Disorders of consciousness
Disorder of consciousness also called impaired consciousness, is a state where consciousness has been affected by damage to the brain.
The main disorders of consciousness are:
- Coma
- Vegetative state
- Minimally conscious state
Consciousness requires both wakefulness and awareness.
Wakefulness is the ability to open your eyes and have basic reflexes such as coughing, swallowing and sucking.
Awareness is associated with more complex thought processes and is more difficult to assess. Currently, the assessment of awareness relies on physical responses being detected during an examination.
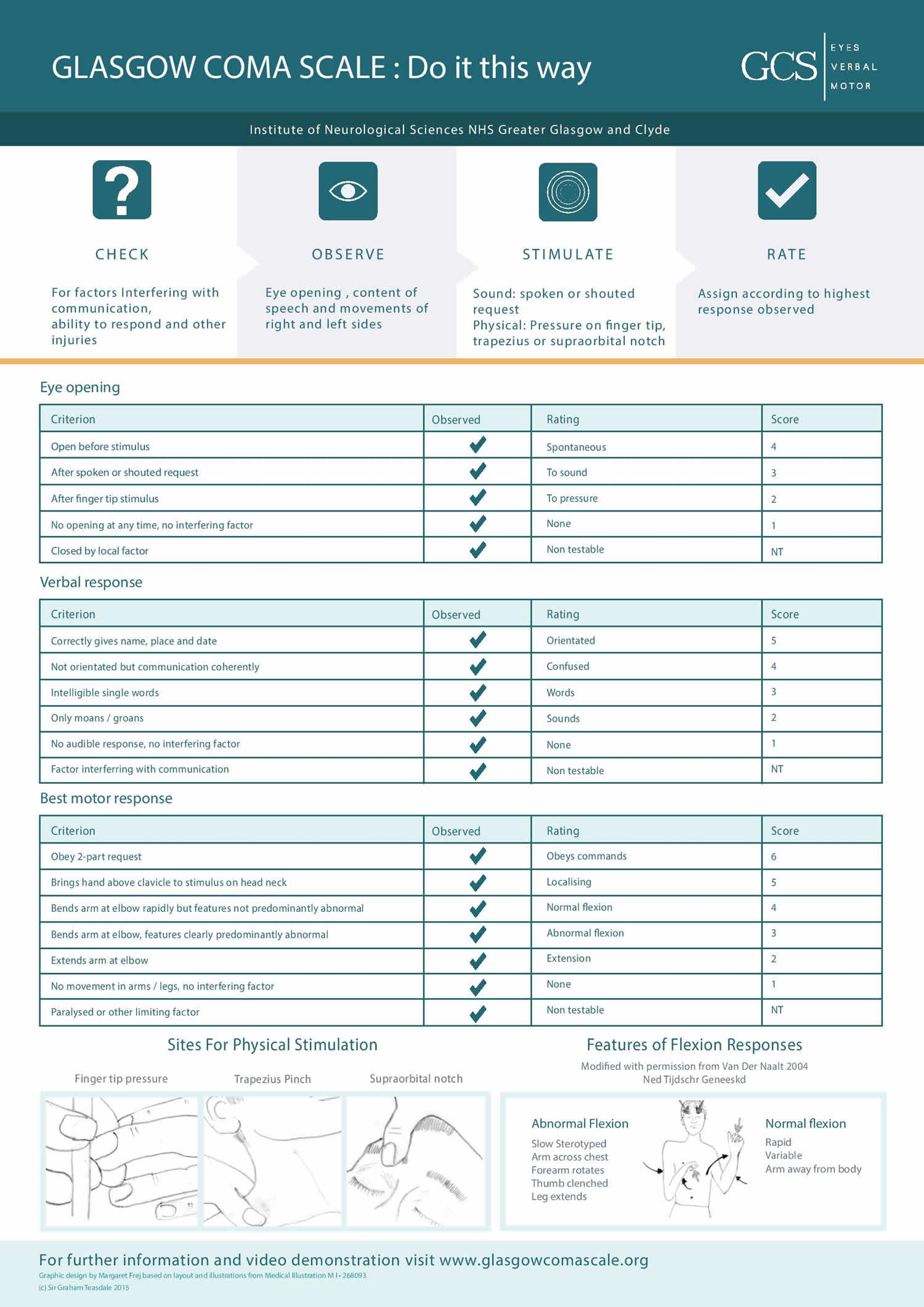
Doctors assess a person’s level of consciousness using a tool called the Glasgow Coma Scale or GCS, a neurological scale that aims to give a reliable, objective way of recording the general level of consciousness in patients with traumatic brain injury (TBI) and to to help gauge the severity of an acute brain injury 1. A person’s level of consciousness is monitored constantly for signs of improvement or deterioration. The Glasgow Coma Scale (GCS) assesses three things:
- Eye opening (E) – a score of 1 means no eye opening, and 4 means opens eyes spontaneously
- Verbal response to a command (V) – a score of 1 means no response, and 5 means alert and talking
- Voluntary movements in response to a command (M) – a score of 1 means no response, and 6 means obeys commands
The Glasgow Coma Scale score is determined by the sum of the score in each of the 3 categories, with a maximum score of 15 and a minimum score of 3, as follows:
- Glasgow Coma Scale score = eye opening (E) + motor response (M) + verbal response (V)
Based on motor responsiveness, verbal performance, and eye opening to appropriate stimuli, the Glascow Coma Scale was designed and should be used to assess the depth and duration coma and impaired consciousness. Glasgow Coma Scale helps to gauge the impact of a wide variety of conditions such as acute brain damage due to traumatic and/or vascular injuries or infections, metabolic disorders (e.g., hepatic or renal failure, hypoglycemia, diabetic ketosis), etc. Education is necessary to the proper application of the Glasgow Coma Scale 2. The predictive value of the GCS, even when applied early, is limited 3. Despite these and other limitations 4, health care practitioners continue to use Glasgow Coma Scale widely.
Glasgow Coma Scale was initially used to assess level of consciousness after head injury, and the Glasgow Coma Scale is now used by first aid, emergency medical services, and doctors as being applicable to all acute medical and trauma patients. In hospitals it is also used in monitoring chronic patients in the intensive care. The Glasgow Coma Scale was published in 1974 by Graham Teasdale and Bryan J. Jennett, professors of neurosurgery at the University of Glasgow’s Institute of Neurological Sciences at the city’s Southern General Hospital 5.
Eye Opening Response (E)
- Spontaneous–open with blinking at baseline = 4 points
- To verbal stimuli, command, speech = 3 points
- To pain only (not applied to face) = 2 points
- No response = 1 point
Verbal Response (V)
- Oriented conversation = 5 points
- Confused conversation, but able to answer questions = 4 points
- Inappropriate words = 3 points
- Incomprehensible speech or sounds = 2 points
- No response = 1 point
Motor Response (M)
- Obeys verbal commands for movement = 6 points
- Purposeful movement to painful stimuli = 5 points
- Withdraws in response to painful stimuli = 4 points
- Flexion in response to painful stimuli (decorticate posturing) = 3 points
- Extension response in response to painful stimuli (decerebrate posturing) = 2 points
- No response = 1 point
Total Glasgow Coma Scale score = 15
- Total Glasgow Coma Scale score 15 is Normal
- Total Glasgow Coma Scale score 3-14 is Abnormal
The Glasgow Coma Scale is often used to help define the severity of traumatic brain injury (TBI). Mild head injuries are generally defined as those associated with a GCS score of 13-15, and moderate head injuries are those associated with a GCS score of 9-12. A GCS score of 8 or less defines a severe head injury. These definitions are not rigid and should be considered as a general guide to the level of injury.
Every brain injury is different, but generally, brain injury is classified as:
- Severe Head Injury: Glasgow Coma Score 8 or less
- Moderate Head Injury: Glasgow Coma Score 9-12
- Mild Head Injury: Glasgow Coma Score 13-15
Mild brain injuries can result in temporary or permanent neurological symptoms and neuroimaging tests such as CT scan or MRI may or may not show evidence of any damage.
Moderate and severe brain injuries often result in long-term impairments in cognition (thinking skills), physical skills, and/or emotional/behavioral functioning.
Brain injury is classified as:
- Glasgow Coma Scale 8-15 and somnolence: Sleepy, easy to wake
- Glasgow Coma Scale 8-15 and stupor: Hypnoid, hard to wake
- Glasgow Coma Scale 13-15: Mild Head Injury
- Glasgow Coma Scale 9–12: Moderate Head Injury
- Glasgow Coma Scale 3–8: Coma = No eye opening, no ability to follow commands and no word verbalizations
- Glasgow Coma Scale ≤ 8: Severe Head Injury
- Glasgow Coma Scale 7-8: Light coma; Coma Grade I
- Glasgow Coma Scale 5-6: Light coma; Coma Grade II
- Glasgow Coma Scale 4: Deep coma; Coma Grade III
- Glasgow Coma Scale 3: Deep coma; Coma Grade IV
Limitations of the Glasgow Coma Scale
Factors like drug use, alcohol intoxication, shock, or low blood oxygen can alter a patient’s level of consciousness. These factors could lead to an inaccurate score on the Glasgow Coma Scale.
Disorders of consciousness causes
Disorders of consciousness can occur if the parts of the brain involved with consciousness are damaged.
These types of brain injury can be divided into:
- Traumatic brain injury (TBI) – traumatic brain injury occurs when an object or outside force causes severe trauma to the brain. traumatic brain injury is most often caused by car accident, a fall from a great height or violent assault
- Non-traumatic brain injury – where the injury to the brain is caused by a health condition, such as a stroke, heart attacks, severe brain infections (such as meningitis, an infection of the outer layer of the brain, or encephalitis, an infection of the brain itself), drug overdoses, poisoning, almost drowning or other types of suffocation, such as smoke inhalation, a blood vessel bursting leading to bleeding inside the brain (the medical term for this is a ruptured aneurysm)
- Progressive brain damage – where the brain is gradually damaged over time (for example, because of Alzheimer’s disease, Parkinson’s disease or a brain tumor)
Disorders of consciousness diagnosis
It takes extensive testing to assess levels of wakefulness and awareness before a disorder of consciousness can be confirmed. This may involve tests such as brain scans, but is largely based on the specific features a person displays, such as whether they can respond to commands.
Glasgow Coma Scale
Doctors can score a person’s level of consciousness using a tool called the Glasgow Coma Scale (GCS).
Glasgow Coma Scale (GCS) assesses 3 things:
- Eye opening (E) – a score of 1 means the person doesn’t open their eyes at all, and 4 means they open their eyes spontaneously
- Verbal response to a command (V) – 1 means no response, and 5 means a person is alert and talking
- Voluntary movements in response to a command (M) – 1 means no response, and 6 means a person can follow commands
A lower GCS score indicates a more severely impaired consciousness, such as a coma, although this level will be monitored regularly to look for any changes.
Other scoring systems
There are also more specific scoring systems based on more detailed observations of a person’s behavior.
One example is known as the JFK Coma Recovery Scale-Revised (CRS-R). This system uses 23 different items, each with individual scales to assess how a person is responding.
Brain scans
Brain scans are used to help assess the level of brain damage in someone with impaired consciousness. They can also check for signs of any complications, such as hydrocephalus, a build-up of fluid on the brain. There are several types of scans that can assess brain structure.
A CT scan or an MRI scan are used if the person is able to tolerate it.
Research brain scans
There are separate scans that can show areas of brain activity as well as brain damage. These are only used in research settings at the moment, but may be useful if a person can’t move or speak. One example is a functional magnetic resonance (fMRI) scan. An fMRI scan is able to show changes if the brain is responding to light and sounds. But they don’t necessarily show awareness, as the brain is able to respond to stimulation even without the person actually being aware of it. Research is being carried out into ways brain scans can be used to show true awareness.
Coma
A coma is a state of unconsciousness where a person shows no signs of being awake and no signs of being aware. Someone who is in a coma is unconscious and has minimal brain activity. A person in a coma lies with their eyes closed and doesn’t respond to their environment, voices or pain or be able to communicate or move voluntarily, and basic reflexes, such as coughing and swallowing, are be greatly reduced. They may be able to breathe on their own, although some people require a machine to help them breathe. Complications may develop during a coma, including pressure sores, bladder infections, blood clots in the legs and other problems.
Over time, the person may start to gradually regain consciousness and become more aware. A coma usually lasts for less than 2 to 4 weeks, during which time a person may wake up or progress into a vegetative state or minimally conscious state.
A coma can result from injury to the brain, such as a severe head injury or stroke. A coma can also be caused by severe alcohol poisoning or a brain infection (encephalitis).
People with diabetes could fall into a coma if their blood glucose levels suddenly became very low (hypoglycemia) or very high (hyperglycemia).
Most people in a coma will have a total Glasgow Coma Scale (GCS) score of 8 or less. A lower score means someone may have experienced more severe brain damage and could be less likely to recover.
In the short term, a person in a coma will normally be looked after in an intensive care unit (ICU). Treatment involves ensuring their condition is stable and body functions, such as breathing and blood pressure, are supported while the underlying cause is treated.
In the longer term, healthcare staff will give supportive treatment on a hospital ward. This can involve providing nutrition, trying to prevent infections, moving the person regularly so they don’t develop bedsores and gently exercising their joints to stop them becoming tight.
Coma causes
Many types of problems can cause coma. Some examples are:
- Traumatic brain injuries (TBI). Traumatic brain injuries, often caused by traffic collisions or acts of violence, are common causes of comas.
- Stroke. Reduced or interrupted blood supply to the brain (stroke), which may be caused by blocked arteries or a burst blood vessel, can result in a coma.
- Tumors. Tumors in the brain or brainstem can cause a coma.
- Diabetes. In people with diabetes, blood sugar levels that become too high (hyperglycemia) or too low (hypoglycemia) can cause a coma.
- Lack of oxygen. People who have been rescued from drowning or those who have been resuscitated after a heart attack may not awaken due to lack of oxygen to the brain.
- Infections. Infections such as encephalitis and meningitis cause swelling (inflammation) of the brain, spinal cord or the tissues that surround the brain. Severe cases of these infections can result in brain damage or a coma.
- Seizures. Ongoing seizures may lead to a coma.
- Toxins. Exposure to toxins, such as carbon monoxide or lead, can cause brain damage and a coma.
- Drugs and alcohol. Overdosing on drugs or alcohol can result in a coma.
Coma symptoms
The signs and symptoms of a coma commonly include:
- Closed eyes
- Depressed brainstem reflexes, such as pupils not responding to light
- No responses of limbs, except for reflex movements
- No response to painful stimuli, except for reflex movements
- Irregular breathing
Coma diagnosis
Because people in a coma can’t express themselves, doctors must rely on physical clues and information provided by families and friends. Be prepared to provide information about the affected person, including:
- Events leading up to the coma, such as vomiting or headaches
- Details about how the affected person lost consciousness, including whether it occurred suddenly or over time
- Any noticeable signs or symptoms prior to losing consciousness
- The affected person’s medical history, including other conditions he or she may have had in the past, such as a stroke or transient ischemic attacks
- Recent changes in the affected person’s health or behavior
- The affected person’s drug use, including prescription and over-the-counter medications as well as unapproved medications or illegal, recreational drugs
Physical exam
In a physical exam, doctors will check the affected person’s movements and reflexes, response to painful stimuli, and pupil size. Doctors will observe breathing patterns to help diagnose the cause of the coma. Doctors also may check the skin for signs of any bruises due to trauma.
To determine the affected person’s level of consciousness, doctors may speak loudly or press on the angle of the jaw or nail bed. Doctors will watch for signs of arousal, such as vocal noises, eyes opening or movement.
Doctors will test reflexive eye movements. These tests can help determine the cause of the coma and the location of brain damage.
Doctors also may squirt ice-cold or warm water into the affected person’s ear canals and observe eye reactions.
Laboratory tests
Blood samples will be taken to check for:
- Complete blood count (CBC)
- Electrolytes, glucose, thyroid, kidney and liver function
- Carbon monoxide poisoning
- Drug or alcohol overdose
A spinal tap (lumbar puncture) can check for signs of infections in the nervous system. During a spinal tap, a doctor or specialist inserts a needle into the spinal canal and collects a small amount of fluid for analysis.
Brain scans
Imaging tests help doctors pinpoint areas of brain injury. Tests may include:
- Computerized tomography (CT) scan. A CT scan uses a series of X-rays to create a detailed image of the brain. A CT scan can show a brain hemorrhage, tumors, strokes and other conditions. This test is often used to diagnose and determine the cause of a coma.
- Magnetic resonance imaging (MRI). An MRI uses powerful radio waves and magnets to create a detailed view of the brain. An MRI can detect brain tissue damaged by an ischemic stroke, brain hemorrhages and other conditions. MRI scans are particularly useful for examining the brainstem and deep brain structures.
- Electroencephalography (EEG). An EEG measures the electrical activity inside the brain. Doctors attach small electrodes to the scalp. Doctors send a low electrical current through the electrodes. The brain’s electrical impulses are then recorded. This test can determine if seizures may be the cause of a coma.
Coma treatment
A coma is a medical emergency. Doctors will first check the affected person’s airway and help maintain breathing (respiration) and circulation. Doctors may give breathing assistance, blood transfusions and other supportive care.
Emergency personnel may administer glucose or antibiotics intravenously, even before blood test results return, in case of diabetic shock or an infection affecting the brain.
Treatment varies, depending on the cause of the coma. A procedure or medications to relieve pressure on the brain due to brain swelling may be needed.
If the coma is the result of drug overdose, doctors will give medications to treat the condition. If the coma is due to seizures, doctors will administer medications to control seizures.
Other treatments may focus on medications or therapies to address an underlying disease, such as diabetes or liver disease.
Sometimes the cause of a coma can be completely reversed and the affected person will regain normal function. But if the affected person has suffered severe brain damage, he or she may sustain permanent disabilities or may never regain consciousness. The person may enter a persistent vegetative state or become brain dead.
Recovering from a coma
A coma usually only lasts a few weeks, during which time the person may start to gradually wake up and gain consciousness, or progress into a different state of unconsciousness called a vegetative state or minimally conscious state.
- a vegetative state – where a person is awake but shows no signs of being aware of their surroundings or themselves
- a minimally conscious state – where a person has limited awareness that comes and goes
Some people may recover from these states gradually, while others may not improve for years, if at all.
People who do wake up from a coma usually come round gradually. They may be very agitated and confused to begin with.
Some people will make a full recovery and be completely unaffected by the coma. Others will have disabilities caused by the damage to their brain. They may need physiotherapy, occupational therapy and psychological assessment and support during a period of rehabilitation, and may need care for the rest of their lives.
The chances of someone recovering from a coma largely depend on the severity and cause of their brain injury, their age and how long they’ve been in a coma. But it’s impossible to accurately predict whether the person will eventually recover, how long the coma will last and whether they’ll have any long-term problems.
Vegetative state
Vegetative state also called unresponsive wakefulness syndrome, is when a person is awake but is showing no signs of awareness. On recovery from the coma state, vegetative state is characterized by the return of arousal without signs of awareness. In contrast, a coma is a state that lacks both awareness and wakefulness. Absence of awareness can only be inferred by lack of responsiveness to the environment and not as lack of consciousness that we may not be able to detect by behavioral measures. For this reason, many authors have suggested that the term ‘Unresponsive Wakefulness Syndrome’ 6 or ‘post-coma unresponsiveness’ are more accurate descriptive terms for vegetative state.
A person in a vegetative state may:
- open their eyes
- wake up and fall asleep at regular intervals
- have basic reflexes (such as blinking when they’re startled by a loud noise or withdrawing their hand when it’s squeezed hard)
They’re also able to regulate their heartbeat and breathing without assistance.
But a person in a vegetative state doesn’t show any meaningful responses, such as following an object with their eyes or responding to voices. They also show no signs of experiencing emotions nor of cognitive function.
Vegetative state patients’ eyes might be in a relatively fixed position, may track moving objects (visual pursuit), or move in a completely unsynchronized manner. Sleep-wake cycles may resume or patients may appear to be in a state of chronic wakefulness. They may grind their teeth, swallow, smile, shed tears, grunt, moan, or scream without any apparent external stimulus. vegetative state patients do not respond to sound, hunger, or pain. Patients cannot obey verbal commands and lack local motor responses. Additionally vegetative state patients cannot talk in comprehensible terms and may become noisy, restless, and hypermobile.
One of the most challenging tasks facing clinicians is that of differentiating vegetative state from minimally conscious (vegetative state) states.
Whilst neuroimaging such as MRI is widely used in assessing brain damage and functional abilities, behavioral assessment has, until now, been the “gold standard” for detecting signs of consciousness and thereby for determining diagnosis.
If a person is in a vegetative state for a long time, it may be considered to be:
- a continuing vegetative state when it’s been longer than 4 weeks
- a permanent vegetative state when it’s been more than 6 months if caused by a non-traumatic brain injury, or more than 12 months if caused by a traumatic brain injury
If a person is diagnosed as being in a permanent vegetative state, recovery is extremely unlikely but not impossible.
Criteria for vegetative state
A vegetative state is when a person is awake but showing no signs of awareness.
Doctors are particularly careful when diagnosing a permanent vegetative state, as there’s a risk of misdiagnosis.
A confident diagnosis can only be made if the following criteria have been met:
- the cause of the brain injury has been established (for example, if a case of meningitis is suspected, a diagnosis can be confirmed by testing the fluid that surrounds the brain for infection)
- it’s been confirmed drugs or medication aren’t responsible for the symptoms
- it’s been confirmed treatable problems with the body’s chemistry (a metabolic disorder) aren’t responsible for the symptoms of loss of awareness (an example of a metabolic disorder is a diabetic coma, where people lose consciousness because their blood sugar levels are either dangerously high or dangerously low)
- the possibility of a treatable cause in the brain, such as a brain tumour, has been ruled out by brain imaging scans
- examinations have been carried out by a trained assessor experienced in prolonged disorders of consciousness
For a permanent vegetative state to be confirmed, the above criteria must apply and either:
- 6 months must have passed since the start of symptoms after a non-traumatic brain injury
- 12 months must have passed since the start of symptoms after a traumatic brain injury
Vegetative state treatment
Careful, ongoing assessment of the patient, using empirically validated assessment tools (eg the Coma Recovery Scale-Revised) is essential in order to evaluate and measure signs of progress, improvement or deterioration. Treatment is addressed at presenting symptoms and the patient’s needs; vegetative state patients require constant monitoring and assistance with feeding, hydration, hygiene, assisted movement and physical therapies (to help prevent ulcers and blood clots in the legs), and elimination of waste products.
Currently no treatment for vegetative state exists that would satisfy the efficacy criteria of evidence-based medicine. Pharmacological methods, surgery, physical therapy, and various stimulation techniques have been suggested. Pharmacological therapy mainly uses activating substances such as tricyclic antidepressants or methylphenidate 7. Surgical methods (eg. deep brain stimulation) are used infrequently due to the invasiveness of the procedures. Stimulation techniques include sensory stimulation, sensory regulation, music and musicokinetic therapy, social-tactile interaction, etc.
Treatment can’t ensure recovery from a state of impaired consciousness, however supportive treatment is used to give the best chance of natural improvement. This can involve:
- providing nutrition through a feeding tube
- making sure the person is moved regularly so they don’t develop pressure ulcers
- gently exercising their joints to prevent them becoming tight
- keeping their skin clean
- managing their bowel and bladder – for example, using a catheter to drain the bladder
- keeping their teeth and mouth clean
- efforts should be made to establish functional communication and environmental interaction when possible. Offering opportunities for periods of meaningful activity – such as listening to music or watching television, being shown pictures or hearing family members talking
Sensory stimulation:
- visual – showing photos of friends and family, or a favorite film
- hearing – talking or playing a favorite song
- smell – putting flowers in the room or spraying a favorite perfume
- touch – holding their hand or stroking their skin with different fabrics
While not empirically validated, families have reported benefits from arousal regimes, such as those implemented by Dr Ted Freeman (e.g., Coma Arousal Therapy). This intensive therapy involves family members taking the patient through a regimen of controlled auditory, visual and physical stimulation for up to six hours a day every day.
Vegetative state prognosis
Many patients emerge spontaneously from vegetative state within a few weeks. Some people improve gradually, whereas others stay in a state of impaired consciousness for years. Many people never recover consciousness.
The chances of recovery depend on the extent of injury to the brain and age, with younger patients having a better chance of recovery than older patients. Generally, adults have about a 50 percent chance and children a 60 percent chance of recovering consciousness from vegetative state within the first 6 months in the case of traumatic brain injury. For non-traumatic injuries such as strokes, the recovery rate falls within the first year. After this period the chances that vegetative state patient will regain consciousness are very low and, of those patients who do recover consciousness, most experience significant disability. The longer a patient is in vegetative state the more severe the resulting disabilities are likely to be.
Some patients who have entered a vegetative state go on to regain a degree of awareness (see Minimally Conscious State). The likelihood of significant functional improvement for vegetative state patients diminishes over time. There are only isolated cases of people recovering consciousness after several years. The few people who do regain consciousness after this time often have severe disabilities caused by the damage to their brain.
Minimally conscious state
A person who shows clear but minimal or inconsistent awareness is classified as being in a minimally conscious state. The minimally conscious state is a defined as severely altered consciousness in which minimal but definite, sustained and/or reproducible behavioral evidence of awareness of self or environment is demonstrated.
A person in a minimally conscious state may have periods where they can communicate or respond to commands, such as moving a finger when asked.
A person may enter a minimally conscious state after being in a coma or vegetative state. In some cases a minimally conscious state is a stage on the route to recovery, but in others it’s permanent.
As with vegetative state, a continuing minimally conscious state means it’s lasted longer than 4 weeks.
However, it’s more difficult to diagnose a permanent minimally conscious state because it depends on things like:
- the type of brain injury
- how severe the injury is
- how responsive the person is
In most cases, a minimally conscious state isn’t usually considered to be permanent until it’s lasted several years.
To make the diagnosis of minimally conscious state, limited but clearly discernible evidence of self or of environmental awareness must be demonstrated on a reproducible or sustained basis by one or more of the following behaviors:
- Follow simple commands (eg touch your nose, look up).
- Gestural or verbal yes/no responses (regardless of accuracy).
- Intelligible verbalization.
- Purposeful behavior that is not due to reflexive activity. For example, appropriate smiling or crying in response to emotional but not to neutral topics or stimuli – reaching for objects demonstrating a clear relationship between object location and direction of reach – touching or holding objects appropriately in relation to the size and shape of the object – pursuit eye movement or sustained fixation that occurs in direct response to moving or salient stimuli.
Minimally conscious state treatment
Treatment can’t ensure recovery from a state of impaired consciousness, however supportive treatment is used to give the best chance of natural improvement. This can involve:
- providing nutrition through a feeding tube
- making sure the person is moved regularly so they don’t develop pressure ulcers
- gently exercising their joints to prevent them becoming tight
- keeping their skin clean
- managing their bowel and bladder – for example, using a catheter to drain the bladder
- keeping their teeth and mouth clean
- efforts should be made to establish functional communication and environmental interaction when possible. Offering opportunities for periods of meaningful activity – such as listening to music or watching television, being shown pictures or hearing family members talking
Sensory stimulation:
- visual – showing photos of friends and family, or a favorite film
- hearing – talking or playing a favorite song
- smell – putting flowers in the room or spraying a favorite perfume
- touch – holding their hand or stroking their skin with different fabrics
In all circumstances, the patient should be treated with dignity, and caregivers should be cognizant of the patient’s potential for understanding and perception of pain. In early minimally conscious state, prevention of complications and maintenance of bodily integrity should be emphasized because of the likelihood of further improvement. While not empirically validated, families have reported benefits from arousal regimes, such as those implemented by Dr Ted Freeman (e.g., Coma Arousal Therapy). The therapy involves family members taking the coma patient through a regimen of controlled auditory, visual and physical stimulation for up to six hours a day every day.
A person with experience in neurologic assessment of patients with impaired consciousness should be primarily responsible for establishing the diagnosis and prognosis and for coordinating clinical management. An additional opinion of a physician or other professional with particular expertise in the evaluation, diagnosis, and prognosis of patients in minimally conscious state is recommended when the assessment will impact critical management decisions.
Minimally conscious state prognosis
To date, the natural history and long-term outcome of minimally conscious state has not been adequately investigated. minimally conscious state may occur in a variety of neurologic conditions, such as traumatic brain injury, stroke, progressive degenerative disorders, tumors, neurometabolic diseases, and congenital or developmental disorders. Following an acute injury, minimally conscious state can be a transitional or permanent state. Although it is not known how many patients will emerge from minimally conscious state twelve months or more after injury, most patients in minimally conscious state for this length of time remain severely disabled. The likelihood of significant functional improvement for minimally conscious state patients diminishes over time.
References- Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975 Mar 1. 1(7905):480-4.
- Rowley G, Fielding K. Reliability and accuracy of the Glasgow Coma Scale with experienced and inexperienced users. Lancet 1991; 337:535-538
- Waxman K, Sundine MJ, Young RF. Is early prediction of outcome in severe head injury possible? Arch Surg 1991; 126:1237-1242
- Eisenberg HM. Outcome after head injury: Part I: general Considerations, in Becker DP, Povlishock JR (eds): Central Nervous System Trauma Status Report, 1985. Washington, DC: U.S. Government Printing Office, 1988:271-280
- Teasdale G, Jennett B. Assessment of coma and impaired conciousness: a practical scale. Lancet. 1974; 2:81-84.
- Laureys, S., Celesia, G.G., Cohadon, F. et al. Unresponsive wakefulness syndrome: a new name for the vegetative state or apallic syndrome. BMC Med 8, 68 (2010). https://doi.org/10.1186/1741-7015-8-68
- Dolce G., Sazbon L. The Post-traumatic Vegetative State. Stuttgart, Germany: Georg Thieme; 2002.