What are eye exercises
Eye exercises or vision training consists of a variety of programs designed to enhance visual efficiency and processing 1. Eye exercises or orthoptics, typically addresses how well both eyes work together. Eye exercises may include 1:
- muscle relaxation techniques,
- biofeedback,
- eye patches,
- eye massages,
- the use of under-corrected prescription lenses, and/or
- nutritional supplements.
Training is most often provided by an optometrist.
Eye exercises are often prescribed in vision therapy to resolve issues relating to vergence, ocular motility disorders, accommodative dysfunction, amblyopia, learning disabilities, dyslexia, asthenopia, myopia, motion sickness, sports performance, stereopsis, visual field defects, and visual acuity 2. Eye exercises are also practiced to enhance sports performance and used during yoga to promote general well-being 3. However, few studies exist on evaluating the outcomes and efficacy of this type of therapy. One such study found a measurable effect of eye exercise in patients with convergence problems 4. Additional research suggests eye exercise facilitates improvement in stereoscopic skills and visual field remnants after brain damage 5; and there has been evidence to link visual attention and visual working memory 6. Aside from these areas, there exists no other research implicating eye exercise as an effective treatment for other types of visual or cognitive deficits. Despite this lack of empirical peer reviewed research, eye exercise remains a popular technique/therapy as demonstrated by a Google search of “eye exercise.”
A study 7 on eye exercises suggests that eye exercises may prove useful in enhancing cognitive performance on tasks related to attention and memory over a very brief course of training. Moreover, further research is needed on eye exercises to determine whether they are an effective treatment for patients with cognitive and eye-related disorders 7.
Perhaps the most popular type of vision therapy is the ‘See Clearly’ technique established by ophthalmologist William Horatio Bates 8. His book, The Cure of Imperfect Sight by Treatment without Glasses 9, highlights a wide assortment of possible therapeutic eye exercises, one of which requires patients to shifting their fixation between two targets repeatedly without staring. Discussion on Bates eye exercises can be found at the end of this article.
Eye Comfort Exercises 10
- Blinking (produces tears to help moisten and lubricate the eyes).
- Yawning (produces tears to help moisten and lubricate the eyes).
- Expose eyes to natural light.
Eye Movements Exercises 10
- Close eyes.
- Slowly and gently move eyes up to the ceiling, then slowly down to the floor.
- Repeat 3 times.
- Close eyes.
- Slowly and gently move eyes to the left, then slowly to the right.
- Repeat 3 times.
Focus Change Eye Exercises 10
- Hold one finger a few inches away form the eye.
- Focus on the finger.
- Slowly move the finger away.
- Focus far into the distance and then back to the finger.
- Slowly bring the finger back to within a few inches of the eye.
- Focus on something more than 8 feet away.
- Repeat 3 times.
One randomized controlled trial of biofeedback training for control of accommodation for myopia reported no statistically significant benefits from training 11. Another randomized controlled trial conducted in 2013 12, which investigated vision training modalities to evaluate changes in peripheral refraction profiles in myopes, also found no evidence of benefits. In other studies 13, 14, 15 undertaken over the last 60 years, an improvement in subjective visual acuity in myopes with no corresponding improvement in objective VA has been reported.
In summary, based on evidence obtained from at least one properly designed randomized controlled trial, visual training for control of accommodation has no effect on myopia 1. In other studies obtained from well-designed controlled trials without randomization, an improvement in subjective visual acuity for patients with myopia that have undertaken visual training has been shown, but no corresponding physiological cause for the improvement has been demonstrated 1. It is postulated that the improvements in myopic patients noted in these studies were due to improvements in interpreting blurred images, changes in mood or motivation, creation of an artificial contact lens by tear film changes, or a pinhole effect from miosis of the pupil 1.
No evidence was found that visual training 1) has any effect on the progression of myopia; 2) improves visual function for patients with hyperopia or astigmatism; or 3) improves vision lost through disease processes, such as age-related macular degeneration, glaucoma, or diabetic retinopathy 1.
Eye exercises for myopia
Myopia is a public health problem worldwide, especially in Asian countries such as Singapore, Japan and China 16. Myopic retinopathy occurs in about 40% of highly myopic eyes 17 and has become the second leading cause of blindness and low vision in Chinese, ranging from 7.7%–32.7% 18, 19. Myopia has emerged as a major health issue in east Asia, because of its increasingly high prevalence in the past few decades (now 80-90% in school-leavers) and because of the sight-threatening pathologies associated with high myopia, which now affects 10-20% of those completing secondary schooling in this part of the world 17.
Myopic retinopathy is also one of the most common causes (6%) of visual impairment and blindness in European-derived populations 20. Therefore, any kind of method designed for preventing or slowing myopia progression deserve scientific evaluation on its efficacy and safety for controlling myopia.
Chinese eye exercises, a kind of massage around periocular acupoints, were originated and imbued with theories of traditional Chinese medicine 21. Since 1963, the Chinese government has endorsed these exercises in the belief that they protect vision and may prevent myopia in children. They have become a community ritual and a living habit of students in primary and middle school in China for half a century. Meanwhile, myopia prevalence in Chinese children has increased remarkably and reached epidemic levels (30.1%~78.4%) in recent decades 22, 23. Therefore, it would not appear that these eye exercised play a critical role in preventing myopia 24 or alleviate eyestrain. A 2011 Cochrane Review 24 found no conclusions can be drawn for the benefit of co-acupressure for slowing progress of myopia in children. Further evidence in the form of randomized controlled trials are needed before any recommendations can be made for the use of acupuncture treatment in clinical use. These trials should compare acupuncture to placebo and have large sample sizes. Other types of acupuncture (such as auricular acupuncture) should be explored further as well as compliance with treatment for at least six months or longer. Axial length elongation of the eye should be investigated for at least one year. The potential to reduce/eliminate pain from acupuncture experienced by children should also be reviewed.
Although it was reported that doing Chinese eye exercises might not related to the prevalence of myopia in children 25, some argue that the prevalence might have been much greater had children not performed the exercises. Some studies showed that about 90% of Chinese children didn’t perform these exercises correctly although they did them everyday 26. Most Chinese children couldn’t find the exact periocular acupoints and didn’t have accurate pressure and manipulation skills for the exercises 27, 26.
The finding from this study 28 indicated that Chinese eye exercises did not correct near and distant visual acuity, however, it transiently alleviate accommodative lag in children at a statistically but probably clinically insignificant level. This conclusion was in agreement with the 2011 Cochrane Review 24 that showed no conclusions can be drawn for the benefit of co-acupressure for slowing progress of myopia in children.
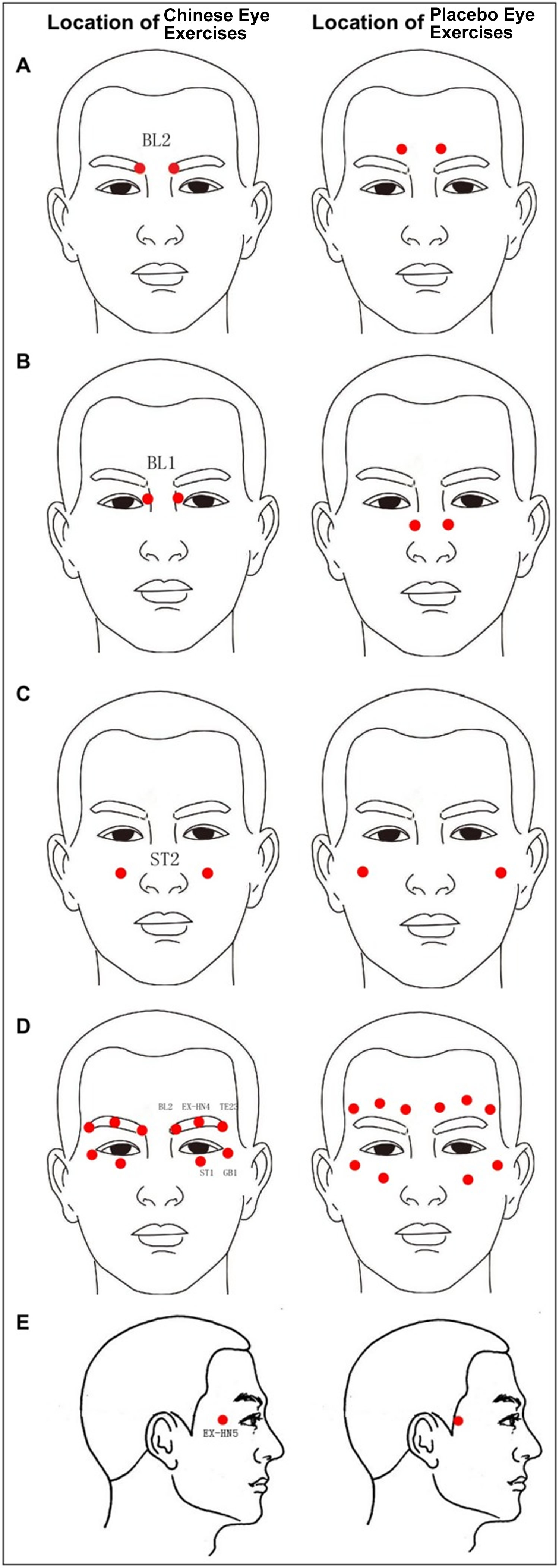
Figure 1. Locations of acupoints of standard Chinese Eye Exercises and Placebo point eye exercises
[Source 28]Table 1. Manipulation Methods Used in the Standard Chinese Eye Exercises
| Acupoint Code (Name in Chinese) | Manipulation | Location of standard Chinese eye exercises |
|---|---|---|
| 1-BL2 (cuanzhu) | Press in circle for 1min | In the supraorbital notch and at the median end of the eyebrow |
| 2-BL1 (jingming) | Press in circle for 1min | In the depression slightly above the inner canthus |
| 3-ST2 (sibai) | Press in circle for 1min | Directly below the pupil, in the depression of the infraorbital foramen |
| 4-EX-HN5 (taiyang) | Press in circle for 30s | Flat part at each side of the forehead |
| TE-23 (sizhukong), EX-HN4 (yuyao), BL2 (cuanzhu),GB1 (tongziliao), ST1 (chengqi) | Scrape the eyebrows for 30s | On the orbit |
Eye exercises for double vision
Eye exercises for double vision, convergence insufficiency, heterophoria, and intermittent strabismus have been in use for over 70 years 29. Convergence insufficiency is the inability to maintain binocular function (keeping the two eyes working together) while working at a near distance 30. Typically, one eye will turn outward (intermittent exotropia) when focusing on a word or object at near. Common symptoms of convergence insufficiency include diplopia (double vision) and headaches when reading. Many patients will complain that they have difficulty concentrating on near work (computer, reading, etc.) and that the written words will move around and become blurry after prolonged periods of reading. Patients may be noted to squint or close one eye when reading. Symptoms can vary with convergence insufficiency and not all symptoms are present in every patient 30 and loss of comprehension after short periods of reading or performing close activities 31, 32. Thus, convergence insufficiency may negatively impact health-related quality of life, potentially interfering with reading and near work performed for school, work, and/or leisure.
Convergence insufficiency is diagnosed by an ophthalmologist, optometrist or orthoptist after obtaining a history of the patient’s symptoms and measuring convergence ability. The examination includes determining the distance from the eyes that the patient can hold the eyes together without double vision (near point of convergence) and the amount of prism that can be placed in front of the eyes at a particular distance before double vision is seen (fusional vergence amplitude). Presence of any refractive errors, eye muscle dysfunction, or weaknesses in accommodation (near focusing) should also be evaluated.
Does every patient who meets criteria for convergence insufficiency require treatment ?
During a routine eye examination, convergence weakness may be diagnosed even without the above-mentioned symptoms. Some patients test in the office as having poor convergence; however, they are asymptomatic. This may be the result of true convergence weakness, but is often found when the patient is distracted, shy, overly excited or does not understand the directions given. These patients should either be retested at another time or simply watched for symptoms of diplopia or headaches with near work. A patient who is not having difficulty with near tasks but tests positive for convergence insufficiency in the office does not require any treatment but should be followed.
Conversely, a child with adequate convergence in the office may occasionally have symptoms at home or school consistent with convergence insufficiency. In these cases, a course of treatment for convergence weakness can be instituted and the child followed for improvement in symptoms.
What is the method of treatment for convergence insufficiency ?
Convergence insufficiency can often be treated by practicing convergence through exercises. These exercises may be prescribed by an orthoptist (a medical technician who is specifically trained in ocular muscle function and binocular vision) or by an ophthalmologist. There is also a computer program available which may be used on a home computer to increase convergence ability. The results of the computer program are often followed by your eye care professional with print outs that can be brought in to the office visit.
Which method of treatment will be used for an individual patient depends on the age of the patient requiring treatment, the proximity to an orthoptist or vision therapist and the preference of the patient. Important aspects to consider in choosing a treatment regimen are the convenience and expense of treatment as any method chosen tends to be successful if the prescribed regimen in followed. Most studies show that a short course of treatment is usually successful. Prolonged therapy does not show significant advantages and is usually unnecessary.
Is convergence insufficiency permanent ?
Patients with convergence insufficiency are often permanently cured after exercises to strengthen their convergence. Continued near work following convergence therapy tends to help maintain adequate convergence once treatment is discontinued. At times, convergence insufficiency symptoms will resurface after illness, lack of sleep or increased near work demands. If treatment had been successful previously, an additional course of treatment tends be successful at resolving recurrent symptoms.
Are there associated problems with vision in patients with convergence insufficiency ?
Patients with convergence insufficiency usually have a normal range of refractive errors and good visual function. Testing for accommodative amplitude (the ability to focus each eye individually at near) is always performed by the specialist evaluating convergence. Rarely, this is also found to be weak. If both accommodation and convergence are weak, reading glasses, sometimes with prism added, may be a great option for these patients. It is very difficult to improve accommodation with exercises.
Eye exercises for double vision
Eye exercises for double vision or convergence insufficiency may involve intensive, clinic-based vision training or simpler, home-based, exercises. Orthoptists have generally adopted less intensive methods over the decades, while “vision therapy” textbooks and some branches of optometry continue to support intensive therapy 33. Orthoptists are allied health care practitioners traditionally involved in the management of patients with eye movement disorders and specifically with strabismus (squint), double vision and amblyopia (lazy eye). The lack of strong evidence was identified by the Convergence Insufficiency Treatment Trial Group in designing a large multicenter trial 34 comparing the effects of different treatment regimens on convergence insufficiency, a condition where most professionals agree that exercises are effective. Studies clearly suggest that children receiving office-based therapy had the best outcome 35, 36 compared to home-based methods; however, despite great efforts in the study design, true treatment effects and particularly the added benefit of therapist encouragement on simple exercises, could have accounted for apparent additional improvements in patients receiving intensive office therapy.
The Convergence Insufficiency Treatment Trial (CITT) is the first large-scale, randomized clinical trial to evaluate active treatments for symptomatic convergence insufficiency in children (9-17 years of age). The treatment prescribed was either home-based or office-based therapy involving a sequence of activities to develop efficient visual skills. The CITT trials 35 showed that 35% of patients improved with office-based placebo therapy, indicating that placebo and encouragement effects were significant. The additional advantage that the CITT found of in-office therapy could be due to the additive effects of patients being taught the importance of effort in addition to the eye exercises themselves rather than the intrinsic superiority of the more specific or intensive therapeutic techniques. The CITT trials also found that the specific form of vision therapy/orthoptics described as office-based vergence/accommodative therapy with home reinforcement is the most effective form of treatments for symptomatic convergence insufficiency in children, with about 75% of patients achieving normalization of or improvement in symptoms and signs within a 12-week period.
1) Home-based Pencil Push-ups
The Convergence Insufficiency Treatment Trial (CITT) pencil push-ups procedure used a pencil with 20/60 size letters and a white index card placed in the background to provide a suppression check by using physiological diplopia awareness. The goal of the procedure was to move the pencil to within 2 to 3 cm of the brow, just above the nose on each push-up. Patients were instructed to perform the pencil push-ups procedure 15 minutes per day, 5 days per week. They maintained home therapy log forms, recording the closest distance that they could maintain fusion after each 5 minutes of therapy
2) Home-based Computer Vergence/Accommodative Therapy and Pencil Push-ups
The home-based computer vergence/accommodative therapy and pencil push-ups group practiced the same pencil push-up procedure as the home-based pencil push-ups group. In addition, they performed fusional vergence and accommodative therapy procedures with the Home Therapy System (HTS) computer software (Home Therapy Systems, Gold Canyon, AZ). The vergence base in, vergence base out, auto-slide vergence, and jump ductions vergence programs using random dot stereopsis targets were used for fusional vergence training and the accommodative rock program was used for accommodative therapy. Therapy was prescribed to be performed at home for 20 minutes per day (15 minutes for HTS and 5 minutes for pencil push-ups), 5 days per week. Patients maintained a home therapy log form and recorded the closest distance to which they could converge and maintain fusion for pencil push-up therapy and the level completed for each session of computer therapy.
3) Office-based vergence/accommodative therapy with home reinforcement
Patients in the office-based treatment groups were scheduled for weekly in-office appointments with the therapist lasting approximately 60 minutes per visit during which time in-office procedures were performed, home therapy procedures were demonstrated, the home therapy log was reviewed, and the therapist verbally motivated the patient in an attempt to maximize adherence. Patients in the office-based treatment groups were prescribed 15 minutes of home therapy procedures to be completed 5 days per week. To enhance compliance we asked patients to log their home therapy activities including minutes spent on therapy and therapy goals achieved.
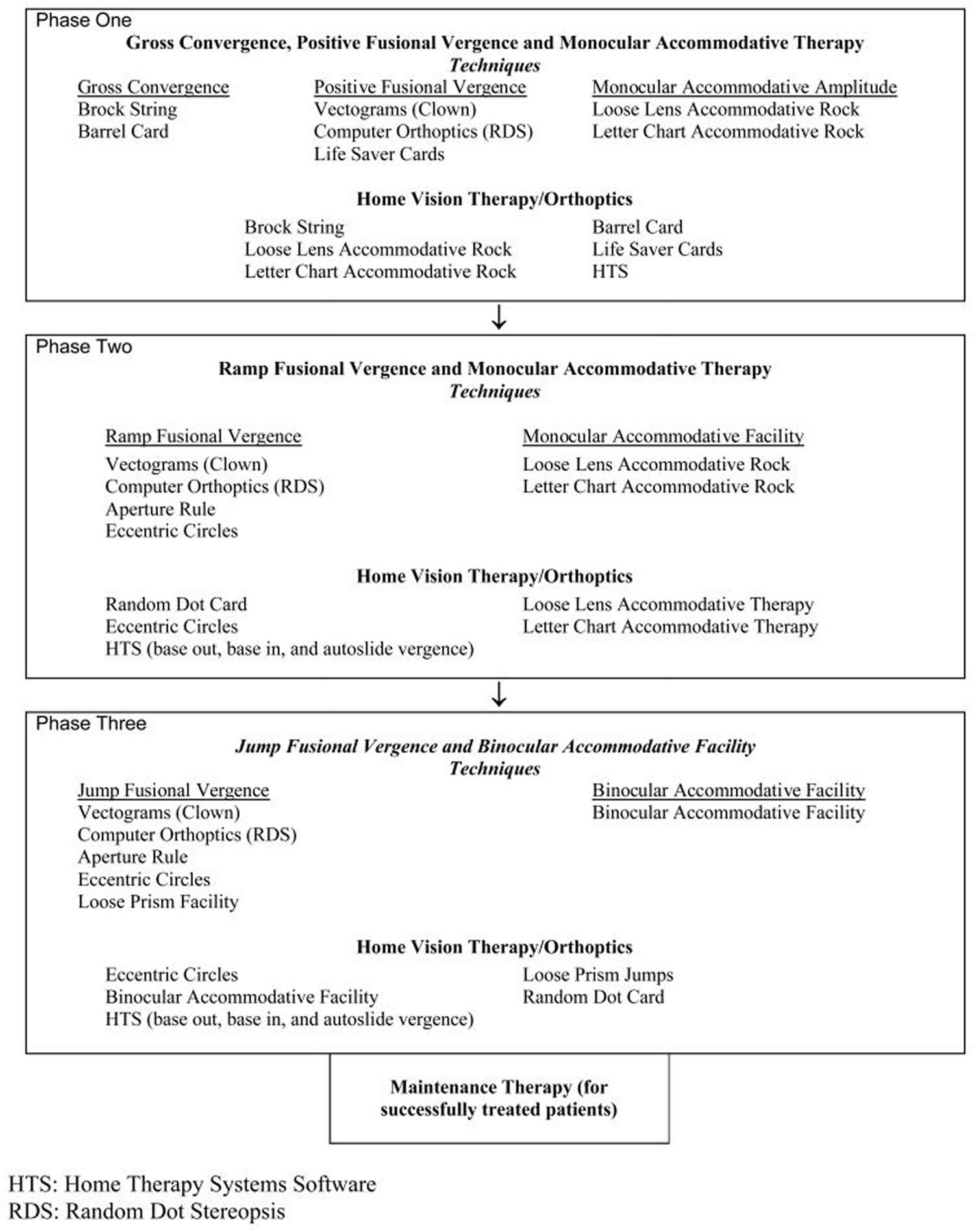
Office-based vergence/accommodative therapy with home reinforcement was administered by a therapist on an individual basis combined with procedures to perform at home. The treatment program consisted of 3 phases. Within each phase there were a number of subcategories wherein therapy procedures were arranged sequentially from easiest to most difficult. The therapy program is summarized in Table 2 and described in detail in Chapter 8 of the CITT Manual of Procedures that can be accessed at https://optometry.osu.edu/CITT-about.
Table 2. Office-Based Vergence/Accommodative Therapy With Home Reinforcement Protocol
[Source 37]Six eye exercise groups: accommodation, vergence, both, convergence in excess of accommodation, accommodation in excess of convergence. Although exercises stressing more convergence than accommodation (positive relative vergence/ negative relative accommodation) would be expected to lead to better convergence gain and responses for near than for accommodation, and exercises stressing accommodation more than convergence (positive relative accommodation or negative relative vergence) would be expected to have the opposite effect, neither strategy made any significant difference over the no treatment (nil) group.
True treatment effects were small and significantly better only after vergence exercises to a nonaccommodative target, and rarely related to the response they were designed to improve. Exercising accommodation without convergence made no difference to accommodation to cues containing detail. Additional effort improved objective responses the most.
Is convergence insufficiency treatment always successful ?
Occasionally, a patient will not respond to therapy. In these cases, prism glasses may be used for reading in order to artificially align the eyes and allow for more comfortable binocular vision. In rare cases, surgical intervention may be suggested.
Using of base-out prisms which force the eyes to work harder to converge. They are used only during short periods of time while performing therapy as they are very tiring to the eyes.
Base-in prisms can be used to artificially align the eyes for reading; however, their use will make it unlikely that the patient will develop stronger convergence on their own.
Patching is not an option to strengthen convergence because wearing a patch will disrupt any ability to exercise binocular function (use the two eyes together). Occasionally, patients will patch one eye temporarily in order to relieve double vision during times when a large amount of near work is required.
Eye exercises for lazy eye
Amblyopia (lazy eye), is a major developmental visual disorder that occurs in 1–5% of the world population and is typically caused by an early abnormal visual experience which occurs during a well defined critical period, which is around 6–8 years of age in children. Typical causes of amblyopia are strabismus, image degradation due to refractive errors, or congenital cataract 38. The most common form of the disorder, unilateral amblyopia, results in a marked visual acuity impairment in the affected eye, together with reduced stereopsis, and low contrast and motion sensitivity. The physiology of the retina is generally spared in amblyopia 39, while the lateral geniculate nucleus of the thalamus can appear atrophic 40. There is large consensus, however, that amblyopia is prevalently caused by neural dysfunctions occurring in the primary visual cortex 41.
Most important, recovery of normal visual functions is almost impossible after critical period end, i.e., after 8 years of age in children. Thus, the critical period for the appearance of amblyopia is paralleled by a sensitive period for the success of therapeutic strategies 42.
Currently there is no human studies on eye exercises for lazy eye (amblyopia). The only research we could find was on mice. That research 43 has demonstrated that voluntary physical exercise and visual perceptual learning, two totally non invasive procedures, share the remarkable capability to potentiate plasticity in the adult visual cortex, favoring recovering of visual functions in adult amblyopic rodents. Running and locomotion is associated not only with activation of cortical Vasoactive Intestinal Peptide neurons, but also with increases in multiple neuromodulators, including serotonin, which has been shown to be enhanced by environmental enrichment 44 and to promote adult primary visual plasticity 45. The impact of physical exercise on amblyopic adults remains to be elucidated, with preliminary results in this laboratory study showing a strong enhancement of visual cortical plasticity in healthy subjects after a period of voluntary physical activity 46.
Bates eye exercises
William Horatio Bates was a fully trained ophthalmologist in the late 1800s 47. William Bates attributed nearly all sight problems to habitual strain of the eyes, and felt that glasses were harmful and never necessary. Bates self-published a book, Perfect Sight Without Glasses, as well as a magazine, Better Eyesight Magazine, detailing his approach to helping people relax such “strain”, and thus, he claimed, improve their sight. His techniques centered on visualization and movement. He placed particular emphasis on imagining black letters and marks, and the movement of such. He also felt that exposing the eyes to sunlight would help alleviate the “strain” 48.
Despite continued anecdotal reports of successful results, including well-publicised support by Aldous Huxley, Bates’ techniques have not been objectively shown to improve eyesight 49.
Bates’ techniques have never been scientifically established to improve eyesight 49. Several of Bates’ techniques, including “sunning”, “swinging”, and “palming”, were combined with healthy changes to diet and exercise in a 1983 randomized controlled trial of myopic children in India. After 6 months, the experimental groups “did not show any statistically significant difference in refractive status”, though the children in the treatment group “subjectively … felt relieved of eye strain and other symptoms” 50.
In 1967 the British Medical Journal observed that “Bates advocated prolonged sun-gazing as the treatment of myopia, with disastrous results” 51.
Natural vision correction is the belief that you can improve your vision with eye exercises, relaxation techniques, and an eye massage every now and then. Some people swear by it. Others say it’s nonsense. However, there’s no proof the technique works, only wishful thinking, says Michael Repka, a professor at Johns Hopkins University School of Medicine 52.
Bates main physiological proposition—that the eyeball changes shape to maintain focus—has consistently been contradicted by observation 53. In 1952, optometry professor Elwin Marg wrote of Bates, “Most of his claims and almost all of his theories have been considered false by practically all visual scientists” 54. Prof. Marg concluded that the Bates method owed its popularity largely to “flashes of clear vision” experienced by many who followed it 55. Such occurrences have since been explained as a contact lens-like effect of moisture on the eye 56, or a flattening of the lens by the ciliary muscles 57, 58.
The Bates method has been criticized not only because there is no good evidence it works, but also because it can have negative consequences for those who attempt to follow it: they might damage their eyes through overexposure of their eyes to sunlight, put themselves and others at risk by not wearing their corrective lenses while driving, or neglect conventional eye care, possibly allowing serious conditions to develop 54, 59.
In his writings, Bates discussed several techniques that he claimed helped patients to improve their sight. He wrote “The ways in which people strain to see are infinite, and the methods used to relieve the strain must be almost equally varied” 9, emphasizing that no single approach would work for everyone. His techniques were all designed to help disassociate this “strain” from seeing and thereby achieve “central fixation”, or seeing what is in the central point of vision without staring. He asserted that “all errors of refraction and all functional disturbances of the eye disappear when it sees by central fixation” and that other conditions were often relieved as well 48.
Palming
Bates suggested closing the eyes for minutes at a time to help bring about relaxation 60. He asserted that the relaxation could be deepened in most cases by “palming”, or covering the closed eyes with the palms of the hands, without putting pressure on the eyeballs 48. If the covered eyes did not strain, he said, they would see “a field so black that it is impossible to remember, imagine, or see anything blacker”, since light was excluded by the palms. However, he reported that some of his patients experienced “illusions of lights and colors” sometimes amounting to “kaleidoscopic appearances” as they “palmed”, occurrences he attributed to his ubiquitous “strain” and that he claimed disappeared when one truly relaxed 60. This phenomenon, however, was almost certainly caused by Eigengrau or “dark light”. In fact, even in conditions of perfect darkness, as inside a cave, neurons at every level of the visual system produce random background activity that is interpreted by the brain as patterns of light and color 61.
Figure 8. Bates palming technique requires placing the palms of the hands over the eyes and imagining colorful pictures
Sunning
Bates believed that the eyes were benefited by exposure to sunlight. He stated that “persons with normal sight can look directly at the sun, or at the strongest artificial light, without injury or discomfort,” 62 and gave several examples of patients’ vision purportedly improving after sungazing – this is at variance with the well-known risk of eye damage that can result from direct sunlight observation.
Bates said that, just as one should not attempt to run a marathon without training, one should not immediately look directly at the sun, but he suggested that it could be worked up to. He acknowledged that looking at the sun could have ill effects, but characterized them as being “always temporary” and in fact the effects of strain in response to sunlight. He wrote that he had cured people who believed that the sun had caused them permanent eye damage 63. In his magazine, Bates later suggested exposing only the white part of the eyeball to direct sunlight, and only for seconds at a time, after allowing the sun to shine on closed eyelids for a longer period 64.
- Warning: The Bates’ Sunning procedure is potentially harmful to your vision may even lead to loss of vision or blindness ! Looking at the sun without wearing proper protective sunglasses, the retina or even worse, the macula can be burnt. Sun-gazing in any form is potentially hazardous to your vision.
Movement
Bates thought that the manner of eye movement affected the sight. He suggested “shifting”, or moving the eyes back and forth to get an illusion of objects “swinging” in the opposite direction. Bates believed that the smaller the area over which the “swing” was experienced, the greater was the benefit to sight. He also indicated that it was usually helpful to close the eyes and imagine something “swinging”. By alternating actual and mental shifting over an image, Bates wrote, many patients were quickly able to shorten the “shift” to a point where they could “conceive and swing a letter the size of a period in a newspaper” 65. One who mastered this would attain the “universal swing”, Bates believed 48.
Perhaps finding Bates’ concepts of “shifting” and “swinging” too complicated, some proponents of vision improvement, such as Bernarr Macfadden, suggested simply moving the eyes up and down, from side to side, and shifting one’s gaze between a near-point and a far-point 48.
Visualization
Bates placed importance on mental images, as he felt relaxation was the key to clarity of imagination as well as of actual sight 66. He claimed that one’s poise could be gauged by the visual memory of black; that the darker it appeared in the mind, and the smaller the area of black that could be imagined, the more relaxed one was at the moment 67. Bates recommended that patients think of the top letter from an eye chart and then visualize progressively smaller black letters, and eventually a period or comma 48. But he emphasized his view that the clear visual memory of black “cannot be attained by any sort of effort”, stating that “the memory is not the cause of the relaxation, but must be preceded by it” 67 and cautioned against “concentrating” on black, as he regarded an attempt to “think of one thing only” as a strain 60.
While Bates preferred to have patients imagine something black, he also reported that some found objects of other colors easiest to visualize, and thus were benefited most by remembering those, because, he asserted, “the memory can never be perfect unless it is easy” 67. Scientists reason that the only benefit to eyesight gained from such techniques is itself imagined, and point out that familiar objects, including letters on an eye chart, can be recognized even when they appear less than clear 61.
Clinical implications
- The placebo effect and memorisation
This begs the question of what is the cause of the improvements in vision reported by people who use Bates method ? It could be partly due to the placebo effect, in that randomized controlled trials have shown significant improvements in visual acuity and symptoms with placebo ‘treatments’ of glasses with no power 68 or ‘sugar pills’ 69. Given that the placebo effect appears to be greater the more dramatic the treatment (four placebo sugar pills a day are more effective than two for eradicating gastric ulcers, salt water injections are a more effective treatment for pain than sugar pills) 70, perhaps the regimen proposing the largest array of strenuous eye exercises would provide the largest placebo effect. Part of any improvement may be simply memorisation, in that most of the Bates method books include a Snellen letter chart for readers to monitor their visual acuity and with repetitive measurements, some learning of the subset of letters is likely 71, 72.
- Blur adaptation and perceptual learning
However, the most likely causes of improvements in vision are blur adaptation 73, 74, 75, 76, 77, 78 (in the short-term) and perceptual learning[27-30] (in the longer term and if demanding visual tasks are involved in the treatment). Both of these topics are discussed in articles in this issue of OPO by Sotiris Plainis and colleagues of the University of Crete 78, 79. It is now well known that with sudden blur (such as when taking off myopic glasses or when blur lenses are added in research experiments), the visual system will adapt to improve visual acuity 73, 74, 75, 76, 77, 78, likely by increasing the gain of high spatial frequency channels and decreasing the gain of low frequency channels 75. Improvements of more than two lines of acuity have been reported[22, 24, 26] and these are typically greater in myopes[22, 26] and possibly greatest in high myopes 78. However, blur adaptation seems short-lasting (the time course of the condition is as yet unclear) and long-term improvements may be more likely using perceptual learning (which may trigger and/or enhance the process of blur adaptation) 80 which has been shown to lead to improvements in distance visual acuity in adult amblyopes 81, 82 and in the ‘good eye’ of patients with severe impairment in the other eye 79 and improvements in near visual acuity to a level where reading glasses were not necessary in early presbyopes 83. The suggestion is that perceptual learning (repeated practice on a demanding visual task) can increase the efficiency of neural processing in order to perform ‘de-blurring’ of blurred images and retrieve the information for further processing 83. Given that the Bates method emphasizes repeated relaxation of the eyes, rather than repeated practice on a demanding task, it seems likely that its positive effects are dominated by blur adaptation plus the placebo effect and memorisation rather than perceptual learning.
Conclusion
Don’t waste your money on Bates eye exercises. Save your money and time on other corrective eye exercises and wear your glasses or contact lenses if they could help you see better right away.
References- American Academy of Ophthalmology. Visual Training for Refractive Errors CTA – 2013. https://www.aao.org/complimentary-therapy-assessment/visual-training-refractive-errors-cta–october-200
- A systematic review of the applicability and efficacy of eye exercises. Rawstron JA, Burley CD, Elder MJ. J Pediatr Ophthalmol Strabismus. 2005 Mar-Apr; 42(2):82-8. https://www.ncbi.nlm.nih.gov/pubmed/15825744/
- Chinese eye exercises. Roy FH. J Pediatr Ophthalmol Strabismus. 1980 May-Jun; 17(3):198-202. https://www.ncbi.nlm.nih.gov/pubmed/7391914/
- The efficacy of vision therapy for convergence excess. Gallaway M, Schieman M. J Am Optom Assoc. 1997 Feb; 68(2):81-6. https://www.ncbi.nlm.nih.gov/pubmed/9120214/
- Vision therapy for oculomotor dysfunctions in acquired brain injury: a retrospective analysis. Ciuffreda KJ, Rutner D, Kapoor N, Suchoff IB, Craig S, Han ME. Optometry. 2008 Jan; 79(1):18-22. https://www.ncbi.nlm.nih.gov/pubmed/18156092/
- Interactions between working memory, attention and eye movements. Theeuwes J, Belopolsky A, Olivers CN. Acta Psychol (Amst). 2009 Oct; 132(2):106-14. https://www.ncbi.nlm.nih.gov/pubmed/19233340/
- Di Noto P, Uta S, DeSouza JFX. Eye Exercises Enhance Accuracy and Letter Recognition, but Not Reaction Time, in a Modified Rapid Serial Visual Presentation Task. Hamed SB, ed. PLoS ONE. 2013;8(3):e59244. doi:10.1371/journal.pone.0059244. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3602039/
- Visual training: current status in ophthalmology. Helveston EM. Am J Ophthalmol. 2005 Nov; 140(5):903-10. https://www.ncbi.nlm.nih.gov/pubmed/16310470/
- Bates, William H. (1920). “Chapter 9: The Cause and Cure of Errors of Refraction”. Perfect Sight Without Glasses. New York: Central Fixation Publishing Co. pp. 89–105. ISBN 88-900756-3-5.
- Office of Management, National Institutes of Health. Exercises and Stretches. https://www.ors.od.nih.gov/sr/dohs/HealthAndWellness/Ergonomics/Pages/exercises.aspx
- Koslowe KC, Spierer A, Rosner M, Belkin M. Evaluation of accommotrac biofeedback training for myopia control. Optom Vis Sci 1991;68:338-43.
- Radhakrishnan H, Allen PM, Calver RI, Theagarayan B, Price H, Rae S, Sailoganathan A, O’Leary DJ. Peripheral refractive changes associated with myopia progression. Invest Ophthalmol Vis Sci 2013: 54: 1573-1581.
- Angi MR, Caucci S, Pilotto E, et al. Changes in myopia, visual acuity, and psychological distress after biofeedback visual training. Optom Vis Sci 1996;73:35-42.
- Rupolo G, Angi M, Sabbadin E, et al. Treating myopia with acoustic biofeedback: a prospective study on the evolution of visual acuity and psychological distress. Psychosom Med 1997;59:313-7.
- Gilmartin B, Gray LS, Winn B. The amelioration of myopia using biofeedback of accommodation: a review. Ophthalmic Physiol Opt 1991;11:304-13.
- Worldwide prevalence and risk factors for myopia. Pan CW, Ramamurthy D, Saw SM. Ophthalmic Physiol Opt. 2012 Jan; 32(1):3-16. https://www.ncbi.nlm.nih.gov/pubmed/22150586/
- Myopia. Morgan IG, Ohno-Matsui K, Saw SM. Lancet. 2012 May 5; 379(9827):1739-48. https://www.ncbi.nlm.nih.gov/pubmed/22559900/
- Prevalence and causes of low vision and blindness in a rural chinese adult population: the Handan Eye Study. Liang YB, Friedman DS, Wong TY, Zhan SY, Sun LP, Wang JJ, Duan XR, Yang XH, Wang FH, Zhou Q, Wang NL, Handan Eye Study Group. Ophthalmology. 2008 Nov; 115(11):1965-72. https://www.ncbi.nlm.nih.gov/pubmed/18684506/
- Prevalence and causes of visual impairment in an elderly Chinese population in Taiwan: the Shihpai Eye Study. Hsu WM, Cheng CY, Liu JH, Tsai SY, Chou P. Ophthalmology. 2004 Jan; 111(1):62-9. https://www.ncbi.nlm.nih.gov/pubmed/14711715/
- Prevalence and causes of visual impairment and blindness among 9980 Scandinavian adults: the Copenhagen City Eye Study. Buch H, Vinding T, La Cour M, Appleyard M, Jensen GB, Nielsen NV. Ophthalmology. 2004 Jan; 111(1):53-61. https://www.ncbi.nlm.nih.gov/pubmed/14711714/
- On the merits of ancient Chinese eye acupressure practices. Ostberg O, Horie Y, Feng Y. Appl Ergon. 1992 Oct; 23(5):343-8. https://www.ncbi.nlm.nih.gov/pubmed/15676881/
- Refractive Error Study in Children: results from Shunyi District, China. Zhao J, Pan X, Sui R, Munoz SR, Sperduto RD, Ellwein LB. Am J Ophthalmol. 2000 Apr; 129(4):427-35. https://www.ncbi.nlm.nih.gov/pubmed/10764849/
- Prevalence of myopia in urban and rural children in mainland China. He M, Zheng Y, Xiang F. Optom Vis Sci. 2009 Jan; 86(1):40-4. https://www.ncbi.nlm.nih.gov/pubmed/19104465/
- Wei ML, Liu JP, Li N, Liu M. Acupuncture for slowing the progression of myopia in children and adolescents. Cochrane Database of Systematic Reviews 2011, Issue 9. Art. No.: CD007842. DOI: 10.1002/14651858.CD007842.pub2. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD007842.pub2/full
- [Myopia prevalence and influencing factor analysis of primary and middle school students in our country]. Xie HL, Xie ZK, Zhou F, Hu L. Zhonghua Yi Xue Za Zhi. 2013 Apr 2; 93(13):999-1002. https://www.ncbi.nlm.nih.gov/pubmed/23886264/
- Xiong R, Liu Q (2001) Survey on the nonstandard performance of Chinese eye exercises in children. Chin J School Health 22: 566.
- Zhao R, He X-G, Zhu J-f (2012) Beliefs and behavior related to Chinese students eye exercises among primary and secondary school teachers and students in Shanghai Chin J Sch Health 33: 270–272.
- Li S-M, Kang M-T, Peng X, et al. Efficacy of Chinese Eye Exercises on Reducing Accommodative Lag in School-Aged Children: A Randomized Controlled Trial. Pan C-W, ed. PLoS ONE. 2015;10(3):e0117552. doi:10.1371/journal.pone.0117552. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4350838/
- Chavasse F. 7th ed. Balliere Tindall & Cox; London: 1939. Worth’s Squint; p. 514.
- American Association for Pediatric Ophthalmology and Strabismus. Convergence Insufficiency. https://www.aapos.org/terms/conditions/38
- Convergence insufficiency. Daum KM. Am J Optom Physiol Opt. 1984 Jan; 61(1):16-22. https://www.ncbi.nlm.nih.gov/pubmed/6702996/
- Scheiman M, Gallaway M. The long-term effectiveness of vision therapy for the treatment of convergence insufficiency. Optom Vis Sci. 1997;74:S 167.
- Griffin J., Grisham J. Butterworth-Heinemann; Boston, MA: 2002. Binocular Anomalies: Diagnosis and Vision Therapy.
- Convergence insufficiency treatment study group The convergence insufficiency treatment trial: design, methods, and baseline data. Ophthalmic Epidemiol. 2008;15:24–36. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2782898/
- Convergence insufficiency treatment study group Randomized clinical trial of treatments for symptomatic convergence insufficiency in children. Arch Ophthalmol. 2008;126:1336–1349. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2779032/
- Fray K.J. Fusional amplitudes: exploring where fusion falters. Am Orthoptic J. 2013;63:41–54. https://www.ncbi.nlm.nih.gov/pubmed/24141750
- Convergence Insufficiency Treatment Trial Investigator Group. The Convergence Insufficiency Treatment Trial: Design, Methods, and Baseline Data. Ophthalmic epidemiology. 2008;15(1):24-36. doi:10.1080/09286580701772037. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2782898/
- Amblyopia. Holmes JM, Clarke MP. Lancet. 2006 Apr 22; 367(9519):1343-51. https://www.ncbi.nlm.nih.gov/pubmed/16631913/
- Electroretinograms and visual evoked potentials in long-term monocularly deprived cats. Baro JA, Lehmkuhle S, Kratz KE. Invest Ophthalmol Vis Sci. 1990 Jul; 31(7):1405-9. https://www.ncbi.nlm.nih.gov/pubmed/2365572/
- SINGLE-CELL RESPONSES IN STRIATE CORTEX OF KITTENS DEPRIVED OF VISION IN ONE EYE. WIESEL TN, HUBEL DH. J Neurophysiol. 1963 Nov; 26():1003-17. https://www.ncbi.nlm.nih.gov/pubmed/14084161/
- Understanding the neural basis of amblyopia. Barrett BT, Bradley A, McGraw PV. Neuroscientist. 2004 Apr; 10(2):106-17. https://www.ncbi.nlm.nih.gov/pubmed/15070485/
- Effects of early pattern deprivation on visual development. Lewis TL, Maurer D. Optom Vis Sci. 2009 Jun; 86(6):640-6. https://www.ncbi.nlm.nih.gov/pubmed/19417706/
- Sale A, Berardi N. Active training for amblyopia in adult rodents. Frontiers in Behavioral Neuroscience. 2015;9:281. doi:10.3389/fnbeh.2015.00281. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4621305/
- Baroncelli L., Sale A., Viegi A., Maya Vetencourt J. F., De Pasquale R., Baldini S., et al. . (2010). Experience-dependent reactivation of ocular dominance plasticity in the adult visual cortex. Exp. Neurol. 226, 100–109. 10.1016/j.expneurol.2010.08.009. https://www.ncbi.nlm.nih.gov/pubmed/20713044
- Maya Vetencourt J. F., Sale A., Viegi A., Baroncelli L., De Pasquale R., O’Leary O. F., et al. . (2008). The antidepressant fluoxetine restores plasticity in the adult visual cortex. Science 320, 385–388. 10.1126/science.1150516. https://www.ncbi.nlm.nih.gov/pubmed/18420937
- A cycling lane for brain rewiring. Lunghi C, Sale A. Curr Biol. 2015 Dec 7; 25(23):R1122-3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5040496/
- Karatz MA. William Horatio Bates, M.D., and the Bates method of eye exercises. N Y State J Med. 1975 Jun;75(7):1105-10. https://www.ncbi.nlm.nih.gov/pubmed/1095980
- Gardner, Martin (1957). “Chapter 19: Throw Away Your Glasses!”. Fads and Fallacies in the Name of Science. Courier Dover Publications. pp. 230–241. ISBN 0-486-20394-8.
- Skarnulis, Leanna (5 February 2007). “Natural Vision Correction: Does It Work ? http://www.webmd.com/eye-health/features/natural-vision-correction-does-it-work
- Mohan, Madan (1983). “Therapy of myopia”. Indian Journal of Ophthalmology. 31 (6): 741–3. https://www.ncbi.nlm.nih.gov/pubmed/6676257
- Ridgway AE. Solar retinopathy. British Medical Journal. 1967;3(5559):212-214. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1842517/pdf/brmedj02145-0032a.pdf
- The Johns Hopkins University, Hopkins Medicine. Michael Xavier Repka, M.D. http://www.hopkinsmedicine.org/profiles/results/directory/profile/0000767/michael-repka
- Pollack, Philip (1956). “Chapter 3: Fallacies of the Bates System”. The Truth about Eye Exercises. Philadelphia: Chilton Company. https://babel.hathitrust.org/cgi/pt?id=uc1.b4399673;view=1up;seq=7
- Chou, Brian (15 September 2004). “Exposing the Secrets of Fringe Eye Care”. Review of Optometry. 141 (9). https://www.reviewofoptometry.com/article/exposing-the-secrets-of-fringe-eye-care
- Marg, Elwin (April 1952). “Flashes of clear vision and negative accommodation with reference to the Bates Method of visual training”. American Journal of Optometry & Archives of American Academy of Optometry. 29 (4): 167–84. http://journals.lww.com/optvissci/Citation/1952/04000/_FLASHES__OF_CLEAR_VISION_AND_NEGATIVE.1.aspx
- “Complementary Therapy Assessments: Visual Training for Refractive Errors”. American Academy of Ophthalmology. August 2013. Retrieved 20 March 2014. https://www.aao.org/complimentary-therapy-assessment/visual-training-refractive-errors-cta–october-200
- Raz, A.; Marinoff, G. P.; Landzberg, K. S.; Guyton, D. L. (2004). “Substrates of negative accommodation”. Binocular Vision & Strabismus Quarterly. 19 (2): 71–74.
- Raz, A.; Marinoff, G. P.; Zephrani, Z. R.; Schweizer, H. R.; Posner, M. I. (2004). “See clearly: suggestion, hypnosis, attention, and visual acuity”. International Journal of Clinical and Experimental Hypnosis. 52 (2): 159–187. https://www.ncbi.nlm.nih.gov/pubmed/15115060
- Grierson, Ian (2000). “Exercises for Eyes as an Alternative to Glasses”. The Eye Book: Eyes and Eye Problems Explained. Liverpool University Press. pp. 58–60. https://books.google.com.au/books?id=YY0inTk-CEcC&pg=PA58&redir_esc=y#v=onepage&q&f=false
- Bates, William H. (1920). “Chapter 12: Palming”. Perfect Sight Without Glasses. New York: Central Fixation Publishing Co. pp. 123–135. ISBN 88-900756-3-5.
- Pollack, Philip (1956). “Chapter 3: Fallacies of the Bates System”. The Truth about Eye Exercises. Philadelphia: Chilton Company.
- Bates, William H. (June 1920). “Sun-gazing”. Better Eyesight. New York: Central Fixation Publishing Co.
- Bates, William H. (1920). “Chapter 17: Vision Under Adverse Conditions a Benefit to the Eyes”. Perfect Sight Without Glasses. New York: Central Fixation Publishing Co. pp. 183–197. ISBN 88-900756-3-5.
- Bates, William H. (July 1929). “The Use of the Sun Glass”. Better Eyesight. New York: Central Fixation Publishing Co.
- Bates, William H. (1920). “Chapter 15: Shifting and Swinging”. Perfect Sight Without Glasses. New York: Central Fixation Publishing Co. pp. 159–171. ISBN 88-900756-3-5.
- Leavitt, Frank J. (2007). “How to Save the World: Alternatives to Biomedical Research”. Ethics in Biomedical Research: International Perspectives. Rodopi. pp. 203–207.
- Bates, William H. (1920). “Chapter 13: Memory as an Aid to Vision”. Perfect Sight Without Glasses. New York: Central Fixation Publishing Co. pp. 136–147. ISBN 88-900756-3-5.
- Scheiman M, Cotter S, Rouse M et al. Randomised clinical trial of the effectiveness of base-in prism reading glasses versus placebo reading glasses for symptomatic convergence insufficiency in children. Br J Ophthalmol 2005; 89: 1318–1323. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1772876/
- Elliott DB. Evidence-based optometry and in-practice research. Ophthalmic Physiol Opt 2012; 32: 81–82. http://onlinelibrary.wiley.com/doi/10.1111/j.1475-1313.2012.00899.x/full
- Moerman DE. Meaning, Medicine and the ‘Placebo Effect’ (Cambridge Studies in Medical Anthropology). University Press: Cambridge, 2002.
- McMonnies CW. Chart memory and visual acuity measurement. Clin Exp Optom 2001; 84: 26–33. https://www.ncbi.nlm.nih.gov/pubmed/12366341
- McMonnies CW. Passive letter subset memory and reliability of visual acuity assessment. Invest Ophthalmol Vis Sci 2010; 51: 6907–6908. http://iovs.arvojournals.org/article.aspx?articleid=2128102
- Pesudovs K & Brennan NA. Decreased uncorrected vision after a period of distance fixation with spectacle wear. Optom Vis Sci 1993; 70: 528–531. https://www.ncbi.nlm.nih.gov/pubmed/8355963
- George S & Rosenfield M. Blur adaptation and myopia. Optom Vis Sci 2004; 81: 543–547. https://www.ncbi.nlm.nih.gov/pubmed/15252354
- Mon-Williams M, Tresilian JR, Strang NC, Kochhar P & Wann JP. Improving vision: neural compensation for optical defocus. Proc Biol Sci 1998; 265: 71–77. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1688761/
- Cufflin MP, Mankowska A & Mallen EA. Effect of blur adaptation on blur sensitivity and discrimination in emmetropes and myopes. Invest Ophthalmol Vis Sci 2007; 48: 2932–2939. https://www.ncbi.nlm.nih.gov/pubmed/17525230
- Vera-Diaz FA, Woods RL & Peli E. Shape and individual variability of the blur adaptation curve. Vision Res 2010; 50: 1452–1461. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2902630/
- Poulere E, Moschandreas J, Kontadakis GA, Pallikaris IG & Plainis S. Effect of blur and subsequent adaptation on visual acuity using letter and Landolt C charts: differences between emmetropes and myopes. Ophthalmic Physiol Opt 2013; 33: 130–137. https://www.ncbi.nlm.nih.gov/pubmed/23297779
- Giannakopoulou T, Plainis S, Pallikaris IG & Tsilimbaris MK. Contrast sensitivity in the ‘good eye’ of adult patients with severe impairment in the other eye. Ophthalmic Physiol Opt 2013; 33: 150–156. https://www.ncbi.nlm.nih.gov/pubmed/23347379
- Polat U, Schor C, Tong JL et al. Training the brain to overcome the effect of aging on the human eye. Sci Rep 2012; 2: 278. https://www.nature.com/articles/srep00278
- Levi DM & Li RW. Improving the performance of the amblyopic visual system. Philos Trans R Soc Lond B Biol Sci 2009; 364: 399–407. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2674474/
- Astle AT, Webb BS & McGraw PV. Can perceptual learning be used to treat amblyopia beyond the critical period of visual development? Ophthalmic Physiol Opt 2011; 31: 564–573. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3428831/
- Polat U, Schor C, Tong JL et al. Training the brain to overcome the effect of aging on the human eye. Sci Rep 2012; 2: 278. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3284862/