What is a corneal abrasion
A corneal abrasion is a superficial scratch or cut (abrasion) on the clear outer layer, the protective “window” at the front of your eye (cornea). Your cornea can be scratched by contact with dust, dirt, sand, wood shavings, metal particles, contact lenses or even the edge of a piece of paper. Corneal abrasions caused by plant matter (such as a pine needle) usually require special attention as they can cause a delayed inflammation inside the eye (iritis).
Injury (trauma) is the most common cause for corneal abrasions. The most common trauma causes are:
- Scratches from fingernails (human and animal).
- Foreign objects hitting the cornea (e.g., dirt, wood splinters, metal shavings, plants, tree branches, etc).
- Curling irons.
- Excessive rubbing of the eye.
- Overexposure to ultraviolet light.
- Arc welding light exposure.
- Over wearing of contact lenses.
- Ill-fitting contact lenses.
- Torn contact lenses.
- Makeup brushes.
- Paper cuts.
- Chemical burns.
- Irregular eyelashes rubbing the cornea or falling off into the eye.
- A foreign object that gets caught under the eyelid, which then irritates the cornea each time you blink.
Other causes of corneal abrasion include underlying eye conditions, such as:
- Inability to fully close the eyelids.
- Abnormalities of the lid position.
- Severe dry eye conditions.
- Severe, chronic blepharitis (inflamed eyelids).
Signs and symptoms of corneal abrasion include:
- Pain
- A gritty feeling in the eye
- Tearing
- Redness
- Sensitivity to the light
- Headache
Corneal abrasions are fairly common. Those who wear contact lenses or work in dusty, dirty, windy, or debris-laden areas are more likely to get a corneal abrasion.
In case of corneal abrasion, seek prompt medical attention. Left untreated, it could become infected and result in a corneal ulcer.
There are precautions that you can take to prevent getting a corneal abrasion. These include:
- Wearing protective eyewear for all conditions that might result in a corneal abrasion, such as working around the garden, working on grinding machines, etc.
- Being extra careful when using makeup brushes and curling irons.
- Taking excellent care of and using excellent hygiene with contact lenses.
- Never sleeping in contact lenses, regardless of manufacture notes.
See your doctor or ophthalmologist if:
- Persistent pain beyond the first day or pain that is increasing despite self-care.
- You suspect that a piece of metal, wood, or plant material hit the eye with high speed and may have penetrated the eye, not just irritated it.
- Any abrasion caused by chemicals, heat burn, makeup brushes, or plant materials.
- You suspect that a foreign object really is stuck in your eye.
- Recurrence of the pain and other symptoms days after the initial injury.
- Mucoid or pus-like discharge.
- No improvement with self-care after 24 hours.
- Progressive vision loss.
- You have symptoms of corneal ulcers or an infection.
- You have been diagnosed with corneal ulcer and your symptoms become worse after treatment.
- Your vision is affected.
- You develop eye pain that is severe or becoming worse.
- Your eyelids or the skin around your eyes becomes swollen or red.
- You have a headache in addition to your other symptoms.
Corneal abrasion home treatment
If you have a corneal abrasion, you need to see an eye care professional for an evaluation. Most corneal abrasions heal completely without leaving any scars and have no permanent effect on vision. However, a deeper abrasion (scratch), especially in the center of the cornea, may leave a faint scar that can sometimes cause blurring of vision and sensitivity to glare.
Immediate steps you can take for a corneal abrasion are to:
- Rinse your eye with clean water or a saline solution. You can use an eyecup or a small, clean drinking glass positioned with its rim resting on the bone at the base of your eye socket. If you have quick access to a work site eye-rinse station, use it. Rinsing the eye may wash out a foreign object.
- Blink several times. This may remove small particles.
- Pull the upper eyelid over the lower eyelid. This may cause your eye to tear, which may help wash out the particle. Or it may cause the lashes of your lower eyelid to brush away an object from under your upper eyelid.
Use the following pointers to avoid making the injury worse:
- Don’t try to remove an object that is embedded in your eyeball or makes it difficult to close your eye.
- Don’t rub your eye after an injury.
- Don’t touch your eyeball with cotton swabs, tweezers or other instruments.
- If you use contact lenses, don’t wear them while your eye is healing. Contact lens wearers should always have a back-up pair of glasses for when contact lenses shouldn’t be worn.
- Using artificial tears to bathe the eye.
- Using sunglasses to reduce light sensitivity.
Corneal abrasion healing time
Most corneal abrasions are superficial and heal spontaneously without treatment in a day or two. Larger corneal abrasions are treated with antibiotic drops or ointment to protect against infection while new cells grow to replace the ones that were damaged. Sometimes, depending on the size of the corneal abrasion, a patch is placed over the closed lid. A patch helps decrease pain and make your cornea heal faster. An eye should not be patched continuously for more than 24 hours. The patch should be removed at least daily and the antibiotic drop or ointment put in the eye again.
How fast do corneal abrasions heal?
In order for the corneal abrasion to heal a new superficial layer- the epithelium should grow and cover the defect. Therefore, corneal healing time depends on the size of the corneal abrasion and the overall health of the cornea. An abrasion on a healthy cornea should heal in 1-5 days.
Why are corneal abrasions so painful?
The cornea is very sensitive due to numerous nerve terminations that transmit the sensation of pain to the brain in order to help us recognize that something foreign is in the eye before it damages the surface of the eye. This is why having a corneal abrasion is a very painful experience.
How is dye used to detect a corneal abrasion?
A yellow dye called fluorescein is placed on the surface of the eye. The dye fills in the corneal defect and will light up green (will fluoresce) in a cobalt blue light to show where the defect is.
What is a corneal erosion?
The new epithelium that grows when the abrasion heals sometimes is not tightly attached to the layers below and sloughs off in the area of the original abrasion after the defect has healed. Corneal erosions can occur with little or no trauma to the eye. Corneal erosions often occur upon awakening. Corneal erosions are often as painful as the original abrasion. If you experience pain after a corneal abrasion has healed you should notify your ophthalmologist.
What is recurrent corneal abrasion?
If the corneal abrasion heals and then suddenly recurs days later, this may be a sign of recurrent corneal erosion, which requires specific medical care by an eye care professional. Use of topical anesthetic solutions is only for purposes of diagnosis. Using these drops more than once or twice is dangerous because it slows healing and could lead to more serious conditions.
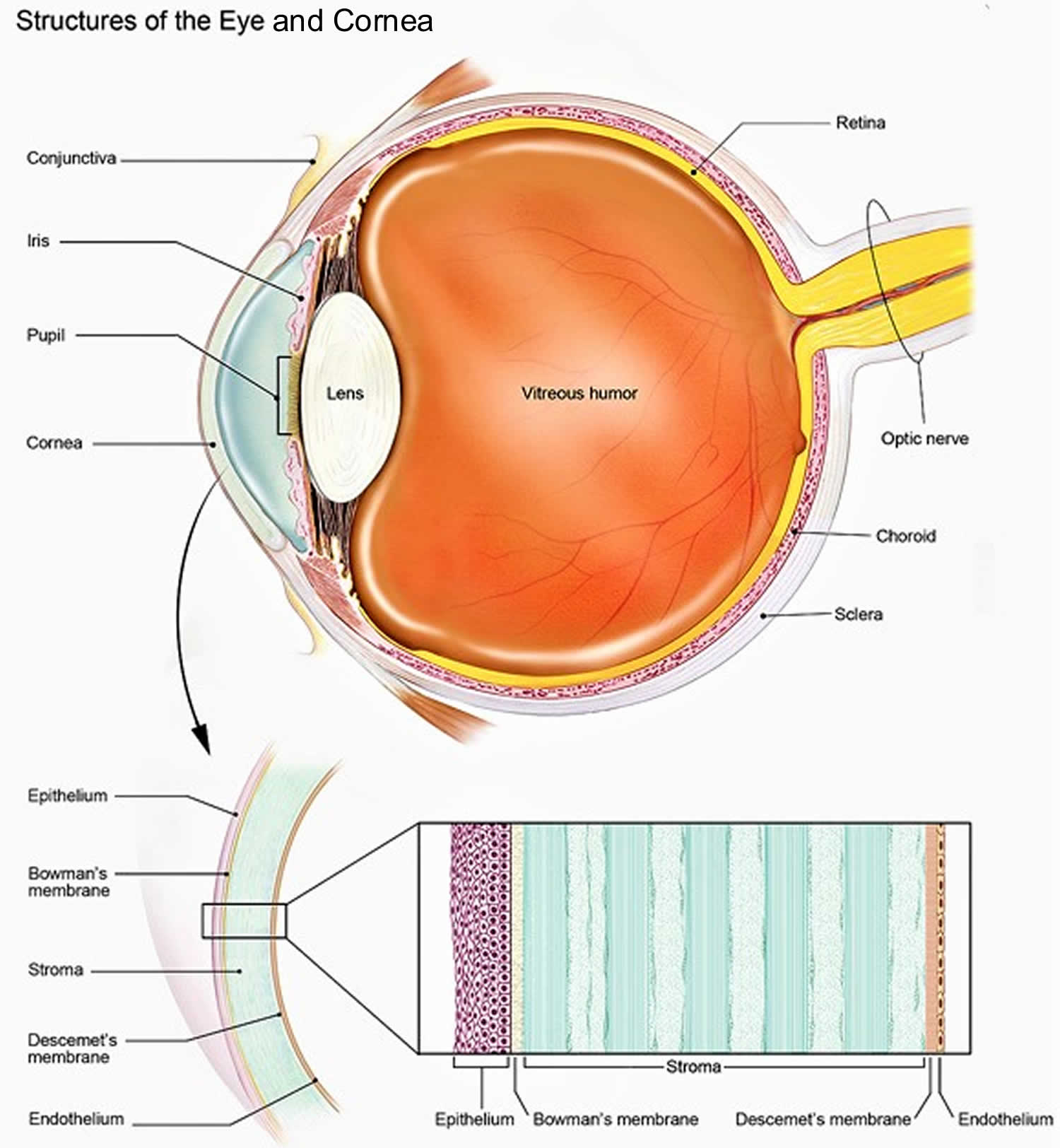
What is the cornea?
The cornea is the eye’s outermost layer. It is the clear, dome shaped surface that covers the front of the eye. The cornea plays an important role in focusing your vision.
What are the parts of the cornea?
Although the cornea may look clear and seem to lack substance, it is a highly organized tissue. Unlike most tissues in the body, the cornea contains no blood vessels to nourish or protect it against infection. Instead, the cornea receives its nourishment from tears and the aqueous humor (a fluid in the front part of the eye that lies behind the cornea).
The tissues of the cornea are arranged in three basic layers, with two thinner layers, or membranes, between them. Each of these five layers has an important function. These layers are (Figure 2):
Epithelium
The epithelium is the cornea’s outermost layer. Its primary functions are to:
- block the passage into the eye of foreign material, such as dust, water, and bacteria; and
- provide a smooth surface to absorb oxygen and nutrients from tears, which are then distributed to the other layers of the cornea.
The epithelium is filled with thousands of tiny nerve endings, which is why your eye may hurt when it is rubbed or scratched. The part of the epithelium that epithelial cells anchor and organize themselves to is called the basement membrane.
Bowman’s membrane
The next layer behind the basement membrane of the epithelium is a transparent film of tissue called Bowman’s layer, composed of protein fibers called collagen. If injured, Bowman’s layer can form a scar as it heals. If these scars are large and centrally located, they may cause vision loss.
Stroma
Behind Bowman’s layer is the stroma, which is the thickest layer of the cornea. It is composed primarily of water and collagen. Collagen gives the cornea its strength, elasticity, and form. The unique shape, arrangement, and spacing of collagen proteins are essential in producing the cornea’s light-conducting transparency.
Descemet’s Membrane
Behind the stroma is Descemet’s membrane, a thin but strong film of tissue that serves as a protective barrier against infection and injuries. Descemet’s membrane is composed of collagen fibers that are different from those of the stroma, and are made by cells in the endothelial layer of the cornea (see above). Descemet’s membrane repairs itself easily after injury.
Endothelium
The endothelium is the thin, innermost layer of the cornea. Endothelial cells are important in keeping the cornea clear. Normally, fluid leaks slowly from inside the eye into the stroma. The endothelium’s primary task is to pump this excess fluid out of the stroma. Without this pumping action, the stroma would swell with water and become thick and opaque.
In a healthy eye, a perfect balance is maintained between the fluid moving into the cornea and the fluid pumping out of the cornea. Unlike the cells in Descemet’s membrane, endothelial cells that have been destroyed by disease or trauma are not repaired or replaced by the body.
What does the cornea do?
The cornea acts as a barrier against dirt, germs, and other particles that can harm the eye. The cornea shares this protective task with the eyelids and eye sockets, tears, and the sclera (white part of the eye). The cornea also plays a key role in vision by helping focus the light that comes into the eye. The cornea is responsible for 65-75 percent of the eye’s total focusing power.
The cornea and lens of the eye are built to focus light on the retina, which is the light-sensitive tissue at the back of the eye. When light strikes the cornea, it bends—or refracts—the incoming light onto the lens. The lens refocuses that light onto the retina, which starts the translation of light into vision. The retina converts light into electrical impulses that travel through the optic nerve to the brain, which interprets them as images.
The refractive process the eye uses is similar to the way a camera takes a picture. The cornea and lens in the eye act as the camera lens. The retina is like the film (in older cameras), or the image sensor (in digital cameras). If the image is not focused properly, the retina makes a blurry image.
The cornea also serves as a filter that screens out damaging ultraviolet (UV) light from the sun. Without this protection, the lens and the retina would be exposed to injury from UV rays.
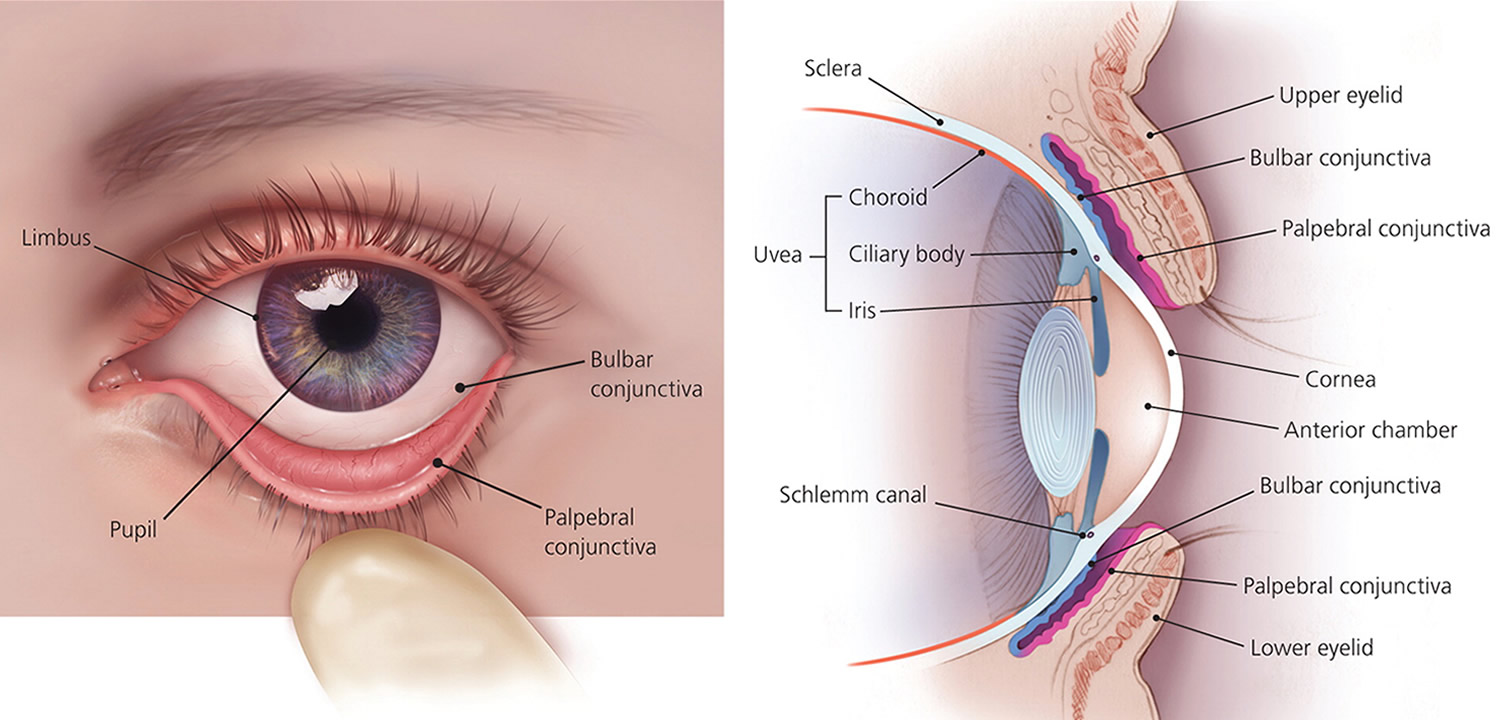
Figure 1. Eye anatomy
Corneal abrasion vs Corneal ulcer
A corneal ulcer is an open sore on the cornea. A corneal ulcer is often caused by an infection, but severe dry eye or other eye disorders can cause it too.
Corneal ulcer causes
A corneal ulcer usually occurs after corneal trauma or with an irregular ocular surface, which allows bacteria, fungus, or parasites to enter the cornea and cause an infection with inflammation.
Corneal ulcers are most commonly caused by an infection with bacteria, viruses, fungi, or a parasite.
- Acanthamoeba keratitis occurs in contact lens users. It is more likely to happen in people who make their own homemade cleaning solutions.
- Fungal keratitis can occur after a corneal injury involving plant material. It may also occur in people with a suppressed immune system.
- Herpes simplex keratitis is a serious viral infection. It may cause repeated attacks that are triggered by stress, exposure to sunlight, or any condition that lowers the immune response.
Corneal ulcers or infections may also be caused by:
- Eyelids that do not close all the way, such as with Bell palsy
- Foreign bodies in the eye
- Scratches (abrasions) on the eye surface
- Severely dry eyes
- Severe allergic eye disease
- Various inflammatory disorders
Wearing contact lenses, such as soft contacts that are left in overnight, may cause a corneal ulcer.
Risk factors for corneal ulcer
Trauma from a foreign body (including contact lenses), severe dry eyes, or eyelid disease can predispose patients to corneal infections. Contact lens overuse or poor contact lens hygiene also puts a patient at higher risk for such infections due to the bacteria and other organisms that can grow on the contact lenses, cases, and in re-used contact lens solution.
Corneal ulcer prevention
Things you can do to prevent corneal ulcer include:
- Wash your hands well when handling your contact lenses.
- Avoid wearing contact lenses overnight.
- Get prompt treatment for an eye infection to prevent ulcers from forming.
Corneal ulcer symptoms
Symptoms of infection or corneal ulcers include:
- Blurry or hazy vision
- Eye that appears red or bloodshot
- Itching and discharge
- Sensitivity to light (photophobia)
- Very painful and watery eyes
- White patch on the cornea that you may or may not be able to see when looking in the mirror
- The feeling of having something in your eye
- Pus or other discharge
- Swelling of the eyelids
See your ophthalmologist immediately if you think you have a corneal ulcer or have any eye symptoms that concern you. Corneal ulcers can badly and permanently damage your vision and even cause blindness if they are not treated.
Corneal ulcer possible complications
Untreated corneal ulcers and infections may lead to:
- Loss of the eye (rare)
- Severe vision loss
- Scars on the cornea
Corneal ulcer treatment
Treatment for corneal ulcers and infections depends on the cause. Treatment should be started as soon as possible to prevent scarring of the cornea.
If the exact cause is not known, you may be given antibiotic drops that work against many kinds of bacteria.
Once the exact cause is known, you may be given drops that treat bacteria, herpes, other viruses, or a fungus. In the case of suspected fungal or parasitic infection, a patient may receive special antibiotics specifically targeted at these organisms.
Corticosteroid eye drops may be used to reduce swelling and inflammation in certain conditions.
After the infection is resolved, residual corneal scarring or thinning can occur, and occasionally corneal transplantation may be recommended to restore vision. Early treatment may help reduce the risk of complications. Frequent visits to an eye care professional may be necessary for several months to eliminate the problem.
Your doctor may also recommend that you:
- Avoid eye makeup
- DO NOT wear contact lenses at all, or do not wear them at night
- Take pain medicines
- Wear protective glasses
Corneal ulcer prognosis
Many people recover completely and have only a minor change in vision. However, a corneal ulcer or infection can cause long-term damage and affect vision.
Corneal abrasion symptoms
Although it is very difficult to see a corneal abrasion with the naked eye, you have to be suspicious of this if you have experienced any of the causes of trauma mentioned above. The most common symptom of a corneal erosion or abrasion is pain, often like there is something in your eye. You also may experience eye redness, light sensitivity, blurred vision, and tearing.
Along with that is the unrelenting painful feeling that something is in your eye that just won’t wash out, plus:
- Lots of watery tearing.
- Sensitivity to light (especially bright light).
- Blurry vision.
- Redness of the eye.
- Spasm of the muscles surrounding the eye resulting in squinting.
These symptoms may not necessarily mean that you have a corneal erosion or abrasion. However, if you experience one or more of these symptoms, contact your doctor or ophthalmologist for a complete exam.
Corneal abrasion diagnosis
Detecting a corneal abrasion requires the use of fluorescein dye, which highlights the injured tissue during an eye exam. If present, underlying corneal disease also can be diagnosed during an eye exam. Special imaging or other testing is usually not necessary.
How to treat corneal abrasion
A corneal erosion or abrasion typically heals quickly, often within a few days to a week. It is important not to rub your eye during the healing process as the new epithelial cells are fragile and can easily be rubbed off. If bacteria get into the tissues under the protective corneal epithelium, infection or a corneal ulcer can result. These complications can be very serious and cause loss of vision. Proper care by you and your ophthalmologist are necessary to help prevent serious consequences.
After assurance that there is nothing more serious than an abrasion, your ophthalmologist will most likely tightly patch your eye for a day or two after instilling an anesthetic drop and antibiotic ointment. Anesthetic drops can relieve pain and facilitate examination but may keep the eye from healing properly if used repeatedly. Anesthetic drops should never be used as a treatment. Very tight patching is indicated for those corneal abrasions that are felt to be essentially clean. Otherwise, patching may not be done. This facilitates healing of the damaged corneal epithelium and also reduces pain by preventing the blinking eyelid from irritating the affected area. Since both eyes move together and the eye is most painful when it moves, it is often helpful to rest the other eye as well.
Your doctor may also clean and sweep (debride) the area of the abrasion to remove any possible dirty or contaminated tissue. If there is an underlying basis for the abrasion, care for this is needed to prevent recurrence. If the abrasion was contact-lens–related, you may be required to be reevaluated regarding your contact lenses as to fit and type.
If the problem is recurrent erosion, your doctor will begin specific treatment for that condition. Long after an abrasion has healed it may spontaneously recur, and is often noticeable upon awakening in the morning. Recurrent corneal erosions often require repeat patching or the use of ointments at bedtime. Sometimes a soft or bandage-type contact lens is used to facilitate healing. Occasionally, treatment of the corneal surface with minor surgery is necessary to prevent recurrences.