Cervical motion tenderness
Cervical motion tenderness also known as Chandelier sign, is a gynecological bimanual examination finding that could be indicative of peritoneal infection or certain pelvic inflammatory processes such as pelvic inflammatory disease (PID) 1. Cervical motion tenderness is a significant clinical finding that can change the differential diagnosis for a patient and is assessable in female patients of various ages.
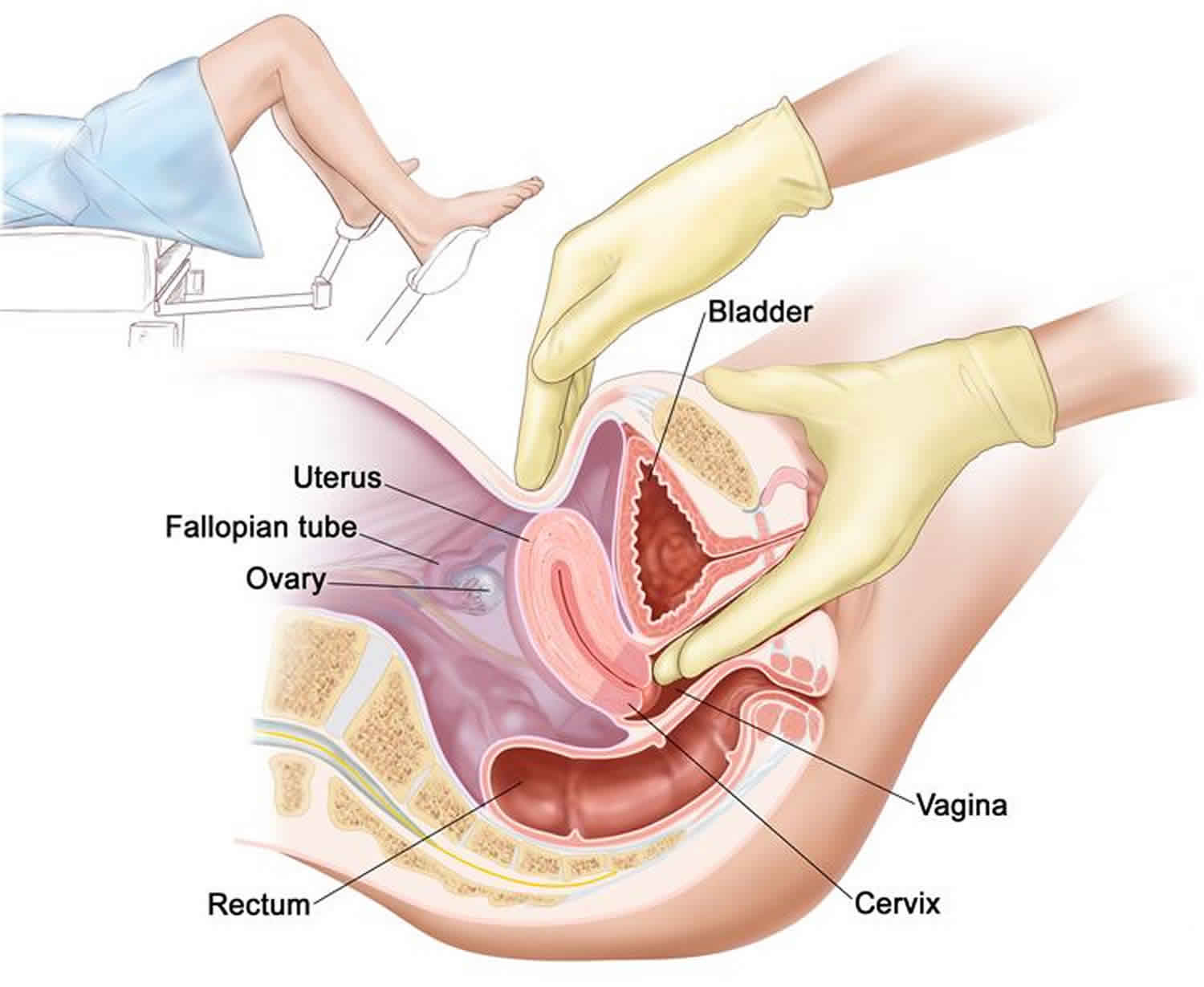
Pelvic examination starts with an exterior examination and progresses to the examination of the introitus, the vagina, and the cervix. Further details of the pelvic examination will be excluded from this activity; however, all components of the pelvic examination are essential for a comprehensive assessment of the patient. Evaluation of cervical motion tenderness occurs during the bimanual examination, performed by inserting the index finger and middle finger into the vagina until they are at the limit of the vaginal vault in the posterior fornix, which is posterior and caudad to the cervix. The examiner then uses their other hand to place pressure on the abdominal wall, over the suprapubic region. Each hand applies pressure towards the opposite hand, which allows for circumferential examination of the cervix for size, position, shape, mobility, and to assess if there is any present tenderness or palpable masses. After cervical motion testing, it is crucial to continue onto the bimanual examination of the uterus for a complete assessment. This is accomplished by applying anterior pressure towards the patient’s abdominal wall and assessing for the size, position, shape, tenderness, and mobility of the uterus itself. To finish the bimanual assessment examination of the adnexa is performed by placing the fingers to the side of the cervix, deep to the lateral fornix with pressure towards the anterior abdominal wall, and applying pressure with the abdominal hand toward the symphysis overlying the supporting structures including the ovaries. This will allow the examiner to distinguish the location of any acute tenderness, and note if there is any isolated cervical motion tenderness. This technique may vary in patients with different body mass index classes 2.
Additionally, there is documentation of utilizing sonography to assess for cervical motion tenderness, in which cervical motion undergoes evaluation when performing a transvaginal ultrasound. This also serves the purpose of visualizing the pelvic structures after discovering this exam finding. In the study conducted by Tayal et al. 3, out of the 30 patients enrolled across various body mass index classes, physician confidence was higher in clinical findings of uterine and adnexal tenderness, but there was no increase in confidence of cervical motion tenderness or retrovaginal tenderness. Although further studies are warranted, the expectation is that physical exam skills remain paramount in ascertaining a medical diagnosis, though the use of sonography clearly has a place in the assessment of a patient.
Cervical motion tenderness in and of itself can be indicative of peritoneal irritation. Cervical motion tenderness alone can add to the differential diagnosis of any process that has peritoneal involvement across different organ systems. Gastrointestinal: appendicitis, diverticulitis, inflammatory bowel disease, hernia, perforated abdominal viscus, abdominal wall hematoma. Urinary: ureteral lithiasis, interstitial cystitis. Gynecological: ectopic pregnancy 4, endometriosis, endometritis, pelvic inflammatory disease (PID) 5, tubo-ovarian abscess, ovarian or adnexal torsion 6, chronic pelvic cellulitis, vaginitis, cervicitis, pelvic thrombophlebitis 7. That is why it is essential to distinguish the location of the tenderness and if any additional pelvic structures are involved.
Cervical motion tenderness causes
Cervical motion tenderness is an indication of peritoneal irritation. Cervical motion tenderness could be indicative of peritoneal infection or certain pelvic inflammatory processes such as pelvic inflammatory disease (PID) 8.
Other causes of cervical motion tenderness include:
- Gastrointestinal: appendicitis, diverticulitis, inflammatory bowel disease, hernia, perforated abdominal viscus, abdominal wall hematoma.
- Urinary: ureteral lithiasis, interstitial cystitis.
- Gynecological: ectopic pregnancy 4, endometriosis, endometritis, pelvic inflammatory disease (PID) 5, tubo-ovarian abscess, ovarian or adnexal torsion 6, chronic pelvic cellulitis, vaginitis, cervicitis, pelvic thrombophlebitis 7.
That is why it is essential to distinguish the location of the tenderness and if any additional pelvic structures are involved.
References- Cortes EG, Adamski JJ. Chandelier Sign. [Updated 2019 Aug 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK545286
- Plumptre I, Mulki O, Granados A, Gayle C, Ahmed S, Low-Beer N, Higham J, Bello F. Standardizing bimanual vaginal examination using cognitive task analysis. Int J Gynaecol Obstet. 2017 Oct;139(1):114-119.
- Tayal VS, Bullard M, Swanson DR, Schulz CJ, Bacalis KN, Bliss SA, Norton HJ. ED endovaginal pelvic ultrasound in nonpregnant women with right lower quadrant pain. Am J Emerg Med. 2008;26(1):81–85. doi: 10.1016/j.ajem.2007.02.029
- Zucchini S, Marra E. Diagnosis of emergencies/urgencies in gynecology and during the first trimester of pregnancy. J Ultrasound. 2014 Mar;17(1):41-6.
- Lusby H, Brooks A, Hamayoun E, Finley A. Uncommon cause of pelvic inflammatory disease leading to toxic shock syndrome. BMJ Case Rep. 2018 Sep 23;2018
- Dewey K, Wittrock C. Acute Pelvic Pain. Emerg. Med. Clin. North Am. 2019 May;37(2):207-218.
- Waheed A, Foris LA, Lipe DN, King KC. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jul 7, 2019. Septic Thrombophlebitis
- Lewiss RE, Saul T, Goldflam K. Sonographic cervical motion tenderness: A sign found in a patient with pelvic inflammatory disease. Crit Ultrasound J. 2012;4(1):20. Published 2012 Sep 18. doi:10.1186/2036-7902-4-20 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3480933