Couvelaire uterus
Couvelaire uterus also known as uteroplacental apoplexy or Couvelaire syndrome, is a rare but non-fatal complication of severe form of placental abruption 1. Couvelaire uterus was first described in the medical literature by Dr. Alexandre Couvelaire, a French obstetrician in 1912 2. Couvelaire uterus occurs when vascular damage within the placenta causes hemorrhage from placental blood vessels that progresses to and infiltrates the wall of the uterus causing placental separation, followed by infiltration in the lateral portions of the uterus 1. Occasionally, the infiltrations reach the peritoneal cavity 3. Couvelaire uterus can only be diagnosed by direct visualization of the uterus or biopsy (or both), with characteristic ecchymosis discoloration, secondary to extravasation of blood into the myometrium and serosa 1. For this reason, its occurrence is perhaps underreported and underestimated in the literature. Couvelaire uterus or Couvelaire syndrome is estimated to complicate 5% of all cases of abruption 4.
Couvelaire uterus does not usually affect the uterus ability to contract, particularly after amniotomy and decompression to allow constriction of spiral arteries 5. Couvelaire uterus often resolves spontaneously 6.
Couvelaire uterus is managed conservatively 1. The myometrial bleeds seldom interfere with uterine contractions enough to cause significant postpartum hemorrhage. The uterus usually responds well to intravenous oxytocin. It is important to remember that Couvelaire uterus should not be used as an indication for hysterectomy and should be discouraged 3.
Couvelaire uterus key points
- Couvelaire uterus or uteroplacental apoplexy is a rare non-fatal complication of abruptio placentae (placental abruption).
- Diagnosis is made on visual inspection of the uterus 1.
- Within the medical literature, case reports have documented patients with Couvelaire uterus which progressed to massive placenta abruption requiring blood transfusion 7.
- Management is conservative and hysterectomy is usually not required 1.
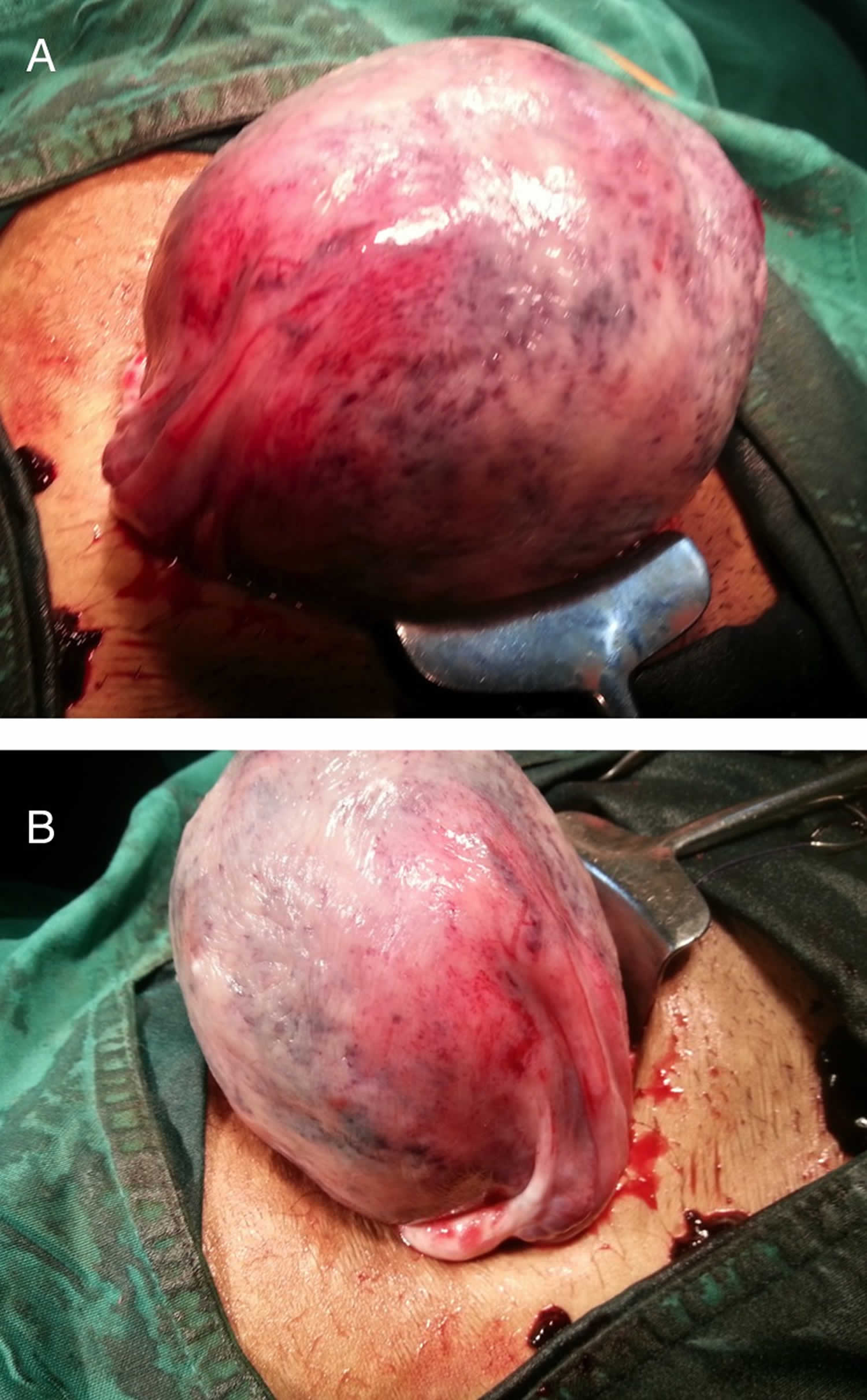
Figure 1. Couvelaire uterus
Footnote: (A,B) The dark purple and copper color patches with ecchymosis and indurations diagnostic of Couvelaire uterus (uteroplacental apoplexy). Hemorrhagic infiltration in the lateral portions of the uterus is also seen.
[Source 3 ]Couvelaire uterus causes
The exact cause of Couvelaire uterus is unknown; however, Couvelaire uterus has been associated with placenta abruption, placenta previa, amniotic fluid embolism, coagulopathy, ruptured uterus from a transverse lie and preeclampsia 8. With a case report of the association of Couvelaire uterus with placenta accreta 9.
In early stages of hemorrhage resulting from pathologic vascular damage within the placenta itself, blood seeps into the decidua basalis, ultimately causing a separation of the placenta 10. The hemorrhage often progresses, and the walls of the uterus, usually in the lateral portions, may become infiltrated with blood 11. Occasionally, such effusions of blood extend beneath the tubal serosa, into the connective tissue of the broad ligaments, and into the substance of the ovaries, as well as free in the peritoneal cavity 12.
The primary cause of placental abruption is usually unknown, but multiple risk factors have been identified 13. However, only a few events have been closely linked to placental abruption.
Risk factors in abruptio placentae include the following:
- Maternal hypertension – Most common cause of abruption, occurring in approximately 44% of all cases
- Maternal trauma (eg, motor vehicle collision, assaults, falls) – Causes 1.5-9.4% of all cases
- Cigarette smoking
- Alcohol consumption
- Cocaine use
- Short umbilical cord
- Sudden decompression of the uterus (eg, premature rupture of membranes, delivery of first twin)
- Retroplacental fibromyoma
- Retroplacental bleeding from needle puncture (ie, postamniocentesis)
- Idiopathic (probable abnormalities of uterine blood vessels and decidua) 14
- Previous placental abruption
- Chorioamnionitis 15
- Prolonged rupture of membranes (24 hour or longer)
- Maternal age 35 years or older
- Maternal age younger than 20 years
- Male fetal sex
- Low socioeconomic status
- Elevated second trimester maternal serum alpha-fetoprotein (associated with up to a 10-fold increased risk of placental abruption)
- Subchorionic hematoma 16
Cigarette smoking and tobacco abuse
Cigarette smoking increases a patient’s overall risk of placental abruption 17.
A prospective cohort study showed the risk of placental abruption to be increased by 40% for each year of smoking prior to pregnancy.
In addition to the increased risk of placental abruption caused by tobacco abuse, the perinatal mortality rate of infants born to women who smoke and have an abruption is increased 18.
Cocaine (powder or crack) abuse
The hypertension and increased levels of catecholamines caused by cocaine abuse are thought to be responsible for a vasospasm in the uterine blood vessels that causes placental separation and abruption. However, this hypothesis has not been definitively proven.
The rate of abruption in patients who abuse cocaine has been reported to be approximately 13-35% and may be dose-dependent 19.
Trauma
Abdominal trauma is a major risk factor for placental abruption.
Motor vehicle accidents often cause abdominal trauma. The lower seat belt should extend across the pelvis, not across the midabdomen, where the fetus is located.
Trauma may also be due to domestic abuse or assault, both of which are underreported.
Thrombophilia
While it was previously thought that patients who experienced early or severe abruptions were at increased risk of having a specific thrombophilia, this is no longer thought to be the case and screening of patients with an abruption is no longer recommended.
Couvelaire uterus symptoms
The main symptom of placental abruption is vaginal bleeding. You also may have discomfort and tenderness or sudden, ongoing belly or back pain. Sometimes, these symptoms may happen without vaginal bleeding because the blood is trapped behind the placenta and uterine wall. If you have any of these symptoms, see your health care provider.
- If the separation is slight, you may have only light bleeding. You may also have cramps or feel tender in your belly.
- If the separation is moderate, you may have heavier bleeding. Cramps and belly pain will be more severe.
- If more than half the placenta detaches, you may have belly pain and heavy bleeding. You may also have contractions. The baby may move more or less than normal.
Frequency of symptoms in placental abruption is as follows 20:
- Vaginal bleeding – 80%
- Abdominal or back pain and uterine tenderness – 70%
- Fetal distress – 60%
- Abnormal uterine contractions (eg, hypertonic, high frequency) – 35%
- Idiopathic premature labor – 25%
- Fetal death – 15%
Vaginal bleeding
Vaginal bleeding is present in 80% of patients diagnosed with placental abruptions.
Bleeding may be significant enough to jeopardize fetal and maternal health in a relatively short period.
Remember that 20% of abruptions are associated with a concealed hemorrhage, and the absence of vaginal bleeding does not exclude a diagnosis of abruptio placentae.
Contractions or uterine tenderness
Contractions and uterine hypertonus are part of the classic triad observed with placental abruption.
Uterine activity is a sensitive marker of abruption and, in the absence of vaginal bleeding, should suggest the possibility of an abruption, especially after some form of trauma or in a patient with multiple risk factors.
Decreased fetal movement
This may be the presenting complaint.
Decreased fetal movement may be due to fetal jeopardy or death.
Couvelaire uterus diagnosis
Couvelaire uterus can only be diagnosed by direct visualization of the uterus or biopsy (or both), with characteristic appearance of a purplish or copper-colored ecchymosis discoloration, secondary to extravasation of blood into the myometrium and serosa 1. Histologically, blood is found between muscle bundles, in perivascular tissue, and in the subserosa. The decidual spiral arterioles may show acute atheromatous processes, with foamy macrophages present 11.
Laboratory studies
Multiple laboratory studies may be helpful in the management of this problem.
CBC count
A complete blood cell (CBC) count can help to determine the patient’s current hemodynamic status, but findings are not reliable for estimating acute blood loss.
In an acute hemorrhage, the fall in hematocrit value lags several hours behind the bleeding and may be falsely decreased by the administration of crystalloid fluids during resuscitation.
Fibrinogen study
Pregnancy is associated with hyperfibrinogenemia; therefore, modestly depressed fibrinogen levels may represent significant coagulopathy. A fibrinogen level of less than 200 mg/dL suggests that the patient has a severe abruption.
The goal should be to keep the fibrinogen level above 100 mg/dL, which can be accomplished via transfusion of fresh frozen plasma or cryoprecipitate, as necessary.
Prothrombin time (PT) or activated partial thromboplastin time (aPTT)
Some form of disseminated intravascular coagulation (DIC) is present in up to 20% of patients with severe abruptions.
Because many of these patients require cesarean delivery, knowing a patient’s coagulation status is imperative.
Blood urea nitrogen (BUN) or creatinine study
The hypovolemic condition brought on by a significant abruption also affects renal function.
The condition usually self-corrects without significant residual dysfunction, if fluid resuscitation is timely and adequate.
Blood and Rh types
The patient should have her blood typed and at least 2 units of packed red blood cells crossmatched in the event she requires a transfusion.
The blood Rh type is important to determine, because patients who are Rh-negative require Rh immune globulin to prevent isoimmunization, which could affect future pregnancies.
Kleihauer-Betke test
Findings help to detect fetal red blood cells in the maternal circulation.
If the abruption is significant, inadvertent transfusion of fetal blood into the maternal circulation may occur. In women who are Rh-negative, this fetal-to-maternal transfusion may lead to isoimmunization of the mother to Rh factor. Kleihauer-Betke test findings help to determine the volume of fetal blood transfused into the maternal circulation.
All patients who are D-negative should receive Rho (D) immune globulin (RhoGAM) after significant trauma. Kleihauer-Betke test findings may help to determine the appropriate dosage of Rho (D) immune globulin in cases of significant fetal-maternal hemorrhage.
Ultrasonography
Ultrasonography is a readily available and important imaging modality for assessing bleeding in pregnancy.
The quality and sensitivity of ultrasonography in detecting placental abruptions has improved significantly; however, it is not a sensitive modality for this purpose—findings are positive in only 25% of cases confirmed at delivery, and the negative predictive value is low at around 50%.
In addition, there does not appear to be any clinical difference in presentation between women who have an abruption seen on ultrasonography and those who do not.
Ultrasonographic studies do help to quickly diagnose placenta previa as the etiology of bleeding, if present 21.
Placental abruption shows as a retroplacental clot on an ultrasonographic image, but not all abruptions are ultrasonographically detectable.
In the acute phase, a hemorrhage is generally hyperechoic, or even isoechoic, compared with the placenta; a hemorrhage does not become hypoechoic for nearly a week.
Ultrasonography can help to exclude other causes of third-trimester bleeding. Possible findings consistent with an abruption include (1) retroplacental clot (ie, hyperechoic to isoechoic in the acute phase, changing to hypoechoic within a wk), (2) concealed hemorrhage, or (3) expanding hemorrhage.
Nonstress test
External fetal monitors often reveal fetal distress, as evidenced by late decelerations, fetal bradycardia, or decreased beat-to-beat variability.
An increase in the uterine resting tone may also be noticed, along with frequent contractions that may progress to uterine hyperstimulation.
Biophysical profile
A biophysical profile (BPP) can be used to help evaluate patients with chronic abruptions who are being managed conservatively.
A biophysical profile score of less than 6 (maximum of 10) may be an early sign of fetal compromise.
A modified biophysical profile (nonstress test with amniotic fluid index) is sometimes used for monitoring in this situation.
Couvelaire uterus treatment
Couvelaire uterus is managed conservatively 1. The myometrial bleeds seldom interfere with uterine contractions enough to cause significant postpartum hemorrhage. The uterus usually responds well to intravenous oxytocin. It is important to remember that Couvelaire uterus should not be used as an indication for hysterectomy and should be discouraged 3.
Initial management of placental abruption
- Begin continuous external fetal monitoring for the fetal heart rate and contractions.
- Obtain intravenous access using 2 large-bore intravenous lines.
- Institute crystalloid fluid resuscitation for the patient.
- Type and crossmatch blood.
- Begin a transfusion if the patient is hemodynamically unstable after fluid resuscitation.
- Correct coagulopathy, if present.
- Administer Rh immune globulin if the patient is Rh-negative.
- Begin course of corticosteroids for fetal lung maturity (if the patient is less than 37 weeks gestation and they have not been previously given during pregnancy) 22.
Vaginal delivery
This is the preferred method of delivery for a fetus that has died secondary to placental abruption.
The ability of the patient to undergo vaginal delivery depends on her remaining hemodynamically stable.
Delivery is usually rapid in these patients secondary to increased uterine tone and contractions.
Cesarean delivery
Cesarean delivery is often necessary for fetal and maternal stabilization.
While cesarean delivery facilitates rapid delivery and direct access to the uterus and its vasculature, it can be complicated by the patient’s coagulation status. Because of this, a vertical skin incision, which has been associated with less blood loss, is often used when the patient appears to have DIC.
The type of uterine incision is dictated by the gestational age of the fetus, with a vertical or classic uterine incision often being necessary in the preterm patient.
If hemorrhage cannot be controlled after delivery, a cesarean hysterectomy may be required to save the patient’s life.
Before proceeding to hysterectomy, other procedures, including correction of coagulopathy, ligation of the uterine artery, administration of uterotonics (if atony is present), packing of the uterus, and other techniques to control hemorrhage, may be attempted.
References- Hubbard JL, Hosmer SB. Couvelaire uterus. J Am Osteopath Assoc. 1997;97(9):536-537. doi:10.7556/jaoa.1997.97.9.536
- Couvelaire A. Deux nouvelles observations d’apoplexie utero-placentaire (hemorrhagies retro-placentaires avec infiltration sanguine de la pavoi musculaire de l’uterus). Ann Gynecol Obstet 1912;9:486
- Rathi M, Rathi SK, Purohit M, Pathak A. Couvelaire uterus. BMJ Case Rep. 2014;2014:bcr2014204211. Published 2014 Mar 31. doi:10.1136/bcr-2014-204211 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3975566
- Habek D, Selthofer R, Kulas T. Uteroplacental apoplexy (Couvelaire syndrome). Wien Klin Wochenschr. 2008;120(3-4):88. doi:10.1007/s00508-008-0931-7
- Habek D, Selthofer R, Kulas T. Uteroplacental apoplexy (Couvelaire syndrome). Wien Klin Wochenschr 2008;120:88 10.1007/s00508-008-0931-7
- Beckmann CR, Ling FW, Barzansky BM, et al (eds): Obstetrical hemorrhage, in Obstetrics and Gynecology, ed 2. 1995. Baltimore, Md, Williams & Wilkins, 1995, p 122
- Rathi M, Rathi SK, Purohit M, Pathak A: Couvelaire uterus. BMJ CaseRep 2014; doi:10.11136/bcr-2014-204211
- Mahendra G, Ravindra S. Pukale, Vijayalakshmi S, Priya. Couvelaire uterus – A case report. IAIM, 2015; 2(3): 142-145. https://iaimjournal.com/wp-content/uploads/2015/03/20-Couvelaire-uterus.pdf
- A 30-Year-Old Female Found to Have a Couvelaire Uterus With Placenta Accreta During Planned Cesarean Delivery. MILITARY MEDICINE, 182, 3/4:e1877, 2017
- Pratola D, Wilkin P: The placenta, umbilical cord, and amniotic sac, in Gompel C, Silver-berg SG (eds): Pathology in Gynecology and Obstetrics, ed 3. Philadelphia, Pa, JB lippincott Co, 1985, P 498.
- Pauerstein CJ: Abnormalities and diseases of the placenta and apendages, in Novak ER, Woodroff JD (eds): Novak’s Gynecologic and Obstetric Pathology, ed 8. Philadelphia, Pa, WB Saunders Co, 1979, p 622.
- Cunningham FG, MacDonald PC, Gant NF, et al (eds): Obstetrical hemorrhage, in William’s Obstetrics, ed 20. Stamford, Conn, Appleton & Lange, 1997, pp 751-752.
- Workalemahu T, Enquobahrie DA, Gelaye B, Thornton TA, Tekola-Ayele F, Sanchez SE, et al. Abruptio placentae risk and genetic variations in mitochondrial biogenesis and oxidative phosphorylation: replication of a candidate gene association study. Am J Obstet Gynecol. 2018 Dec. 219 (6):617.e1-617.e17
- Ananth CV, Oyelese Y, Yeo L, Pradhan A, Vintzileos AM. Placental abruption in the United States, 1979 through 2001: temporal trends and potential determinants. Am J Obstet Gynecol. 2005 Jan. 192(1):191-8.
- Rana A, Sawhney H, Gopalan S. Abruptio placentae and chorioamnionitis-microbiological and histologic correlation. Acta Obstet Gynecol Scand. 1999 May. 78(5):363-6.
- Tuuli MG, Norman SM, Odibo AO, Macones GA, Cahill AG. Perinatal outcomes in women with subchorionic hematoma: a systematic review and meta-analysis. Obstet Gynecol. 2011 May. 117(5):1205-12.
- Ananth CV, Smulian JC, Vintzileos AM. Incidence of placental abruption in relation to cigarette smoking and hypertensive disorders during pregnancy: a meta-analysis of observational studies. Obstet Gynecol. 1999 Apr. 93(4):622-8.
- Ananth CV, Savitz DA, Bowes WA Jr, Luther ER. Influence of hypertensive disorders and cigarette smoking on placental abruption and uterine bleeding during pregnancy. Br J Obstet Gynaecol. 1997 May. 104(5):572-8.
- Hoskins IA, Friedman DM, Frieden FJ. Relationship between antepartum cocaine abuse, abnormal umbilical artery Doppler velocimetry, and placental abruption. Obstet Gynecol. 1991 Aug. 78(2):279-82.
- Abruptio Placentae Clinical Presentation. https://emedicine.medscape.com/article/252810-clinical
- Kramer MS, Usher RH, Pollack R. Etiologic determinants of abruptio placentae. Obstet Gynecol. 1997 Feb. 89(2):221-6.
- Antenatal Corticosteroid Therapy for Fetal Maturation. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2017/08/antenatal-corticosteroid-therapy-for-fetal-maturation