What is a lazy eye
“Lazy eye” also sometimes called amblyopia, is the medical term used when the vision in one eye (common) or both eyes (less common) is reduced because the eye fails to work properly with the brain 1. Amblyopia is when vision in one or both eyes does not develop properly during childhood. The eye itself looks normal, but for various reasons the brain favors the other eye. Amblyopia is a neurodevelopmental disorder that arises from abnormal processing of visual images that leads to a functional reduction of visual acuity and its associated risk factors 2. This normal visual development disruption must occur during the critical period of visual development (the first 8-10 years of life). This is why a complete eye exam is recommended for all children between ages 3 and 5. The depth of damage depends on the severity of the blurred vision, the length of time of the abnormal vision, and the age of onset of the insult. An estimated 2%–3% of the population suffer from amblyopia 3. Amblyopia is a common problem in babies and young children. Approximately 3-5% of children are affected by amblyopia. Amblyopia generally develops from birth up to age 7 years. Unless it is successfully treated in early childhood amblyopia usually persists into adulthood, and is the most common cause of permanent one-eye vision impairment among children and young and middle-aged adults.
Lazy eye can result from any condition that prevents the eye from focusing clearly. Sometimes this causes the weaker (“lazy”) eye to wander outward, inward, upward or downward. When an eye wanders causing misalignment of the two eyes, that condition is called strabismus. With strabismus, the eyes can cross in (esotropia) or turn out (exotropia). Amblyopia and strabismus are commonly confused. When most people think of “lazy eye” they are actually thinking of wandering or misaligned eyes, which is strabismus. “Lazy eye” is amblyopia — poor vision in one or both eyes. This poor vision (amblyopia) can lead to eye misalignment (strabismus). Strabismus is more commonly referred to as crossed eyes, wandering eyes, or drifting eyes. If for some reason one eye of a child has decreased vision, the brain will not use that eye and it becomes lazy (reduced vision) from lack of use. That is amblyopia — the eye is lazy from lack of use. If one eye happens to be looking somewhere other than the other eye, that is strabismus. Lazy eyes with amblyopia just do not see well, it DOES NOT mean they wander or drift 4.
Occasionally, amblyopia is caused by a clouding of the front part of the eye, a condition called cataract.
Early vision screening by a pediatrician, family doctor or an ophthalmologist is important in detecting children with amblyopia as young as possible. A number of eye diseases can contribute to the development of amblyopia.
In 2016, the American Academy of Pediatrics, American Association for Pediatric Ophthalmology and Strabismus, American Academy of Certified Orthoptists, and American Academy of Ophthalmology released a joint clinical report recommending preschool vision screening 5. The joint report recommends vision assessment in children aged 6 months to 3 years with physical examination (eg, external inspection, the fixation and follow test, the red reflex test, and pupil examination). Instrument-based vision screening (with autorefractors or photoscreeners) may be used, when available, in children aged 1 to 3 years. Visual acuity screening may be attempted at age 3 years using HOTV or Lea Symbols charts; children aged 4 to 5 years should have visual acuity assessed using HOTV or Lea Symbols charts, the cover-uncover test, and the red reflex test 6, 5.
The American Academy of Family Physicians recommends vision screening in all children at least once between the ages of 3 and 5 years to detect amblyopia or its risk factors; it concluded that the current evidence is insufficient to assess the balance of benefits and harms of vision screening in children younger than 3 years 7.
The American Optometric Association recommends initial vision screening in infants at birth. Regular comprehensive eye examinations should occur at age 6 months, age 3 years, and prior to entry into first grade; eye examinations should then occur at 2-year intervals unless children are considered at high risk for vision abnormalities 8.
The US Preventive Services Task Force 9 makes recommendations about the effectiveness of specific preventive care services for patients without obvious related signs or symptoms. It bases its recommendations on the evidence of both the benefits and harms of the service and an assessment of the balance. The US Preventive Services Task Force recommended vision screening for amblyopia and its risk factors in children aged 3 to 5 years (B recommendation). The USPSTF concluded that the evidence was insufficient to assess the balance of benefits and harms of vision screening in children younger than 3 years (I statement) 10.
Amblyopia treatment should be started as early as possible because 4:
- over time the amblyopic “lazy” eye could become permanently blind;
- depth perception (3-D vision) could be lost; and
- if the other, better-seeing, eye becomes diseased or injured, the amblyopic “lazy” eye cannot replace the loss in vision.
It’s important to start treatment for lazy eye as soon as possible in childhood, when the complicated connections between the eye and the brain are forming. The best results occur when treatment starts before age 7, although half of children between the ages of 7 and 17 respond to treatment.
Amblyopia is usually corrected by making the child use their weaker eye. This is often done by putting a patch over the child’s stronger eye. In some cases, eye drops can be used to blur vision in the stronger eye. Or the child may wear eyeglasses with a lens that blurs vision in that eye. It generally takes several weeks to several months to strengthen vision in the weaker eye. Once the child has better vision in that eye, they may need to wear an eye patch part-time for a few years. This is because there is a chance that eye can weaken again. Remember to keep all appointments with the child’s ophthalmologist who will carefully monitor your child’s vision. Careful and prolonged follow-up is needed for all children who have been successfully completed previous treatment for amblyopia 11.
Table 1. Risk Factors for Amblyopia
| Risk Factor c | Age, month | ||
|---|---|---|---|
| 12-30 | 31-48 | >48 | |
| Astigmatism, diopters | >2.0 | >2.0 | >1.5 |
| Hyperopia, diopters | >4.5 | >4.0 | >3.5 |
| Anisometropia, diopters | >2.5 | >2.0 | >1.5 |
| Myopia, diopters | >-3.5 | >-3.0 | >-1.5 |
| Manifest strabismus in primary position, prism diopters | >8 | >8 | >8 |
| Media opacity, mm | >1 | >1 | >1 |
a Adapted from Donahue et al.12
b Amblyopia is a neurodevelopmental disorder that arises from abnormal processing of visual images that leads to a functional reduction of visual acuity. It results from conditions that interfere with normal binocular vision. Specific conditions associated with amblyopia are anisometropia (a difference in refractive power between the eyes, in which one foveal image is more blurred than the other), strabismus (ocular misalignment, in which each eye does not have the same image on the fovea), and deprivation (caused by the blockage of the visual pathway, often attributable to cataracts, ptosis, or refractive error due tomyopia, hyperopia, and/or astigmatism) 13, 14, 15, 16, 17. Strabismic and anisometropic amblyopia can coexist. Strabismus can also inhibit development of normal binocular vision in the absence of amblyopia 18.
c Ptosis has been removed from the list because nearly all amblyopia-related ptosis occurs in the setting of superimposed anisometropia.12
Is my child at risk for amblyopia?
Some children are born with amblyopia and others develop it later in childhood. The chances of having amblyopia are higher in kids who:
- Were born early (premature birth)
- Were smaller than average at birth
- Have a family history of amblyopia, childhood cataracts, or other eye conditions
- Have developmental disabilities
Table 2. Major Types of Lazy Eye (Amblyopia) and Identifying Characteristics
| Type of amblyopia | Characteristics |
|---|---|
| Common | |
| Strabismic | Eye misalignment leads to visual cortex suppression |
| Anisometropic (refractive) | Difference in refraction (from prescription lenses) between eyes leads to the vision in the eye with a higher prescription being chronically blurred |
| Combined strabismic and refractive | Eye misalignment with refractive error leads to visual cortex suppression and chronic image blur |
| Less common | |
| Ametropic | Bilateral high, symmetric refractive error leads to chronic image blur in both eyes, and subsequent subnormal visual cortex development |
| Deprivation (rare) | Obstruction of visual axis leads to visual cortex suppression |
Refractive amblyopia
Refractive amblyopia happens when there is a large or unequal amount of refractive error (glasses strength) between a child’s eyes. The brain learns how to see well from the eye that has less need for glasses and does NOT learn to see well from the eye that has a greater need for glasses. The vision problem may be invisible because the child does not complain of blurry vision. The child sees well with the better seeing eye. Additionally, the amblyopic eye may not look any different from the normal seeing eye. Therefore, parents and pediatricians may not think there is a problem because the child’s eyes look normal. For these reasons, this kind of amblyopia in children may not be found until the child has a vision test. This kind of amblyopia can affect one or both eyes and can be best helped if the problem is found early.
Strabismic amblyopia
Strabismic amblyopia develops when the eyes are not straight. One eye may turn in, out, up or down. When this happens, the brain begins to ignore, or “turns off” the eye that is not straight and the vision subsequently drops in that eye.
Deprivation amblyopia
Deprivation amblyopia develops when cataracts or similar conditions “deprive” young children’s eyes of visual experience. If not treated very early, these children never learn to see very well and can have very poor vision. Sometimes this kind of amblyopia can affect both eyes.
What causes lazy eye
Normal vision develops during the first few years of life. At birth infants have very poor vision, however as they use their eyes the vision improves because the vision centers in the brain are developing. If infants are not able to use their eyes from various reasons the vision centers do not develop properly and the vision is decreased despite normal appearance of the structures of the eyes.
Amblyopia can result from any condition that prevents the eye from focusing clearly. Amblyopia can be caused by the misalignment of the two eyes—a condition called strabismus. With strabismus, the eyes can cross in (esotropia) or turn out (exotropia). Occasionally, amblyopia is caused by a clouding of the front part of the eye, a condition called cataract. Cataract is often the most severe type of amblyopia.
The most common cause is refractive error in one or both eyes that is not corrected early in childhood resulting in poor development of the visual function in the affected eye/s. This is called refractive amblyopia 1. Amblyopia can occur when one eye is more nearsighted, more farsighted, or has more astigmatism. These terms refer to the ability of the eye to focus light on the retina. Farsightedness, or hyperopia, occurs when the distance from the front to the back of the eye is too short. Eyes that are farsighted tend to focus better at a distance but have more difficulty focusing on near objects. Nearsightedness, or myopia, occurs when the eye is too long from front to back. Eyes with nearsightedness tend to focus better on near objects. Eyes with astigmatism have difficulty focusing on far and near objects because of their irregular shape.
Another common cause is strabismus or eye misalignment. This is called strabismic. Rarely there is a structural anomaly that impairs the visual function like a droopy eyelid or opacity in the visual axis like cataract or corneal scar. This is called deprivation amblyopia. Multiple causative factors can coexist.
Risk factors associated with an increased risk of lazy eye include:
- Premature birth
- Small size at birth
- Family history of lazy eye, childhood cataracts, or other eye conditions
- Developmental disabilities
A positive family history of strabismus, amblyopia, or media opacities would increase the risk of amblyopia in the child 20. Children who have conditions that increase the risk of strabismus, anisometropia, or media opacities (ex. Down syndrome) would also be at increased risk for the development of amblyopia. The risk of developing amblyopia, from a condition that is known to cause amblyopia, diminshes as the child approaches 8-10 years of age. In addition, the depth of amblyopia is typically less severe the older the child is at the time of onset of the amblyogenic factor.
Strabismus
This is when the eyes point in two different directions. One eye may be focused straight ahead while the other turns in, out, up, or down. To avoid seeing double, the child’s brain may ignore the image from the eye that is not focused straight ahead. But this can keep that eye from developing properly.
Refractive errors
Having a refractive error means being nearsighted, farsighted, or having astigmatism (distorted or blurry vision). A child may have a refractive error that is worse in one eye. That eye can “turn off,” and vision will not develop properly. This can be difficult to tell since the child’s vision seems fine when using both eyes.
Cloudiness in the normally clear parts of the eye
Some children are born with a cataract, where the eye’s normally clear lens is cloudy. This can keep vision from developing properly in that eye.
Lazy eye symptoms
Sometimes lazy eye is not evident without an eye exam. Patients with unilateral amblyopia are often asymptomatic. Occasionally, patients will complain that one eye is blurry, or younger children may report discomfort in the affected eye. Torticollis occurs infrequently. Poor depth perception or clumsiness may be noted. This is why the American Association for Pediatric Ophthalmology and Strabismus, the American Academy of Pediatrics, and the American Academy of Ophthalmology all support pre-kindergarten vision screening for children.
Signs and symptoms of lazy eye may include:
- An eye that wanders inward or outward
- Eyes that appear to not work together
- Poor depth perception
- Squinting or shutting an eye
- Head tilting
- Abnormal results of vision screening tests
See your child’s doctor if you notice his or her eye wandering after the first few weeks of life. A vision check is especially important if there’s a family history of crossed eyes (strabismus), childhood cataracts or other eye conditions.
Lazy eye complications
The main complication of amblyopia is an irreversible, lifelong decrease in vision. These visual functional abnormalities include reductions in visual acuity, contrast sensitivity, vernier acuity, spatial distortion, abnormal spatial interactions, and impaired contour detection 21. Patients with amblyopia will have binocular abnormalities such as impaired stereoscopic acuity and abnormal binocular summation. The monocular vision deficits are usually specific to only the amblyopic eye. However, subclinical deficits of the non-amblyopic eye have also been demonstrated.
People with amblyopia have difficulty seeing three-dimensional images hidden in stereoscopic displays such as autostereograms. Perception of depth, however, from monocular cues such as size, perspective, and motion parallax in the non-amblyopic eye typically remains normal.
Learning may also be impaired in children with amblyopia. Children with amblyopia read and answer multiple-choice questions slower than children that do not have amblyopia 22. Another possible complication of amblyopia includes worsening strabismus due to impaired binocular fusion.
Lastly, overly aggressive amblyopia therapy (especially in younger patients) can produce reverse amblyopia of the sound eye. A new strabismus or a decompensation of an exisiting strabismus can also occur. Patches can be irritating to the skin, and the skin underlying the patch can become hypopigmented relative to the rest of the facial skin. There is also a potential social stigma associated with wearing the patch to school in some cases. Atropine use can cause side effects related to the use of this medication: flushing, rapid heart rate, mood changes (uncommon) and photophobia (common) would be examples of side effects occurring with the use of this medication. Reverse amblyopia can also occur with atropine use as can decompensation of existing strabismus or development of a new strabismus. Cases of reverse amblyopia are infrequent and usually mild. Most cases resolve with discontinuation of treatment.
How is lazy eye (amblyopia) diagnosed ?
Your child might not be aware of having better vision in one eye than the other. And you may not realize it either unless your child has strabismus or other eye problem you can see 23.
The American Academy of Pediatrics and the American Association for Pediatric Ophthalmology and Strabismus recommend vision screening in children three years and older with an eye chart–based test in the physician’s office 24, 25, 26. Because treatment is more likely to succeed if initiated at a younger age 27, it is crucial to make the diagnosis of amblyopia as early as possible. A meta-analysis of four randomized clinical trials evaluating the effect of age on response to amblyopia treatment concluded that children seven years and older were less responsive to treatment than children three to six years of age 28. There was also a trend of greater responsiveness in children three to younger than five years, compared with children five to younger than seven years with severe amblyopia. Although the U.S. Preventive Services Task Force recommends vision screening for all children at least once between three and five years of age, it found insufficient evidence that vision screening for children younger than three years leads to improved visual outcomes 29.
Table 3. Techniques for Pediatric Vision Screening
| Age | Tests | Referral Criteria Comments |
| Newborn to 12 months |
|
|
| 12 to 36 months |
|
|
| 36 months to 5 years |
| Visual acuity thresholds
|
| 5 years and older*
*Repeat screening every 1-2 years after age 5.
|
|
|
Clinical Examination
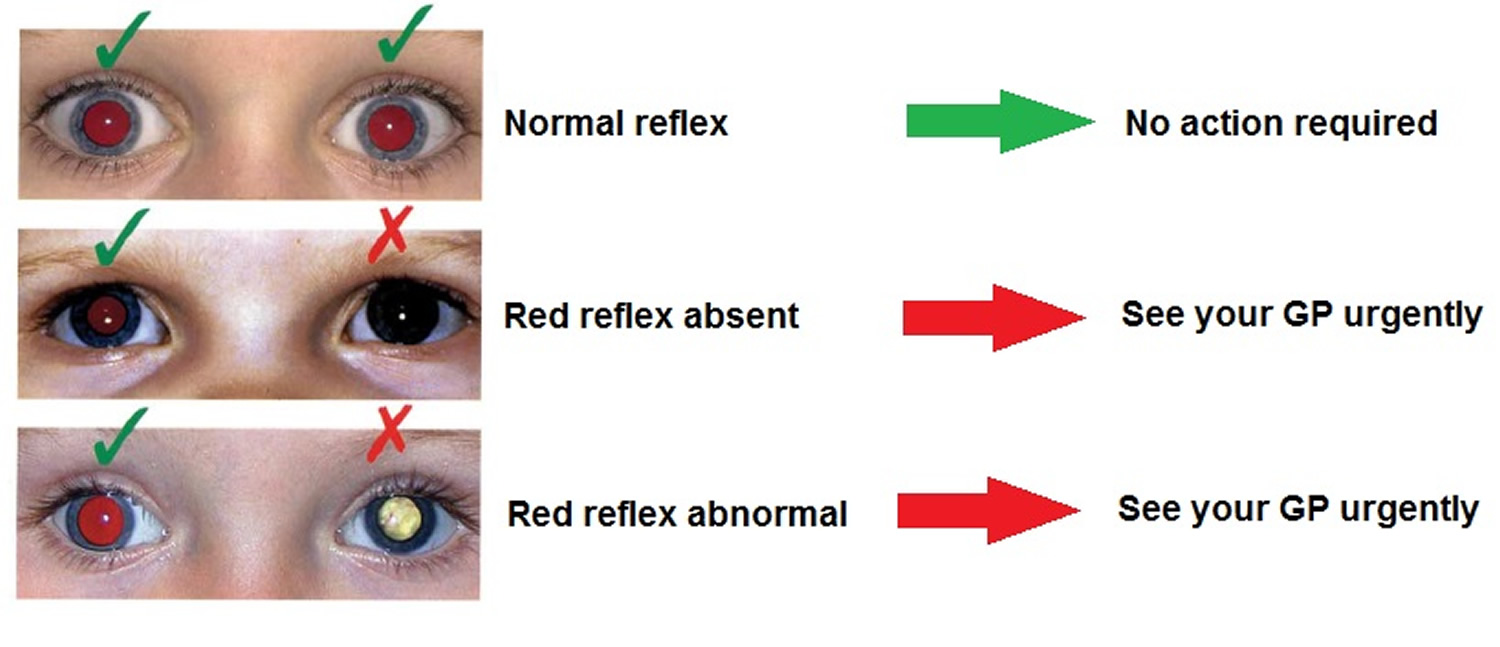
In infants and children, red reflex testing (in which a direct ophthalmoscope is used to compare the reflex in both eyes for asymmetry) is valuable in detecting risk factors for amblyopia, such as a cataract, refractive error, and retinal pathology (Figure 1). Fixation preference of one eye can signify amblyopia. In infants and children up to two-and-a-half years of age, using a toy or other near fixation target to hold the child’s attention, one eye is occluded with an occluder or adhesive patch, and fixation behavior is observed. When the other eye is then occluded, a similar fixation behavior is expected. If a child consistently appears uncooperative when patching one eye, amblyopia is suspected. In children with straight eyes, fixation preference can be determined by using a prism over one eye to induce separate visual images (induced tropia test). In a child with strabismus, fixation preference is often easily determined in the nondeviating eye (Figure 2).
Photoscreening
Photoscreening provides another approach to vision screening. The equipment is designed for use with minimal personnel training and has been associated with successful amblyopia treatment in children identified with risk factors 30. A child’s red reflex of both eyes taken simultaneously with digital or flash photography is evaluated for signs of uncorrected refractive error. The sensitivity in detecting amblyopia among photoscreeners is between 63 and 98 percent 31, 32. However, photoscreeners have high false-positive rates, leading to higher rates of referral of children with normal vision. Although photoscreening should not replace traditional vision chart testing, it may be a useful adjunct in children who cannot cooperate for vision chart testing.
Figure 1. Red Reflex
Figure 2. Child with right esotropia (in-turning of right eye) resulting in right eye amblyopia

Note: Child with right esotropia demonstrated with asymmetric corneal light reflex. The patient has a left eye fixation preference and amblyopia of the right eye.
Figure 3. Child with vertical deviation strabismus

Note: This child has a dissociated vertical deviation strabismus in which one eye will periodically drift upward, while the other eye stays put. Surgery can be curative.
VISION TESTING
In children three years and older, vision testing is performed monocularly with standard eye charts. The charts are labeled with the proper testing distance of 10 or 20 feet (approximately 3 or 6 m). The most advanced test that a child can perform is recommended, because picture testing may mildly overestimate vision compared with letter testing. The American Association for Pediatric Ophthalmology and Strabismus vision screening guidelines are provided in Table 3 25. Any child three-and-a-half to five years of age with best-corrected vision less than 20/40 in either eye, or five years and older with best-corrected vision less than 20/32 in either eye, or with a two-line difference between eyes, should be referred to a pediatric ophthalmologist 25. Children should be tested with lines of letters, and not a single letter, because the latter can overestimate vision. An adhesive patch to cover the eye is preferred for testing over a handheld occluder, because children may peek around the occluder unnoticed, and amblyopia can be missed. Patients with nystagmus (rapid involuntary movements of the eyes) should have their vision tested with both eyes first, which gives their true functioning visual acuity. When a patch or occluder is placed over one eye, increased nystagmus may occur, further decreasing the patient’s vision. This results in falsely lowered monocular visual acuity.
Ophthalmologists diagnose amblyopia by checking to see if vision differs between the two eyes. To check a baby’s or young child’s vision, the ophthalmologist may cover one of the child’s eyes and watch how well they can follow a moving object. The doctor may also watch how the child reacts when one eye is covered. If one eye has amblyopia and the other is covered, the child may try to look above or below the patch, pull it off or cry 23.
The ophthalmologist will do a complete medical eye exam, looking for other eye problems that could be affecting vision 23.
Poor vision in one eye does not always mean a child has amblyopia 23. In some cases, wearing glasses to correct a refractive error in one eye can improve vision.
When should a child’s vision be tested ?
All children should have their vision checked by their pediatrician, family physician or ophthalmologist at or before their 4th birthday 23. If there is a family history of misaligned eyes, childhood cataracts or serious eye disease, an ophthalmologist should check their eyes when they are an infant.
Most doctors test vision as part of a child’s medical exam. If they see any sign of eye problems, they may send a child to an ophthalmologist for further tests.
Clinical History
Children with a family history of strabismus or amblyopia have an increased risk of amblyopia. If a child has amblyopia, siblings should be observed for risk factors and undergo vision screening. If the child with amblyopia required glasses before two-and-a-half years of age, and did not have strabismus as a detectable risk factor, it is reasonable to refer a younger sibling for a comprehensive dilated eye examination.
Physicians should ask parents about torticollis (abnormal head posture), nystagmus, squinting of one eye, or strabismus. Torticollis, nystagmus, and squinting of one eye can all indicate strabismus. Torticollis with visual tasks may be a sign of strabismus, because the child may adopt a head position to better align his or her eyes. Torticollis is commonly associated with vertical strabismus, such as in congenital superior oblique palsy.
Children with nystagmus may adopt a head turn to find a visual area in which their nystagmus decreases (null zone), thus improving their vision. They may also demonstrate eye crossing while fixing on a near target as a result of converging their eyes to dampen the nystagmus. Any patient with strabismus is at risk of amblyopia, so a child with torticollis requires a comprehensive eye examination to rule out eye misalignment. Squinting of one eye, especially in bright light conditions, can be a sign of intermittent exotropia, or eye wandering.
The diagnosis of amblyopia is made when a child has decreased vision usually associated with an amblyogenic risk factor and without ocular structural abnormalities. It can also be diagnosed in a child after removal of a visual axis obstruction (i.e., cataract) with persistent reduced vision. The diagnosis of amblyopia is always determined with best-corrected vision.
Lazy eye treatment
Amblyopia is usually corrected by making the child use their weaker eye 33. This can be done by putting a patch over the child’s stronger eye 33. Another way is to make vision blurry in the stronger eye using eye drops 33. Or the child may wear eyeglasses with a lens that blurs vision in the good eye 33.
It can take several weeks to several months for vision to get stronger in the weaker eye. Once the child has better vision in that eye, he or she may need to wear an eye patch part-time for a few years. This helps keep their vision strong.
In some cases, the ophthalmologist will recommend surgery to correct certain eye problems causing amblyopia. After surgery, the child may need to keep wearing a patch or otherwise cover the strong eye until his or her vision improves.
It is possible to prevent vision loss from amblyopia. But treatment only works if your child only uses the weaker eye to see 33. Children do not like to have their stronger eye patched or blurred. However, you need to help your child do what is best for them.
- When a child has amblyopia, it is important to make vision stronger in the weak eye 33. Even if eye problems causing amblyopia are corrected with glasses or surgery, the amblyopia itself must be treated. If not, the child may have lifelong vision problems 33.
When should amblyopia be treated ?
Early treatment is always best 34. If necessary, children with refractive errors (nearsightedness, farsightedness or astigmatism) can wear glasses or contact lenses when they are as young as one week old. Children with cataracts or other “amblyogenic” conditions are usually treated promptly in order to minimize the development of amblyopia.
How old is TOO old for amblyopia treatment ?
A recent National Institutes of Health study confirmed that SOME improvement in vision can be attained with amblyopia therapy initiated in younger teenagers (through age 14 years) 34. Better treatment success is achieved when treatment starts early, however.
What happens if amblyopia is not treated ?
If amblyopia is not treated the vision in the affected eye/s will be permanently decreased causing deficits in depth perception and peripheral vision. Moreover if the good eye becomes injured or affected by a disease, significant lifetime disability may result.
The ophthalmologist will give the instructions and monitor the progress but the patient and the family will do the hard work of actually performing the treatment. Children do not like to have their good eye patched, especially if the vision in the amblyopic eye is very low, but parents must stand by them and help them do what’s best. Parents play probably the most important role in a successful treatment.
How can you get early treatment for amblyopia ?
Some forms of amblyopia, such as that associated with large-deviation strabismus, may be easily detected by parents. Other types of amblyopia (from high refractive error) might cause a child to move very close to objects or squint his or her eyes. Still other forms of amblyopia may NOT be obvious to parents and therefore must be detected by Vision Screening.
How is amblyopia treated in children ?
Individual treatment plans depend on the age of the patient, the severity of amblyopia, and compliance with patching or atropine regimen and follow-up. For example, a seven-year-old patient with anisometropia who is initially diagnosed with dense amblyopia would likely benefit from a combination of glasses with patching instead of observation with glasses alone. A similar three-year-old patient may be treated with glasses alone, followed by patching after any improvement in vision stabilizes. Surveillance for occlusion amblyopia (decreased vision in the patched eye due to deprivation) and amblyopia recurrence after successful treatment are critical. Amblyopia recurs in 25 percent of children after patching is discontinued 35. Tapering the amount of time a patch is worn each day at the end of treatment reduces the risk of recurrence.
Treating amblyopia involves forcing the child to use the eye with weaker vision. There are two common ways to treat amblyopia 1:
Patching
An adhesive patch is worn over the stronger eye for weeks to months. This therapy forces the child to use the eye with amblyopia. Patching stimulates vision in the weaker eye and helps parts of the brain involved in vision develop more completely. A less utilized therapy option is the Bangerter filter, in which a graded adhesive is applied to the child’s glasses over the lens of the nonamblyopic eye, producing a blurred image. This is mostly used in older children who prefer a less noticeable option than patching.
An National Eye Institute study 36 showed that patching the unaffected eye of children with moderate amblyopia for two hours daily works as well as patching for six hours daily 1. Shorter patching time can lead to better compliance with treatment and improved quality of life for children with amblyopia. However, a recent study 37 showed that children whose amblyopia persists despite two hours of daily patching may improve if daily patching is extended to 6 hours.
Previously, eye care professionals thought that treating amblyopia would be of little benefit to older children. However, results from a nationwide clinical trial 38 showed that many children from ages seven to 17 years old benefited from treatment for amblyopia. This study shows that age alone should not be used as a factor to decide whether or not to treat a child for amblyopia.
During which activities should patching be performed ?
There is no particular activity that will improve the vision more than another activity. The most important part of treatment is keeping the patch on for the prescribed treatment time. As long as the child is conscious and has his or her eyes open, visual input will be processed by the amblyopic eye. On the other hand, the child may be more cooperative or more open to bargaining if patching is performed during certain, favorite activities (such as watching a preferred television program or video). Some eye doctors believe that the performance of near activities (reading, coloring, hand-held computer games) during treatment may be more stimulating to the brain and produce better or more rapid recovery of vision.
Should patching be performed during school hours ?
In many instances, school is an excellent time to patch, taking advantage of a nonparental authority figure. Patching during school hours gives the class an opportunity to learn valuable lessons about accepting differences between children. While in most instances, children may not need to modify their school activities while patching, sometimes adjustments such as sitting in the front row of the classroom will be necessary. If the patient, teacher, and classmates are educated appropriately, school patching need not be a socially stigmatizing experience. On the other hand, frequently a parental or other family figure may be more vigilant in monitoring patching than is possible in the school setting. Parents should be flexible in choosing when to schedule patching.
What if my child refuses to wear the patch ?
Many children will resist wearing a patch at first. Successful patching may require persistence and plenty of encouragement from family members, neighbors, teachers, etc. Children will often throw a temper-tantrum, but then they eventually learn not to remove the patch. Another way to help is to provide a reward to the child for keeping the patch on for the prescribed time period.
How long does amblyopia patching therapy take to work ?
Although vision improvement frequently occurs within weeks of beginning patching treatment, optimal results often take many months. Once vision has been improved, less (maintenance) patching or periodic use of atropine eyedrops may be required to keep the vision from slipping or deteriorating. This maintenance treatment may be advisable for several months to years.
Atropine
A drop of a drug called atropine is placed in the stronger eye to temporarily blur vision so that the child will use the eye with amblyopia, especially when focusing on near objects. Atropine 1% eye drops block parasympathetic innervation to the ciliary muscle and pupil, causing temporary loss of accommodation (focusing at near) and pupillary dilation. Atropine is more effective in farsighted eyes, because removing the ability to accommodate in such eyes does not allow the child to focus at near. The goal of atropine use is to stimulate preferential near fixation of the amblyopic eye, leading to visual improvement.
National Eye Institute-supported research 39 has shown that atropine eye drops, when placed in the unaffected eye once a day, work as well as eye patching. Atropine eye drops are sometimes easier for parents and children to use.
However, not all children benefit from eye drop treatment for amblyopia. Eye drops (such as atropine) do not work as well when the stronger eye is nearsighted or when the degree of amblyopia is severe 34.
What happens if amblyopia treatment does not work ?
In some cases, treatment for amblyopia may not succeed in substantially improving vision. It is hard to decide to stop treatment, but sometimes it is best for both the child and the family. Children who have amblyopia in one eye and good vision only in their other eye can wear safety glasses and sports goggles to protect the normal eye from injury. As long as the good eye stays healthy, these children function normally in most aspects of society
In most cases loss of vision from amblyopia can be prevented or successfully treated if started early enough and if the degree of amblyopia is not extreme.
Can surgery be performed to treat amblyopia ?
There is no surgery to improve the vision for amblyopia. Surgery can be performed to straighten misaligned eyes such as crossing. Surgery to make the eyes straight can only help enable the eyes to work together as a team. Children with strabismic amblyopia still need close monitoring and treatment for the amblyopia, and this treatment is usually performed before strabismus surgery is considered.
Children who are born with cataracts may need surgery to take out the cataracts. After surgery, the child will usually need vision correction with glasses or contact lenses and patching.
Can amblyopia be treated in adults ?
Studies are very limited at this time, and scientists don’t know the success rate for treating amblyopia in adults. During the first seven to ten years of life, the visual system develops rapidly. Important connections between the eye and the brain are created during this period of growth and development. Scientists are exploring whether treatment for amblyopia in adults can improve vision.
Lazy eye treatment in older children and adults
Although it is true that amblyopia can be treated more effectively in younger children, several studies have shown that older children and adults with amblyopia are also able to respond to amblyopia treatment 11. A randomized Pediatric Eye Disease Investigator Group (PEDIG) trial assessing treatment of amblyopia in children aged 7 to 17 years 40 revealed the following results:
- Amblyopia improved with optical correction alone in about one fourth of patients aged 7 to 17 years,
- For patients aged 7 to 12 years, 2 to 6 hours per day of patching together with near visual activities and atropine improved visual acquity even if the amblyopia had been treated previously,
- Even for patients 13 to 17 years of age, patching for 2 to 6 hours per day together with near visual activities improved visual acquity when amblyopia had not been treated previously.
A recent analysis of the Preferred Practice Pattern for amblyopia by the American Academy of Ophthalmology recommended treatment for children up to 10 years of age 41.
Lazy eye surgery
“Lazy eye surgery” does not exist 4. Lazy eye (amblyopia) cannot be treated with surgery. It can only be treated when the patient is a child. The younger it is detected and treated the better. In fact, after age 6 the success rate of treatment goes way down. Glasses and eye patches are the most common treatments for amblyopia, or lazy eye.
Strabismus, or eye misalignment, CAN be treated with surgery on the eye muscles. This surgery can be performed on both adults and children. Eye muscle surgery can improve not only the cosmetic appearance of the eyes but also visual function.
When most people ask about “lazy eye surgery,” they are really talking about strabismus surgery, or surgery to correct misalignment of the eyes.
If you are considering eye muscle surgery, here are the key facts to know:
- The surgery works by either loosening or tightening the eye muscles. This changes the alignment of the eyes relative to each other.
- Approximately 1.2 million eye alignment surgeries are performed each year, making it the third most common eye surgery in the United States.
- Eye muscle surgery has a high success rate and serious complications are extremely rare.
- It is a one-day procedure that usually does not require staying overnight in the hospital.
- Children can return to school after a few days of rest. Most adults can return to work within a week.
- Pain, soreness, redness, and double vision are the most common side effects of eye muscle surgery. These are usually temporary.
The are two main types of surgery:
- Recession is when an eye muscle is detached and then reattached further away from the front of the eye to weaken the muscle.
- Resection is when a portion of an eye muscle is removed to make the muscle stronger.
Whether you are looking into this “lazy eye surgery” for yourself or your child, a vital first step is to discuss your goals and expectations for the surgery with your ophthalmologist.
Lazy eye exercises
Currently there is no human studies on eye exercises for lazy eye (amblyopia). The only research we could find was on mice. That research 42 has demonstrated that voluntary physical exercise and visual perceptual learning, two totally non invasive procedures, share the remarkable capability to potentiate plasticity in the adult visual cortex, favoring recovering of visual functions in adult amblyopic rodents. Running and locomotion is associated not only with activation of cortical Vasoactive Intestinal Peptide neurons, but also with increases in multiple neuromodulators, including serotonin, which has been shown to be enhanced by environmental enrichment 43 and to promote adult primary visual plasticity 44. The impact of physical exercise on amblyopic adults remains to be elucidated, with preliminary results in this laboratory study showing a strong enhancement of visual cortical plasticity in healthy subjects after a period of voluntary physical activity 45.
New treatments for lazy eye
New technologies have been incorporated into standard therapy for amblyopia as our understanding of the pathophysiological basis of amblyopia has increased.
Intermittent occlusion glasses
With regard to advances in occlusion therapy for amblyopia, an electronic device, Amblyz liquid crystal intermittent occlusion glasses (XPAND 3D Group, Ljubljana, Slovenia), has been introduced 11. Intermittent occlusion glasses are programmed to unilaterally alternate between opaque and transparent phases at 30-second intervals, providing effective occlusion of the fellow eye 50% of the time they are worn. Because these glasses are more child friendly and do not produce the side effects seen with adhesive skin patches, they may potentially improve compliance with occlusion therapy. However, a recent study to monitor objective compliance with intermittent occlusion glasses using a microsensor affixed to the glasses found that general compliance was not as high as was anticipated for this new technology (averaging 51.6%) and varied greatly from patient to patient (range, 10% to 97%), and in addition, daily compliance decreased slightly over time 46. There have been several studies assessing the effectiveness of the intermittent occlusion glasses 47, 48; however, there has been only one randomized clinical trial comparing the effectiveness of liquid crystal occlusion glasses and adhesive occlusion patches 49. After 12 weeks of treatment, 4 hours daily intermittent occlusion therapy with liquid crystal glasses was not inferior to 2 hours daily patching when treating children 3 to 8 years of age with moderate, unilateral amblyopia 49. However, there have been no further studies to confirm the effectiveness of intermittent occlusion therapy glasses, in terms of age, severity and subtype of amblyopia.
Perceptual learning
Perceptual learning refers to any relatively permanent and consistent change in the perception of a sensory task following repeated practice 50. Visual performance may be improved with repetitive practice of specific controlled visual tasks. Persistence of binocular cortical communication in subjects with amblyopia is the basis for the hypothesis that activation of these persistent binocular neural circuits might awaken an amblyopic eye. Since the Cambridge Stimulator treatment described in the 1970s 51, which was the first application of perceptual learning theory to amblyopia, perceptual learning to various visual tasks has resulted in improvement in orientation discrimination, stereoacuity and contrast sensitivity, even in adults with amblyopia 52. Perceptual learning seems to be a promising method; however small numbers of participants in the previously published studies and lack of long-term follow-up currently limit widespread use of perceptual learning as a therapeutic option for amblyopia.
Dichoptic training
It has been suggested that patching may further disrupt binocularity and theoretically may not be an ideal method to restore binocular cortical function in amblyopic patients 53. Dichoptic presentation refers to presenting different images to each eye. Given the amblyopic eye has lower contrast sensitivity compared to the sound eye, when employing dichoptic presentation as a treatment method, children with amblyopia are trained on tasks in which reduced contrast images are presented to the sound eye while higher contrast images are shown to the amblyopic eye in order to balance cortical input and overcome inter-ocular suppression. Binocular visual stimulation using computer games played on a smartphone or computer tablet has been suggested as a means to improve not only visual acuity, but also binocular function 54. Early non-randomized studies of binocular visual stimulation have demonstrated promising results 55, 56, 57. Recently, several clinical trials employing different testing protocols and different age groups with or without prior amblyopia treatment have been completed to investigate the effectiveness of binocular computer tablet treatment for amblyopia 53. A Pediatric Eye Disease Investigator Group (PEDIG) trial has compared visual acuity improvement in children with amblyopia treated with a binocular iPad game for 1 hour a day vs. part-time patching for 2 hours a day in 385 children aged 5 to 12 years with amblyopia 56. At 16 weeks, mean amblyopic-eye visual acuity improved 1.05 lines in the binocular group and 1.35 lines in the patching group, with an adjusted treatment group difference of 0.31 lines (favoring patching). Binocular treatment of amblyopia using videogames has been performed to compare the effectiveness of a binocular video game with a placebo video game for improving visual functions 54. The results indicated that the binocular video game did not improve visual outcomes more than the placebo video game in older children and adults 54. In children aged 13 to 16 years, improvement in amblyopic eye visual acuity with a binocular iPad game was not better than patching 58. There was no benefit with respect to visual acuity or stereoacuity after 4 or 8 weeks of treatment with the dichoptic binocular Dig Rush iPad game in children aged 7 to 12 years who had received no previous treatment for amblyopia other than spectacles 53. Although research has been ongoing, to date, evidence supporting the inclusion of binocular treatment for amblyopic patients remains insufficient.
Transcranial magnetic stimulation
Transcranial magnetic stimulation (TMS) is an established, safe, and noninvasive technique for stimulating the human brain. The technique is based on the principle of electromagnetic induction, whereby a brief magnetic field is generated within a plastic-coated coil of wire that is placed on the head above the cortical area to be stimulated. The magnetic field passes painlessly through the skull and induces a weak electrical current within the underlying region of cortex. As a result, the neural excitability of the stimulated region may be temporarily altered. The first study to assess the effect of repetitive transcranial magnetic stimulation (TMS) on visual function in adult with amblyopia demonstrated a transient improvement in contrast sensitivity 59. Transcranial magnetic stimulation is expected to enhance the effects of traditional amblyopia treatments 60. The effects of repeated applications of transcranial magnetic stimulation as a therapeutic option in amblyopia are currently being investigated.
Pharmacologic therapy
Dopamine concentrations have been found to be decreased in the retina with deprivation amblyopia 61. Increasing retinal dopamine concentrations may have a beneficial effect in amblyopia. In the first study using levodopa, the immediate metabolic precursor of dopamine, as a possible treatment in adult amblyopia, a single administration of levodopa temporarily improved contrast sensitivity and decreased scotoma size in the amblyopic eye 62. A Pediatric Eye Disease Investigator Group (PEDIG) randomized trial of levodopa as a treatment for residual amblyopia in children aged 7 to 12 years showed that treatment with oral levodopa while continuing to patch for 2 hours daily did not produce a clinically or statistically meaningful improvement in visual acuity compared to placebo and patching 63. Cytidine diphosphatecholine is a complex organic molecule that acts as an intermediate in the biosynthesis of cell membrane phospholipids and has been hypothesized to protect the anatomic and structural integrity of cell membranes, thereby preventing nerve cell damage 64. A study with adult amblyopic patients demonstrated improvement in VA with citicoline augmentation of patching that was not sustained following cessation of the medication 65. Early studies in amblyopic children were promising, showing treatment effects with citicoline both alone and in addition to patching 66. Potential long-term effects of using levodopa and other medications with psychoactive and extrapyramidal effects in an immature nervous system of children are of concern 67. Restoring cortical plasticity and reducing interocular suppression have received attention as novel therapeutic strategies for amblyopia 68.
Lazy eye prognosis
The keys to amblyopia prognosis are younger age at detection/treatment, short course until intervention, compliance with treatment and the severity of amblyopia 21. The effectiveness of intensive screening protocols to detect amblyopia at a young age has been shown to result in a better visual acuity of the amblyopic eye at age 7.5 years. Most patients do improve with treatment, but often residual amblyopia remains. At least 75% of children treated with occlusion therapy do show a good return of vision. However, in at least 50% of children, there is a slight decrease in visual acuity over time. The best outcomes are in children who are referred early in life. However, in many cases, the actual real-life images may be slightly altered in many children as they grow 69. However, if treated, more than 70% of patients have significant vision improvement within 12 months. Even after treatment, there may be some decline in vision over the coming years. Risk factors for failure to restore vision include age at which treatment for the condition started (later treatment tends to have a worse outcome), deprivation amblyopia, and poor initial visual acuity.
With cessation of amblyopia treatment there is a risk of recurrence. In one study, the risk of recurrence was higher with better visual acuity at the time of cessation of treatment, a greater number of lines improved during the previous treatment, and a prior history of recurrence. Orthotropia or excellent stereoacuity at the time of patching cessation did not appear to have a protective effect on the risk of recurrence. In a prospective study of cessation of treatment in children aged 3 to <8 years with successfully treated amblyopia due to anisometropia, strabismus or both, the risk of amblyopia recurrence was found to be 24%. Patients treated with 6 to 8 hours of daily patching had a 4-fold greater odds of recurrence if patching was stopped abruptly rather than when it was reduced to 2 hours per day prior to cessation. Careful and prolonged follow-up during the amblyogenic years, is needed for all children who have been previously treated for amblyopia to prevent a recurrence. In general, the younger amblyopes are treated, the better the likelihood of improvement.
Most textbooks do not recommend trying amblyopia therapy in the second decade of life but some improvement can be obtained in select cases. A study of amblyopia therapy in children aged 7-17 years found that amblyopia improves to some degree with optical correction alone in about one fourth of patients. However most required additional treatment for amblyopia 70. For patients aged 7 to 12 years, 2 to 6 hours per day of patching with near visual activities and atropine improved visual acuity even if the amblyopia had been previously treated. For patients 13 to 17 years, improvement was only noted in those children who had not been previously treated. The degree of improvement in these older children was much more modest than results from other studies of younger children, so the importance of early detection and treatment remains.
Studies have demonstrated that amblyopic children read significantly more slowly than controls, even when the vision in the amblyopic eye is only reduced to 20/30 vision 71. Amblyopia can also impact academic related fine-motor outcomes, such as multiple-choice answer completion time 22.
References- The National Eye Institute, National Institutes of Health. Facts About Amblyopia. https://nei.nih.gov/health/amblyopia/amblyopia_guide
- Doshi NR, Rodriguez ML. Amblyopia. Am Fam Physician. 2007;75(3):361-367.
- Centers for Disease Control and Prevention. Common Eye Disorders. https://www.cdc.gov/visionhealth/basics/ced/index.html
- American Academy of Ophthalmology. Lazy Eye Surgery Facts. https://www.aao.org/eye-health/tips-prevention/lazy-eye-surgery-facts
- Donahue SP, Baker CN; Committee on Practice and Ambulatory Medicine, American Academy of Pediatrics; Section on Ophthalmology, American Academy of Pediatrics; American Association of Certified Orthoptists; American Association for Pediatric Ophthalmology and Strabismus; American Academy of Ophthalmology. Procedures for the evaluation of the visual system by pediatricians. Pediatrics. 2016;137(1).
- Jonas DE, Amick HR, Wallace IF, et al. Vision Screening in Children Ages 6 Months to 5 Years: A Systematic Review for the US Preventive Services Task Force. Evidence Synthesis No. 153. AHRQ Publication No. 17-05228-EF-1. Rockville, MD: Agency for Healthcare Research and Quality; 2017.
- American Academy of Family Physicians. Clinical preventive service recommendation: visual difficulties and impairment. http://www.aafp.org/patient-care/clinical-recommendations/all/visual.html
- American Optometric Association. Optometric clinical practice guideline: pediatric eye and vision examination. https://www.aoa.org/documents/optometrists/CPG-2.pdf
- US Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/Page/Document/evidence-summary/vision-in-children-ages-6-months-to-5-years-screening
- Final Recommendation Statement. Vision in Children Ages 6 Months to 5 Years: Screening. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/vision-in-children-ages-6-months-to-5-years-screening
- Park S. H. (2019). Current Management of Childhood Amblyopia. Korean journal of ophthalmology : KJO, 33(6), 557–568. https://doi.org/10.3341/kjo.2019.0061
- Donahue SP, Arthur B, Neely DE, Arnold RW, Silbert D, Ruben JB; POS Vision Screening Committee. Guidelines for automated preschool vision screening: a 10-year, evidence-based update. J AAPOS. 2013;17(1):4-8.
- Pascual M, Huang J, Maguire MG, et al; Vision In Preschoolers (VIP) Study Group. Risk factors for amblyopia in the vision in preschoolers study. Ophthalmology. 2014;121(3):622-629.
- Ying GS, Huang J, Maguire MG, et al; Vision in Preschoolers Study Group. Associations of anisometropia with unilateral amblyopia, interocular acuity difference, and stereoacuity in preschoolers. Ophthalmology. 2013;120(3):495-503.
- Arnold RW. Amblyopia risk factor prevalence. J Pediatr Ophthalmol Strabismus. 2013;50(4):213-217.
- Pai AS, Rose KA, Leone JF, et al. Amblyopia prevalence and risk factors in Australian preschool children. Ophthalmology. 2012;119(1):138-144.
- Pai AS, Wang JJ, Samarawickrama C, et al. Prevalence and risk factors for visual impairment in preschool children: the Sydney Paediatric Eye Disease Study. Ophthalmology. 2011;118(8):1495-1500.
- Ciner EB, Schmidt PP, Orel-Bixler D, et al. Vision screening of preschool children: evaluating the past, looking toward the future. Optom Vis Sci. 1998;75(8):571-584.
- Identification and Treatment of Amblyopia. Am Fam Physician. 2013 Mar 1;87(5):348-352. http://www.aafp.org/afp/2013/0301/p348.html
- Amblyopia. https://eyewiki.org/Amblyopia
- Blair K, Cibis G, Gulani AC. Amblyopia. [Updated 2022 Jan 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430890
- Kelly, K. R., Jost, R. M., De La Cruz, A., & Birch, E. E. (2018). Multiple-Choice Answer Form Completion Time in Children With Amblyopia and Strabismus. JAMA ophthalmology, 136(8), 938–941. https://doi.org/10.1001/jamaophthalmol.2018.2295
- American Academy of Ophthalmology. Amblyopia: Lazy Eye Diagnosis. https://www.aao.org/eye-health/diseases/amblyopia-lazy-eye-diagnosis
- Committee on Practice and Ambulatory Medicine, Section on Ophthalmology, American Association of Certified Orthoptists; American Association for Pediatric Ophthalmology and Strabismus; American Academy of Ophthalmology. Eye examination in infants, children, and young adults by pediatricians. Pediatrics. 2003;111(4 pt 1):902–907.
- American Association for Pediatric Ophthalmology and Strabismus. Vision Screening Recommendations – Techniques for Pediatric Vision Screening. https://aapos.org/terms/conditions/131
- American Academy of Pediatrics Section on Ophthalmology and Committee on Practice and Ambulatory Medicine, American Academy of Ophthalmology, American Association for Pediatric Ophthalmology and Strabismus. American Association of Certified Orthoptists. Instrument-based pediatric vision screening policy statement. Pediatrics. 2012;130(5):983–986.
- Kirk VG, Clausen MM, Armitage MD, Arnold RW. Preverbal photoscreening for amblyogenic factors and outcomes in amblyopia treatment: early objective screening and visual acuities. Arch Ophthalmol. 2008;126(4):489–492.
- Holmes JM, Lazar EL, Melia BM, et al.; Pediatric Eye Disease Investigator Group. Effect of age on response to amblyopia treatment in children. Arch Ophthalmol. 2011;129(11):1451–1457.
- U.S. Preventive Services Task Force. Screening for visual impairment in children ages 1 to 5 years. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/visual-impairment-in-children-ages-1-5-screening
- Teed RG, Bui CM, Morrison DG, Estes RL, Donahue SP. Amblyopia therapy in children identified by photoscreening. Ophthalmology. 2010;117(1):159–162.
- Matta NS, Arnold RW, Singman EL, Silbert DI. Comparison between the plusoptiX and MTI photoscreeners. Arch Ophthalmol. 2009;127(12):1591–1595.
- Donahue SP, Baker JD, Scott WE, et al. Lions Clubs International Foundation Core Four Photoscreening: results from 17 programs and 400,000 preschool children. J AAPOS. 2006;10(1):44–48.
- American Academy of Ophthalmology. Amblyopia: Lazy Eye Treatment. https://www.aao.org/eye-health/diseases/amblyopia-lazy-eye-treatment
- American Association for Pediatric Ophthalmology and Strabismus. Amblyopia. https://aapos.org/terms/conditions/21
- Holmes JM, Melia M, Bradfield YS, Cruz OA, Forbes B; Pediatric Eye Disease Investigator Group. Factors associated with recurrence of amblyopia on cessation of patching. Ophthalmology. 2007;114(8):1427–1432.
- Repka MX, Beck RW, Holmes JM, Birch EE, Chandler DL, Cotter SA, Hertle RW, Kraker RT, Moke PS, Quinn GE, Scheiman MM, Pediatric Eye Disease Investigator Group. A Randomized Trial of Patching Regimens for Treatment of Moderate Amblyopia in Children. Arch Ophthalmol. 2003 May. https://www.ncbi.nlm.nih.gov/pubmed/12742836
- Pediatric Eye Disease Investigator Group, Wallace DK, Lazar EL, et al. A Randomized Trial of Increasing Patching for Amblyopia. Ophthalmology. 2013;120(11):10.1016/j.ophtha.2013.04.008. doi:10.1016/j.ophtha.2013.04.008. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3833469/
- Scheiman MM, Hertle RW, Beck RW, Edwards AR, Birch E, Cotter SA, Crouch ER Jr, Cruz OA, Davitt BV, Donahue S, Holmes JM, Lyon DW, Repka MX, Sala NA, Silbert DI, Suh DW, Tamkins SM, Pediatric Eye Disease Investigator Group. Randomized Trial of Treatment of Amblyopia in Children Aged 7 to 17 Years. Arch Ophthalmol. 2005 Apr. https://www.ncbi.nlm.nih.gov/pubmed/15824215
- Pediatric Eye Disease Investigator Group. A Randomized Trial of Atropine Vs. Patching for Treatment of Moderate Amblyopia in Children. Arch Ophthalmol. 2002 Mar. https://www.ncbi.nlm.nih.gov/pubmed/11879129
- Scheiman MM, Hertle RW, Beck RW, Edwards AR, Birch E, Cotter SA, Crouch ER Jr, Cruz OA, Davitt BV, Donahue S, Holmes JM, Lyon DW, Repka MX, Sala NA, Silbert DI, Suh DW, Tamkins SM; Pediatric Eye Disease Investigator Group. Randomized trial of treatment of amblyopia in children aged 7 to 17 years. Arch Ophthalmol. 2005 Apr;123(4):437-47. doi: 10.1001/archopht.123.4.437
- Wallace DK, Repka MX, Lee KA, Melia M, Christiansen SP, Morse CL, Sprunger DT; American Academy of Pediatric Ophthalmology/Strabismus Preferred Practice Pattern Pediatric Ophthalmology Panel. Amblyopia Preferred Practice Pattern®. Ophthalmology. 2018 Jan;125(1):P105-P142. doi: 10.1016/j.ophtha.2017.10.008
- Sale A, Berardi N. Active training for amblyopia in adult rodents. Frontiers in Behavioral Neuroscience. 2015;9:281. doi:10.3389/fnbeh.2015.00281. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4621305/
- Baroncelli L., Sale A., Viegi A., Maya Vetencourt J. F., De Pasquale R., Baldini S., et al. . (2010). Experience-dependent reactivation of ocular dominance plasticity in the adult visual cortex. Exp. Neurol. 226, 100–109. 10.1016/j.expneurol.2010.08.009. https://www.ncbi.nlm.nih.gov/pubmed/20713044
- Maya Vetencourt J. F., Sale A., Viegi A., Baroncelli L., De Pasquale R., O’Leary O. F., et al. . (2008). The antidepressant fluoxetine restores plasticity in the adult visual cortex. Science 320, 385–388. 10.1126/science.1150516. https://www.ncbi.nlm.nih.gov/pubmed/18420937
- A cycling lane for brain rewiring. Lunghi C, Sale A. Curr Biol. 2015 Dec 7; 25(23):R1122-3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5040496/
- Wang, J., Jin, J., Malik, A., Shoge, R., Meiyeppen, S., Pang, Y., Yin, K., Allen, M., Scombordi, B., Soni, A., Neely, D. E., & Januschowski, K. (2019). Feasibility of monitoring compliance with intermittent occlusion therapy glasses for amblyopia treatment. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus, 23(4), 205.e1–205.e5. https://doi.org/10.1016/j.jaapos.2019.04.009
- Erbağcı I, Okumuş S, Öner V, Coşkun E, Çelik O, Ören B. Using liquid crystal glasses to treat ambyopia in children. J AAPOS. 2015 Jun;19(3):257-9. doi: 10.1016/j.jaapos.2015.04.001
- Spierer A, Raz J, Benezra O, Herzog R, Cohen E, Karshai I, Benezra D. Treating amblyopia with liquid crystal glasses: a pilot study. Invest Ophthalmol Vis Sci. 2010 Jul;51(7):3395-8. doi: 10.1167/iovs.09-4568
- Wang, J., Neely, D. E., Galli, J., Schliesser, J., Graves, A., Damarjian, T. G., Kovarik, J., Bowsher, J., Smith, H. A., Donaldson, D., Haider, K. M., Roberts, G. J., Sprunger, D. T., & Plager, D. A. (2016). A pilot randomized clinical trial of intermittent occlusion therapy liquid crystal glasses versus traditional patching for treatment of moderate unilateral amblyopia. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus, 20(4), 326–331. https://doi.org/10.1016/j.jaapos.2016.05.014
- Polat U. Restoration of underdeveloped cortical functions: evidence from treatment of adult amblyopia. Restor Neurol Neurosci. 2008;26(4-5):413-24.
- Campbell, F. W., Hess, R. F., Watson, P. G., & Banks, R. (1978). Preliminary results of a physiologically based treatment of amblyopia. The British journal of ophthalmology, 62(11), 748–755. https://doi.org/10.1136/bjo.62.11.748
- Xi, J., Jia, W. L., Feng, L. X., Lu, Z. L., & Huang, C. B. (2014). Perceptual learning improves stereoacuity in amblyopia. Investigative ophthalmology & visual science, 55(4), 2384–2391. https://doi.org/10.1167/iovs.13-12627
- Pediatric Eye Disease Investigator Group, Holmes, J. M., Manny, R. E., Lazar, E. L., Birch, E. E., Kelly, K. R., Summers, A. I., Martinson, S. R., Raghuram, A., Colburn, J. D., Law, C., Marsh, J. D., Bitner, D. P., Kraker, R. T., & Wallace, D. K. (2019). A Randomized Trial of Binocular Dig Rush Game Treatment for Amblyopia in Children Aged 7 to 12 Years. Ophthalmology, 126(3), 456–466. https://doi.org/10.1016/j.ophtha.2018.10.032
- Gao, T. Y., Guo, C. X., Babu, R. J., Black, J. M., Bobier, W. R., Chakraborty, A., Dai, S., Hess, R. F., Jenkins, M., Jiang, Y., Kearns, L. S., Kowal, L., Lam, C., Pang, P., Parag, V., Pieri, R., Raveendren, R. N., South, J., Staffieri, S. E., Wadham, A., … BRAVO Study Team (2018). Effectiveness of a Binocular Video Game vs Placebo Video Game for Improving Visual Functions in Older Children, Teenagers, and Adults With Amblyopia: A Randomized Clinical Trial. JAMA ophthalmology, 136(2), 172–181. https://doi.org/10.1001/jamaophthalmol.2017.6090
- Birch, E. E., Li, S. L., Jost, R. M., Morale, S. E., De La Cruz, A., Stager, D., Jr, Dao, L., & Stager, D. R., Sr (2015). Binocular iPad treatment for amblyopia in preschool children. Journal of AAPOS : the official publication of the American Association for Pediatric Ophthalmology and Strabismus, 19(1), 6–11. https://doi.org/10.1016/j.jaapos.2014.09.009
- Holmes, J. M., Manh, V. M., Lazar, E. L., Beck, R. W., Birch, E. E., Kraker, R. T., Crouch, E. R., Erzurum, S. A., Khuddus, N., Summers, A. I., Wallace, D. K., & Pediatric Eye Disease Investigator Group (2016). Effect of a Binocular iPad Game vs Part-time Patching in Children Aged 5 to 12 Years With Amblyopia: A Randomized Clinical Trial. JAMA ophthalmology, 134(12), 1391–1400. https://doi.org/10.1001/jamaophthalmol.2016.4262
- Kelly, K. R., Jost, R. M., Dao, L., Beauchamp, C. L., Leffler, J. N., & Birch, E. E. (2016). Binocular iPad Game vs Patching for Treatment of Amblyopia in Children: A Randomized Clinical Trial. JAMA ophthalmology, 134(12), 1402–1408. https://doi.org/10.1001/jamaophthalmol.2016.4224
- Manh, V. M., Holmes, J. M., Lazar, E. L., Kraker, R. T., Wallace, D. K., Kulp, M. T., Galvin, J. A., Shah, B. K., Davis, P. L., & Pediatric Eye Disease Investigator Group (2018). A Randomized Trial of a Binocular iPad Game Versus Part-Time Patching in Children Aged 13 to 16 Years With Amblyopia. American journal of ophthalmology, 186, 104–115. https://doi.org/10.1016/j.ajo.2017.11.017
- Barker AT, Jalinous R, Freeston IL. Non-invasive magnetic stimulation of human motor cortex. Lancet. 1985 May 11;1(8437):1106-7. doi: 10.1016/s0140-6736(85)92413-4
- Hess RF, Thompson B. New insights into amblyopia: binocular therapy and noninvasive brain stimulation. J AAPOS. 2013 Feb;17(1):89-93. doi: 10.1016/j.jaapos.2012.10.018
- Iuvone PM, Tigges M, Fernandes A, Tigges J. Dopamine synthesis and metabolism in rhesus monkey retina: development, aging, and the effects of monocular visual deprivation. Vis Neurosci. 1989;2(5):465-71. doi: 10.1017/s0952523800012360
- Gottlob I, Stangler-Zuschrott E. Effect of levodopa on contrast sensitivity and scotomas in human amblyopia. Invest Ophthalmol Vis Sci. 1990 Apr;31(4):776-80. https://iovs.arvojournals.org/article.aspx?articleid=2199671
- Pediatric Eye Disease Investigator Group, Repka, M. X., Kraker, R. T., Dean, T. W., Beck, R. W., Siatkowski, R. M., Holmes, J. M., Beauchamp, C. L., Golden, R. P., Miller, A. M., Verderber, L. C., & Wallace, D. K. (2015). A randomized trial of levodopa as treatment for residual amblyopia in older children. Ophthalmology, 122(5), 874–881. https://doi.org/10.1016/j.ophtha.2015.01.002
- Pawar, P. V., Mumbare, S. S., Patil, M. S., & Ramakrishnan, S. (2014). Effectiveness of the addition of citicoline to patching in the treatment of amblyopia around visual maturity: a randomized controlled trial. Indian journal of ophthalmology, 62(2), 124–129. https://doi.org/10.4103/0301-4738.128586
- Campos EC, Bolzani R, Schiavi C, Baldi A, Porciatti V. Cytidin-5′-diphosphocholine enhances the effect of part-time occlusion in amblyopia. Doc Ophthalmol. 1996-1997;93(3):247-63. doi: 10.1007/BF02569065
- Campos EC, Schiavi C, Benedetti P, Bolzani R, Porciatti V. Effect of citicoline on visual acuity in amblyopia: preliminary results. Graefes Arch Clin Exp Ophthalmol. 1995 May;233(5):307-12. doi: 10.1007/BF00177654
- Razeghinejad MR, Nowroozzadeh MH, Eghbal MH. Levodopa and Other Pharmacologic Interventions in Ischemic and Traumatic Optic Neuropathies and Amblyopia. Clin Neuropharmacol. 2016 Jan-Feb;39(1):40-8. doi: 10.1097/WNF.0000000000000115
- Vagge A, Nelson LB. Amblyopia update: new treatments. Curr Opin Ophthalmol. 2016 Sep;27(5):380-6. doi: 10.1097/ICU.0000000000000293
- Kraus, C. L., & Culican, S. M. (2018). New advances in amblyopia therapy II: refractive therapies. The British journal of ophthalmology, 102(12), 1611–1614. https://doi.org/10.1136/bjophthalmol-2018-312173
- Pediatric Eye Disease Investigator Group. Randomized trial of treatment of amblyopia in children aged 7 to 17 years. Arch Ophthalmol 2005;123(4):437-47.
- Kelly KR, Jost RM, De La Cruz A, et al. Slow reading in children with anisometropic amblyopia is associated with fixation instability and increased saccades. J AAPOS. 2017 Dec;21(6):447-451.