What is farmer’s lung
Farmer’s lung is a type of hypersensitivity pneumonitis, which is a noninfectious allergic lung disease that is caused by inhaling mold spores in the dust from moldy hay, straw, or grain. Farmer’s lung disease disrupts the normal function of your lungs, where oxygen enters and carbon dioxide exits the bloodstream. Farmer’s lung is one of the more serious respiratory hazards to which farmers are exposed. Many farmers are forced to leave the occupation due to the physical limitations caused by farmer’s lung. Unfortunately, the number of farmers affected by farmer’s lung has been increasing in recent years. This is likely the result of a growing awareness among farmers about their health and a subsequent increase in the frequency of doctor visits by farmers.
The chances of acquiring farmer’s lung are greatest in late winter and early spring. This is mainly because farmers feed hay and grain materials, which are likely to contain mold spores. Farmers also tend to feed baled hay inside during the colder months. This increases the likelihood of inhaling mold spores because they are more concentrated in a confined space such as a barn. Mold spore inhalation may be a problem when you are cleaning out grain bins or opening new silos. Mold spores may be released from the top layer of silage.
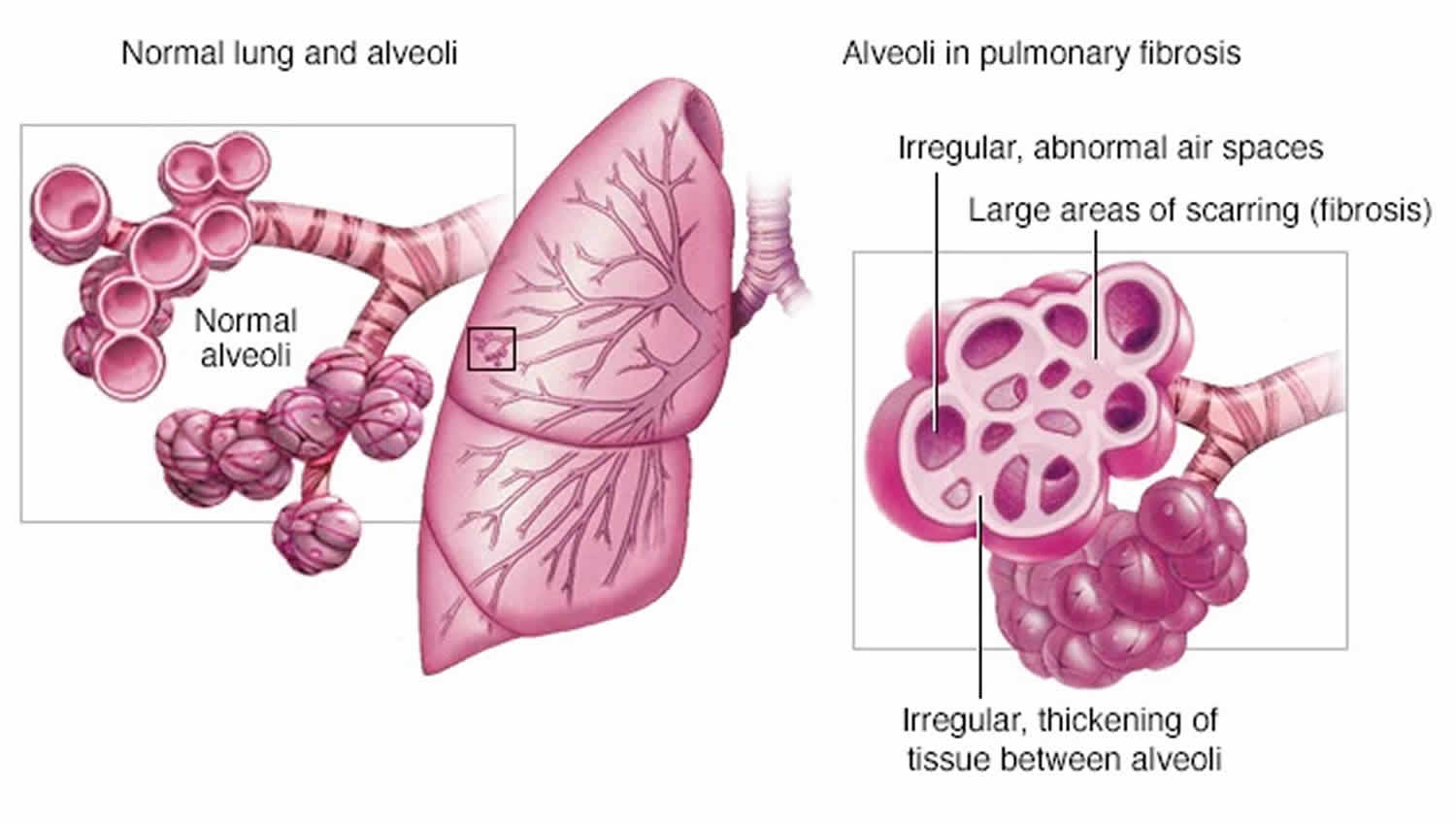
Delaying medical treatment for farmer’s lung often worsens the situation. Permanent damage has often occurred by the time a farmer sees a doctor. In some cases scar tissue (pulmonary fibrosis) has already developed, which further interferes with normal lung function.
Do not self-diagnose. Always check with your doctor if you suspect you have farmer’s lung. Contact your doctor immediately, if you have any of the following symptoms:
- Sudden illness that develops a few hours after you handled moldy crop material.
- Chronic cough.
- General feeling of tiredness or depression.
Your family doctor may not be familiar with farmer’s lung and may mistake your symptoms for a cold, asthma, flu, or even pneumonia. Therefore, you must work with your doctor so he/she can make a correct diagnosis. Make sure to tell your doctor that you are a farmer and whether you have been exposed to moldy crop material. Also, be sure to inform him/her of the types of chemicals and/or dusts to which you are exposed.
Farmer’s lung can be controlled in many ways. For example, your doctor may write a prescription for medication that relieves the symptoms of farmer’s lung. Unfortunately, farmer’s lung cannot be cured.
Figure 1. Normal lung
Figure 2. Farmer’s lung
What are mold spores and why are they so dangerous?
Just as plants produce seeds for reproduction, molds produce tiny spores. These spores are less than 4 microns in size – so small that as many as 250,000 spores can fit on the head of a pin. On the farm, molds tend to grow in stored hay, grain, or silage when moisture content is high (30 percent) and storage areas are poorly ventilated.
Mold spores attach themselves to airborne dust particles when farmers move or work with hay, grain, or silage materials in which mold spores have grown. As a result, farmers inhale both dust particles and mold spores. In fact, a farmer can inhale up to 750,000 of these spores per minute.
Your body has natural defense mechanisms (such as coughing and sneezing) that help prevent dust and other particles from entering your lungs. However, mold spores can often bypass these defenses because of their small size and overwhelming numbers.
Mold spores move into, accumulate, and settle into the lower lungs. Since most gas exchange takes place in the lower lungs, toxins produced by the spores travel through the bloodstream with the oxygen. The body’s reaction to the toxins causes permanent scarring of the lung tissue, which affects the lungs’ ability to transfer oxygen into the bloodstream. Each exposure to mold spores increases the damage. The body’s last defense against these spores is to develop an allergic reaction that causes cold- or pneumonia-like symptoms.
Farmer’s lung disease cause
Farmer’s lung is caused by inhaling mold spores in the dust from moldy hay, straw, or grain. The pathogenesis of farmer’s lung depends on the intensity, frequency, and duration of exposure and on host response to the causative mold spores or antigen. Both humoral and cell-mediated immune responses seem to play a role in pathogenesis. During acute episodes, acute neutrophilic infiltration is followed by lymphocytic infiltration of the airways. Levels of interleukins 1 and 8 and tumor necrosis factor-alpha are increased 1. These cytokines have proinflammatory and chemotactic properties. They cause the recruitment of additional inflammatory mediators, resulting in direct cellular damage and changes in the complement pathway, which provide the necessary stimuli to increase vascular permeability and migration of leukocytes to the lung 2.
Farmer’s lung thermophilic actinomycetes species include the following 3:
- Saccharopolyspora rectivirgula (formerly Micropolyspora faeni)
- Thermoactinomyces vulgaris
- Thermoactinomyces viridis
- Thermoactinomyces sacchari
- Aspergillus species
These organisms flourish in areas of high humidity and prefer temperatures of 104-140 °F (40-60°C) 4. The thermophilic actinomycetes are ubiquitous organisms usually found in contaminated ventilation systems and in decaying compost, hay, and sugar cane (bagasse). Exposure to large quantities of contaminated hay is the most common source of inhalational exposure for farmers who develop farmer’s lung; therefore, grain farmers are not at risk for the development of the disease 4. Farmer’s lung is often a disease of dairy farmers who handle contaminated hay during the winter months. Most cases of farmer’s lung occur in cold, damp climates in late winter and early spring when farmers use stored hay to feed their livestock.
If the acute exposure is large, a dramatic increase in inflammation leads to increased vascular permeability, which can alter the alveolar capillary units, thus promoting hypoxemia and decreased lung compliance. If the exposure is prolonged and continuous, collagen deposition and destruction of the lung parenchyma occur with resultant decreased lung volumes.
Strong evidence suggests the involvement of immune complex–induced tissue injury (type 3 hypersensitivity). The timing of development of symptoms after exposure supports this conclusion. The presence of antigen-specific immunoglobulin and complement activation and deposition in the lung also supports immune-complex or type 3 hypersensitivity in the pathogenesis of farmer’s lung.
Cell-mediated, delayed-type hypersensitivity (type 4 hypersensitivity) also plays a major role in the pathogenesis of this syndrome. The presence of lymphocytes, macrophages, and granulomas in the alveolar spaces and the interstitium supports this conclusion.
Farmer’s lung disease prevention
Farmers can control or even minimize the possibility of getting farmer’s lung by complying to the following preventative measures:
- Identify contaminants in the work environment.
- Minimize the amount and type of contaminants in the work environment.
- Avoid exposure to contaminants and mold spores and dust from decayed grains and forages.
- Limit exposure to all contaminants.
- Operate within a controlled environment whenever possible (e.g., cab, control room, etc.)
- Use mechanical controls to remove air contaminants (e.g., fans, exhaust blowers, filters, etc.)
- Maximize ventilation in dusty areas.
- Move work outside whenever possible.
- Avoid dusty work in confined areas.
- Wear respirators, masks, or other protective equipment.
If you decide to use some form of respiratory protection, make sure to select the appropriate device for the task. For example, most farmers wear dust masks to protect themselves from farmer’s lung. However, these will not work if you are exposed to extremely high levels of mold spores or you already have developed farmer’s lung.
If you have farmer’s lung, talk to your doctor about the type of equipment that will offer the most protection because every exposure increases the risk of serious permanent lung damage. Furthermore, make sure the personal protection equipment fits well and is properly maintained.
When you must work with moldy material
- Wet down feed before transferring it to minimize dust.
- Convert to mechanical or automated feeding or feed-handling systems.
- Wet down the top of the silo before uncapping ensiled material.
- Use some wetting techniques when cleaning out grain bins or other dusty areas.
- Use respiratory protection when handling moldy or dusty materials.
Management to prevent mold spore growth
- Use mold inhibitors.
- Bale hay, ensile crops, and harvest and store grain at recommended moisture contents.
- Dry grain properly before storage.
- Properly ventilate storage buildings.
- Adequately ventilate crops to cool them down.
- Always use a plastic sheet to cap open silos (not plant material) holding down the edges with heavy weights (e.g., tires).
Farmer’s lung disease symptoms
Farmers will develop specific symptoms of farmer’s lung based on the amount of dust and spores to which they have been exposed or the intensity of their body’s reaction to the dust and spores. Farmers are also likely to develop an increased sensitivity to mold exposure over time and will have more severe reactions with lighter exposures. In all cases, each additional exposure will aggravate the problem.
The symptoms of farmer’s lung may be most severe for a 12 to 48 hour period after exposure to mold spores. However, the symptoms may remain for as long as two weeks. Acute farmer’s lung is the short-term form of the disease. Farmers typically develop chronic farmer’s lung due to repeated exposure to mold spores over time, usually because they continue to ignore the symptoms of acute farmer’s lung. However, it is possible to develop chronic farmer’s lung even after one acute attack.
Acute state
Acute state usually begins four to eight hours after exposure to mold spores. Most farmers ignore the symptoms because they are so similar to those of the common cold.
Typical acute state symptoms include:
- Severe shortness of breath with any exertion.
- Headache.
- Irritating cough.
Subacute state
Subacute state is more serious because the symptoms will be more severe and will last longer even with no further exposure to mold spores.
Typical subacute state symptoms include:
- Progressively increasing severe shortness of breath with any exertion.
- Chronic coughing.
- Physical weakness.
- Occasional fever and sweating at night.
- Appetite depression.
- General aches and pains.
Chronic state
Chronic state is the most serious because of its gradual onset and its long-lasting debilitation. In the chronic state, the disease becomes irreversible.
Typical chronic state symptoms:
- Progressively increasing severe shortness of breath with any exertion.
- Chronic coughing.
- Physical weakness.
- Occasional fever and sweating at night.
- Appetite depression.
- General aches and pains.
Farmer’s lung disease complications
Farmer’s lung may cause the following potentially fatal complications if the condition is not diagnosed or well controlled by treatment.
- Irreversible lung damage and permanently reduced lung function because of severe fibrosis and impaired ability to oxygenate the blood during normal breathing.
- Pulmonary hypertension due to damage of blood vessels in the lungs.
- Heart failure because inflammation makes it harder for the heart to pump blood to and through the lungs.
Farmer’s lung disease diagnosis
No single diagnostic or clinical laboratory study is specific to the diagnosis of farmer’s lung. During the physical exam, your doctor will use a stethoscope to listen carefully to your lungs while you breathe.
Physical examination
In acute farmer’s lung, physical findings are as follows:
- Fever
- Tachycardia
- Nonproductive cough
- Rales (abnormal lung sounds characterized by discontinuous clicking or rattling sounds)
- Rales that persist after fever subsides
- Wheezing (rare)
In subacute farmer’s lung, physical findings are as follows:
- Normal examination findings between presentations
- Anorexia
- Weight loss
- Chronic nonproductive cough
- Generalized fatigue
In chronic farmer’s lung, physical findings are as follows:
- Bibasilar rales
- Clubbing – More often observed in patients with chronic farmer’s lung with long-standing hypoxemia and parenchymal damage
- Anorexia
- More severe dyspnea
- Weight loss
- Impaired exercise tolerance
To distinguish farmer’s lung from other lung disorders, you’ll likely have one or more of the following tests to confirm or disprove a diagnosis:
- Take a blood test. Blood tests to detect high levels of white blood cells and other immune cells and factors in your blood that indicate your immune system is activated and causing inflammation somewhere in your body.
- Take a chest X-ray. Chest x-rays to image the lungs and look for inflammation or damage such as fibrosis in your lungs.
- Computed tomography (CT) to image the lungs and look for inflammation or damage such as fibrosis. CT scans, particularly high-resolution ones, can help distinguish between types of hypersensitivity pneumonitis.
- Administer a breathing capacity test.
- Administer an inhalation challenge. Inhalation challenge tests to see if a controlled exposure to a suspected causative substance triggers your immune system and the onset of common signs and symptoms such as an increase in temperature, increase in white blood cell levels, rales that are heard during a physical exam, or reduced lung function. A positive test can confirm an inhaled substance triggers your immune system. A negative test does not rule out that you have hypersensitivity pneumonitis, because it may mean a different untested environmental substance is causing your condition. Before having this test, talk to your doctor about the benefits and possible risks of this procedure.
- Bronchoalveolar lavage (BAL) to collect fluid from your lungs that can be tested for high levels of white blood cells and other immune cells. High levels of these cells mean your body is making an immune response in your lungs, but low levels do not rule out hypersensitivity pneumonitis.
- Lung biopsies to see if your lung tissue shows signs of inflammation, fibrosis, or other changes known to occur in hypersensitivity pneumonitis.
- Perform an immunological investigation. Precipitin tests to see if you have antibodies in your blood that recognize and bind to a causative substance. While a positive test means that you have been exposed to a substance, it cannot confirm you have hypersensitivity pneumonitis. This is because some people without this condition also have antibodies in their blood to these substances. If you have antibodies to a substance, your doctor may have you perform an inhalation challenge test to see if a new exposure to the same substance can activate your immune system and cause a new acute flare.
- Perform a lung function test to see if you show signs of restriction such as reduced breathing capacity or abnormal blood oxygen levels and check if you have obstructed airways. These tests help assess the severity of your lung disease and when repeated they can help monitor whether your condition is stable or worsening over time. Lung function tests may be normal between acute flares.
- Review your clinical history.
Imaging tests
Imaging tests are useful because in most cases, pneumonia affects only a small, localized portion of your lungs, while the effects of farmer’s lung are often spread throughout all five lobes of your lungs.
- Chest X-ray. This painless test causes a small amount of radiation to pass through your chest to produce images of your lungs. X-rays take only a few minutes to perform.
- Computerized tomography (CT). CT scans combine X-ray images taken from many different angles into detailed cross-sectional images. This painless test involves lying on a narrow table that slides into a large, doughnut-shaped machine. CT scans typically take less than 15 minutes to perform. Computerized tomography gives much greater detail of changes in your lungs than what a chest X-ray can provide.
Pulmonary function tests
A test called spirometry measures the amount of air that you’re able to inhale and exhale in a specific period of time. Your doctor may also measure how efficiently your lungs transfer gases from the air into the bloodstream during exercise.
Another way to assess how well your lungs are working is to measure the oxygen in your blood with an oximeter — a device that painlessly clamps on your finger.
Spirometer
A spirometer is a diagnostic device that measures the amount of air you’re able to breathe in and out and the time it takes you to exhale completely after you take a deep breath.
Bronchoscopy
A bronchoscopy is a procedure that uses a flexible tube threaded down your throat to view your airways and collect samples from your lungs.
During bronchoscopy, your doctor may flush a section of your lung with a saltwater solution to collect lung cells and other materials. This flushing procedure is known as a lavage. Your doctor may also insert a tiny tool through the scope to remove a small sample of cells from the lung tissue for testing.
Surgical lung biopsy
In some cases, your doctor may want to examine larger samples of tissue from several locations in your lungs that cannot be reached via bronchoscopy. A surgical procedure to obtain these samples may be necessary. Lung biopsies will reveal inflammation, fibrosis, and possibly granulomas in subacute and chronic farmer’s lung. They are not usually performed for acute farmer’s lung.
Farmer’s lung disease treatment
If you have farmer’s lung, your doctor will recommend eliminating exposure to the allergen irritating your lungs. This step should help lessen your symptoms. In a patient with acute farmer’s lung, pulmonary function improves once antigen exposure is eliminated. Between episodes of acute disease, activity may be unlimited.
In severe cases of farmer’s lung, treatment may also include:
- Corticosteroids. These drugs work by suppressing your immune system, reducing inflammation in your lungs. Corticosteroids are usually taken as a pill. However, long-term corticosteroid use also increases your risk of developing infections and is associated with the thinning of bones (osteoporosis).
- Oxygen therapy. If you’re having a lot of trouble breathing, you may need oxygen therapy through a mask or plastic tubing with prongs that fit into your nostrils. Some people need oxygen therapy constantly, while others might need it only during exercise or sleep.
- Bronchodilators to relax the muscles in the airways and open your airways to make breathing easier.
- Opioids to control shortness of breath or chronic cough that is resistant to other treatments. Regular (e.g. several times a day, for several weeks or more) or longer use of opioids can lead to physical dependence and possibly addiction.
Systemic corticosteroids (combined with avoidance measures) are the primary agents used to treat farmer’s lung.
Nonsteroidal anti-inflammatory drugs (NSAIDs) (eg, cromolyn, nedocromil) or systemic immune modulators are not indicated for treatment at this time.
Lifestyle and home remedies
A diagnosis of farmer’s lung may mean that you’ll have to make changes to your lifestyle to protect your health. You’ll need to avoid known triggers as much as possible.
For example, if your job duties expose you to substances that irritate your lungs, talk to your doctor and supervisor at work about ways to protect yourself, such as wearing a pollen mask or personal dust respirator. If a hobby is causing the problem, you may have to find a different hobby.
Lung transplants
If your condition is not adequately controlled by avoidance strategies or medicines and you develop serious complications, you may be a candidate for a lung transplant. During this procedure, healthy donor lung will be transplanted into you to replace the damaged lung. Two important things to know:
- This procedure is not a cure. This is because your immune system will be the same after the procedure. This means that if you are exposed again to the substances that triggers your immune system, new inflammation may damage the transplanted donor lung tissue.
- This procedure is not for everyone. Even if you are a candidate for this procedure, it may be difficult to find a matching organ donor. Lung transplants are serious medical procedures with their own risks. Talk to your doctor about what procedures are right for you.
Living with farmer’s lung
If you have farmer’s lung, you can take steps to control the condition and prevent complications by receiving routine follow-up care, monitoring your condition, preventing new acute flares and complications, and learning about and preparing for serious complications.
Receive routine follow-up care
In addition to treatments you are using to control your condition, your doctor may recommend other medical care to improve your quality of life, vaccines to prevent lung infections, and lifestyle changes such as physical activity and quitting smoking to improve overall health and avoid some complications.
- Other medical care: Your doctor may evaluate how your condition is affecting your activity level and mental health. To improve your quality of life, your doctor may recommend other treatments to address pain, fatigue, or mental health concerns that you may have.
- Vaccines: Remember that your condition causes you to have reduced lung function, particularly if you have subacute or chronic farmer’s lung. Your doctor may recommend that you receive routine pneumococcal and flu (influenza) vaccines to avoid lung infections that can further impair your reduced lung function.
- Physical activity: Patients with farmer’s lung benefit from regular exercise. Before starting any exercise program, ask your doctor about what level of physical activity is right for you.
- Quitting smoking: If you smoke, quit. Although smoking does not increase the risk of developing farmer’s lung, some studies suggest smoking can worsen disease and shorten survival for people with chronic farmer’s lung compared to nonsmokers with chronic farmer’s lung. Another study reported lung cancer in patients who smoked and had chronic farmer’s lung.
Monitor your condition
If you have been diagnosed with subacute or chronic farmer’s lung, your doctor may recommend follow-up testing to see how well your treatment is working and if your disease is improving, stable, or worse. To monitor your condition, your doctor may recommend repeating tests used earlier to diagnose farmer’s lung such as chest x-rays, computed tomography (CT) scans, or lung function tests.
Your doctor may determine your disease is worse if you have new or more severe fibrosis or lung function problems. High-resolution CT scans may be more informative than lung function tests at assessing disease progression.
There is a growing recognition that disease tends to be worse, such as greater lung fibrosis, if it starts in childhood or early adult life. Therefore, more careful monitoring may be required for younger patients with farmer’s lung.
Prevent new acute flares and serious complications over your lifetime
To help prevent new acute flares and complications, your doctor may recommend tests to identify the substances causing your condition, as well as additional screening tests to prevent potentially fatal complications.
- Identification of substances causing your condition: If you do not know the environmental substances causing your condition, your doctor may recommend diagnostic precipitin and inhalation challenge tests. Identification can help avoid the environmental sources of the substances causing your condition. Successful avoidance strategies can help you live a longer, prevent new acute flares, and slow or stop progression to chronic disease with serious complications.
- Screening for serious complications: If you have been diagnosed with chronic farmer’s lung, your doctor may recommend echocardiography and right-heart catheterization to evaluate pulmonary artery pressure and screen for pulmonary hypertension. Pulmonary hypertension can occur in people who have chronic farmer’s lung, particularly in patients with more severe disease who have poorer lung function and reduced exercise capacity.
- Bellanger AP, Reboux G, Botterel F, et al. New evidence of the involvement of Lichtheimia corymbifera in farmer’s lung disease. Med Mycol. 2010 Nov. 48(7):981-7
- Deschenes D, Provencher S, Cormier Y. Farmer’s lung-induced hypersensitivity pneumonitis complicated by shock. Respir Care. 2012 Mar. 57(3):464-6.
- Barrera C, Valot B, Rognon B, Zaugg C, Monod M, Millon L. Draft genome sequence of the principal etiological agent of farmer’s lung disease, Saccharopolyspora rectivirgula. Genome Announc. 2014 Dec 18. 2, 6.
- Farmer’s Lung. https://emedicine.medscape.com/article/298811-overview