Floppy baby syndrome
Floppy baby syndrome also known as hypotonia, which means decreased muscle tone or a state of low muscle tone often involving reduced muscle strength. It is important to recognize that hypotonia is not equivalent to weakness. Hypotonia is not a specific medical disorder, but a potential manifestation of many different diseases and disorders that affect motor nerve control by the brain or muscle strength.
Floppy baby syndrome can be a condition on its own, called benign congenital hypotonia, or it can be indicative of another problem where there is progressive loss of muscle tone, such as muscular dystrophy or cerebral palsy. Hypotonia is usually detected during infancy.
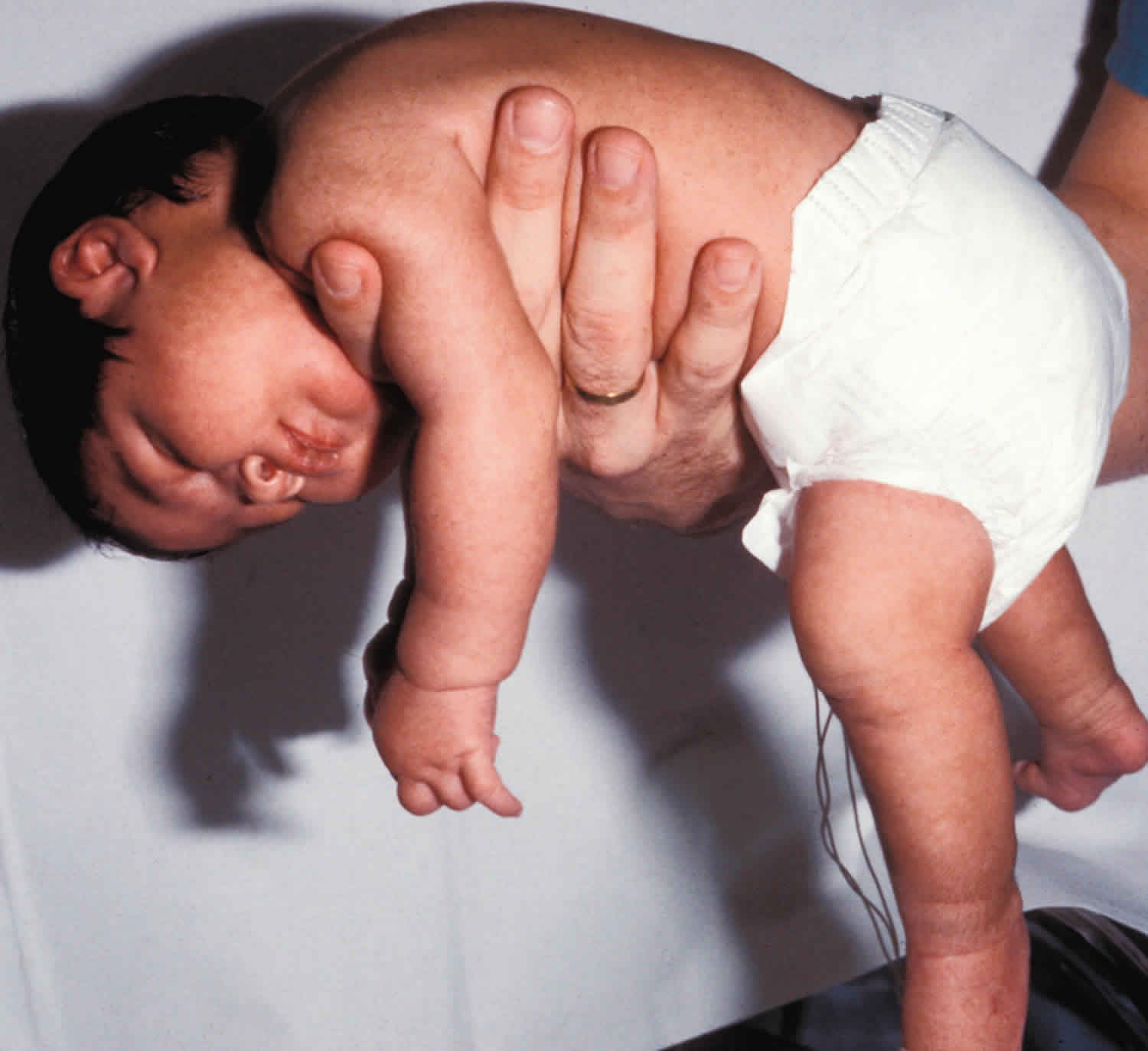
- An infant with hypotonia exhibits a floppy quality or “rag doll” feeling when he or she is held.
- Infants may lag behind in acquiring certain fine and gross motor developmental milestones that enable a baby to hold his or her head up when placed on the stomach, balance themselves or get into a sitting position and remain seated without falling over.
- There is a tendency for hip, jaw and neck dislocations to occur.
- Some children with hypotonia may have trouble feeding, if they are unable to suck or chew for long periods.
- A child with hypotonia may also have problems with speech or exhibit shallow breathing.
Hypotonia is a lack of resistance to passive movement, whereas muscle weakness results in impaired active movement. Central hypotonia originates from the central nervous system, while peripheral hypotonia is related to problems within the spinal cord, peripheral nerves and/or skeletal muscles 1. Recognizing hypotonia, even in early infancy, is usually relatively straightforward, but diagnosing the underlying cause can be difficult and often unsuccessful. The long-term effects of hypotonia on a child’s development and later life depend primarily on the severity of the muscle weakness and the nature of the cause. Some disorders have a specific treatment but the principal treatment for most hypotonia of idiopathic or neurologic cause is physical therapy, occupational therapy for remediation, and/or music therapy.
Hypotonia is thought to be associated with the disruption of afferent input from stretch receptors and/or lack of the cerebellum’s facilitatory efferent influence on the fusimotor system, the system that innervates intrafusal muscle fibers thereby controlling muscle spindle sensitivity 2. On examination a diminished resistance to passive movement will be noted and muscles may feel abnormally soft and limp on palpation 2. Diminished deep tendon reflexes also may be noted. Hypotonia is a condition that can be helped with early intervention.
Hypotonia causes
Hypotonia are usually of unknown origin. Hypotonia can be caused by a variety of conditions, scientists believe that hypotonia may be caused by a variety of conditions such trauma that involve the central nervous system, environmental factors, genetic disorders and muscle disorders 1. A retrospective, cross–sectional study was done in Iran to find out the main cause of hypotonia, they found that central hypotonia was the cause in (94.4%) and peripheral in (3.7%) 3. The most common cause of central hypotonia was idiopathic central hypotonia, followed by cerebral palsy, brain structural abnormality, inborn errors of metabolism , genetic disorders and syndrome 3.
Some common causes of hypotonia can include but are not limited to:
- Idiopathic central hypotonia (persistent hypotonia without other cause)
- Down syndrome
- Muscular dystrophy
- Cerebral palsy
- Prader-Willi syndrome
- Myotonic dystrophy
- Marfan syndrome
- Tay-Sachs disease
- Hypotonic cerebral palsy
- Intracranial hemorrhage
- Hypoxic ischemic encephalopathy (damage to cells in the central nervous system due to inadequate oxygen)
- Structural brain anomalies:
- Holoprosencephaly caused by the failure of the embryonic forebrain to divide into the double lobes of the cerebral hemispheres. The result is a single-lobed brain structure and severe skull and facial defects that may affect the eyes, nose, and upper lip.
- Peroxisomal disorders is a group of congenital diseases characterized by the absence of normal peroxisomes in the cells of the body. Peroxisomes are special organelles within a cell that contain enzymes responsible for critical cellular processes, including oxidation of fatty acids, biosynthesis of membrane phospholipidsandcholesterol. The patient usually has developmental delayand mental retardation. Hypotonia, which in the most severe cases is generalized. Facial abnormalities, including high forehead, frontal bossing (swelling), small face, and slanted eyes.
Congenital is disease a person is born with (including genetic disorders presenting within 6 months)
Genetic disorders are the most common cause:
- 22q13 deletion syndrome (Phelan–McDermid syndrome)
- 3-Methylcrotonyl-CoA carboxylase deficiency 4
- Achondroplasia
- Aicardi syndrome
- Autism spectrum disorders 5
- Canavan disease
- Centronuclear myopathy (including myotubular myopathy)
- Central core disease
- CHARGE syndrome
- Cohen syndrome
- Costello syndrome
- Dejerine–Sottas disease (HMSN Type III)
- Down syndrome (Trisomy 21) — most common
- Ehlers–Danlos syndrome
- Familial dysautonomia (Riley–Day syndrome)
- FG syndrome
- Fragile X syndrome
- Griscelli syndrome Type 1 (Elejalde syndrome)
- Disorder Growth Hormone Disorder Pituitary Dwarfism
- Holocarboxylase synthetase deficiency / Multiple carboxylase deficiency 6
- Krabbe disease
- Leigh’s disease
- Lesch–Nyhan syndrome 7
- Marfan’s syndrome
- Menkes syndrome
- Methylmalonic acidemia
- Myotonic dystrophy
- Niemann–Pick disease
- Nonketotic hyperglycinemia (NKH) or Glycine encephalopathy (GCE)
- Noonan syndrome
- Neurofibromatosis
- Patau syndrome (Trisomy 13)
- Prader–Willi syndrome, a very rare genetic disorder, in which seven genes on chromosome 15 are missing or unexpressed. They usually have slow mental development, small hands and feet as compared to the body, almond shaped eyes, and skeletal abnormalities, such as a narrow bifrontal skull. Symptoms also include floppy infants
- Rett syndrome
- Septo-optic dysplasia (de Morsier syndrome)
- Snyder–Robinson syndrome (SRS)
- Spinal muscular atrophy (SMA)
- Succinic semialdehyde dehydrogenase deficiency (SSADH)
- Tay–Sachs disease
- Werdnig–Hoffmann syndrome – Spinal muscular atrophy with congenital degeneration of anterior horns of spinal cord. Autosomal recessive.
- Wiedemann–Steiner syndrome
- Williams syndrome, a rare neurodevelopmental disorder caused by a deletion of about 26 genes from the long arm of chromosome 7. It is characterized by a distinctive, “elfin” facial appearance, along with a low nasal bridge; mental retardation and cardiovascular problems, such as supravalvular aortic stenosis.
- Zellweger syndrome (cerebrohepatorenal syndrome)
Developmental disability
- Cerebellar ataxia (congenital)
- Sensory processing disorder
- Developmental coordination disorder
- Hypothyroidism (congenital)
- Hypotonic cerebral palsy
- Teratogenesis from in utero exposure to Benzodiazepines
Acquired – onset occurs after birth
- Genetic
- Muscular dystrophy (including Myotonic dystrophy) – most common
- Metachromatic leukodystrophy
- Rett syndrome
- Spinal muscular atrophy
- Infections
- Encephalitis
- Guillain–Barré syndrome
- Infant botulism
- Meningitis
- Poliomyelitis
- Sepsis
- Toxins
- Infantile acrodynia (childhood mercury poisoning)
- Autoimmunity disorders
- Myasthenia gravis – most common
- Abnormal vaccine reaction
- Celiac disease 8
- Metabolic disorder
- Mitochondrial encephalomyopathies (chronic progressive disorders affecting neuromuscular system. Symptoms are induced by insufficient energy supply resulting from a deficiency of oxidative phosphorylation.
- Hypervitaminosis
- Kernicterus
- Rickets
- Neurological
- Traumatic brain injury, such as the damage that is caused by Shaken baby syndrome
- Lower motor neuron lesions
- Upper motor neuron lesions
- Miscellaneous
- Central nervous system dysfunction, including cerebellar lesions and cerebral palsy
- Hypothyroidism
- Sandifer syndrome
- Neonatal Benzodiazepine withdrawal syndrome in children born to mothers treated in late pregnancy with benzodiazepine medications[10]
Hypotonia signs and symptoms
The following are common symptoms associated with hypotonia. Each child may experiences symptoms differently. Symptoms vary depending on the underlying cause of the problem.
- Decreased muscle tone, muscles feel soft and doughy
- Ability to extend limb beyond its normal limit
- Weak ligaments and joints. Since the muscles that support the bone joints are soft, there is a tendency for hip, jaw, and neck dislocations.
- Failure to acquire motor related developmental milestones (such as holding head up without support from parent, rolling over, sitting up without support, walking)
- Problems with feeding (inability to suck or chew for prolonged periods). Hypotonic children also have trouble feeding and are unable to suck or chew for long periods.
- Shallow breathing or breathing difficulties
- Mouth hangs open with tongue protruding (under-active gag reflex)
Some hypotonias are not progressive and are of an unknown origin, a condition known as benign congenital hypotonia.
- Central nervous system function and intelligence in children is normal.
- Children with benign congenital hypotonia may not experience developmental delay.
- Some children acquire gross motor skills (sitting, walking, running, jumping) more slowly than most.
The signs and symptoms of hypotonia resemble that of other conditions. Always consult a physician for a diagnosis.
Hypotonia diagnosis
Your child’s doctor will obtain a medical history for your family and your child and will perform a physical examination that will likely include a detailed muscle function and neurological examination. The latter, also called a neuro exam, may be performed with instruments, such as lights and reflex hammers, and usually does not cause any pain to the child.
- assessment of motor and sensory skills
- balance and coordination
- mental status (the child’s level of awareness and interaction with the environment)
- reflexes
- functioning of the nerves
Diagnostic testing for hypotonia
Depending on what your child’s doctor suspects, the following tests may also be used to find out what’s causing your child’s muscle weakness:
- Magnetic Resonance Imaging (MRI) – A diagnostic procedure that uses a combination of large magnets, radio frequencies and a computer to produce detailed images of organs and structures within the body. This test is done to rule out any associated abnormalities of the spinal cord and nerves
- Computerized Tomography Scan (also called a CT or CAT scan) – A diagnostic imaging procedure that uses a combination of X-rays and computer technology to produce cross-sectional images (often called “slices”), both horizontally and vertically, of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat and organs. CT scans are more detailed than general X-rays
- Blood tests
- EMG (electromyogram) – a test used to evaluate nerve and muscle function
- EEG (electroencephalogram) – a test that measures the electrical activity in the brain, called brain waves. An EEG measures brain waves through small button electrodes that are placed on your child’s scalp
- Spinal tap also called lumbar puncture, a spinal tap is done to measure the amount of pressure in the spinal canal and/or to remove a small amount of cerebral spinal fluid (CSF) for testing. Cerebral spinal fluid is the fluid that bathes your child’s brain and spinal cord
- Karyotype – This test, a chromosomal analysis from a blood test, is used to determine whether the problem is the result of a genetic disorder
- Muscle biopsy: a sample of muscle tissue is removed and examined under a microscope.
- Creatine kinase (CK) test: elevated CK level in blood indicating muscles are damaged or degenerating
Hypotonia treatment
Specific treatment for hypotonia will be determined by your child’s physician based on:
- your child’s age, overall health, and medical history
- the extent of the condition
- the underlying cause of the condition
- your child’s tolerance for specific medications, procedures, or therapies
- expectations for the course of the condition
- your opinion or preference.
Once the correct diagnosis is confirmed, the cause is treated first, followed by symptomatic and supportive therapy for the hypotonia.
- Physical therapy can improve fine motor control and overall body strength.
- Occupational and speech-language therapy can help breathing, speech, and swallowing difficulties.
- Therapy for infants and young children may also include sensory stimulation programs.
No specific therapy is required to treat benign congenital hypotonia, but children with this problem may periodically need treatment for common occurrences associated with hypotonia, such as recurrent joint dislocations.
If the underlying cause is known, treatment is tailored to the specific disease, followed by symptomatic and supportive therapy for the hypotonia. In very severe cases, treatment may be primarily supportive, such as mechanical assistance with basic life functions like breathing and feeding, physical therapy to prevent muscle atrophy and maintain joint mobility, and measures to try to prevent opportunistic infections such as pneumonia. Treatments to improve neurological status might involve such things as medication for a seizure disorder, medicines or supplements to stabilize a metabolic disorder, or surgery to help relieve the pressure from hydrocephalus (increased fluid in the brain).
Treatment programs to help increase muscle strength and sensory stimulation programs are developed once the cause of your child’s hypotonia is established. Such programs usually involve physical therapy through an early intervention or school-based program among other forms of therapy.
The National Institute of Neurological Disorders and Stroke states that physical therapy can improve motor control and overall body strength in individuals with hypotonia. This is crucial to maintaining both static and dynamic postural stability, which is important since postural instability is a common problem in people with hypotonia 2. A physiotherapist can develop patient specific training programs to optimize postural control, in order to increase balance and safety 2. To protect against postural asymmetries the use of supportive and protective devices may be necessary 2. Physical therapists might use neuromuscular/sensory stimulation techniques such as quick stretch, resistance, joint approximation, and tapping to increase tone by facilitating or enhancing muscle contraction in patients with hypotonia.[3] For patients who demonstrate muscle weakness in addition to hypotonia strengthening exercises that do not overload the muscles are indicated 2. Electrical Muscle Stimulation, also known as Neuromuscular Electrical Stimulation (NMES) can also be used to “activate hypotonic muscles, improve strength, and generate movement in paralyzed limbs while preventing disuse atrophy” 2. When using NMES it is important to have the patient focus on attempting to contract the muscle(s) being stimulated. Without such concentration on movement attempts, carryover to volitional movement is not feasible 2. Neuromuscular Electrical Stimulation (NMES) should ideally be combined with functional training activities to improve outcomes.
Occupational therapy can assist the patient with increasing independence with daily tasks through improvement of motor skills, strength, and functional endurance. Speech-language therapy can help with any breathing, speech, and/or swallowing difficulties the patient may be having. Therapy for infants and young children may also include sensory stimulation programs.” A physical therapist may recommend an ankle/foot orthosis to help the patient compensate for weak lower leg muscles. Toddlers and children with speech difficulties may benefit greatly by using sign language.
Hypotonia prognosis
Central hypotonia due to static usually improves with time. The prognosis is worst for hypotonia of progressive central disorders.
Children with mild hypotonia may not experience developmental delay, although some children acquire gross motor skills (sitting, walking, running, jumping) more slowly than most. Most hypotonic children eventually improve with therapy and time. Some children are more severely affected, requiring walkers and wheelchairs and other adaptive and assistive equipment.
References- Central Hypotonia. Sarah Bagher(2009). https://www.kau.edu.sa/Files/165003/Files/48267_Central%20hypotonia.pdf
- O’Sullivan S. B. (2007). Strategies to Improve Motor Function. In S. B. O’Sullivan, & T. J. Schmitz (Eds.), Physical Rehabilitation (5th Ed.) Philadelphia: F.A. Davis Company.
- Amirsalari S, Kavehmanesh Z, Khalili Matinzadeh Z, Afsharpayman S, Torkaman M, Javadipour M, et al. Hypotonia in infants and young children: An etiological analysis. Pak J Med Sci 2008; 24(5):744-47.
- 3-methylcrotonyl-CoA carboxylase deficiency. https://ghr.nlm.nih.gov/condition/3-methylcrotonyl-coa-carboxylase-deficiency
- Xue Ming, et al. Prevalence of motor impairment in autism spectrum disorders. Brain and Development. Volume 29, Issue 9, October 2007, Pages 565–570.
- Holocarboxylase Synthetase Deficiency / Multiple Carboxylase Deficiency. https://www.genedx.com/test-catalog/disorders/holocarboxylase-synthetase-deficiency-multiple-carboxylase-deficiency
- Kliegman, Robert. Nelson Textbook of Pediatrics (20 ed.). p. 747. ISBN 978-1455775668
- Zelnik N, Pacht A, Obeid R, Lerner A (June 2004). “Range of neurologic disorders in patients with celiac disease”. Pediatrics. 113 (6): 1672–6. CiteSeerX 10.1.1.545.9692. doi:10.1542/peds.113.6.1672