Coronary steal syndrome
Coronary steal syndrome also known as coronary steal, coronary steal phenomenon or cardiac steal syndrome, refers to myocardial ischemia caused by myocardial blood flow redistribution (“steal”) away from poorly perfused (flow restricted) to well-perfused areas, leading to ischemia. Coronary steal is conventionally defined as a fall in absolute coronary perfusion (ml/min/g) of collateralized myocardium after coronary arteriolar vasodilation, usually after IV administration of dipyridamole 1. Coronary steal has been studied experimentally 2, demonstrated in humans 3 and occurs in 10 to 30 percent of patients with coronary artery disease undergoing dipyridamole perfusion imaging, as evidenced by chest pain, ECG changes, and abnormal perfusion scans 4. In clinical setting coronary artery steal is an important, useful diagnostic sign seen during dipyridamole perfusion imaging that indicates severe coronary artery disease and viable myocardium, most commonly associated with significant collateral supply, occasionally without collaterals and with abnormal perfusion images; it may occur rarely with subendocardial small vessel dysautonomia in the absence of coronaryartery disease 1. Myocardial ischemia due to coronary steal is generally believed to be manifested clinically by measuring a pressure drop proximal to the collateral origin during adenosine induced hyperemic flow. A quantitative signature of coronary steal may help diagnose the early symptoms of myocardial ischemia and triple vessel disease.
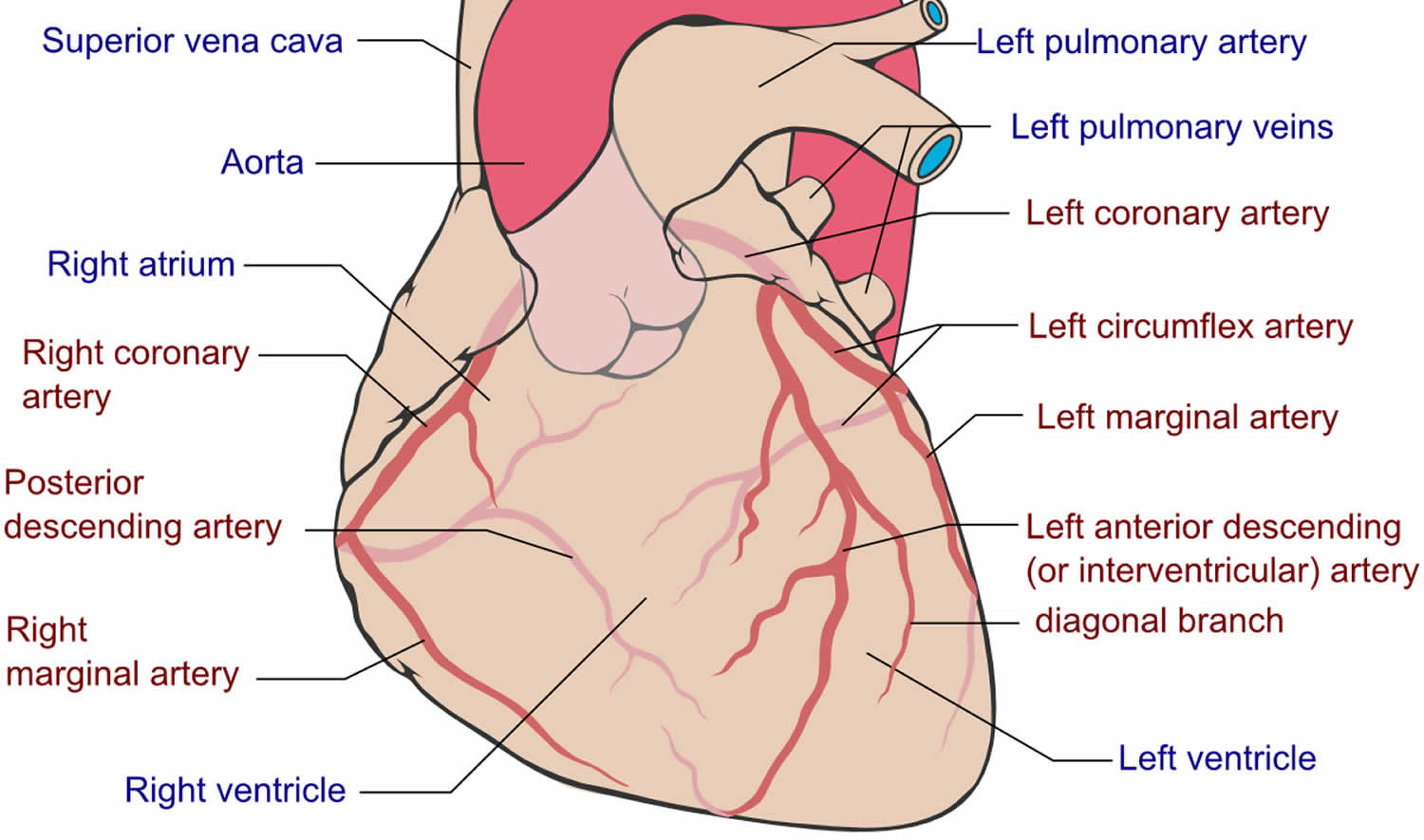
Coronary steal occurs when dilation of one coronary artery (e.g., during exercise or vasodilator therapy) “steals” blood away from those parts of the heart that is already maximally dilated because of the presence of significant coronary stenosis (partial or complete blockage in the lumen of a coronary artery). Coronary steal happens as a result of the narrowed coronary arteries being always maximally dilated to compensate for the decreased upstream blood supply. Thus, dilating the resistance vessels in the coronary circulation causes blood to be shunted away from the coronary vessels supplying the ischemic zones, creating more ischemia. Figure 2 shows a left main coronary artery with a moderate stenosis, which bifurcates to a left anterior descending artery (LAD) with a significant proximal stenosis and a circumflex artery that is free of disease. The vascular bed supplied by the diseased left anterior descending (LAD) artery is likely maximally vasodilated with minimal resistances due to activation of autoregulatory mechanisms, to keep the myocardial flow to this bed constant. This is because the combined effect of the left main stenosis and left anterior descending artery stenosis decrease the perfusion pressure distal to the left anterior descending artery stenosis significantly, and therefore the blood supply to the distal left anterior descending artery vasculature would be reduced if this distal left anterior descending artery vasculature had not been maximally vasodilated. On the other hand, the moderate left main stenosis may not alter substantially the perfusion pressure to the circumflex, and therefore a normal blood flow to the distal circumflex vasculature may be maintained in the presence of normal resistances (no need for vasodilation in the vasculature distal to the circumflex).
In this scenario, in the presence of vasodilatory stimulus such as physical exercise or a vasodilatory medication (e.g., dobutamine, dipyridamole), the resistances of the vascular bed of the circumflex artery would decrease and the respective blood flow would increase. The resistance in the left anterior descending artery territory could not decrease further, as this vascular bed is already at maximal vasodilation. However, the increased blood flow and decreased resistance in the circumflex territory would decrease the perfusion pressure of the circumflex and left anterior descending artery (P2) distal to the left main stenosis, as the overall resistance of the vascular bed supplied by the left main would decrease (due to the vasodilation of the circumflex vascular bed mediated by the autoregulatory mechanisms due to physical exercise of drugs with vasodilatory effects). This reduction in the perfusion pressure of left anterior descending artery (P2) would induce a decrease in the perfusion pressure of the left anterior descending artery vascular bed distal to the left anterior descending artery stenosis (P3). This would inevitably lead to a further decrease of the blood flow to the distal left anterior descending artery vascular bed, as the perfusion pressure to the already maximally vasodilated vascular bed falls and further vasodilation is not possible. Therefore, in this scenario, there is redistribution of blood flow with an increase of flow in the circumflex territory, coupled by an erroneous decrease of the blood flow in the left anterior descending artery vascular bed, resulting in a deterioration of ischemia and hypoxia of the left anterior descending artery vascular bed.
Figure 1. Coronary artery anatomy
Figure 2. Coronary steal syndrome
Abbreviations: LC = left coronary artery; LAD = left anterior descending artery; LC = left main coronary artery; CFX = left circumflex artery; R1 and R2 = stenosis
Footnotes: The pressure distal to the left anterior descending artery (LAD) lesion (P3) divided by resistance of the vasculature supplied by the left anterior descending artery (LAD) (RLAD) determines blood flow in the LAD-supplied distal vascular beds (FLAD). The vascular bed supplied by the LAD is maximally dilated (i.e., at minimal resistance, RLAD) due to autoregulation in response to the large reduction in pressure distal to the LAD lesion (P3) caused by the combined left main coronary artery (LC) and left anterior descending artery (LAD) stenotic lesions (R1 and R2, respectively). Blood flow in the left circumflex artery (CFX)-supplied vascular beds (FC) is determined by P2 divided by the resistance of the distal vascular beds supplied by the circumflex artery (RC). If the left main coronary artery (LC) lesion does not reduce P2 to a value below the autoregulatory range of the left circumflex artery (CFX)-supplied vascular beds, then these beds will not be maximally dilated and therefore can still decrease their resistance (RC) in response to increased metabolic demand by the heart or to vasodilator drugs.
In the above example, vasodilator stimuli (e.g., exercise or drugs) will decrease resistance (RC) and increase vascular beds (FC). When this increase in left circumflex artery (CFX) blood flow occurs, the increased flow across R1 supplying the increase in vascular beds (FC) will further decrease P2 because the pressure gradient across R1 (P1 – P2) is proportionate to the change in flow. (Note: P1 will remain relatively constant because it is determined by aortic pressure; therefore, P2 decreases as the pressure gradient increases.) The reduction in P2 will cause P3 to decrease, thereby reducing the perfusion pressure to the LAD vascular beds. When this occurs, FLAD will decrease. Remember that RLAD is already minimal (i.e., maximally dilated) due to the low P3 and therefore is incapable of dilating further in response to a vasodilator stimulus. The net result is that left circumflex artery (CFX) blood flow increases while left anterior descending artery (LAD) blood flow decreases (i.e., vascular steal). This redistribution of flow leads to ischemia and hypoxia (especially during augmented oxygen demand) in the myocardium supplied by the left anterior descending artery (LAD).
Coronary steal syndrome causes
Coronary steal is a phenomenon wherein during a situation where blood flow favors the more patent coronary artery compared to the one with stenosis. During stress tests, where the heart is subjected to increased demand, there is a proportionate increase in blood flow to supply the demand from the heart. Since fluid flows more easily down the path of least resistance, the coronary artery which is more patent, i.e. open, would get the bulk of the blood flow, causing the blood to be “stolen” from the less patent, more stenotic arteries or arterioles. This is the basis for the nuclear stress tests where images are taken before and after stress and areas of lower tracer uptake are considered positive for stenosis.
Most cases of coronary steal syndrome are associated with coronary arteriovenous fistulas in older patients with no coronary artery disease, which present as stable angina although unstable angina and arrhythmias have also been rarely observed 5. Coronary arteriovenous fistula can be congenital or acquired, 90% being congenital 6. Persistence of embryonic sinusoids that perfuse primitive myocardium may lead to a fistulous connection between the coronary arteries and cardiac chambers (coronary cameral fistula) 7. Failure to the obliteration of embryonic connection between coronary arteries and other mediastinal vessels (bronchial, pericardial, or mediastinal arteries) or superior vena cava may result in the coronary arteriovenous fistula 8. The acquired coronary arteriovenous fistulae, although rare, can result from cardiac trauma, procedures (coronary stent placement, coronary artery bypass grafting, chest irradiation), or cardiac disease (myocardial infarction, and coronary vasculitis) 9.
Risk factors for coronary artery disease include:
- Age. Getting older increases your risk of damaged and narrowed arteries.
- Sex. Men are generally at greater risk of coronary artery disease. However, the risk for women increases after menopause.
- Family history. A family history of heart disease is associated with a higher risk of coronary artery disease, especially if a close relative developed heart disease at an early age. Your risk is highest if your father or a brother was diagnosed with heart disease before age 55 or if your mother or a sister developed it before age 65.
- Smoking. People who smoke have a significantly increased risk of heart disease. Breathing in secondhand smoke also increases a person’s risk of coronary artery disease.
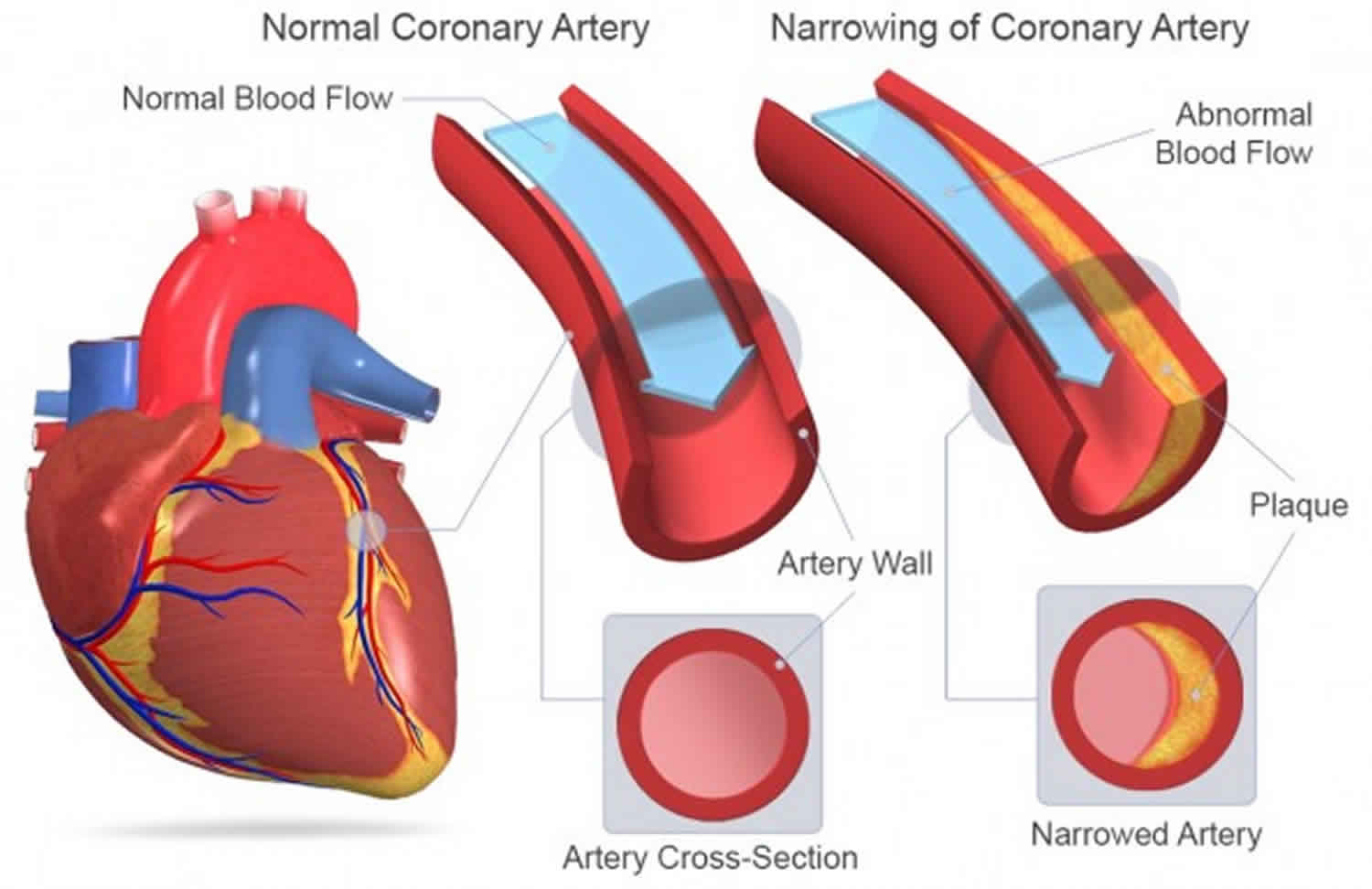
- High blood pressure. Uncontrolled high blood pressure can result in hardening and thickening of your arteries, narrowing the channel through which blood can flow.
- High blood cholesterol levels. High levels of cholesterol in your blood can increase the risk of formation of plaque and atherosclerosis. High cholesterol can be caused by a high level of low-density lipoprotein (LDL) cholesterol, known as the “bad” cholesterol. A low level of high-density lipoprotein (HDL) cholesterol, known as the “good” cholesterol, can also contribute to the development of atherosclerosis.
- Diabetes. Diabetes is associated with an increased risk of coronary artery disease. Type 2 diabetes and coronary artery disease share similar risk factors, such as obesity and high blood pressure.
- Overweight or obesity. Excess weight typically worsens other risk factors.
- Physical inactivity. Lack of exercise also is associated with coronary artery disease and some of its risk factors, as well.
- High stress. Unrelieved stress in your life may damage your arteries as well as worsen other risk factors for coronary artery disease.
- Unhealthy diet. Eating too much food that has high amounts of saturated fat, trans fat, salt and sugar can increase your risk of coronary artery disease.
Risk factors often occur together and one may trigger another. For instance, obesity can lead to type 2 diabetes and high blood pressure. When grouped together, certain risk factors make you even more likely to develop coronary artery disease. For example, metabolic syndrome — a cluster of conditions that includes high blood pressure; high triglycerides; low HDL, or “good,” cholesterol; high insulin levels and excess body fat around the waist — increases the risk of coronary artery disease.
Sometimes coronary artery disease develops without any classic risk factors. Researchers are studying other possible risk factors, including:
- Sleep apnea. This disorder causes you to repeatedly stop and start breathing while you’re sleeping. Sudden drops in blood oxygen levels that occur during sleep apnea increase blood pressure and strain the cardiovascular system, possibly leading to coronary artery disease.
- High-sensitivity C-reactive protein (hs-CRP). This protein appears in higher-than-normal amounts when there’s inflammation somewhere in your body. High hs-CRP levels may be a risk factor for heart disease. It’s thought that as coronary arteries narrow, you’ll have more hs-CRP in your blood.
- High triglycerides. This is a type of fat (lipid) in your blood. High levels may raise the risk of coronary artery disease, especially for women.
- Homocysteine. Homocysteine is an amino acid your body uses to make protein and to build and maintain tissue. But high levels of homocysteine may increase your risk of coronary artery disease.
- Preeclampsia. This condition that can develop in women during pregnancy causes high blood pressure and a higher amount of protein in urine. It can lead to a higher risk of heart disease later in life.
- Alcohol use. Heavy alcohol use can lead to heart muscle damage. It can also worsen other risk factors of coronary artery disease.
- Autoimmune diseases. People who have conditions such as rheumatoid arthritis and lupus (and other inflammatory conditions) have an increased risk of atherosclerosis.
Coronary steal syndrome symptoms
Clinically, coronary steal is manifested by chest pain (angina) and ST depression on ECG after IV dipyridamole and it is usually a sign of severe coronary artery disease with viable myocardium.
Coronary arteriovenous fistula signs and symptoms:
A small coronary arteriovenous fistula that is not jeopardizing myocardial blood supply can remain asymptomatic. However, patients with a large fistula can present with ischemic symptoms like angina from coronary steal phenomenon. Left to right shunt may also cause right ventricular volume overload. They can manifest with features of right-sided heart failure like dyspnea, extremity swelling, orthopnea, and syncope. The clinician should suspect coronary arteriovenous fistula in patients with unexplained heart failure, with a history of chest trauma irradiation, myocardial infarction, or cardiac procedures. On examination, signs of congestive heart failure like raised jugular venous pressure, positive hepatojugular reflux, pedal edema, and pleural effusion can be present. Chest auscultation may reveal continuous murmur from increased flow in the large fistula and collaterals. A loud S2 and early diastolic murmur in the pulmonary area can point to pulmonary hypertension.
Coronary artery disease signs and symptoms:
- Chest pain (angina). You may feel pressure or tightness in your chest, as if someone were standing on your chest. This pain, called angina, usually occurs on the middle or left side of the chest. Angina is generally triggered by physical or emotional stress. The pain usually goes away within minutes after stopping the stressful activity. In some people, especially women, the pain may be brief or sharp and felt in the neck, arm or back.
- Shortness of breath. If your heart can’t pump enough blood to meet your body’s needs, you may develop shortness of breath or extreme fatigue with activity.
- Heart attack. A completely blocked coronary artery will cause a heart attack. The classic signs and symptoms of a heart attack include crushing pressure in your chest and pain in your shoulder or arm, sometimes with shortness of breath and sweating.
Women are somewhat more likely than men are to have less typical signs and symptoms of a heart attack, such as neck or jaw pain. And they may have other symptoms such as shortness of breath, fatigue and nausea.
Sometimes a heart attack occurs without any apparent signs or symptoms.
Coronary steal syndrome diagnosis
There are limited noninvasive measurements used for the detection of coronary artery in human hearts, mostly using positron emission tomography (PET). Heart ischemia is provoked by increasing myocardial oxygen demand and possibly by reducing supply (e.g. via exercise, or the use of dobutamine). Alternatively, vasodilators such as dipyridamole or adenosine are used to cause myocardial blood flow redistribution (steal) via collaterals from poorly perfused (flow restricted) to well-perfused areas, leading to ischemia. Systemic hypotension that occurs due to systemic vasodilatation exacerbates the steal phenomenon.
Your doctor may order other diagnostic tests including:
- Electrocardiogram (ECG). An electrocardiogram records electrical signals as they travel through your heart. An ECG can often reveal evidence of a previous heart attack or one that’s in progress.
- Echocardiogram. An echocardiogram uses sound waves to produce images of your heart. During an echocardiogram, your doctor can determine whether all parts of the heart wall are contributing normally to your heart’s pumping activity. Parts that move weakly may have been damaged during a heart attack or be receiving too little oxygen. This may be a sign of coronary artery disease or other conditions.
- Exercise stress test. If your signs and symptoms occur most often during exercise, your doctor may ask you to walk on a treadmill or ride a stationary bike during an ECG. Sometimes, an echocardiogram is also done while you do these exercises. This is called a stress echo. In some cases, medication to stimulate your heart may be used instead of exercise.
- Nuclear stress test. This test is similar to an exercise stress test but adds images to the ECG recordings. It measures blood flow to your heart muscle at rest and during stress. A tracer is injected into your bloodstream, and special cameras can detect areas in your heart that receive less blood flow.
- Cardiac catheterization and angiogram. During cardiac catheterization, a doctor gently inserts a catheter into an artery or vein in your groin, neck or arm and up to your heart. X-rays are used to guide the catheter to the correct position. Sometimes, dye is injected through the catheter. The dye helps blood vessels show up better on the images and outlines any blockages. If you have a blockage that requires treatment, a balloon can be pushed through the catheter and inflated to improve the blood flow in your coronary arteries. A mesh tube (stent) is typically used to keep the dilated artery open.
- Cardiac CT scan. A CT scan of the heart can help your doctor see calcium deposits in your arteries that can narrow the arteries. If a substantial amount of calcium is discovered, coronary artery disease may be likely.
- A CT coronary angiogram, in which you receive a contrast dye that is given by IV during a CT scan, can produce detailed images of your heart arteries.
Coronary steal syndrome treatment
For coronary arteriovenous fistula, spontaneous closure is reported in 1% to 2% of cases 8. Small asymptomatic fistulas do not require treatment and are monitored for complications. American College of Cardiology and American Heart Association guidelines recommend closure of fistulas greater than 250 mm irrespective of symptoms, all symptomatic fistula regardless of size, including myocardial ischemia, arrhythmia, ventricular dysfunction, and endarteritis 10.
The closure of the fistula can be achieved either from a percutaneous transcatheter approach or surgically via sternotomy 8. Indications for endocardial or epicardial surgical ligation are: large fistula with high blood flow, tortuous and aneurysmal fistula, multiple communications and drainage sites, and need for a simultaneous distal bypass. Patients with proximal fistula origin, single drain site, non-tortuous fistula, simple and easily accessible fistula are suitable candidates for occlusion with coils, detachable balloons, vascular plugs, and duct occluders 8.
Treatment for coronary artery disease usually involves lifestyle changes and, if necessary, drugs and certain medical procedures.
Lifestyle changes
Making a commitment to the following healthy lifestyle changes can go a long way toward promoting healthier arteries:
- Quit smoking.
- Eat healthy foods.
- Exercise regularly.
- Lose excess weight.
- Reduce stress.
Drugs
Various drugs can be used to treat coronary artery disease, including:
- Cholesterol-modifying medications. These medications reduce (or modify) the primary material that deposits on the coronary arteries. As a result, cholesterol levels — especially low-density lipoprotein (LDL, or the “bad”) cholesterol — decrease. Your doctor can choose from a range of medications, including statins, niacin, fibrates and bile acid sequestrants.
- Aspirin. Your doctor may recommend taking a daily aspirin or other blood thinner. This can reduce the tendency of your blood to clot, which may help prevent obstruction of your coronary arteries. If you’ve had a heart attack, aspirin can help prevent future attacks. But aspirin can be dangerous if you have a bleeding disorder or you’re already taking another blood thinner, so ask your doctor before taking it.
- Beta blockers. These drugs slow your heart rate and decrease your blood pressure, which decreases your heart’s demand for oxygen. If you’ve had a heart attack, beta blockers reduce the risk of future attacks.
- Calcium channel blockers. These drugs may be used with beta blockers if beta blockers alone aren’t effective or instead of beta blockers if you’re not able to take them. These drugs can help improve symptoms of chest pain.
- Ranolazine. This medication may help people with chest pain (angina). It may be prescribed with a beta blocker or instead of a beta blocker if you can’t take it.
- Nitroglycerin. Nitroglycerin tablets, sprays and patches can control chest pain by temporarily dilating your coronary arteries and reducing your heart’s demand for blood.
- Angiotensin-converting enzyme (ACE) inhibitors and angiotensin 2 receptor blockers (ARBs). These similar drugs decrease blood pressure and may help prevent progression of coronary artery disease.
Procedures to restore and improve blood flow
Sometimes more aggressive treatment is needed. Here are some options:
- Angioplasty and stent placement (percutaneous coronary revascularization): Your doctor inserts a long, thin tube (catheter) into the narrowed part of your artery. A wire with a deflated balloon is passed through the catheter to the narrowed area. The balloon is then inflated, compressing the deposits against your artery walls. A stent is often left in the artery to help keep the artery open. Most stents slowly release medication to help keep the arteries open.
- Coronary artery bypass surgery (CABG): A surgeon creates a graft to bypass blocked coronary arteries using a vessel from another part of your body. This allows blood to flow around the blocked or narrowed coronary artery. Because this requires open-heart surgery, it’s most often reserved for people who have multiple narrowed coronary arteries.
- Coronary Steal. Is It Clinically Important? Chest Volume 96, ISSUE 2, P227-229, August 01, 1989 https://doi.org/10.1378/chest.96.2.227
- The collateral circulation of the heart. Prog Cardiovasc Dis. 1988; 31: 57-77
- Demer LL, Goldstein R, Mullani N, Kirkeeide R, Smalling R, Nishikawa A et al. Coronary steal by noninvasive PET identifies collateralized myocardium. J Nucl Med. 1986; 27: 977
- Chambers CE, Brown KA. Dipyridamole-induced ST segment depression during thallium-201 imaging in patients with coronary artery disease: angiographic and hemodynamic determinants. J Am Coll Cardiol. 1988; 12: 37-41
- Ahmed MF, Mubin A, Syed R, Mahmood AK, Sahni S. Multivessel Coronary Artery Fistula Presenting as Coronary Steal Syndrome Leading to Cardiac Arrest. Cureus. 2020;12(5):e8358. Published 2020 May 30. doi:10.7759/cureus.8358 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7325350
- Challoumas D, Pericleous A, Dimitrakaki IA, Danelatos C, Dimitrakakis G. Coronary arteriovenous fistulae: a review. Int. J. Angiol. 2014 Mar;23(1):1-10.
- Ogden JA. Congenital anomalies of the coronary arteries. Am. J. Cardiol. 1970 Apr;25(4):474-9.
- Yun G, Nam TH, Chun EJ. Coronary Artery Fistulas: Pathophysiology, Imaging Findings, and Management. Radiographics. 2018 May-Jun;38(3):688-703.
- Mangukia CV. Coronary artery fistula. Ann. Thorac. Surg. 2012 Jun;93(6):2084-92.
- Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA, Del Nido P, Fasules JW, Graham TP, Hijazi ZM, Hunt SA, King ME, Landzberg MJ, Miner PD, Radford MJ, Walsh EP, Webb GD. ACC/AHA 2008 Guidelines for the Management of Adults with Congenital Heart Disease: Executive Summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to develop guidelines for the management of adults with congenital heart disease). Circulation. 2008 Dec 02;118(23):2395-451.