What is Duane syndrome
Duane syndrome also known as Duane Retraction Syndrome or Stilling-Turk-Duane Syndrome, is a congenital and non-progressive horizontal disorder of eye movement or a strabismus syndrome 1. Strabismus is more commonly known as “crossed eyes” is a visual problem in which the eyes are not aligned properly and point in different directions. Duane syndrome represents 1%–4% of strabismic population; it is more common in females and more common in left eyes 2. Bilaterality is not uncommon, and nearly 10% of the cases are reported to be familial 3.
Duane syndrome is a common form of congenital (present at birth) cranial dysinnervation disorders that was originally described by an American ophthalmologist, Alexander Duane, in 1905 4, that is characterized by some or all of the following 4, 1:
- Complete or less often partial absence of abduction
- Retraction of globe on adduction
- Narrowing of palpebral fissure during adduction (induced ptosis)
- Partial deficiency of adduction
- Oblique movement with attempts at adduction
- Upshoot or downshoot of globe with adduction (Leash Phenomenon)
- Widening of palpebral aperture with abduction
- Deficiency of convergence
Duane Retraction Syndrome results from an absent or dysplastic abducens motor neurons with aberrant innervations of the lateral rectus muscle by the oculomotor nerve 5.
At birth, affected infants have restricted ability to move the affected eye(s) outward (abduction) and/or inward (adduction) 6. In addition, the globe retracts into the orbit with attempted inward eye movement (adduction), accompanied by narrowing of the palpebral fissure. Most individuals with Duane syndrome have strabismus in primary gaze but can use a compensatory head position to align the eyes, and thus can preserve single binocular vision and avoid diplopia. Individuals with Duane syndrome who lack binocular vision are at risk for amblyopia. Approximately 70% of individuals with Duane syndrome have isolated Duane syndrome (i.e., they do not have other detected congenital anomalies).
Amblyopia occurs in approximately 10% of individuals with Duane syndrome 6; these persons are typically a subset of those with Duane syndrome who lack binocular vision. The amblyopia in Duane syndrome responds to standard therapy if detected early; if not treated promptly, the vision loss from amblyopia is irreversible.
Most individuals with isolated Duane syndrome represent simplex cases (i.e., a single occurrence in a family) of unknown cause 6. Isolated Duane syndrome resulting from a heterozygous pathogenic variant in CHN1 gene is inherited in an autosomal dominant manner with incomplete penetrance. A proband with isolated Duane syndrome may have inherited the pathogenic variant or have a de novo variant. Each child of an individual with Duane syndrome resulting from a CHN1 gene pathogenic variant has a 50% chance of inheriting the condition. Prenatal diagnosis is possible for pregnancies at increased risk for isolated Duane syndrome if the pathogenic variant has been identified in an affected family member.
The ocular motility pattern lies in a wide clinical spectrum, and the choice of treatment must be individualized depending on the severity of the clinical findings. There is no perfect method of treatment and no real “cure” in Duane syndrome 7.
Duane syndrome treatment options:
- Correction of refractive errors
- Treatment of amblyopia if any
- Surgical treatment can be indicated for:
- Correction of strabismus and/or abnormal head position
- Increasing versions and hence increasing field of binocular single vision
- Improvement of globe retraction or upshoot and downshoot.
Duane syndrome epidemiology
- Duane syndrome prevalence of about 1/1000 in general population 8
- Females (60%) > Males (40%) 9
- Accounts for up to 4% of all strabismus cases 8
- Most common type of congenital aberrant ocular innervation 8
- ~70% of Duane syndrome cases are isolated 9
- ~30% of Duane syndrome cases are associated with other congenital anomalies 9
- Okihiro’s syndrome: Duane syndrome and radial ray defects 8
- Wildervanck syndrome: Duane syndrome, Klippel-Feil anomaly, and deafness 8
- Moebius: congenital paresis of facial and abducens cranial nerves 8
- Holt-Oram syndrome: abnormalities of the upper limbs and heart 9
- Morning Glory syndrome: abnormalities of the optic disc 9
- Goldenhar syndrome: malformation of the jaw, cheek and ear, usually on one side of the face 9
- ~80% of cases occur unilaterally, with a LE predominance 8
What do experts know about heredity and Duane syndrome?
Most likely, both genetic and environmental factors play a role in the development of Duane syndrome 9. For those cases that show evidence of having a genetic cause, both dominant and recessive forms of Duane syndrome have been found 9. When a gene is dominant, only one gene from one parent is needed for the individual to express it physically. However, when a gene is recessive, a copy of the gene from both parents is needed for expression.
The chromosomal location of the proposed gene for Duane syndrome is currently unknown. Some research shows that more than one gene may be involved. There is evidence that a gene involved in the development of Duane syndrome is located on chromosome 2. Also, deletions of chromosomal material from chromosomes 4 and 8, as well as the presence of an extra marker chromosome thought to be derived from chromosome 22, have been linked to Duane syndrome.
Duane syndrome types
There are 3 types of Duane Retraction Syndrome with multiple subgroups existing. Huber et al. 10 compartmentalized Duane syndrome into three types based on clinical findings and electromyographic recordings.
The clinical features of the 3 types are similar (as listed below) with the following exceptions:
Duane syndrome type 1
Duane syndrome type 1 comprises 75-80% of patients and the affected eye, or eyes, has limited ability to move outward toward the ear, but the ability to move inward toward the nose is normal or nearly so 9. The eye opening narrows and the eyeball pulls in when looking inward toward the nose, however the reverse occurs when looking outward toward the ear. Duane syndrome type 1 occurs most often as a sporadic, non-familial condition but is sometimes inherited. Duane syndrome type 1 can also be a part of several syndromes that include anomalies in other parts of the body 5.
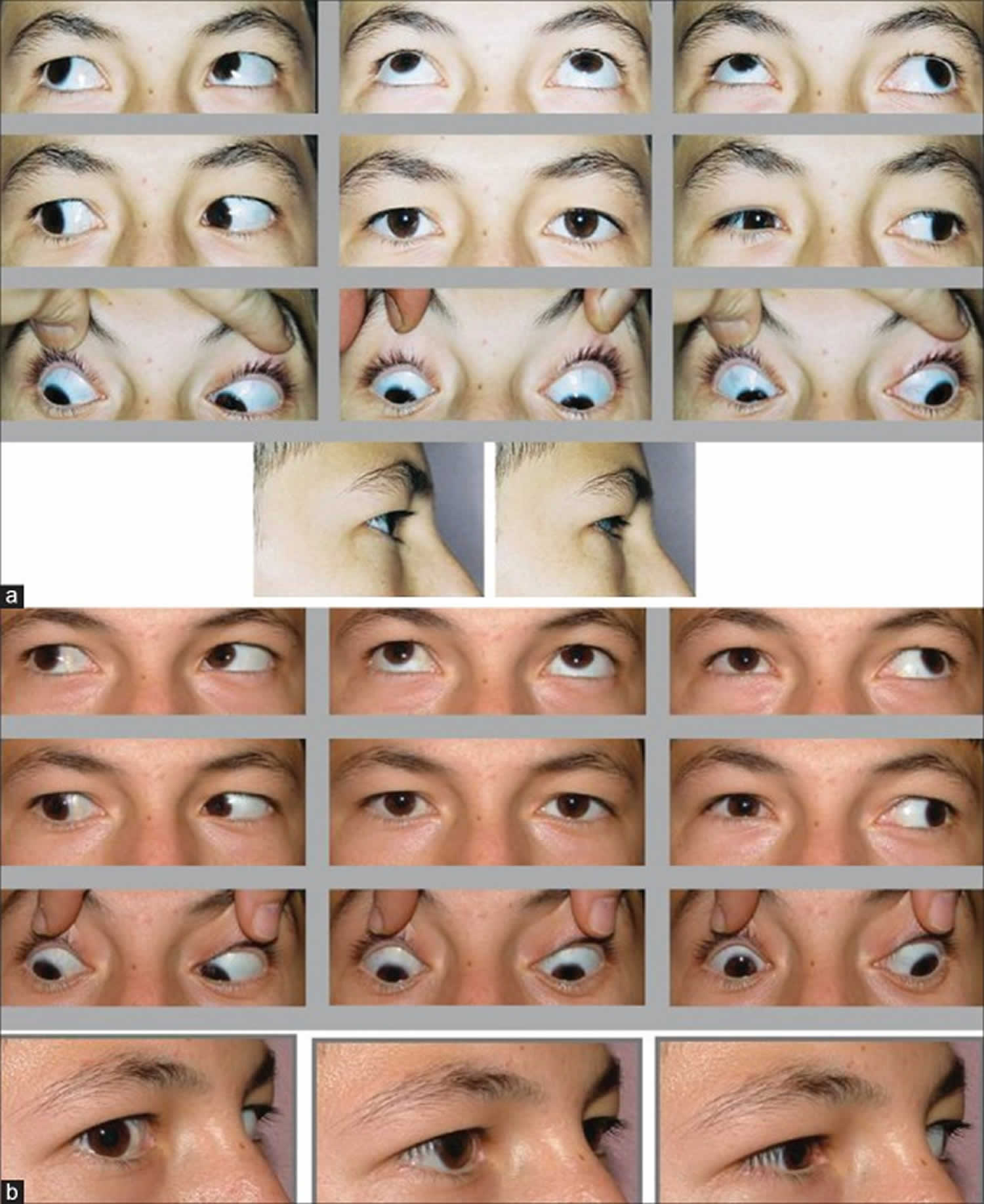
Figure 1. Duane syndrome type 1
Footnote: Left eye Duane Retraction Syndrome type 1 with globe retraction on adduction, upgaze and downgaze. Both vertical rectus muscles were found to have contraction with electromyography on elevation, depression adduction, and abduction
[Source 3 ]Duane syndrome type 2
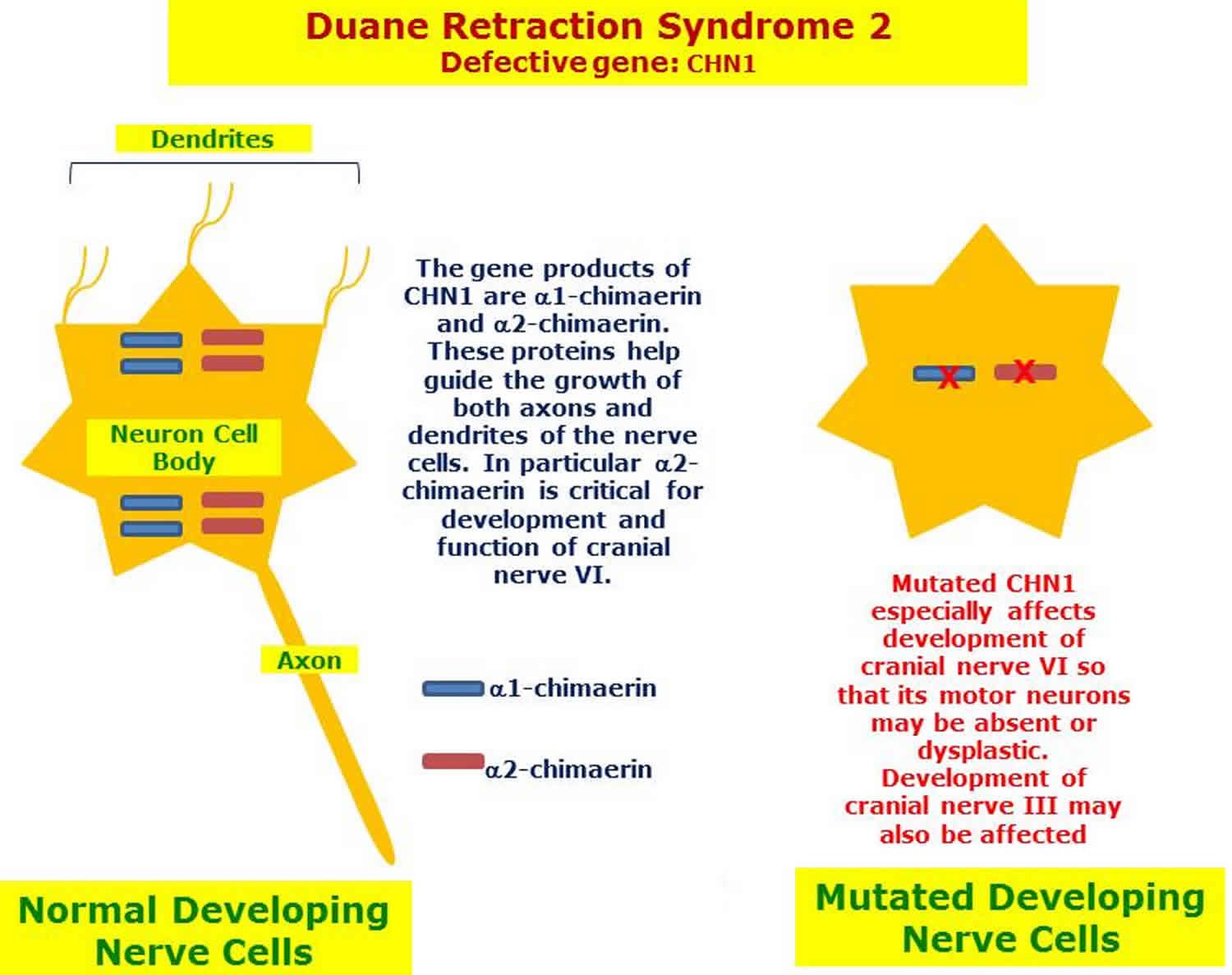
Duane syndrome type 2 comprises 5-10% of patients and the affected eye, or eyes, has limited ability to move inward toward the nose, but the ability to move outward toward the ear is normal or nearly so 9. The eye opening narrows and the eyeball pulls in when looking inward toward the nose. Most Duane syndrome type 2 cases occur sporadically but others are familial and about 30% of affected individuals have other congenital anomalies 11. It is also seen as part of other syndromes such as Goldenhar and Wildervanck 11. In the absence of other anomalies, it is called isolated Duane syndrome. Three heritable types with autosomal dominant familial patterns have also been defined.
Familial isolated Duane syndrome type 2 individuals usually appear in an autosomal dominant pattern of inheritance caused by a mutation in CHN1 (2q31-q32.1) 11. The protein products appear to be involved in early neurological development and are critical to the formation of the cranial nerves that innervate the extraocular muscles.
Mutations in CHN1 are usually absent in nonfamilial cases of Duane syndrome 11.
Figure 2. Duane syndrome type 2
Footnote: (a) Right eye Duane Retraction Syndrome type 2 with up and downshoot and significant globe retraction. (b) Right type 2 after recession of both horizontal recti and Y splitting of lateral rectus muscle. Note the decrease of globe retraction as well as up and downshoot
[Source 3 ]Figure 3. Duane syndrome type 2 genetics
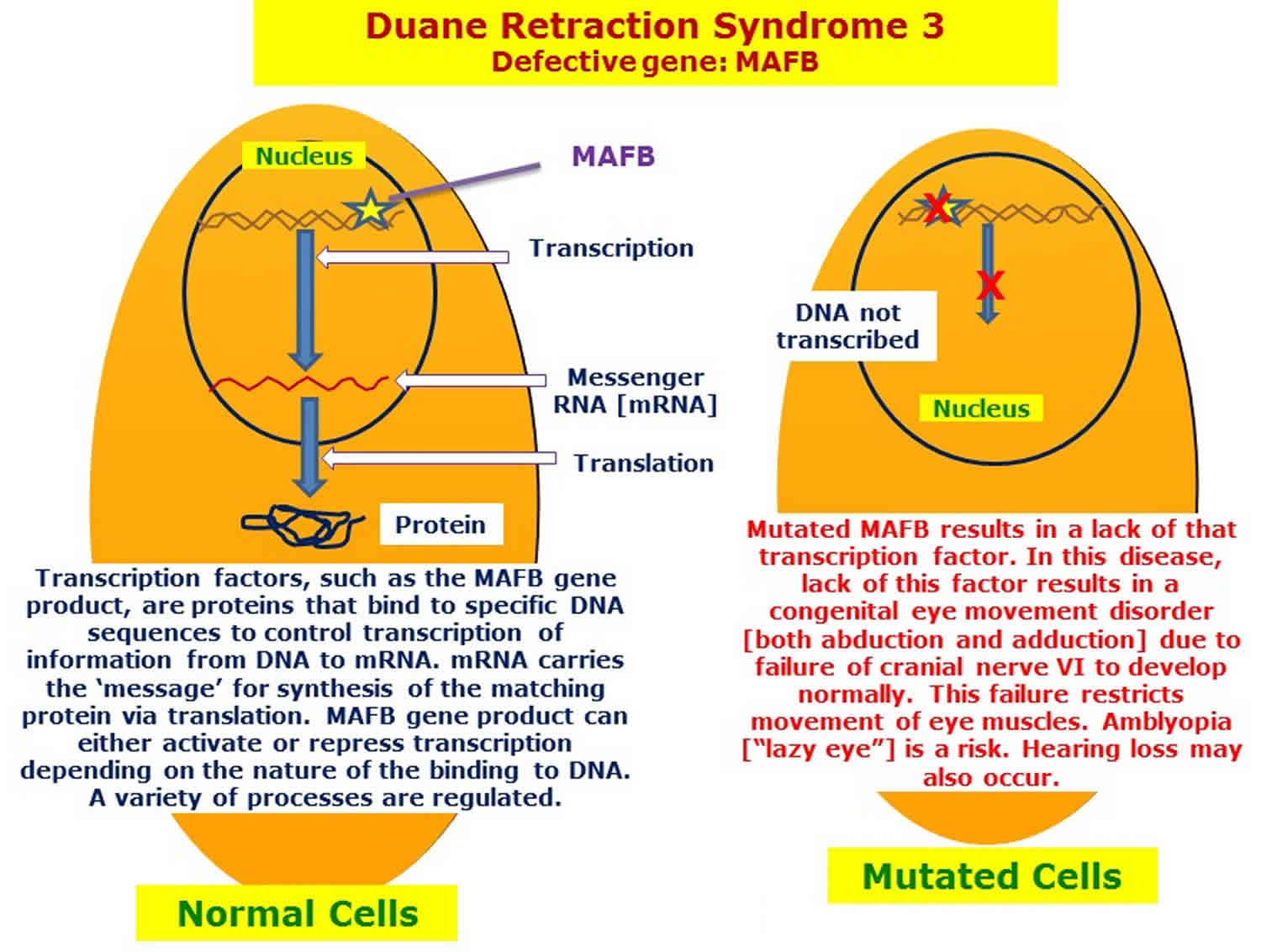
[Source 11 ]Duane syndrome type 3
Duane syndrome type 3 comprises 10-20% of patients, the affected eye, or eyes, has limited ability to move both inward toward the nose and outward toward the ears 9. The eye opening narrows and the eyeball pulls in when looking inward toward the nose and will have a compensatory head turn to the involved side. The ability to adduct in this type is absent to restricted as compared to normal to mildly restricted in types 1 and 2 5.
Sensorineural hearing loss (unilateral or bilateral) may accompany the strabismus profile as reported among 3 of 4 individuals in a single family 12. CT imaging of the temporal bone in one patient revealed a cystic common-cavity anomaly 12.
Duane syndrome type 3 is an autosomal dominant condition resulting from heterozygous mutations in the MAFB gene (20q12) 12. Both single base pair and full gene deletions cause loss of gene function and a dominant-negative effect.
Figure 4. Duane syndrome type 3
Footnote: 31-year-old male presented with history of long-standing globe retraction in the left eye. The patient was diagnosed as having Duane syndrome at the age of 10 months and has been followed by a local ophthalmologist since then. His present concern is globe retraction in the left eye on right gaze and asymmetry of the palpebral fissures on side gazes. There is no history of diplopia in primary gaze.
The left globe retraction especially on attempted right gaze. A mild downshoot of the left eye is also evident in right gaze.
[Source 13 ]Figure 5. Duane syndrome type 3 genetics
Subgroups
Each of these three types can be further classified into three subgroups, depending on where the eyes are when the individual looks straight (the primary gaze):
- Subgroup A: The affected eye is turned inward toward the nose (esotropia).
- Subgroup B: The affected eye is turned outward toward the ear (exotropia).
- Subgroup C: The eyes are in a straight, primary position.
Duane syndrome causes
Common thought is that Duane syndrome is a miswiring of the medial and the lateral rectus muscles, the muscles that move the eyes 9. Also, patients with Duane syndrome lack the abducens nerve, the sixth cranial nerve, which is involved in eye movement. However, the etiology or origin of these malfunctions is, at present, a mystery.
Many researchers believe that Duane syndrome results from a disturbance – either by genetic or environmental factors – during embryonic development. Since the cranial nerves and ocular muscles are developing between the third and eighth week of pregnancy, this is most likely when the disturbance happens.
Presently, it appears that several factors may be involved in causing Duane syndrome. Therefore it is doubtful that a single mechanism is responsible for this condition.
- Myogenic Theory: This theory, suggested by earlier studies, indicates there is fibrosis or inelasticity of the lateral rectus muscles and that the medial rectus muscle inserts abnormally far posteriorly 6.
- Neurogenic Theory: more commonly accepted. Suggested by postmortem studies conducted by M.G. Hotchkiss and coauthors 14 from the John Hopkins University in 1980. A disturbance in embryologic development between weeks 4-8 results in an absent abducens nerve with anomalous innervations of the lateral rectus muscle by a branch of the oculomotor nerve 14. Simultaneous activation of the medial and lateral rectus muscles, as demonstrated by electromyographic (EMG) studies, may be the cause of global retraction 15.
Isolated Duane syndrome
- 90% occur sporadically and are commonly unilateral 8
- Remaining 10% are inherited and these are commonly bilateral with associated vertical movement abnormalities 8:
Syndromic Forms
- Okihiro’s syndrome: Autosomal Dominant (SALL4 mutations) 5
- Goldenhar syndrome: mostly sporadic with both autosomal dominant and recessive forms identified 5
- Wildervanck syndrome: irregularly dominant manner with incomplete penetrance and variable expressivity 4
Risk factors for Duane syndrome
The only known risk factor of an isolated type of Duane Retraction Syndrome is an affected parent, which leads to a 50% chance of passing the gene onto offspring. This risk, however, is only associated with 10% of isolated cases, as 90% of these cases occur sporadically[5]. An affected parent is also a risk factor for the syndromic forms; however, the chance of passing a gene onto offspring varies according to the syndrome.
Duane syndrome prevention
Duane Retraction Syndrome occurs sporadically or is inherited. No means of primary prevention has been identified for this syndrome.
Duane syndrome signs and symptoms
Duane Retraction syndrome is almost always diagnosed early in life with the parents typically noticing the limitation to versions:
- Diplopia
- Strabismus
- Abnormal head position
- Cosmetic concerns: upshoot or downshoot of globe, globe retraction
Signs of Duane Retraction syndrome:
- Strabismus
- Anomalous head position
- Limitation to horizontal versions
- Globe retraction, enophthalmos, pseudo-ptosis
- Upshoot or downshoot of globe
Duane syndrome diagnosis
The diagnosis of Duane Retraction Syndrome is primarily clinical.
Duane syndrome clinical features 1:
- Strabismus: 76% of individuals have frank strabismus in primary gaze
- Limitation of Abduction
- Induced Ptosis on Adduction
- Poor Binocular Vision
- Amblyopia occurs in about 10% of individuals and will respond to standard therapy if detected early
- Anisometropia
- Compensatory Head Turn to Avoid Diplopia
- Good Visual Acuity (except in those with amblyopia)
Molecular genetic testing of CHN1 is available, and is recommended only in familial cases 9. Mutations in the CHN1 gene are associated with familial isolated Duane syndrome 9. Direct sequencing of the CHN1 gene is available as a clinical test, and has to date detected missense mutations in seven patients and affected family members 9. The CHN1 mutations have not been found to be a common cause of simplex Duane retraction syndrome.
Evaluation should include the following 9:
- Family history
- Ophthalmologic examination focusing on primary gaze, head position, extraocular movements, and aberrant movements
- Optional forced duction testing and/or force generation testing
- Photographic documentation for future review
- General physical examination to assess for presence of other associated syndromes, including hearing evaluation.
- Evaluation of family members at risk within the first year of life
- Consider genetics counseling if familial pattern identified
Imaging is not recommended for diagnostic purposes. Brain and orbital MRI can be completed prior to surgical correction for better visualization of orbital anatomy 9.
Duane syndrome treatment
Non-Surgical Management
- Spectacles or contact lenses for refractive error
- Prism glasses to improve the compensatory head position
- Treat amblyopia with standard therapy
- Botulinum Toxin: A study published in the Iranian Journal of Ophthalmology in 2008 investigated the efficacy of injecting botulinum toxin A as a treatment in 4 patients. The results concluded that botulinum toxin decreases the amount of deviation and leash phenomenon (upshoot or downshoot of globe with adduction).
Surveillance
- After diagnosis, ophthalmologic exams are required every 3-6 months to evaluate for amblyopia 6.
- Patients between 7-12 years who are no longer at risk for amblyopia and have good binocular vision can be evaluated annually or biannually 6.
Prevention of secondary complications
Specialist examination early in life to detect refractive errors to prevent amblyopia and avoid compounding the motility problem; amblyopia therapy to prevent vision loss in the less preferred eye; surgery to prevent loss of binocular vision in individuals who abandon the compensatory head posture and allow strabismus to become manifest 6.
Duane syndrome surgery
Surgery cannot cure Duane Retraction Syndrome, but it can correct for the deviation in the primary position, thereby improving a compensatory head position that can occur in some individuals 18. It can also improve the leash phenomenon 9.
Indications for surgery
A patient should be considered for surgical correction if he or she has at least one of the following characteristics 18:
- an abnormal head position greater than or equal to 15 degrees
- a significant deviation in the primary position
- Severe induced ptosis: a reduction of greater than or equal to 50% of the width of the palpebral fissure on adduction 19
Pre-surgical evaluation 9:
- Consider brain and orbital MRI for better visualization of orbital anatomy
- Forced duction testing to confirm tightness of the horizontal rectus muscles
Contraindications to Surgery 19:
- Orthophoria in primary position
- Insignificant face turn
- Young Age
Principles of Surgical Approach 9:
- For types 1 and 3 with head turn: recession of medial rectus muscle or horizontal transposition of vertical rectus muscles
- For types 1 and 3 with Leash Phenomenon and/or severe globe retraction: recession of both medial and lateral rectus muscles with possible Y-splitting of the lateral rectus muscle
- For type 2 with head turn and fixation with uninvolved eye: recession of ipsilateral lateral rectus muscle
- For type 2 with head turn and fixation with involved eye: recession of contralateral lateral rectus muscle
- For type 2 with Leash Phenomenon: recession of lateral rectus muscle with possible Y-splitting
Complications of Surgery
- Undercorrection of primary position esotropia and the compensatory head turn 19
- Overcorrection leading to secondary exotropia 19
- New vertical deviations can occur after vertical rectus transposition procedures 19
- Duane Retraction Syndrome 1. https://disorders.eyes.arizona.edu/handouts/duane-retraction-syndrome-1
- DeRespinis PA, Caputo AR, Wagner RS, Guo S. Duane’s retraction syndrome. Surv Ophthalmol. 1993;38:257–88.
- Pearls and pitfalls in the management of Duane syndrome. Taiwan J Ophthalmol. 2017;7(1):3-11. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5525605/
- Kirkham, T.H. Inheritance of Duane’s syndrome. Brit. J. Ophthal. 1970; 54 : 323-329.
- Andrews CV, Hunter DG, Engle EC. Duane Syndrome. 2007 May 25 [Updated 2015 Mar 19]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2018. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1190 https://www.ncbi.nlm.nih.gov/books/NBK1190/
- Andrews CV, Hunter DG, Engle EC. Duane Syndrome. 2007 May 25 [Updated 2015 Mar 19]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2018. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1190
- Duane Retraction Syndrome. http://eyewiki.org/Duane_Retraction_Syndrome
- Murillo-Correa, Claudia E., Veronica Kon-Jara, Elizabeth C. Engle, and Juan C. Zenteno. Clinical features associated with an I126M α2-chimaerin mutation in a family with autosomal dominant Duane retraction syndrome. J AAPOS. 2009; 13 (3): 245-248.
- Learning About Duane Syndrome. https://www.genome.gov/11508984/
- Huber A, Esslen E, Kloti R, et al. Zum problem des Duane syndromes. Graefes Arch Klin Exp Ophthalmol 1964;167:169-91.
- Duane syndrome type 2. https://disorders.eyes.arizona.edu/disorders/duane-retraction-syndrome-2
- Duane Retraction Syndrome 3. https://disorders.eyes.arizona.edu/disorders/duane-retraction-syndrome-3
- Duane Retraction Syndrome 3. http://webeye.ophth.uiowa.edu/eyeforum/cases/56-duanes-retraction-syndrome.htm
- Hotchkiss, Mary G., Neil R. Miller, Arthur W. Clark, and William R. Green . Bilateral Duane’s Retraction Syndrome A Clinical-Pathologic Case Report. Arch Ophthalmol. 1980; 98: 870-874.
- Duane, Thomas D. Clinical Ophthalmology. Pediatric Ophthalmic Surgery. Vol. 6. Philadelphia, PA: Lippincott Williams & Wilkins; 1994.
- Gobin, M.H. Surgical Management of Duane’s Syndrome. Brit. J. Ophthal. 1974; 58 (301): 301-306.
- Miyake, Noriko et.al. CHN1 Mutations are not a Common Cause of Sporadic Duane’s Retraction Syndrome. Am J Med Genet A. 2010; 152: 215-217.
- Barbe, M E, W E Scott, and P J Kutschke. A simplified approach to the treatment of Duane’s syndrome. Br J Ophthalmol. 2004; 88: 131-138.
- Duane, Thomas D. Clinical Ophthalmology. Strabismus, Refraction, The Lens. Vol. 1. Philadelphia, PA: Lippincott Williams & Wilkins; 1993.