What are cephalosporins
Cephalosporins are a family of bactericidal antibiotics derived from the the fungus Cephalosporum acremonium (previously called Cephalosporium). Cephalosporins are bactericidal (kill bacteria) and work in a similar way to penicillins. Cephalosporins bind to and block the activity of enzymes responsible for making peptidoglycan, an important component of the bacterial cell wall. Cephalosporins are called broad-spectrum antibiotics because they are effective against a wide range of bacteria.
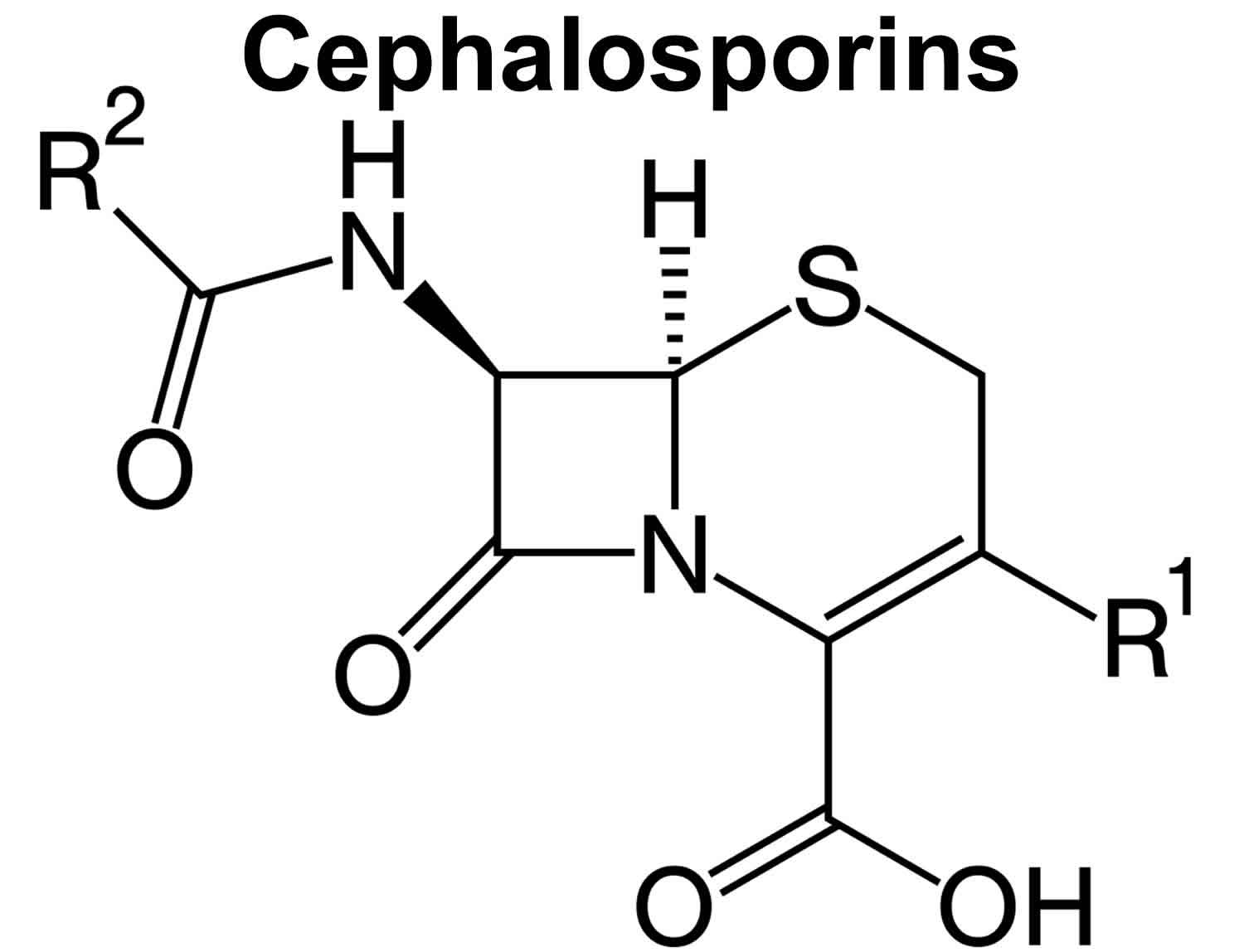
Cephalosporins basic structure is similar to penicillin with a thiazolidine and beta-lactam ring, which has a variable side chain. Cephalosporins bind to the penicillin-binding proteins on bacteria and inhibit synthesis of the bacterial cell wall, causing cell lysis particularly in rapidly growing organisms. Their differences in activity relate to the range of penicillin-binding proteins that they inhibit. Cephalosporins have a broader activity than the standard penicillins, but are also sensitive to some extent to beta-lactamase. Five generations of cephalosporins have been developed with varying antibacterial activity. Cephalosporins are indicated for infections with susceptible organisms. Cephalosporins have variable oral absorption and many must be given parenterally. In the lists below, formulations that are available in oral and parenteral forms are shown separately.
Since the first cephalosporin was discovered in 1945, scientists have been improving the structure of cephalosporins to make them more effective against a wider range of bacteria. Each time the structure changes, a new “generation” of cephalosporins are made. So far there are five generations of cephalosporins. All cephalosporins start with cef, ceph, or kef. Note that this classification system is not used consistently from country to country.
Oral Cephalosporins
The oral cephalosporins are available in both generic and trade formulations and include cefaclor (Ceclor, Raniclor: 2nd), cefadroxil (Duracef: 1st), cefdinir (Omnicef: 3rd), cefditoren (Spectracef: 3rd), cefixime (Suprax: 3rd), cefpodoxime (Vantin: 3rd), cefprozil (Cefzil: 2nd), ceftibuten (Cedax: 3rd), cephalexin (Keftab: Apo-Cephalex, Biocef, Keflex, NovoLexin, Nu-Cephalex: 1st), cefuroxime (Ceftin: 2nd), cephradine (Velosef: 1st), and loracarbef (Lorabid: 2nd). Cefuroxime and cephradine are also available in parenteral forms. The typical dose regimens for oral cephalosporins are 250 to 500 mg two to four times daily for 7 to 14 days. The oral cephalosporins are widely used in medicine for mild-to-moderate infections due to susceptible bacteria.
Oral Cephalosporins
- Cefaclor (2nd)
- Cefadroxil (1st)
- Cefdinir (3rd)
- Cefditoren (3rd)
- Cefixime (3rd)
- Cefpodoxime (3rd)
- Cefprozil (2nd)
- Ceftibuten (1st)
- Cephalexin (1st)
- Cefuroxime (2nd)
- Cephradine (1st)
- Loracarbef (2nd)
Parenteral Cephalosporins
The parenterally administered cephalosporins are widely used as broad spectrum antibiotics for moderate-to-severe infections with susceptible organisms. Despite their widescale use, cases of drug induced liver disease from the cephalosporins are very rare, with only isolated case reports having been published.
Parenterally administered cephalosporins include cefazolin (Ancef: 1st generation), cefepime (Maxipime: 4th), cefoperazone (Cefobid: 3rd), cefotaxime (Claforan: 3rd), cefoxitin (Mefoxin: 2nd), ceftaroline (Teflaro: 5th), ceftazidime (Ceptaz, Fortaz, Tazicef, Tazidime: 3rd), ceftibuten (3rd), ceftizoxime (Cefizox: 3rd), ceftolozane/tazobactam (Zerbaxa: 5th), ceftriaxone (Rocephin: 3rd), cefuroxime (Zinacef: 2nd), and cephradine (1st); the latter two are also available in oral formulations. Most of these cephalosporins can be given either intravenously or intramuscularly and are indicated for therapy of moderate-to-severe bacterial infections caused by susceptible organisms. Typical dose regimens in adults range from 250 mg, 500 mg, 1 gram or 2 grams every 6 to 12 hours for 7 to 14 days. The parenteral cephalosporins are widely used in medicine for serious infections and can be safely given to patients with advanced liver disease, dose modifications being required mainly for renal insufficiency. Many of these agents are also approved for use in children.
Parenteral Cephalosporins
- Cefazolin (1st)
- Cefepime (4th)
- Cefoperazone (3rd)
- Cefotaxime (3rd)
- Cefoxitin (2nd)
- Ceftaroline (5th)
- Ceftazidime (3rd)
- Ceftibuten (3rd)
- Ceftizoxime (3rd)
- Ceftolozane/Tazobactam (5th)
- Cefuroxime (2nd)
- Cephradine (1st)
- Ceftriaxone (3rd)
What are the differences between cephalosporins?
There are currently five “generations” of cephalosporins, with each generation differing slightly in their antibacterial spectrum (ie, how effective they are at killing certain types of bacteria). Within each generation, there are differences in terms of administration (such as oral or intravenous administration), absorption, excretion, and how long the activity of the cephalosporin lasts for in the body.
Cephalosporin generations
First generation cephalosporin
First generation cephalosporins refer to the first group of cephalosporins discovered. Their optimum activity is against gram-positive bacteria such as staphylococci and streptococci. They have little activity against gram-negative bacteria.
First generation cephalosporins include cefadroxil, cefazolin, cephalexin, and cephradine, and these are active against many gram-positive cocci, including penicillinase-producing Staphylococcus aureus.
Cephalexin and cefadroxil can be given by mouth, whereas cefazolin can only be given by injection (IV/IM). There are also differences with regards to how frequently the different first-generation cephalosporins need to be dosed.
First generation cephalosporins may be used to treat infections caused by susceptible bacteria such as:
- Bone infections
- Ear infections (eg, otitis media)
- Skin infections
- Upper respiratory tract infections
- Urinary tract infections.
Table 1. First generation cephalosporins
| Generic name | Brand name examples |
|---|---|
| cefadroxil | Duricef |
| cefazolin | Ancef, Kefzol |
| cephadrine | Discontinued |
| cephalexin | Daxbia, Keflex |
First generation cephalosporins safety
First generation cephalosporins are generally safe, with low toxicity and good efficacy against susceptible bacteria.
Allergic reactions have been reported with cephalosporins (including first generation cephalosporins) and symptoms may include a rash, hives (urticaria), swelling, or rarely, anaphylaxis. Up to 10% of people with a history of penicillin allergy will also be allergic to cephalosporins.
Rarely, seizures have been reported with some cephalosporins; the risk is greatest in those with kidney disease.
Cephalosporins have also been associated with a reduced ability of the blood to clot leading to prolonged bleeding times. People with kidney or liver disease, nutritionally deprived, taking cephalosporins long-term, or concurrently receiving anticoagulant therapy are more at risk.
For a complete list of severe side effects, please refer to the individual drug monographs.
First generation cephalosporins side effects
First generation cephalosporins generally cause few side effects. The most common side effects reported include diarrhea, nausea and vomiting, dyspepsia, gastritis and abdominal pain. Transient liver problems have also been reported.
Rarely, some people may develop a super-infection due to overgrowth of a naturally occurring bacterium called Clostridium difficile, following use of any antibiotic, including cephalosporins. Symptoms may include severe diarrhea.
Uncommonly, an overgrowth of the yeast, Candida albicans, may occur following cephalosporin use, resulting in the symptoms of thrush.
For a complete list of side effects, please refer to the individual drug monographs.
Second generation cephalosporins
Second-generation cephalosporins are more active against gram-negative bacteria, with less activity against gram-positive bacteria.
Second generation cephalosporins include cefaclor, cefoxitin, cefprozil, cefonicid, and cefuroxime; these have broader antibacterial activity, and additional sensitive organisms including Citrobacter, Enterobacter, Haemophilus influenzae, Neisseria and Serratia species.
Second generation cephalosporins have activity against gram-negative aerobes such as Morganella morganii, Neisseria gonorrhoeae (non-penicillinase producing strains), Haemophilus influenzae, Klebsiella species, and Escherichia coli; gram-positive aerobes such as Streptococcus pneumoniae, Staphylococcus aureus, S. epidermidis and S. pyrogenes; and several types of anaerobes.
Some bacteria, such as most strains of Pseudomonas aeruginosa and Acinetobacter species, are resistant to second generation cephalosporins.
Second-generation cephalosporins are more active against gram-negative bacteria than first generation cephalosporins.
Second generation cephalosporins may be used to treat the following types of infections when caused by susceptible strains of bacteria:
- Bone and joint infections
- Gynecological infections
- Intra-abdominal infections
- Lower respiratory tract infections
- Skin and skin structure infections
- Urinary tract infections
Cephalosporins are not usually used as a first-choice antibiotic. They tend to be reserved for use when other antibiotics (often penicillins) cannot be used.
Table 2. Second generation cephalosporins
| Generic name | Brand name examples |
|---|---|
| cefotetan | Cefotan |
| cefoxitin | Mefoxin |
| cefprozil | Cefzil |
| cefuroxime | Ceftin, Zinacef |
| loracarbef | Discontinued |
Second generation cephalosporins safety
Second generation cephalosporins are generally safe, with low toxicity and good efficacy against susceptible bacteria.
Allergic reactions have been reported with all cephalosporins including second generation cephalosporins and symptoms may include a rash, hives (urticaria), swelling, or rarely, anaphylaxis. Up to 10% of people with a history of penicillin allergy will also be allergic to cephalosporins.
Drug-induced hemolytic anemia has been associated with the use of some cephalosporins, including second generation cephalosporins; suspect and investigate further if anemia develops during or after treatment.
Rarely, some people may develop a super-infection due to overgrowth of a naturally occurring bacterium called Clostridium difficile, following use of any antibiotic, including cephalosporins. Symptoms may include severe diarrhea.
Rarely, seizures have been reported with cephalosporins; the risk may be greatest in those with kidney disease.
For a complete list of severe side effects, please refer to the individual drug monographs.
Second generation cephalosporins side effects
Second generation cephalosporins generally cause few side effects. The most common side effects reported include:
- Abdominal pain
- Diarrhea
- Nausea
- Rash
- Vomiting.
Transient increases in liver enzymes have also been reported
For a complete list of side effects, please refer to the individual drug monographs.
Third generation cephalosporins
3rd generation cephalosporins followed the second-generation cephalosporins. No one third-generation cephalosporin treats all infectious disease scenarios.
Third generation cephalosporins include cefdinir, cefditoren, cefixime, cefoperazone, cefotaxime, cefpodoxime, ceftazidime, ceftibuten, ceftizoxime, and ceftriaxone, which are less active than first- and second generation drugs against gram-positive bacteria, but more active against gram-negative organisms and have greater stability against beta-lactamases.
Cefotaxime and ceftizoxime (discontinued) offer the best gram-positive coverage out of all the third-generation agents; ceftazidime and cefoperazone (discontinued) are unique in that they provide antipseudomonal coverage.
Ceftriaxone has a long half-life which allows for once daily dosing and may be used for the treatment of gonorrhea, pelvic inflammatory disease, and epididymo-orchitis. It is also an alternative to penicillins for suspected meningitis.
All the third-generation cephalosporins except for cefoperazone (discontinued) penetrate cerebrospinal fluid.
Third generation cephalosporins may be used to treat the following types of infections when caused by susceptible strains of bacteria:
- Bacteremia/septicemia
- Bone and joint infections
- Central nervous system infections
- Gynecological infections
- Intra-abdominal infections
- Lower respiratory tract infections
- Skin and skin structure infections
- Urinary tract infections.
Cephalosporins are not usually used as a first-choice antibiotic. They tend to be reserved for use when other antibiotics (often penicillins) cannot be used.
There are differences between third-generation cephalosporins with regards to the bacteria they are effective against. No one third-generation cephalosporin treats all infectious disease scenarios.
Cefotaxime and ceftizoxime (discontinued) offer the best gram-positive coverage out of all the third-generation agents; ceftazidime and cefoperazone (discontinued) are unique in that they provide antipseudomonal coverage.
Ceftriaxone has a long half-life which allows for once daily dosing and may be used for the treatment of gonorrhea, pelvic inflammatory disease, and epididymo-orchitis. It is also an alternative to penicillins for suspected meningitis.
All the third-generation cephalosporins except for cefoperazone (discontinued) penetrate cerebrospinal fluid.
Table 3. Third generation cephalosporins
| Generic name | Brand name examples |
|---|---|
| cefdinir | Omnicef |
| cefditoren | Spectracef |
| cefixime | Suprax |
| cefoperazone | Discontinued |
| cefotaxime | Claforan |
| cefpodoxime | Generic |
| ceftazidime | Fortaz, Tazicef |
| ceftibuten | Cedax |
| ceftriaxone | Generic |
Third generation cephalosporins safety
Third generation cephalosporins are generally safe, with low toxicity and good efficacy against susceptible bacteria.
Allergic reactions have been reported with all cephalosporins including third generation cephalosporins and symptoms may include a rash, hives (urticaria), swelling, or rarely, anaphylaxis. Up to 10% of people with a history of penicillin allergy will also be allergic to cephalosporins.
Drug-induced hemolytic anemia has been associated with use of some cephalosporins, including third generation cephalosporins; suspect and investigate further if anemia develops during or after treatment.
Rarely, some people may develop a super-infection due to overgrowth of a naturally occurring bacterium called Clostridium difficile, following use of any antibiotic, including cephalosporins. Symptoms may include severe diarrhea.
Rarely, seizures have been reported with cephalosporins; the risk may be greatest in those with kidney disease.
Cephalosporin should be given exactly as directed. Potentially life-threatening arrhythmias have been reported following rapid bolus administration of cefotaxime, a third generation cephalosporin.
For a complete list of severe side effects, please refer to the individual drug monographs.
Third generation cephalosporins side effects
Third generation cephalosporins generally cause few side effects. The most common side effects reported include:
- Abdominal pain
- Diarrhea
- Injection site inflammation
- Itchy skin
- Nausea
- Rash
- Vomiting.
Transient increases in liver enzymes have also been reported.
For a complete list of side effects, please refer to the individual drug monographs.
Fourth generation cephalosporins
Fourth generation cephalosporins are structurally related to third-generation cephalosporins but possess an extra ammonium group, which allows them to rapidly penetrate through the outer membrane of Gram-negative bacteria, enhancing their activity. They are also active against β-lactamase producing Enterobacteriaceae which may inactivate third-generation cephalosporins.
Some fourth-generation cephalosporins have excellent activity against gram-positive bacteria such as methicillin-susceptible staphylococci, penicillin-resistant pneumococci, and viridans group streptococci.
Fourth generation cephalosporins include cefepime, which are active against a wide range of both gram-positive and gram-negative organisms.
Cefepime is the only fourth generation cephalosporin available in the United States. Cefpirome is available overseas.
Table 4. Fourth generation cephalosporins
| Generic name | Brand name examples |
|---|---|
| cefepime | Maxipime |
Fifth generation cephalosporins
Fifth generation cephalosporins include ceftaroline and ceftolozane/tazabactam, which are active against a wide range of both gram-positive and gram-negative organisms including methicillin resistant Staphylococcus aureus (MRSA). These agents are sometimes referred to as advanced generation rather than fifth generation cephalosporins.
Ceftaroline is currently the only next-generation cephalosporin available in the United States. It is active against methicillin-resistant Staphylococcus aureus (MRSA) and gram-positive bacteria. It also retains the activity of the later-generation cephalosporins and is effective against susceptible gram-negative bacteria.
In adults and children aged two years and older ceftaroline is approved to treat:
- Pneumonia that is acquired in the community (not in hospital)
- Skin and skin structure infections.
Table 5. Fifth generation cephalosporins
| Generic name | Brand name examples |
|---|---|
| ceftaroline | Teflaro |
Fifth generation cephalosporins safety
Next generation cephalosporins are generally safe, with low toxicity and good efficacy against susceptible bacteria.
Allergic reactions have been reported with all cephalosporins including ceftaroline and symptoms may include a rash, hives (urticaria), swelling, or rarely, anaphylaxis. Up to 10% of people with a history of penicillin allergy will also be allergic to cephalosporins.
A positive Coombs test (a test that checks your blood for antibodies that attack red blood cells) has been reported in up to 18% of children and 11% of adults taking ceftaroline. This may be associated with red blood cell hemolysis and drug-induced hemolytic anemia should be suspected if anemia develops during or after treatment.
Rarely, some people may develop a super-infection due to overgrowth of a naturally occurring bacterium called Clostridium difficile, following use of any antibiotic, including cephalosporins. Symptoms may include severe diarrhea.
Rarely, seizures have been reported with ceftaroline; the risk may be greatest in those with kidney disease.
For a complete list of severe side effects, please refer to the ceftaroline drug monograph.
Fifth generation cephalosporins side effects
Ceftaroline generally causes few side effects. The most common side effects reported include:
- Abdominal pain
- Constipation
- Diarrhea
- Dyspepsia
- A headache
- Insomnia
- Itchy skin
- Gastritis
- Nausea
- Rash
- Vomiting.
Transient increases in liver enzymes have also been reported
For a complete list of side effects, please refer to the ceftaroline drug monograph.
What are cephalosporins used for?
Cephalosporins may be used to treat infections caused by susceptible bacteria, such as:
- Bone infections
- Ear infections (eg, otitis media)
- Skin infections
- Upper respiratory tract infections
- Urinary tract infections.
Cephalosporins are not usually used as a first-choice antibiotic. They tend to be reserved for use when other antibiotics (often penicillins) cannot be used.
Are cephalosporins safe?
Cephalosporins are generally safe, with low toxicity and good efficacy against susceptible bacteria.
Allergic reactions have been reported with cephalosporins and symptoms may include a rash, hives (urticaria), swelling, or rarely, anaphylaxis. Up to 10% of people with a history of penicillin allergy will also be allergic to cephalosporins.
Rarely, seizures have been reported with some cephalosporins; the risk is greatest in those with kidney disease.
Cephalosporins have also been associated with a reduced ability of the blood to clot leading to prolonged bleeding times. People with kidney or liver disease, nutritionally deprived, taking cephalosporins long-term, or concurrently receiving anticoagulant therapy are more at risk.
For a complete list of severe side effects, please refer to the individual drug monographs.
What are the side effects of cephalosporins?
Cephalosporins have side effects similar to penicillin, and drug-allergy and hypersensitivity are often (but not always) shared. Cephalosporins generally cause few side effects. The most common side effects reported include abdominal pain, diarrhea, dyspepsia, headache, gastritis, and nausea and vomiting. Transient liver problems have also been reported.
Rarely, some people may develop a super-infection due to overgrowth of a naturally occurring bacterium called Clostridium difficile, following use of any antibiotic, including cephalosporins. Symptoms may include severe diarrhea.
Uncommonly, an overgrowth of the yeast, Candida albicans, may occur following cephalosporin use, resulting in the symptoms of thrush.
For a complete list of side effects, please refer to the individual drug monographs.
The cephalosporins in general have been associated with little hepatotoxicity and only rare instances of drug induced liver injury due to these agents have been published. A special exception is ceftriaxone, a third generation cephalosporin which, when given parenterally, can cause biliary sludge with symptoms of cholecystitis and cholestatic jaundice. For these reasons, other than for ceftriaxone, the cephalosporins will be discussed as a general class rather than individual agents, and separately for the intravenous and oral forms.
The cephalosporins are assigned a likelihood score of causing clinically apparent liver injury as a class. Some have been implicated in only a few cases, but in general the liver injury from cephalosporins is similar from case to case. The typical case of liver injury from cephalosporins is a self-limited cholestatic hepatitis with mild if any immunoallergic features that arises 1 to 3 weeks after starting therapy, sometimes occurring after a single parenteral dose.