What is colorectal cancer screening
Screening is the process of looking for cancer in people who have no symptoms. Colon cancer screening can detect polyps and early cancers in the large intestine. Colon cancer screening can find problems that can be treated before cancer develops or spreads. Regular colon cancer screenings may reduce the risk for death and complications caused by colorectal cancer.
The lifetime risk of developing colorectal cancer is about 1 in 22 (4.49%) for men and 1 in 24 (4.15%) for women 1. This risk is slightly lower in women than in men. Excluding skin cancers, colorectal cancer is the third most common cancer diagnosed in both men and women in the United States. The American Cancer Society’s estimates for the number of colorectal cancer cases in the United States for 2022 are 2, 3:
- New cases 106,180 (colon cancer only)
- New cases of rectal cancer: 44,850
- Deaths: 52,580 (colon and rectal cancers combined)
- About 4.2% of Americans are expected to develop colorectal cancer within their lifetime, and the lifetime risk of dying from colorectal cancer is 1.7% 4. Age-specific incidence and mortality rates show that most colorectal cancer cases are diagnosed after age 54 years and 78% of cases occur in patients aged 55 years and older; about 15% of colorectal cancer cases occur in patients aged 45 to 54 years 3, 5.
- Colorectal cancer is the second leading cause of cancer death in the United States. The death rate was 13.4 per 100,000 men and women per year based on 2015–2019 deaths, age-adjusted.
- Colorectal cancer represents 7.9% of all new cancer cases in the U.S.
- In 2019, there were an estimated 1,369,004 people living with colorectal cancer in the United States.
- 5-Year Relative Survival is 65.1%. Relative survival is an estimate of the percentage of patients who would be expected to survive the effects of their cancer. It excludes the risk of dying from other causes. Because survival statistics are based on large groups of people, they cannot be used to predict exactly what will happen to an individual patient. No two patients are entirely alike, and treatment and responses to treatment can vary greatly.
Several tests can be used to screen for colorectal cancer. You should have a conversation with your physicians to decide which type of screening is best for you.
Colorectal cancer screening tests can be divided into 2 main groups:
- Stool-based tests: These tests check the stool (feces) for signs of cancer. These tests are less invasive and easier to have done, but they need to be done more often.
- Visual (structural) exams: These tests look at the structure of the colon and rectum for any abnormal areas. This is done either with a scope (a tube-like instrument with a light and tiny video camera on the end) put into the rectum, or with special imaging (x-ray) tests.
These tests each have different pros and cons (see Table 1 below), and some of them might be better options for you than others. But the most important thing is to get screened, no matter which test you choose.
If you choose to be screened with a test other than colonoscopy, any abnormal test result should be followed up with colonoscopy.
These tests, as well as others, can also be used when people have symptoms of colorectal cancer or other digestive diseases such as inflammatory bowel disease.
People at increased or high risk of colon cancer—because of a family or a personal history of colon cancer, inflammatory bowel disease, previous radiation to the abdomen or other conditions that increase the risk of colon cancer—might need to start screening before age 45 and be screened more often, typically with a colonoscopy.
There is not enough evidence to say which screening method is best. But, colonoscopy is most thorough. A colonoscopy is currently the “gold standard” for colon cancer screening in the U.S. and some healthcare practitioners may recommend it over other testing options. Talk to your healthcare provider about which test is right for you. A recently published review 6 of data from thirty-one colon cancer screening studies shows that an annual at-home stool test called a fecal immunochemical test (FIT) may be as effective as a colonoscopy at detecting cancer in average-risk adults. While the data review adds support for colon cancer screening with inexpensive and non-invasive stool tests, authors of the study recommend patients discuss with their healthcare practitioners their risk for developing colon cancer and whether an annual stool test is appropriate for them.
Both men and women should have a colon cancer screening test starting at age 50 (or age 45 if following the American Cancer Society Guideline). Some providers recommend that African Americans begin screening at age 45.
With a recent increase in colon cancer in people in their 40s, the American Cancer Society recommends that healthy men and women start screening at age 45. Talk to your provider if you’re concerned.
Colon cancer screening options for people with an average risk for colon cancer:
- Colonoscopy every 10 years starting at age 45 or 50
- Guaiac-based fecal occult blood test (gFOBT) or fecal immunochemical test (FIT) every year (colonoscopy is needed if results are positive)
- Stool DNA (sDNA) every 1 or 3 years (colonoscopy is needed if results are positive)
- Flexible sigmoidoscopy every 5 to 10 years, usually with stool testing guaiac-based fecal occult blood test (gFOBT) done every 1 to 3 years
- Virtual colonoscopy (CT colonoscopy) every 5 years
Screening for higher-risk people
People with certain risk factors for colon cancer may need earlier (before age 50) or more frequent testing.
More common risk factors are:
- A family history of inherited colorectal cancer syndromes, such as familial adenomatous polyposis (FAP) or hereditary nonpolyposis colorectal cancer (HNPCC).
- A strong family history of colorectal cancer or polyps. This usually means close relatives (parent, sibling, or child) who developed these conditions younger than age 60.
- A personal history of colorectal cancer or polyps.
- A personal history of long-term (chronic) inflammatory bowel disease (for example ulcerative colitis or Crohn disease).
Screening for these groups is more likely to be done using colonoscopy.
Table 1. Pros and Cons of colorectal cancer screening tests
| Test | Pros | Cons |
|---|---|---|
| Fecal immunochemical test (FIT) | No direct risk to the colon No bowel prep No pre-test diet or medication changes needed Sampling done at home Fairly inexpensive | Can miss many polyps and some cancers Can have false-positive test results Needs to be done every year Colonoscopy will be needed if abnormal |
| Guaiac-based fecal occult blood test (gFOBT) | No direct risk to the colon No bowel prep Sampling done at home Inexpensive | Can miss many polyps and some cancers Can have false-positive test results Pre-test diet changes (and possibly medication changes) are needed Needs to be done every year Colonoscopy will be needed if abnormal |
| Stool DNA test | No direct risk to the colon No bowel prep No pre-test diet or medication changes needed Sampling done at home | Can miss many polyps and some cancers Can have false-positive test results Should be done every 3 years Colonoscopy will be needed if abnormal Still fairly new – may be insurance coverage issues |
| Colonoscopy | Can usually look at the entire colon Can biopsy and remove polyps Done every 10 years Can help find some other diseases | Can miss small polyps Full bowel prep needed Costs more on a one-time basis than other forms of testing Sedation is usually needed, in which case you will need someone to drive you home You may miss a day of work Small risk of bleeding, bowel tears, or infection |
| CT colonography (virtual colonoscopy) | Fairly quick and safe Can usually see the entire colon Done every 5 years No sedation needed | Can miss small polyps Full bowel prep needed Some false-positive test results Exposure to a small amount of radiation Can’t remove polyps during testing Colonoscopy will be needed if abnormal Still fairly new – may be insurance coverage issues |
| Flexible sigmoidoscopy | Fairly quick and safe Usually doesn’t require full bowel prep Sedation usually not used Does not require a specialist Done every 5 years | Not widely used as a screening test Looks at only about a third of the colon Can miss small polyps Can’t remove all polyps May be some discomfort Very small risk of bleeding, infection, or bowel tear Colonoscopy will be needed if abnormal |
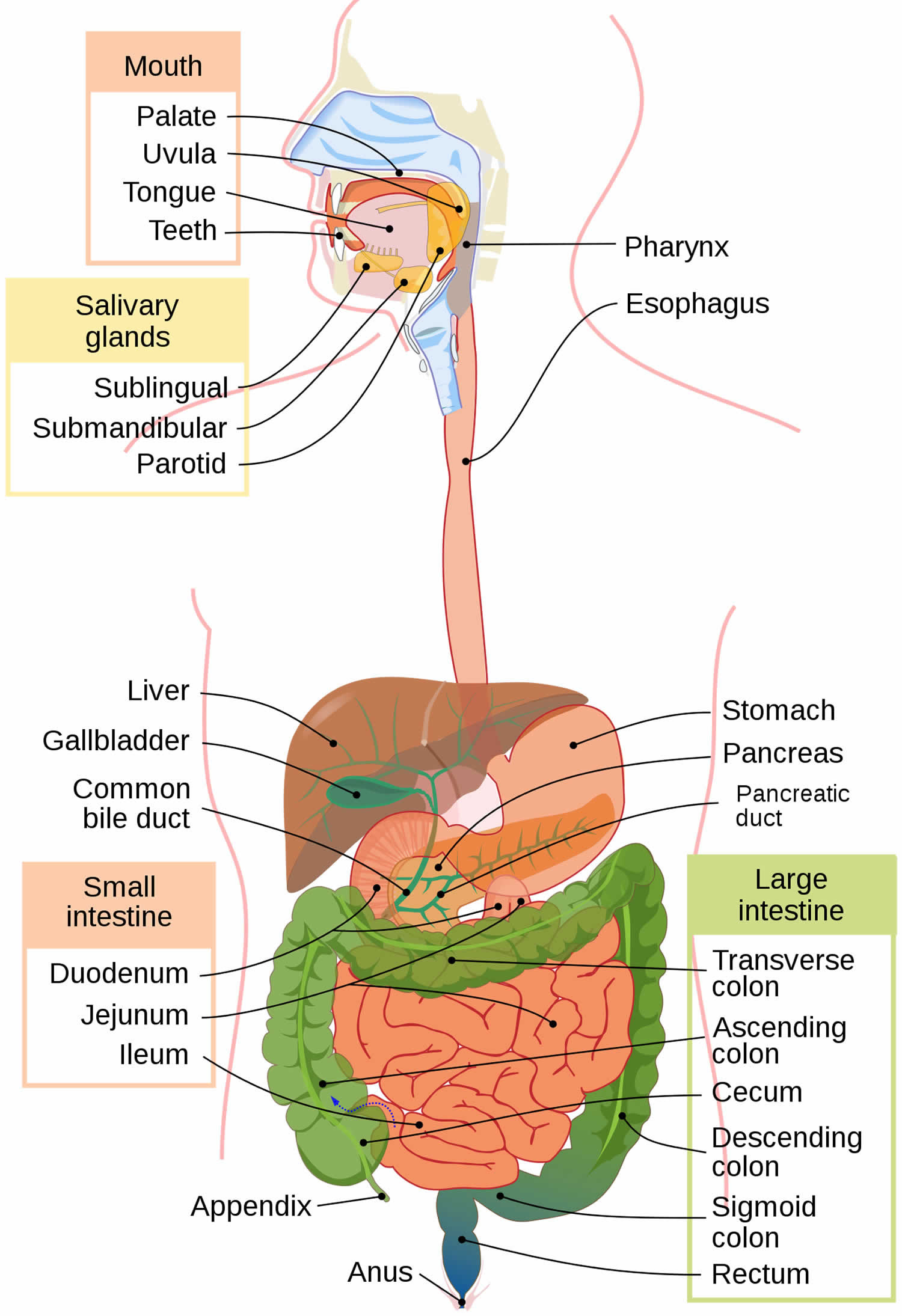
The colon and rectum anatomy
To understand colorectal cancer, it helps to know about the normal structure and function of the colon and rectum.
The colon and rectum make up the large intestine (or large bowel), which is part of the digestive system, also called the gastrointestinal (GI) system (see Figure 1 below). The digestive tract includes the mouth, esophagus, stomach, small intestine, large intestine, and rectum. The large intestine is approximately 5 feet (1.5 meters) long, making up one-fifth of the length of the gastrointestinal (GI) tract 8. The large intestine is responsible for processing indigestible food material (chyme) after most nutrients are absorbed in the small intestine. The large intestine performs an essential role by absorbing water, vitamins, and electrolytes from waste material 9, 10.
The large intestine is composed of 4 parts. It includes the cecum and ascending colon, transverse colon, descending colon, and sigmoid colon. The parts of the colon are named by which way the food is traveling through them.
- The first section is called the ascending colon. It starts with a pouch called the cecum, where undigested food is comes in from the small intestine. It continues upward on the right side of the abdomen (belly).
- The second section is called the transverse colon. It goes across the body from the right to the left side.
- The third section is called the descending colon because it descends (travels down) on the left side.
- The fourth section is called the sigmoid colon because of its “S” shape. The sigmoid colon joins the rectum, which then connects to the anus.
The ascending and transverse colon together are called the proximal colon. The descending and sigmoid colon are called the distal colon.
Figure 1. Gastrointestinal tract (human digestive system)
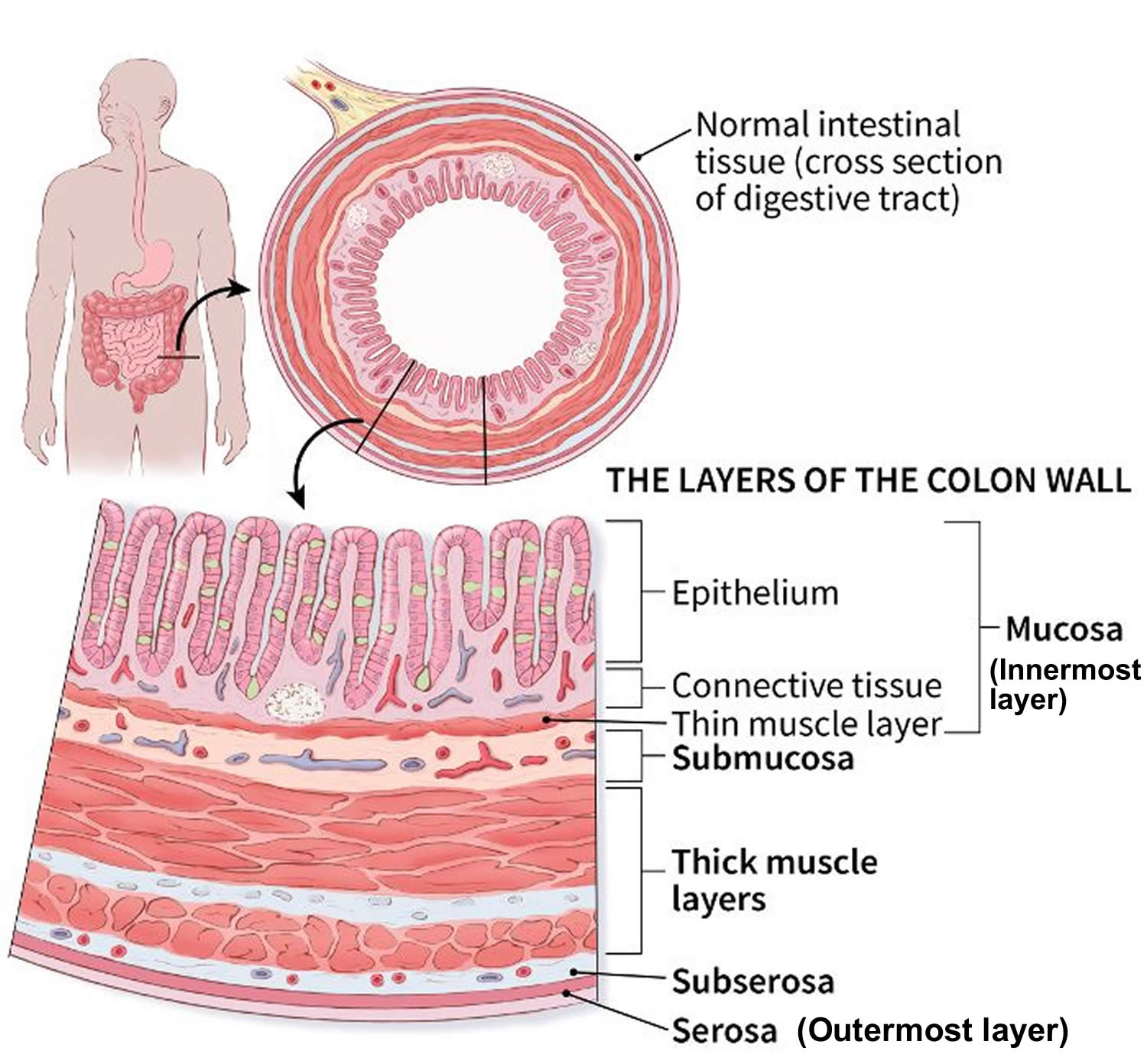
The intestinal wall
The intestinal wall is made up of multiple layers. The 4 layers of the large intestine from the lumen outward are the mucosa, submucosa, muscular layer, and serosa (Figure 2). The muscular layer is made up of 2 layers of smooth muscle, the inner, circular layer, and the outer, longitudinal layer.
Figure 2. Large intestine wall layers
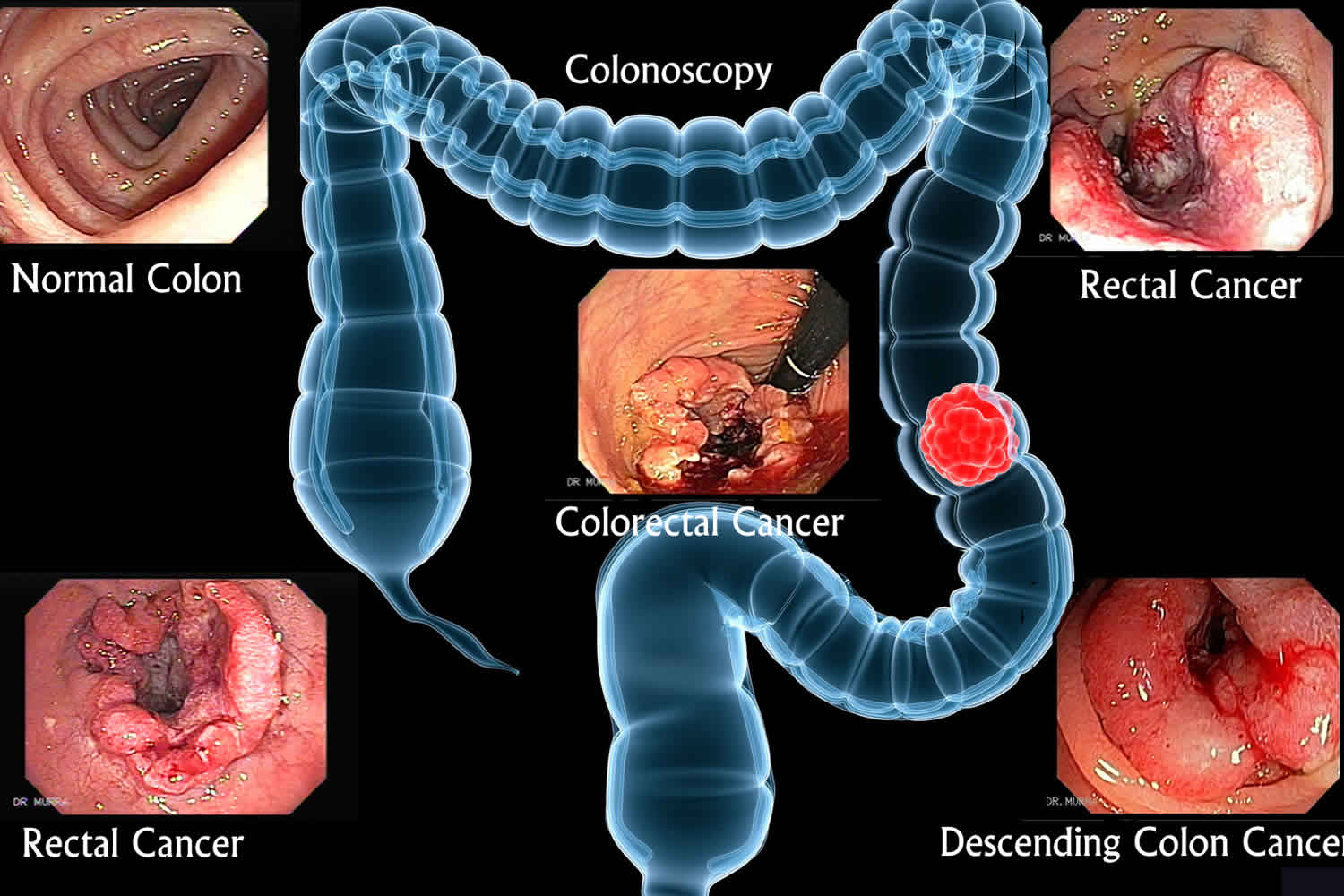
Figure 3. Large intestine anatomy (normal)
Colon cancer screening guidelines
The American Cancer Society 11 recently lowered their recommended starting age for colon cancer screening to age 45 for people with an average risk of colon cancer. That is five years earlier than the American Cancer Society had previously recommended. While no other health organizations have lowered their recommended starting age, the American Cancer Society says they decided to make the change in their latest guidelines because of increasing rates of colon cancer among younger people in recent years.
The American Cancer Society made its decision after reviewing data from a major analysis by staff researchers. The data showed that new cases of colon cancer are occurring at an increasing rate among younger adults. Experts on the American Cancer Society Guideline Development Group determined that beginning screening at age 45 for adults of average risk for colon cancer will result in more lives saved.
Authors of the guideline say that “lowering the starting age is expected to benefit not only the segments of the population who suffer disproportionately from [colon cancer]—blacks, Alaska Natives, and American Indians—but also those individuals otherwise considered to be at average risk.”
People at average risk for colon cancer include those who have:
- No personal history of polyps or colon cancer
- No family history of colon cancer
- No personal history of inflammatory bowel disease (e.g., Crohn disease, ulcerative colitis)
The incidence of colon cancer has decreased over the last twenty years in people age 55 and older due in part to screening that results in the removal of cancerous and precancerous polyps. However, there has been a 51% increase in colon cancer among people younger than age 50 since 1994. Lately, deaths from colon cancer in this age group have also begun to rise. A recent analysis also found that adults born around 1990 have twice the risk of colon cancer and four times the risk of rectal cancer compared with adults born around 1950, who have the lowest risk. The rectum is connected to the colon and screening detects cancer in the rectum too. However, the reason for the increase is not yet understood, according to the new guidelines.
For people at average risk
The American Cancer Society recommends that people at average risk of colorectal cancer start regular screening at age 45. This can be done either with a sensitive test that looks for signs of cancer in a person’s stool (a stool-based test), or with an exam that looks at the colon and rectum (a visual exam). These options are listed below.
- People who are in good health and with a life expectancy of more than 10 years should continue regular colorectal cancer screening through the age of 75.
- For people ages 76 through 85, the decision to be screened should be based on a person’s preferences, life expectancy, overall health, and prior screening history.
- People over 85 should no longer get colorectal cancer screening.
For screening, people are considered to be at average risk if they do not have:
- A personal history of colorectal cancer or certain types of polyps
- A family history of colorectal cancer
- A personal history of inflammatory bowel disease (ulcerative colitis or Crohn’s disease)
- A confirmed or suspected hereditary colorectal cancer syndrome, such as familial adenomatous polyposis (FAP) or Lynch syndrome (hereditary non-polyposis colon cancer or HNPCC)
- A personal history of getting radiation to the abdomen (belly) or pelvic area to treat a prior cancer
The American Cancer Society guidelines do not prioritize a particular screening test—there are several tests that can detect precancerous polyps and/or colon cancer—and instead says patients and their healthcare practitioners should choose from among several tests based on the patient’s preference. How often to be tested depends on which test the patient chooses. Options include:
- Fecal immunochemical test (FIT) or high-sensitivity guaiac-based fecal occult blood test (hsgFOBT) every year
- Stool DNA test every 3 years
- Colonoscopy every 10 years
- CT colonography (virtual colonoscopy using x-ray equipment) every 5 years
- Sigmoidoscopy, every 5 years
If a test other than a colonoscopy indicates a possibility of cancer, that should be followed up with a colonoscopy as soon as possible.
The new guidelines also recommend that after age 75, people discuss the need for screening with their physician. After age 85, there is no longer a need for colon cancer screening, according to the American Cancer Society.
For people at increased or high risk of colorectal cancer
People at increased or high risk of colorectal cancer might need to start colorectal cancer screening before age 45, be screened more often, and/or get specific tests. This includes people with:
- A strong family history of colorectal cancer or certain types of polyps (see Colorectal Cancer Risk Factors)
- A personal history of colorectal cancer or certain types of polyps
- A personal history of inflammatory bowel disease (ulcerative colitis or Crohn’s disease)
- A known family history of a hereditary colorectal cancer syndrome such as familial adenomatous polyposis (FAP) or Lynch syndrome (also known as hereditary non-polyposis colon cancer or HNPCC)
- A personal history of radiation to the abdomen (belly) or pelvic area to treat a prior cancer
The American Cancer Society does not have screening guidelines specifically for people at increased or high risk of colorectal cancer. However, some other professional medical organizations, such as the US Multi-Society Task Force on Colorectal Cancer (USMSTF), do put out such guidelines. These guidelines are complex and are best looked at along with your health care provider. In general, these guidelines divide people into several groups (although the details depend on each person’s specific risk factors).
People at increased risk for colorectal cancer
- People with one or more family members who have had colon or rectal cancer: Screening recommendations for these people depend on who in the family had cancer and how old they were when it was diagnosed. Some people with a family history will be able to follow the recommendations for average risk adults, but others might need to get a colonoscopy (and not any other type of test) more often, and possibly starting before age 45.
- People who have had certain types of polyps removed during a colonoscopy: Most of these people will need to get a colonoscopy again after 3 years, but some people might need to get one earlier (or later) than 3 years, depending on the type, size, and number of polyps.
- People who have had colon or rectal cancer: Most of these people will need to start having colonoscopies regularly within a year of surgery to remove the cancer. Other procedures like ultrasound might also be recommended for some people with rectal cancer, depending on the type of surgery they had.
- People who have had radiation to the abdomen (belly) or pelvic area to treat a prior cancer: Most of these people will need to start having colonoscopies at an earlier age (depending on how old they were when they got the radiation), and might need to be screened more often than normal (such as at least every 5 years).
People at high risk for colorectal cancer
- People with inflammatory bowel disease (Crohn’s disease or ulcerative colitis): These people generally need to get colonoscopies (not any other type of test) every 1 to 2 years, starting at an earlier age.
- People known or suspected to have certain genetic syndromes: These people generally need to have colonoscopy (not any of the other tests). Screening is often recommended to begin at a young age, possibly as early as the teenage years for some syndromes – and needs to be done much more frequently. Specifics depend on which genetic syndrome you have, and other factors.
If you’re at increased or high risk of colorectal cancer (or think you might be), talk to your health care provider to learn more. Your provider can suggest the best screening option for you, as well as determine what type of screening schedule you should follow, based on your individual risk.
USPSTF colon cancer screening guidelines
The US Preventive Services Task Force (USPSTF) colon cancer screening guidelines is in the process of being updated in 2019.
The US Preventive Services Task Force (USPSTF) colon cancer screening guidelines – 2021 recommendations 12:
- Adults aged 45 to 75 years: The USPSTF recommends screening for colorectal cancer starting at age 50 years and continuing until age 75 years. The risks and benefits of different screening methods vary.
- Adults aged 76 to 85 years: The USPSTF recommends that clinicians selectively offer screening for colorectal cancer in adults aged 76 to 85 years. Evidence indicates that the net benefit of screening all persons in this age group is small. The decision to screen for colorectal cancer in adults aged 76 to 85 years should be an individual one, taking into account the patient’s overall health, prior screening history and preferences.
- Adults in this age group who have never been screened for colorectal cancer are more likely to benefit.
- Screening would be most appropriate among adults who 1) are healthy enough to undergo treatment if colorectal cancer is detected and 2) do not have comorbid conditions that would significantly limit their life expectancy.
The US Preventive Services Task Force (USPSTF) recommended screening strategies include 13:
- High-sensitivity guaiac fecal occult blood test (HSgFOBT) or fecal immunochemical test (FIT) every year
- Stool DNA-FIT every 1 to 3 years
- Computed tomography colonography every 5 years
- Flexible sigmoidoscopy every 5 years
- Flexible sigmoidoscopy every 10 years + annual FIT
- Colonoscopy screening every 10 years
Colon cancer screening test
There are several test options for colon cancer screening.
Several test options are available for colorectal cancer screening:
Stool-based tests
This method checks your stool (feces) for blood. Polyps in the colon and small cancers can cause small amounts of bleeding that cannot be seen with the naked eye. But blood can often be found in the stool.
Many people find stool tests easier to have than tests like colonoscopy, and they are typically done at home. But these tests need to be done more often. And if the result from one of these stool tests is positive (abnormal), you’ll still need a colonoscopy to see if you have cancer.
The most common test used is the guaiac-based fecal occult blood test (gFOBT). Two other tests are called the fecal immunochemical test (FIT) and stool DNA test (sDNA).
- Highly sensitive fecal immunochemical test (FIT) every year
- Highly sensitive guaiac-based fecal occult blood test (gFOBT) every year
- Multi-targeted stool DNA test (MT-sDNA) every 3 years
Fecal immunochemical test (FIT)
One way to test for colorectal cancer is to look for occult (hidden) blood in stool. The idea behind this type of test is that blood vessels in larger colorectal polyps or cancers are often fragile and easily damaged by the passage of stool. The damaged vessels usually bleed into the colon or rectum, but only rarely is there enough bleeding for blood to be seen in the stool.
The fecal immunochemical test (FIT) is also called an immunochemical fecal occult blood test (iFOBT). It tests for hidden blood in the stool. This test reacts to part of the human hemoglobin protein, which is found in red blood cells.
For this test, small amounts of stool are collected on cards (or in tubes). You can do this in the privacy of your own home. Unlike the gFOBT (see below), there are no drug or dietary restrictions before the test (as vitamins and foods do not affect the FIT), and collecting the samples may be easier. This test is also less likely to react to bleeding from other parts of the digestive tract, such as the stomach.
This test must be done every year, unlike some other tests (like the visual tests described below).
If the test results are positive (that is, if hidden blood is detected), a colonoscopy will be needed to investigate further. Although blood in the stool can be from cancers or polyps, it can also have other causes, such as ulcers, hemorrhoids, or other conditions.
Collecting the samples
Your health care provider will give you the supplies you need for testing. Have all of your supplies ready and in one place. Supplies typically include a test kit, test cards or tubes, long brushes or other collecting devices, waste bags, and a mailing envelope. The kit will give you detailed instructions on how to collect the samples. Be sure to follow the instructions that come with your kit, as different kits might have different instructions. If you have any questions about how to use your kit, contact your health care provider’s office or clinic. Once you have collected the samples, return them as instructed in the kit.
Guaiac-based fecal occult blood test (gFOBT)
The guaiac-based fecal occult blood test (gFOBT) detects occult (hidden) blood in the stool through a chemical reaction, in a different way than a fecal immunochemical test (FIT). But like the fecal immunochemical test (FIT), this test can’t tell if the blood is from the colon or from other parts of the digestive tract (such as the stomach).
The American Cancer Society recommends the more modern, highly sensitive versions of this test for screening.
This test must be done every year, unlike some other tests (like the visual tests described below).
This test is done with a kit that you can use in the privacy of your own home that allows you to check more than one stool sample. A FOBT done during a digital rectal exam in the doctor’s office (which only checks one stool sample) is not enough for proper screening, as it is likely to miss most colorectal cancers.
If the test results are positive (that is, if hidden blood is detected), a colonoscopy will be needed to find the reason for the bleeding. It’s not enough to simply repeat this test or follow up with tests other than a colonoscopy.
Before the fecal occult blood test test
Some foods or drugs can affect the results of this test, so you may be instructed to avoid the following before this test:
- Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil), naproxen (Aleve), or aspirin, for 7 days before testing. (They can cause bleeding, which can lead to a false-positive result.) Note: People should try to avoid taking NSAIDs for minor aches prior to the test. But if you take these medicines daily for heart problems or other conditions, don’t stop them for this test without talking to your health care provider first.
- Vitamin C in excess of 250 mg daily from either supplements or citrus fruits and juices for 3 days before testing. This can affect the chemicals in the test and make the result negative, even if blood is present.
- Red meats (beef, lamb, or liver) for 3 days before testing. Components of blood in the meat may cause a positive test result.
Some people who are given the test never do it or don’t return it because they worry that something they ate may affect the test. Even if you are concerned that something you ate may alter the test, the most important thing is to get the test done.
Collecting the samples
People having this test will get a kit with instructions from their health care provider’s office or clinic. The kit will explain how to take stool samples at home (usually samples from 3 straight bowel movements are smeared onto small squares of paper). The kit is then returned to the doctor’s office or medical lab (usually within 2 weeks) for testing.
When doing this test, have all of your supplies ready and in one place. Supplies typically include a test kit, test cards, either a brush or wooden applicator, and a mailing envelope. The kit will give you detailed instructions on how to collect the stool samples. Be sure to follow the instructions that come with your kit, as different kits might have different instructions. If you have any questions about how to use your kit, contact your health care provider’s office or clinic. Once you have collected the samples, return them as instructed in the kit.
Stool DNA test
A stool DNA test (also known as a multitargeted stool DNA test, or MT-sDNA) looks for certain abnormal sections of DNA from cancer or polyp cells. Colorectal cancer or polyp cells often have DNA mutations (changes) in certain genes. Cells with these mutations often get into the stool, where tests may be able to detect them. Cologuard®, the only test currently available, tests for both DNA changes and blood in the stool.
Collecting the samples
You’ll get a kit in the mail to use to collect your entire stool sample at home. The kit will have a sample container, a bracket for holding the container in the toilet, a bottle of liquid preservative, a tube, labels, and a shipping box. The kit has detailed instructions on how to collect the sample. Be sure to follow the instructions that come with your kit. If you have any questions about how to use your kit, contact your doctor’s office or clinic. Once you have collected the sample, return it as instructed in the kit.
This test should be done every 3 years. If the test is positive (if it finds DNA changes or blood), a colonoscopy will be needed.
Visual (structural) exams of the colon and rectum
- Colonoscopy every 10 years. A colonoscopy is similar to a sigmoidoscopy, but the entire colon can be viewed. Your health care provider will give you the steps for cleansing your bowel. This is called bowel preparation. During a colonoscopy, you receive medicine to make you relaxed and sleepy.
- CT colonography (virtual colonoscopy) every 5 years. This is called a virtual colonoscopy. CT scans are used as an alternative to a regular colonoscopy.
- Flexible sigmoidoscopy (FSIG) every 5 years. This test uses a small flexible scope to view the lower part of your colon. Because the test only looks at the last one third of the large intestine (colon), it may miss some cancers that are higher in the large intestine.
There are some differences between these tests to consider, but the most important thing is to get screened, no matter which test you choose. Talk to your health care provider about which tests might be good options for you, and to your insurance provider about your coverage.
If a person chooses to be screened with a test other than colonoscopy, any abnormal test result should be followed up with colonoscopy.
Colonoscopy
With colonoscopy, the doctor looks at the entire length of the colon and rectum with a colonoscope, a flexible tube about the width of a finger with a light and small video camera on the end. It’s put in through the anus and into the rectum and colon. Special instruments can be passed through the colonoscope to biopsy (sample) or remove any suspicious-looking areas such as polyps, if needed.
Figure 4. Colonoscopy
Before the colonoscopy test
- Be sure your doctor knows about any medicines you are taking (including daily aspirin, vitamins, or supplements). You might need to change how you take them before the test.
- The colon and rectum must be empty and clean so your doctor can see the entire inner lining during the test. There are different ways to do this, including pills, fluids, and enemas (or combinations of these). For example, you might need to drink large amounts of a liquid laxative solution the evening before the procedure. This often results in spending a lot of time in the bathroom. Because the process of cleaning out the colon and rectum is sometimes unpleasant, it can keep some people from getting this test done. However, newer kits are available to clean out the bowel and may be better tolerated than previous ones. Your health care provider can discuss the options with you.
- Your health care provider will give you specific instructions. It’s important to read them carefully a few days ahead of time, since you may need to follow a special diet for at least a day before the test and to shop for supplies and laxatives. If you’re not sure about any of the instructions, call the health care provider’s office and get your questions answered.
- You will probably also be told not to eat or drink anything after a certain hour the night before your test. If you normally take prescription medicines in the mornings, talk with your doctor or nurse about how to manage them for that day.
- Because a sedative is used to help keep you more comfortable during the test, you will most likely need to arrange for someone you know to take you home after the test. You might need someone to help you get into your home if you are sleepy or dizzy, so many centers that do colonoscopies will not discharge people to go home in a cab or a ridesharing service. If transportation might be a problem, talk with your health care provider about the policy at your hospital or surgery center for using one of these services. There may be other resources available for getting home, depending on the situation.
During the colonoscopy test
The test itself usually takes about 30 minutes, but it may take longer if one or more polyps is found and removed. Before the test starts, you’ll likely be given a sedative (into a vein) to make you feel relaxed and sleepy during the procedure. For most people, this medicine makes them unable to remember the procedure afterward. You’ll wake up after the test is over, but you might not be fully awake until later in the day.
During the test, you’ll be asked to lie on your side with your knees pulled up. A drape will cover you. Your blood pressure, heart rate, and breathing rate will be monitored during and after the test.
Your doctor might insert a gloved finger into the rectum to examine it before putting in the colonoscope. The colonoscope is lubricated so it can be inserted easily into the rectum. Once in the rectum, the colonoscope is passed all the way to the beginning of the colon, called the cecum.
If you’re awake, you may feel an urge to have a bowel movement when the colonoscope is inserted or pushed further up the colon. The doctor also puts air into the colon through the colonoscope to make it easier to see the lining of the colon and use the instruments to perform the test. To ease any discomfort, it may help to breathe deeply and slowly through your mouth.
The doctor will look at the inner walls of the colon as he or she slowly removes the colonoscope. If a small polyp is found, it may be removed and then sent to a lab to check if it has any areas that have changed into cancer. This is because some small polyps may become cancer over time.
If your doctor sees a larger polyp or tumor, or anything else abnormal, a small piece of it will be removed (biopsied) through the colonoscope. It will be checked in the lab to see if it’s cancer, a benign (non-cancerous) growth, or something else.
Possible side effects and complications of colonoscopy
The bowel preparation before the test can be unpleasant.
The test itself might be uncomfortable, but the sedative usually helps with this, and most people feel back to normal once the effects of the sedative wear off. Because air is pumped into the colon and rectum during the test, people sometimes feel bloated, have gas pains, or have cramping for a while after the test until the air passes out.
Some people may have low blood pressure or changes in heart rhythm from the sedation during the test, but these are rarely serious.
If a polyp is removed or a biopsy is done during the colonoscopy, you might notice some blood in your stool for a day or 2 after the test. Serious bleeding is uncommon, but in rare cases, bleeding might need to be treated or can even be life-threatening.
Colonoscopy is a safe procedure, but in rare cases the colonoscope can puncture the wall of the colon or rectum. This is called a perforation. Symptoms can include severe abdominal (belly) pain, nausea, and vomiting. This can be a major (or even life-threatening) complication, because it can lead to a serious abdominal (belly) infection. The hole may need to be repaired with surgery. Ask your doctor about the risk of this complication.
CT colonography (virtual colonoscopy)
This test is an advanced type of computed tomography (CT) scan of the colon and rectum. A CT scan uses x-rays, but instead of taking one picture, like a regular x-ray, a CT scanner takes many pictures as it rotates around you while you lie on a table. A computer then combines these pictures into detailed images of the part of your body being studied.
For CT colonography, special computer programs create both 2-dimensional x-ray pictures and a 3-dimensional view of the inside of the colon and rectum, which lets the doctor look for polyps or cancer.
This test may be especially useful for some people who can’t have or don’t want to have a more invasive test such as a colonoscopy. It can be done fairly quickly, and sedation isn’t needed.
But although this test is not invasive like a colonoscopy, the same type of bowel prep is needed. A small, flexible tube is also put in the rectum for this test to fill the colon and rectum with air. And if polyps or other suspicious areas are seen on this test, a colonoscopy will still be needed to remove them or to explore them fully.
Figure 5. CT colonography
Before the virtual colonoscopy test
It’s important that the colon and rectum are emptied before this test to get the best images. You’ll probably be told to follow a clear liquid diet for at least a day before the test. There are a number of ways to clean out the colon and rectum before the test. Often, the evening before the procedure, you drink large amounts of a liquid laxative solution. This often results in spending a lot of time in the bathroom. The morning of the test, sometimes more laxatives or enemas may be needed to make sure the bowels are empty. Newer kits are available to clean out the bowel and may be better tolerated than previous ones. Your doctor can discuss the options with you.
During the virtual colonoscopy test
CT colonoscopy test is done in a special room with a CT scanner. It takes about 10 minutes. You may be asked to drink a contrast solution before the test to help “tag” any stool left in the colon or rectum, which helps the doctor when looking at the test images. You’ll be asked to lie on a narrow table that’s part of the CT scanner, and will have a small, flexible tube put into your rectum. Air is pumped through the tube into the colon and rectum to expand them to provide better images. The table then slides into the CT scanner, and you’ll be asked to hold your breath for about 15 seconds while the scan is done. You’ll likely have 2 scans: one while you’re lying on your back and one while you’re on your stomach or side.
Possible side effects and complications of CT virtual colonoscopy
There are usually few side effects after this test than after colonoscopy. You may feel bloated or have cramps because of the air in the colon and rectum, but this should go away once the air passes from the body. There’s a very small risk that inflating the colon with air could injure or puncture it, but this risk is thought to be much less than with colonoscopy. Like other types of CT scans, this test also exposes you to a small amount of radiation.
Flexible sigmoidoscopy
During flexible sigmoidoscopy test, the doctor looks at part of the colon and rectum with a sigmoidoscope (a flexible, lighted tube about the thickness of a finger with a small video camera on the end). It’s put in through the anus and into the rectum and moved into the lower part of the colon. Images from the scope are seen on a video screen.
Using the sigmoidoscope, your doctor can look at the inside of the rectum and part of the colon to detect (and possibly remove) any abnormalities. The sigmoidoscope is only about 60 centimeters (about 2 feet) long, so the doctor can see the entire rectum but less than half of the colon with this procedure.
This test is not widely used as a screening test for colorectal cancer in the United States.
Figure 6. Sigmoidoscopy. A thin, lighted tube is inserted through the anus and rectum and into the lower part of the colon to look for abnormal areas
Before the flexible sigmoidoscopy test
Be sure your doctor knows about any medicines you take. You might need to change how you take them before the test.
Your insides must be empty and clean so your doctor can see the lining of the sigmoid colon and rectum. You will get specific instructions to follow to clean them out. You may be asked to follow a special diet (such as drinking only clear liquids) or to use enemas or strong laxatives the day before the test to clean out your colon and rectum.
During the flexible sigmoidoscopy test
A sigmoidoscopy usually takes about 10 to 20 minutes. Most people don’t need to be sedated for this test, but this might be an option you can discuss with your doctor. Sedation may make the test less uncomfortable, but you’ll need some time to recover from it and you’ll need someone with you to take you home after the test.
You’ll probably be asked to lie on a table on your left side with your knees pulled up near your chest. Before the test, your doctor may put a gloved, lubricated finger into your rectum to examine it. For the test itself, the sigmoidoscope is first lubricated to make it easier to insert into the rectum. The scope may feel cold as it’s put in. Air will be pumped into the colon and rectum through the sigmoidoscope so the doctor can see the inner lining better.
If you are not sedated during the procedure, you might feel pressure and slight cramping in your lower belly. To ease discomfort and the urge to have a bowel movement, it may help to breathe deeply and slowly through your mouth. You’ll feel better after the test once the air leaves your colon.
If any polyps are found during the test, the doctor may remove them with a small instrument passed through the scope. The polyps will be looked at in the lab. If a pre-cancerous polyp (an adenoma) or colorectal cancer is found, you’ll need to have a colonoscopy later to look for polyps or cancer in the rest of the colon.
Possible complications and side effects of flexible sigmoidoscopy
Flexible sigmoidoscopy test may be uncomfortable because of the air put into the colon and rectum, but it should not be painful. Be sure to let your doctor know if you feel pain during the procedure. You might see a small amount of blood in your bowel movements for a day or 2 after the test. More serious bleeding and puncture of the colon or rectum are possible complications, but they are very uncommon.
References- Key Statistics for Colorectal Cancer. https://www.cancer.org/cancer/colon-rectal-cancer/about/key-statistics.html
- American Cancer Society: Cancer Facts and Figures 2022. American Cancer Society, 2022. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2022/2022-cancer-facts-and-figures.pdf
- Cancer Stat Facts: Colorectal Cancer. https://seer.cancer.gov/statfacts/html/colorect.html
- SEER Cancer Statistics Review (CSR) 1975-2017. https://seer.cancer.gov/archive/csr/1975_2017
- Imperiale TF, Wagner DR, Lin CY, Larkin GN, Rogge JD, Ransohoff DF. Results of screening colonoscopy among persons 40 to 49 years of age. N Engl J Med. 2002 Jun 6;346(23):1781-5. doi: 10.1056/NEJM200206063462304
- Imperiale TF, Gruber RN, Stump TE, Emmett TW, Monahan PO. Performance Characteristics of Fecal Immunochemical Tests for Colorectal Cancer and Advanced Adenomatous Polyps: A Systematic Review and Meta-analysis. Ann Intern Med. ;170:319–329. doi: 10.7326/M18-2390
- Colorectal Cancer Screening Tests. https://www.cancer.org/cancer/colon-rectal-cancer/detection-diagnosis-staging/screening-tests-used.html
- Azzouz LL, Sharma S. Physiology, Large Intestine. [Updated 2021 Aug 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507857
- Precup G, Vodnar DC. Gut Prevotella as a possible biomarker of diet and its eubiotic versus dysbiotic roles: a comprehensive literature review. Br J Nutr. 2019 Jul 28;122(2):131-140. doi: 10.1017/S0007114519000680
- Sulaiman, S., & Marciani, L. (2019). MRI of the Colon in the Pharmaceutical Field: The Future before us. Pharmaceutics, 11(4), 146. https://doi.org/10.3390/pharmaceutics11040146
- American Cancer Society Guideline for Colorectal Cancer Screening. https://www.cancer.org/cancer/colon-rectal-cancer/detection-diagnosis-staging/acs-recommendations.html
- Colorectal Cancer: Screening Final Recommendation Statement https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/colorectal-cancer-screening
- Clinician Summary of USPSTF Recommendation. Screening for Colorectal Cancer May 2021. https://www.uspreventiveservicestaskforce.org/home/getfilebytoken/xL4XwcPKXBfTWgY5ouzLzy