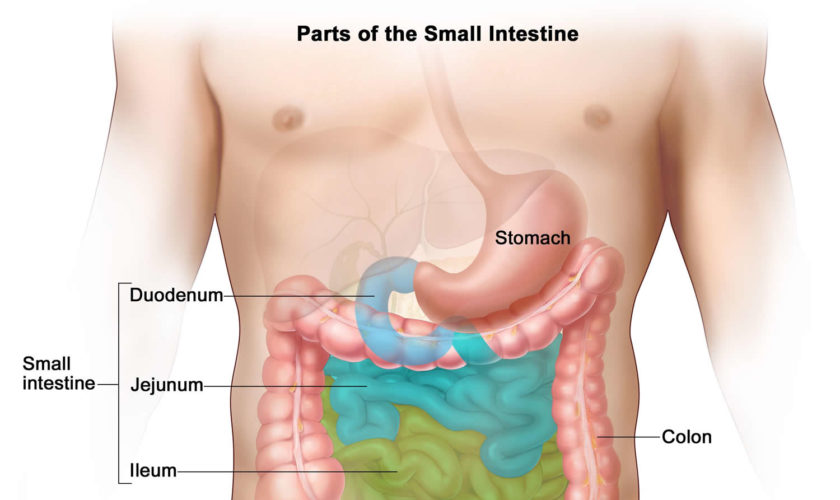
The stomach takes in food from the esophagus (gullet or food pipe), mixes it, breaks it down, and then passes it on to the small intestine in small portions. Following a meal, the mixing movements of the stomach wall aid in producing a semifluid paste of food particles and gastric juice called chyme. Peristaltic waves push the chyme toward the pylorus of the stomach. As chyme accumulates near the pyloric sphincter, the sphincter begins to relax. Stomach contractions push chyme a little at a time into the small intestine.
The rate at which the stomach empties depends on the fluidity of the chyme and the type of food present. Liquids usually pass through the stomach rapidly, but solids remain until they are well mixed with gastric juice. Fatty foods may remain in the stomach from three to six hours; foods high in proteins move through more quickly; carbohydrates usually pass through faster than either fats or proteins.
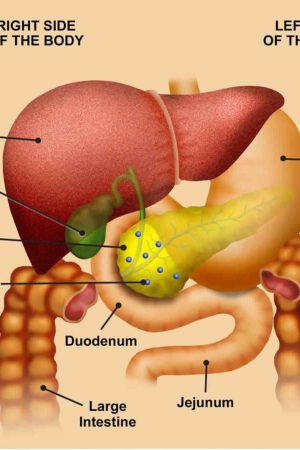
As chyme enters the duodenum (the proximal portion of the small intestine), accessory organs—the pancreas, liver, and gallbladder—add their secretions.
Gastric secretions
The mucous membrane that forms the inner lining of the stomach is thick. Its surface is studded with many small openings called gastric pits located at the ends of tubular gastric glands (Figure 6).
Gastric glands generally contain three types of secretory cells. Mucous cells, in the necks of the glands near the openings of the gastric pits, secrete mucus. Chief cells and parietal cells are in the deeper parts of the glands. The chief cells secrete digestive enzymes, and the parietal cells release a solution containing hydrochloric acid. The products of the mucous cells, chief cells, and parietal cells together form gastric juice.
Pepsin is by far the most important digestive enzyme in gastric juice. The chief cells secrete pepsin in the form of an inactive enzyme precursor called pepsinogen. When pepsinogen contacts hydrochloric acid from the parietal cells, it breaks down rapidly, forming pepsin. Pepsin begins the digestion of nearly all types of dietary protein into polypeptides. This enzyme is most active in an acidic environment, which is provided by the hydrochloric acid in gastric juice.
The mucous cells of the gastric glands (mucous neck cells) and the mucous cells associated with the stomach’s inner surface release a viscous, alkaline secretion that coats the inside of the stomach wall. This coating normally prevents the stomach from digesting itself.
Another component of gastric juice is intrinsic factor, which the parietal cells secrete. Intrinsic factor is necessary for the absorption of vitamin B12 in the small intestine. Table 1 summarizes the major components of gastric juice.
Figure 6. Stomach cells (gastric glands)
Note: Lining of the stomach. Gastric glands include mucous cells, parietal cells, and chief cells. The mucosa of the stomach is studded with gastric pits that are the openings of the gastric glands.
Table 1. Major Components of Gastric Juice
Component | Source | Function |
Pepsinogen | Chief cells of the gastric glands | Inactive form of pepsin |
Pepsin | Formed from pepsinogen in the presence of hydrochloric acid | A protein-splitting enzyme that digests nearly all types of dietary protein into polypeptides |
Hydrochloric acid | Parietal cells of the gastric glands | Provides the acid environment needed for the production and action of pepsin |
Mucus | Mucous cells | Provides a viscous, alkaline protective layer on the stomach’s inner surface |
Intrinsic factor | Parietal cells of the gastric glands | Necessary for vitamin B12 absorption in the small intestine |
Regulation of Gastric Secretions
Gastric juice is produced continuously, but the rate varies considerably and is controlled both neurally and hormonally. When a person tastes, smells, or even sees appetizing food, or when food enters the stomach, parasympathetic impulses on the vagus nerves stimulate the release of the neurotransmitter acetylcholine (Ach). This acetylcholine (Ach) stimulates gastric glands to secrete abundant gastric juice, which is rich in hydrochloric acid and pepsinogen. These parasympathetic impulses also stimulate certain stomach cells to release the peptide hormone gastrin, which increases the secretory activity of gastric glands (Figure 6). Gastrin stimulates cell division in the mucosa of the stomach and intestines, which replaces mucosal cells damaged by normal stomach function, disease, or medical treatments.
As food moves into the small intestine, acid triggers sympathetic impulses that inhibit gastric juice secretion. At the same time, proteins and fats in this region of the intestine cause the intestinal wall to release the peptide hormone cholecystokinin. This hormonal action decreases gastric motility as the small intestine fills with food.
Figure 7. Nerve supply to the stomach
Gastric Absorption
Gastric enzymes begin breaking down proteins, but the stomach wall is not well adapted to absorb digestive products. The stomach absorbs only small volumes of water and certain salts as well as certain lipid-soluble drugs. Alcohol, which is not a nutrient, is absorbed both in the small intestine and in the stomach.
- How does the stomach work ? National Center for Biotechnology Information, U.S. National Library of Medicine. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0072488/[↩]