What does crystals in urine mean
Crystals in urine is also called crystalluria, is a frequent finding in the routine examination of urine sediments. Your urine contains many chemicals. Sometimes these chemicals form solids, called crystals. It’s normal to have a few small urine crystals. Larger crystals or specific types of crystals can become kidney stones. Kidney stones are hard, pebble-like substances that can get stuck in the kidneys. A kidney stone can also be as small as a grain of sand, as big as a pea, or even larger. While kidney stones rarely cause serious damage, they can be very painful.
In most crystals in urine cases the precipitation of crystals of calcium oxalate, uric acid triple phosphate, calcium phosphate and amorphous phosphates or urates, struvite, aminoacids (cystine), purines (2,8-dihydroxyadenine and xanthine) is caused by transient supersaturation of the urine, ingestion of foods, changes of urine temperature and/or pH which occur upon standing after urination 1 and drugs (e.g. sulfamethoxazole, amoxycillin, ceftriaxone, atazanavir) 2. In a minority of cases, however, crystals in urine is associated with pathological conditions such as urolithiasis (formation of stones in the urinary tract), acute uric acid nephropathy, ethylene glycol poisoning 3, hypereosinophilic syndrome. In addition, crystals in urine can be due to drugs such as sulphadiazine, methotrexate, acyclovir, triamterene, piridoxylate, primidone, which under the influence of various factors can crystallize within the tubular lumina and cause renal damage.
If a large number, large size, or certain types of crystal are found in your urine, it may mean you have a kidney stone that requires medical treatment, but it doesn’t always mean you need treatment. Sometimes a small kidney stone can pass through your urine on its own, and cause little or no pain. Also, certain medicines, your diet, and other factors can affect your results. If you have questions about your urine crystal results, talk to your health care provider.
A urine test looking at the amount, size, and type of crystals in your urine is useful for: the diagnosis of lithogenic inherited diseases (e.g. primary hyperoxaluria, cystinuria, adenine phosphoribosyltransferase deficiency); the identification of crystals due to drugs, which may be responsible for acute kidney injury as well as chronic kidney disease; the assessment of metabolic disorders associated with stone formation; the assessment, in stone formers, of the risk of stone recurrence.
Crystals in urine (crystalluria) should be interpreted according to various criteria 4:
- Chemical nature of crystals for abnormal crystals such as struvite, ammonium urate, cystine, dihydroxyadenine, xanthine or drugs;
- Crystalline phase of common chemical species as calcium oxalates, calcium phosphates and uric acids;
- Crystal morphology (calcium oxalates);
- Crystal size (calcium oxalates);
- Crystal abundance (calcium oxalates, calcium phosphates, uric acids, cystine);
- Crystal aggregation (calcium oxalates);
- Frequency of crystalluria assessed on serial first morning urine samples, a very useful tool for long-term surveillance of patients.
Within calcium oxalate crystalluria, presence of whewellite is a marker of elevated oxalate concentration (urine oxalate > 0.3 mmol/L); a crystal number > 200/mm 3 is highly suggestive of heavy hyperoxaluria of genetic or absorptive origin. Predominant weddellite crystalluria is most often indicative of an excessive urine calcium concentration (> 3.8 mmol/L); a dodecahedric aspect of the crystals is a marker for heavy hypercalciuria (> 6 mmol/L) while an increased crystal size (>or= 35 microm) is indicative of simultaneous hypercalciuria and hyperoxaluria. Calculation of the global crystal volume, especially when applied to calcium oxalates or cystine, is a clinically useful tool for the monitoring of patients suffering from primary hyperoxaluria or cystinuria. Lastly, presence of crystalluria in more than 50% of serial first voided morning urine samples is in our experience the most reliable biological marker for detecting the risk of stone recurrence in lithiasic patients.
For clinical diagnostic purpose, some crystals are significant because of their presence alone:
- Cystine, which reveals a congenital cystinuria;
- Dihydroxyadenine resulting from a defect of adenine phosphoribosyltransferase;
- Orotic acid salt as a marker of uridine monophosphate synthetase deficiency;
- Xanthine which is observed in homozygous xanthine deshydrogenase deficiency or in the treatment of Lesh-Nyhan syndrome by high doses of allopurinol;
- Leucine met in leucinosis or Hartnup’s disease;
- Tyrosine met in tyrosinosis or some serious liver diseases;
- Struvite, resulting from the action of urease which exists in some micro-organisms as Proteus species, Providencia stuartii, Ureaplasma urealyticum, Corynebacterium urealyticum and some strains of Klebsiella, Staphylococcus or Pseudomonas species.
- Ammonium urate due to hyperuricosuria and hyperammoniuria with an orientation towards a UTI (urinary tract infection) by urea-splitting bacteria (high pH values) or infectious diarrhea with digestive loss of bases and inadequate intake of phosphorus (normal pH values);
- Drugs from inappropriate dosage or absence of preventive measures.
Global crystal volume
In stone formers, the disappearance of crystalluria indicates that lithogenic activity is under control 5. This result is most often attainable in patients with calcium or uric acid nephrolithiasis, while a complete disappearance of crystalluria is more difficult to achieve in inherited disorders such as primary hyperoxaluria type 1 (PH1), cystinuria or dihydroxyadeninuria, which have a very active and permanent crystallization. In these conditions, a decrease in the amount of crystals present in urine samples, expressed as global crystal volume, is often sufficient to efficiently reduce the lithogenic process 6. By comparing clinical outcomes and variations in global crystal volume in serial urine samples, scientists have determined quantitative thresholds of harmful crystalluria in primary hyperoxaluria type 1 and cystinuria, thus defining the desirable goals to achieve 6. In cystinuric patients, a global crystal volumecys <3000 μm³/mm³ was associated with a significantly decreased risk of stone recurrence 6. In primary hyperoxaluria type 1, a crystal volume <500 μm³/mm³ of urine was associated with a lowered risk of tubular plugging with calcium oxalate crystals in the days following combined liver-kidney transplantation 7, a crucial period when considerable amounts of calcium oxalate stored in bones are excreted through the grafted kidney, with the risk of massive tubular obstruction and loss of the kidney transplant 8. By closely monitoring global crystal volumecaox, early post-transplant care of primary hyperoxaluria type 1 children could be optimized 7, which resulted in improved long-term outcome 9.
What causes crystals in urine
Crystals in urine (crystalluria) is a frequent finding both in normal individuals and in patients suffering from stones in the urinary tract from various causes such as metabolic disorders, inherited diseases or drugs.
Crystals in urine (crystalluria) is an imbalance between promoters and inhibitors; the first are the engine of the crystal formation and the latter (made up of substances of low or high molecular weight) have physicochemical properties opposed to one or more steps of the crystallization process 10. The disruption of equilibrium may be due to an excessive concentration of the promoters or a defect of inhibitor concentration or change in their molecular structure 11. A change in the ionization state of promoters or inhibitors, especially under the influence of urine pH, plays an essential role both in creating this disequilibrium, and also in its restoration by medical treatment. The characteristics of crystals in urine (crystalluria) may be different in subjects at risk of renal stones compared to controls 12. Urinary calculi result from a long-term exposure to supersaturated urine. Because the urine composition is constantly varying according to dietary and drinking habits, the stones may contain several components, some of them being often found in very low proportion. In other cases, the pathological conditions responsible for stone formation may induce urine supersaturation regarding several chemical compounds that may crystallize simultaneously in urine and that will be present together in the stone. Thus, it is clinically relevant to identify stone constituents and provide semi quantitative evaluation of their respective proportions within a stone. Among physical methods, X-ray diffraction and Fourier transform infrared spectroscopy are now universally used for stone analysis. However, when X-ray diffraction or Fourier transform infrared spectroscopy analysis is performed on a powdered sample of the whole stone, no indication is given as to the respective location (core or peripheral layers) of the diverse constituents in the case of mixed stones, even if the stone is large enough to allow a separate analysis of its different parts. Today, chemical methods are yet extensively used for stone analysis. Indeed, chemical methods fail to identify rare purine stones resulting from genetic disorders such as 2,8-dihydroxyadenine 13 or drug-induced calculi 14. Moreover, they are unable to provide reliable information on crystalline phases present in calcium stones. Only physical methods are able to identify such a diversity of components 15.
If the formation of stones is always preceded by crystalluria, the reverse is not true and crystalluria may occur without resulting in stone formation. Therefore, the clinical relevance of crystalluria in kidney stone formers remains largely debated 10. Although some authors proposed crystals in urine as an index of stone disease activity in the early seventies 16, routine search for crystals in urine has not gained widespread popularity in clinical practice and is not currently recommended in the evaluation of stone formers. Indeed, because crystals in urine is occasionally found, in 15%–20% of healthy subjects, presence of crystals in a single urine specimen was regarded as not discriminating between stone formers and non-stone formers 17.
Crystals from metabolic origin are the result of an equilibrium break between two groups of substances, the promoters and the inhibitors of crystallization 2. Promoters are substances excreted by the kidney, whose concentration exceeds the ability of urine to maintain them as soluble molecules and ions. Calcium, oxalate, urate and phosphate ions are the main promoters of crystals 18. Inhibitors, which are either filtered through glomeruli or are produced locally by tubular cells, are substances which are able to avoid or delay crystal formation, growth, aggregation and/or adhesion to the tubular epithelium 19. Among inhibitors, small ions and molecules such as magnesium, citrate and pyrophosphate, form complexes with some promoters, a fact which decreases urine supersaturation 19. Macromolecules such as osteopontin, bikunin, matrix GLA protein, Tamm-Horsfall protein or the urinary fragment 1 of prothrombin also are able to stop crystal growth, aggregation and/or adhesion to the tubular cells, thus allowing the crystals to be eliminated from the kidney with the urine flow 20.
Classification of urinary crystals
More than 100 chemical and crystalline forms have been identified in urinary calculi 21. Among them, 15 are frequent (more than 1% of stones), the other ones being considered as rare but often related to specific lithogenic conditions.
From an epidemiological point of view, calcium oxalate is now the most common chemical component of urinary stones throughout the world. It is associated in a majority of cases with other crystalline phases as minor components that may have a clinical relevance. Stones composed of a mixture of calcium oxalate (calcium oxalate dihydrate and/or calcium oxalate monohydrate) and carbapatite (without struvite) accounted for 19.7% of the total number of stones in our series. In carbapatite stones, identification of the minor components contributes to etiological diagnosis. Presence of brushite, weddellite or octacalcium phosphate pentahydrate is suggestive of hypercalciuria while amorphous carbonated calcium phosphate or whitlockite orient towards urinary tract infection (UTI). Mixtures of calcium oxalate and calcium oxalate monohydrate are common in medullary sponge kidney. Mixtures of whewellite and uric acid must prompt to seek insulin resistance and, often, type 2 diabetes.
Calcium oxalates crystals in urine
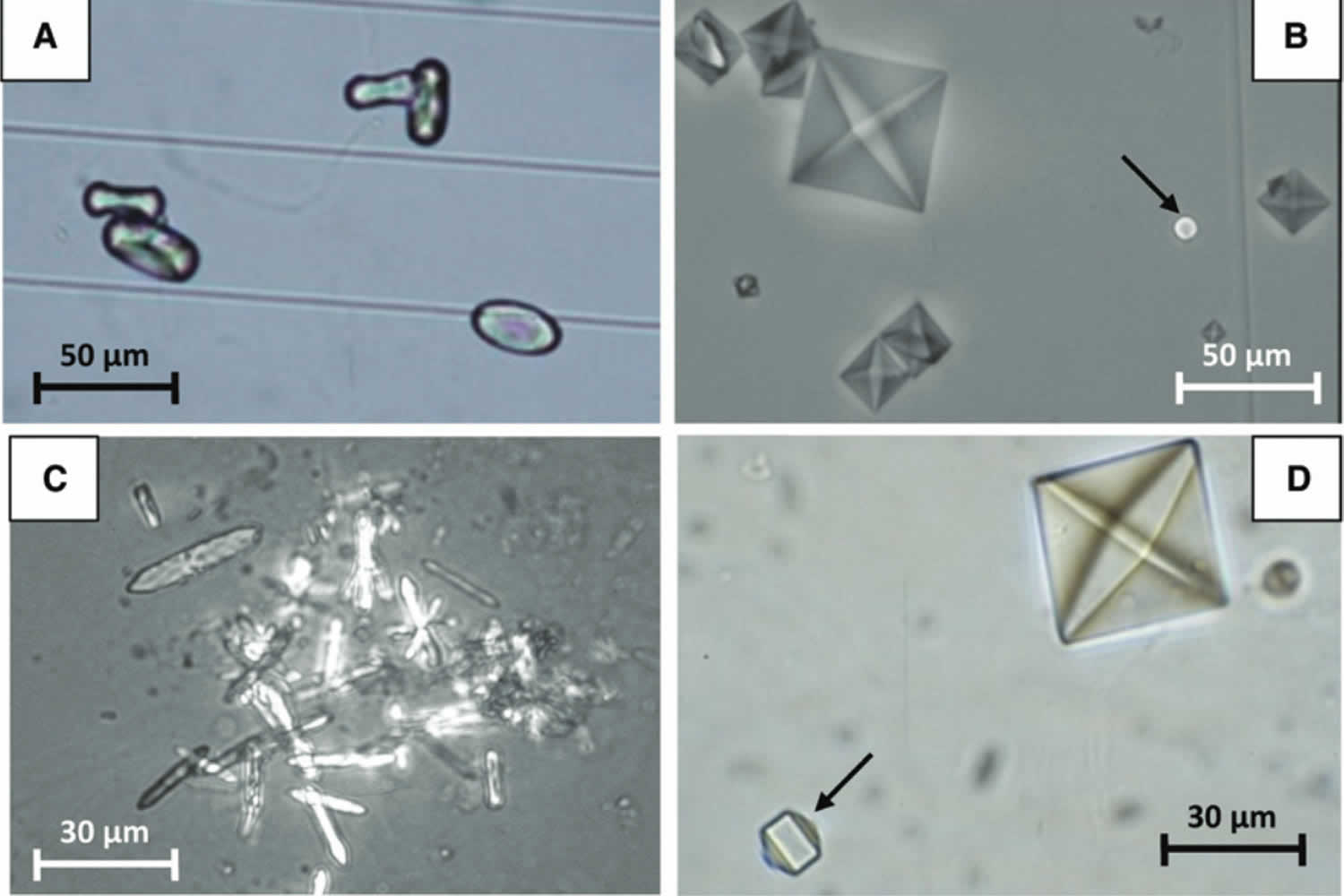
Calcium oxalate monohydrate, or whewellite (Figure 1A) is closely associated with high oxalate concentration in the presence of normal or low calcium 22. Urine samples that contain only whewellite crystals without weddellite are highly suggestive for a high oxalate molar concentration, a fact that should prompt the search for primary hyperoxaluria. Conversely, calcium oxalate dihydrate, or weddellite (Figure 1B), is usually associated with hypercalciuria. In our experience, more than 94% of urine samples containing calcium oxalate crystals with a calcium to oxalate ratio < 5 exhibit whewellite crystals, either alone or accompanied by weddellite. By contrast, more than 90% of urine samples containing calcium oxalate crystals with a calcium to oxalate ratio > 14 contain weddellite alone 23.
Whewellite crystals with oval or dumb-bell shape (Figure 1A) are commonly associated with high levels of urine oxalate, while small crystals resembling erythrocytes may be found in urine with normal or moderately increased oxalate (Figure 1B). Peculiar types of whewellite crystals, with the shape of elongated and narrow hexagons and “diamonds” (Figure 1C) are found in the urine after the ingestion of ethylene glycol, which results in severe hyperoxaluria. Weddellite, in most instances, appears as octahedral (bipyramidal) crystals (Figure 1B), while more rare dodecahedral crystals (Figure 1D) are associated with high concentration of urinary calcium.
Figure 1. Calcium oxalate crystals in urine
Footnote: (A) Whewellite crystals with the typical ovoid shape. (B) Typical octahedral (bipyramidal) crystals of weddellite and a small red-cell like crystal of whewellite (arrow). (C) Elongated hexagonal crystals of whewellite as found in the urine of patients after the ingestion of ethylene-glycol. (D) Octahedral and dodecahedral (arrow) crystals of weddellite.
[Source 2 ]Calcium phosphate crystals in urine
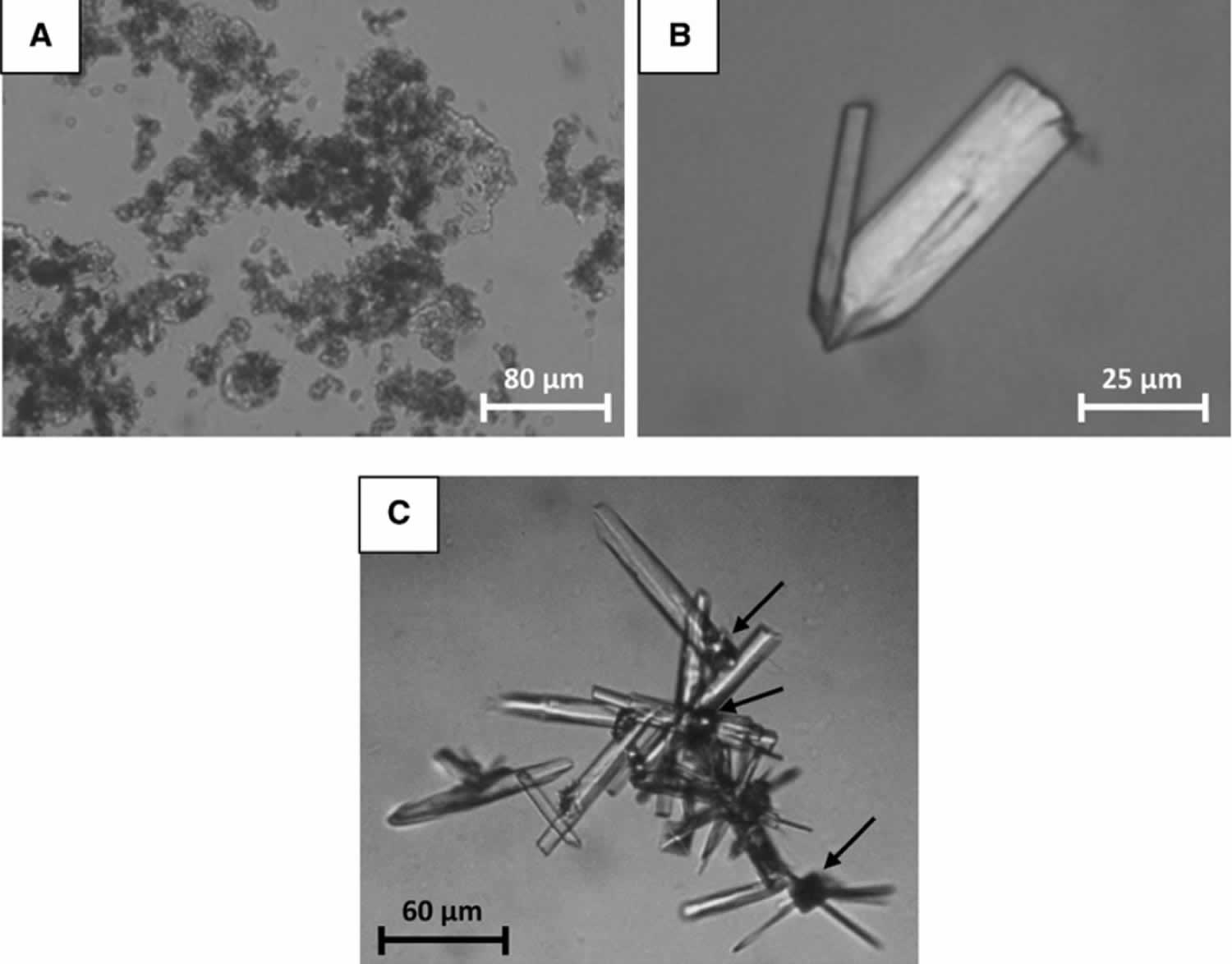
The formation of crystals of calcium orthophosphates (mainly amorphous carbonated calcium phosphate and carbapatites) (Figure 2A) and brushite (dicalcium
phosphate dihydrate) (Figure 2B) depend on different biochemical conditions [19]. Calcium orthophosphate species are mainly dependent on urine pH and they form easily when urine pH is above 6.5. Brushite formation usually requires high concentrations of calcium and phosphate, even though it may also be favored by low citrate concentration. Brushite can also be found in aggregates with weddellite crystals (Figure 2C), being often associated with hypercalciuria.
Figure 2. Calcium phosphate crystals in urine
Footnote: (A) Amorphous granulations of carbonated calcium phosphate. (B) Asymmetrical rod-shaped crystals of calcium hydrogen phosphate dihy-drate (brushite). (C) Crystal aggregate of brushite intermingled with weddellite (arrows).
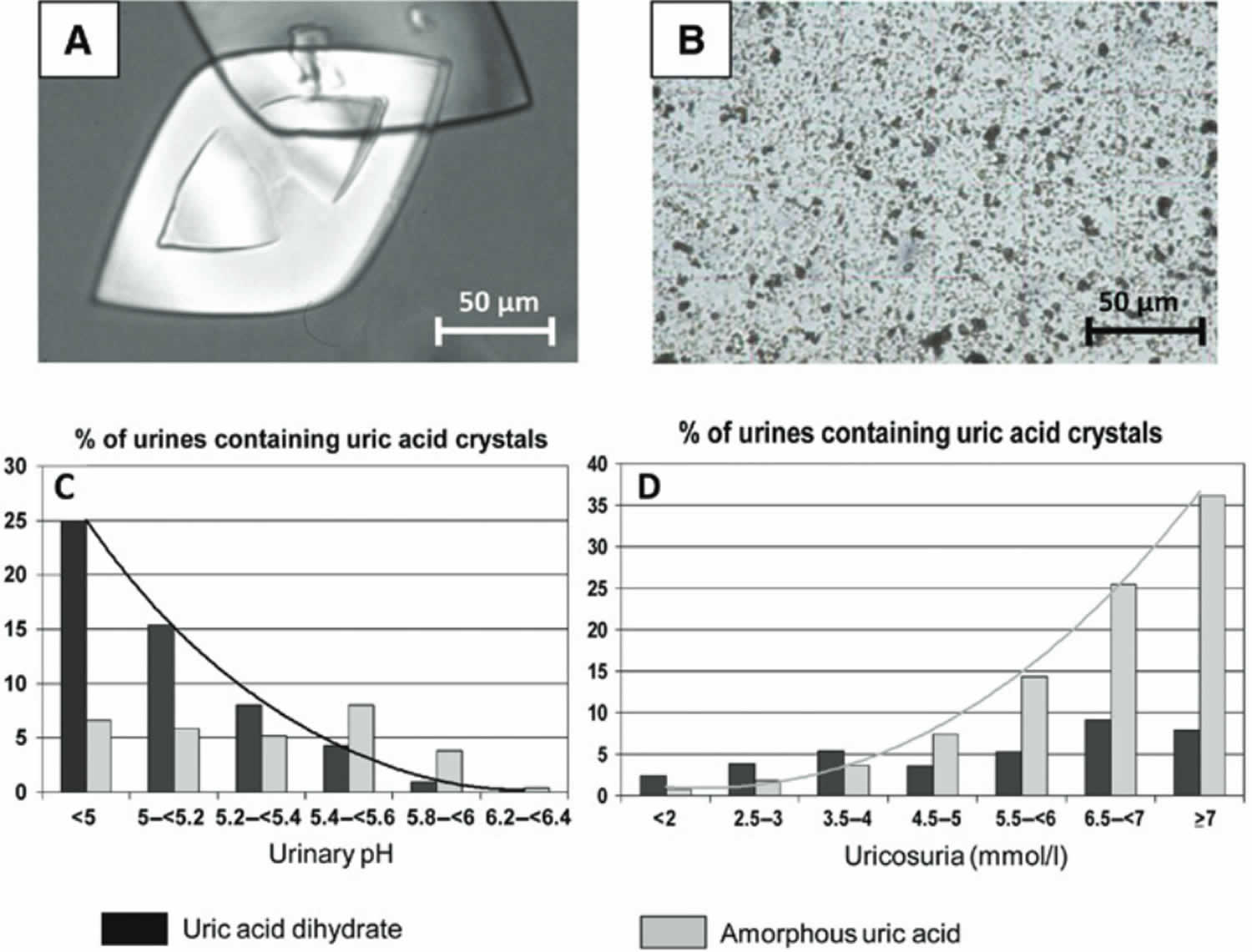
[Source 2 ]Uric acids and urates crystals in urine
Uric acid crystals form in acidic urine. Four types of uric acid precipitates may be found in urine: amorphous uric acid, anhydrous uric acid (uricite) and two hydrated forms, namely uric acid monohydrate and dihydrate. Uric acid dihydrate (Figure 3A) and amorphous uric acid (Figure 3B) are the most common species found in urine. As shown in Figure 3C and D, they depend on different metabolic conditions: uric acid dihydrate is mostly dependent on low urine pH while amorphous uric acid is mainly related to high urine urate concentration.
By contrast, urate salts, such as ammonium hydrogen urate, form in alkaline urine, which explains why this crystalline species may accompany struvite in the case of urinary tract infection by urea-splitting bacteria.
Figure 3. Uric acids and urates crystals in urine
Footnote: (A) Typical lozenges of uric acid dihydrate crystals. (B) Amorphous uric acid granulations. (C) Correlation between uric acid dihydrate crystals and urinary pH. (D) Correlation between amorphous uric acid granulations and uricosuria.
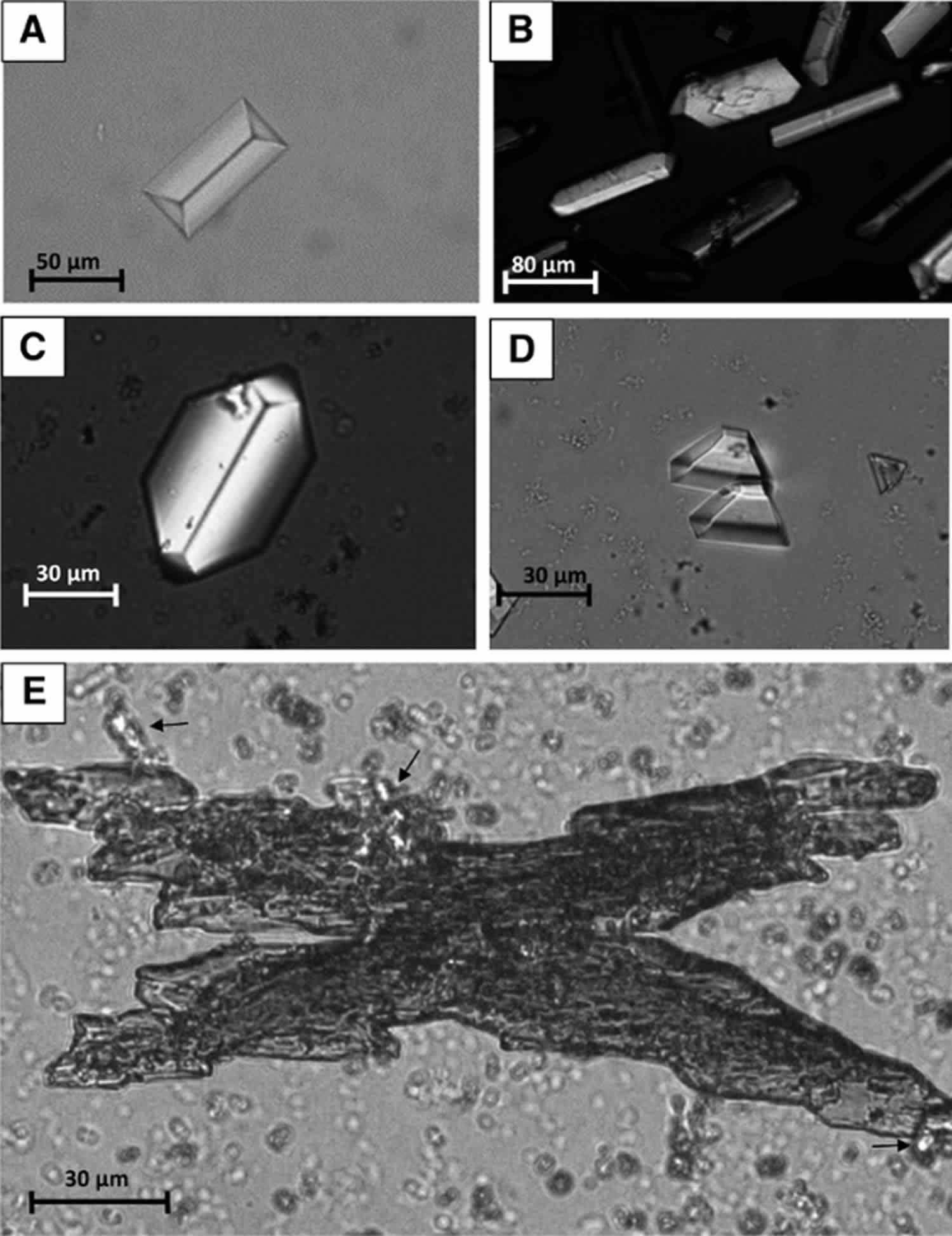
[Source 2 ]Struvite
Magnesium ammonium phosphate hexahydrate or struvite, of which several morphological variants can be observed (Figure 4), precipitates in urine only in the presence of high urine pH associated with high ammonium content. This condition is found only in the case of urinary tract infection by micro-organisms able to hydrolyze urea, which results in the production of high amounts of ammonia and alkaline urine. Thus, struvite may be considered virtually pathognomonic of the presence of urea-splitting bacteria in the urine specimen.
Figure 4. Struvite crystals in urine
Footnote: (A) A coffin-shaped crystal of struvite. (B) Rod-shaped and coffin-shaped crystals of struvite. (C) A hexagonal crystal of struvite and small agglomerates of amorphous carbonated calcium phosphate grains. (D) Trapezoidal crystals of struvite. (E) A large X-shaped crystal of stru-vite with birefringent small aggregates of ammonium hydrogen urate crystals (black arrows).
[Source 2 ]Cystine crystals in urine
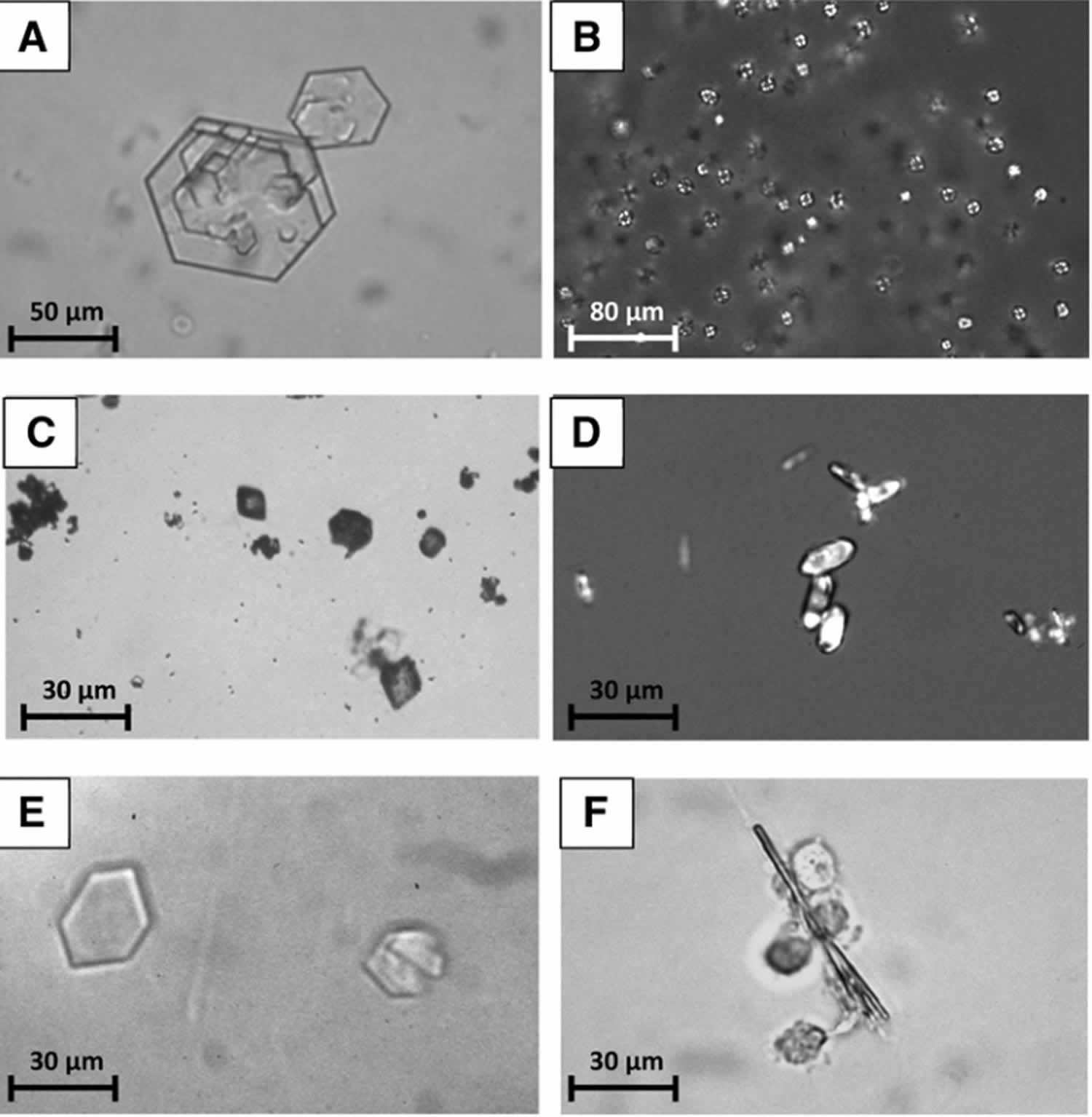
Cystine crystals are pathognomonic of cystinuria, which is a hereditary disease characterized by a proximal tubular dysfunction due to mutations on genes coding for the transporter of dibasic amino acids. Cystine crystals present as hexagonal plates, often irregular, either isolated or in large aggregates (Figure 5A).
Figure 5. Uncommon crystals in urine
Footnote: (A) Cystine crystals. (B) 2,8-dihydroxyadenine crystals as seen by polarized light. (C) Diamond-shaped crystal of N-acetylsulfamethoxazole hydrochloride very similar to uric acid dihydrate crystals. (D) Oval-shaped crystal of N-acetylsulfamethoxazole hydrochloride very similar to whewellite. (E) Hexagonal crystals of N-acetylsulfamethoxazole hydrochloride that may easily be misidentified as cystine crystals. (F) Needle-shaped crystals of atazanavir surrounded by leukocytes.
[Source 2 ]2,8-Dihydroxyadenine crystals in urine
The inherited condition of adenine phosphoribosyltransferase deficiency can be diagnosed by the identification of crystals in urine. In fact, in virtually all untreated patients, characteristic spherical crystals of 2,8-dihydroxyadenine which under polarized light appear as a black Maltese cross, are observed in urine (see Figure 5B above). However, as these crystals can be confused with other spherical crystals such as ammonium hydrogen urate, in suspected cases the investigation with infrared spectroscopy on a centrifuged pellet is mandatory. The same approach is advisable for patients presenting with acute kidney injury due to massive precipitation of 2,8-dihydroxyadenine crystals within the renal tubules [20], in whom only few and atypical crystals can be found in the urine 24.
Xanthine crystals in urine
Xanthine crystals, which are found in xanthinuria, a rare genetic disorder caused by the deficiency of the enzyme xanthine oxidase, present as polarizing granules or sticks without a characteristic aspect. Therefore infrared analysis is required for accurate identification. Tyrosine, leucine or potassium orotate crystals can also be found in urine. However, since they are associated with rare metabolic disease 25, they are an uncommon finding.
Crystals in urine due to drugs
Several drugs, mainly antimicrobial or antiviral agents, may crystallize in urine when used at high dose and/or for long periods 26. Some sulfonamides may induce crystalluria. Among them, N-acetylsulfamethoxazole chlorhydrate, a metabolite of sulfamethoxazole which is widely used in combination with trimethoprim. Crystals, which precipitate at a pH around 5.0, may have the shape of lozenges, hexagons or ovoid structures, which may mimic uric acid dihydrate, cystine or whewellite, respectively (see Figure 5C–E above). N-acetylsulfadiazine, a metabolite of sulfadiazine used in the treatment of cerebral toxoplasmosis, also crystallizes in acidic urine. For an accurate identification of these crystals, infrared spectroscopy is recommended 27.
Occasionally, other antibacterial agents such as aminopenicillines, particularly amoxicilline 28, fluoroquinolones 29 and, more rarely, ceftriaxone may induce crystalluria, which at times may be associated with acute kidney injury due to the intratubular precipitation of crystals.
Antiviral agents currently are a common cause of crystalluria, especially atazanavir 30, an antiprotease widely used in combination therapy in AIDS patients, which form very large bundles of drug needles (150–250 μm or more) (see Figure 5F above). Acyclovir, used in the treatment of herpes virus infections, also forms crystals with an aspect of long, thin needles that may form aggregates.
Other drugs which may cause crystalluria are the inhibitor of HIV-1 protease indinavir, the potassium-sparing diuretic triamterene, the barbiturate primidone, and the antiepileptic felbamate, whose crystals have most unusual and pleomorphic morphologies, a fact which should alert the urine microscopist. Other drugs such as the vasodilator naftidrofuryl oxalate, the gastrointestinal lipase inhibitor orlistat and vitamin C, when given intravenously at high doses, may also cause urinary crystals, which are made up of calcium oxalate undistinguishable from calcium oxalate crystals from other causes 25.
Sulfadiazine, acyclovir, indinavir, triamterene, and MTX are known to cause crystal nephropathy. Recently, several medications, including orlistat, ciprofloxacin, and oral sodium phosphate solution, along with underlying risk factors have been described as causing crystal nephropathy 31.
Crystals in urine symptoms
Symptoms of a kidney stone may include:
- Sharp pains in your abdomen, side, or groin
- Back pain
- Blood in your urine
- Frequent urge to urinate
- Pain when urinating
- Cloudy or bad-smelling urine
- Nausea and vomiting
- Crystalluria: a neglected aspect of urinary sediment analysis. Nephrol Dial Transplant. 1996 Feb;11(2):379-87. https://www.ncbi.nlm.nih.gov/pubmed/8671802
- Crystalluria. Clin Chem Lab Med 2015; 53(Suppl): S1479–S1487 https://doi.org/10.1515/cclm-2015-0860
- Ethylene glycol intoxication: evaluation of kinetics and crystalluria. Am J Med. 1988 Jan;84(1):145-52. https://www.ncbi.nlm.nih.gov/pubmed/3337119
- Clinical value of crystalluria study. [Article in French] Ann Biol Clin (Paris). 2004 Jul-Aug;62(4):379-93. https://www.ncbi.nlm.nih.gov/pubmed/15297232
- M. Daudon, C. Hennequin, G. Boujelben, B. Lacour, P. Jungers. Serial crystalluria determination and the risk of recurrence in calcium stone formers. Kidney Int., 67 (2005), pp. 1934-1943
- M. Daudon, F. Cohen-Solal, F. Barbey, M.F. Gagnadoux, B. Knebelmann, P. Jungers. Cystine crystal volume determination: a useful tool in the management of cystinuric patients. Urol. Res., 31 (2003), pp. 207-211
- P. Jouvet, L. Priqueler, M.F. Gagnadoux, D. Jan, A. Beringer, F. Lacaille, et al. Crystalluria: a clinical useful investigation in children with primary hyperoxaluria post-transplantation. Kidney Int., 53 (1998), pp. 1412-1416
- P. Cochat, S.A. Hulton, C. Acquaviva, C.J. Danpure, M. Daudon, M. De Marchi, et al. Primary hyperoxaluria Type 1: indications for screening and guidance for diagnosis and treatment. Nephrol. Dial. Transpl., 27 (2012), pp. 1729-1736
- M.F. Gagnadoux, F. Lacaille, P. Niaudet, Y. Revillon, P. Jouvet, D. Jan, et al. Long term results of liver-kidney transplantation in children with primary hyperoxaluria. Pediatr. Nephrol., 16 (2001), pp. 946-950
- Clinical value of crystalluria and quantitative morphoconstitutional analysis of urinary calculi. Int J Surg. 2016 Dec;36(Pt D):624-632. doi: 10.1016/j.ijsu.2016.11.023. Epub 2016 Nov 12. https://doi.org/10.1016/j.ijsu.2016.11.023
- The scientific basis of calcium oxalate urolithiasis, Predilection and precipitation, promotion and proscription. World J. Urol., 11 (1993), pp. 59-65
- Calcium oxalate crystalluria and inhibitors of crystallization in recurrent renal stone-formers. Clin. Sci., 43 (1972), pp. 499-506
- 2,8-dihydroxyadenine nephrolithiasis: from diagnosis to therapy. Ann. Biol. Clin., 65 (2007), pp. 585-592
- Urolithiasis in HIVpositive patients treated with atazanavir. Clin. Infect. Dis., 45 (2007), pp. e105-e108
- Quality control in urinary stone analysis results of 44 ring trials (1980–2001). Clin Chem Lab Med, 43 (2005), pp. 298-303
- A new urinary test for stone “activity”. Br. J. Urol., 50 (1978), pp. 442-448
- M. Robert, A.M. Boularan, O. Delbos, et al. Study of calcium oxalate crystalluria on renal and vesical urines in stone formers and normal subjects. Urol. Int., 60 (1998), pp. 41-46
- Asplin JR, Lingeman J, Kahnoski R, Mardis H, Parks JH, Coe FL. Metabolic urinary correlates of calcium oxalate dihydrate in renal stones. J Urol 1998;159:664–8.
- Kok DJ, Papapoulos SE, Bijvoet OL. Excessive crystal agglomera-tion with low citrate excretion in recurrent stone-formers. Lancet 1986;1:1056–8.
- Daudon M, Hennequin C, Bader C, Jungers P, Lacour B, Drueke T. Inhibitors of crystallization. Adv Nephrol 1995;24:167–216
- M. Daudon, P. Jungers. Stone composition and morphology : a window on etiology. J.J. Talati, H.G. Tiselius, D.M. Albala, Z. Ye (Eds.), Urolithiasis: Basic Science and Clinical Practice, Springer Verlag, London (2012), pp. 113-140
- Daudon M. Modèles de cristallisation. In: Jungers P, Daudon M, Le Duc A, editors. Lithiase urinaire. Paris: Flammarion Médecine-Sciences, 1989:158–95.
- Daudon M, Jungers P, Lacour B. Intérêt clinique de l’étude de la cristallurie. Ann Biol Clin 2004;62:379–93.
- Stratta P, Fogazzi GB, Canavese C, Airoldi A, Fenoglio R, Bozzola C, et al. Decreased kidney function and crystal deposi-tion in the tubules after kidney transplant. Am J Kidney Dis 2010;56:585–90.
- Fogazzi GB. The urinary sediment an integrated view 3rd ed. Milano: Elsevier, 2010.
- Daudon M, Jungers P. Drug-induced renal calculi: epidemiology, prevention and management. Drugs 2004;64:245–75.
- Verdesca S, Fogazzi GB, Garigali G, Messa P, Daudon M. Crystalluria: prevalence, different types of crystals and the role of infrared spectroscopy. Clin Chem Lab Med 2011;49:515–20
- Fogazzi GB, Cantu M, Saglimbeni L, Daudon M. Amoxycillin, a rare but possible cause of crystalluria. Nephrol Dial Transplant 2003;18:212–4.
- Fogazzi G, Garigali G, Brambilla C, Daudon M. Ciprofloxacin crystalluria. Nephrol Dial Transplant 2006;21:2982–3.
- de Lastours V, Ferrari Rafael De Silva E, Daudon M, Porcher R, Loze B, Sauvageon H, et al. High levels of atazanavir and darunavir in urine and crystalluria in asymptomatic patients. J Antimicrob Chemiother 2013;68:1850–6
- Drug-induced crystal nephropathy: an update. Expert Opin Drug Saf. 2008 Mar;7(2):147-58. doi: 10.1517/14740338.7.2.147 https://www.ncbi.nlm.nih.gov/pubmed/18324877