What is galantamine
Galantamine or galantamine hydrobromide is used to treat the symptoms of Alzheimer’s disease (a brain disease that slowly destroys the memory and the ability to think, learn, communicate and handle daily activities). Although the etiology of cognitive impairment in Alzheimer’s disease is not fully understood, it has been reported that acetylcholine-producing neurons degenerate in the brains of patients with Alzheimer’s disease. The degree of this cholinergic loss has been correlated with degree of cognitive impairment and density of amyloid plaques (a neuropathological hallmark of Alzheimer’s disease). Galantamine is in a class of medications called a reversible and competitive acetylcholinesterase inhibitor 1. While the precise mechanism of galantamine’s action is unknown, it is postulated to exert its therapeutic effect by enhancing cholinergic function. This is accomplished by increasing the concentration of acetylcholine (ACh) in the brain that is needed for memory and thought, through reversible inhibition of its hydrolysis by cholinesterase. If this mechanism is correct, galantamine’s effect may lessen as the disease process advances and fewer cholinergic neurons remain functionally intact. There is no evidence that galantamine alters the course of the underlying dementing process. Galantamine may improve the ability to think and remember or slow the loss of these abilities in people who have Alzheimer’s disease. However, galantamine will not cure Alzheimer’s disease or prevent the loss of mental abilities at some time in the future.
Galantamine comes as a tablet, an extended-release (long-acting) capsule, and a solution (liquid) to take by mouth. The tablets and liquid are usually taken twice a day, preferably with the morning and evening meals. The extended-release capsules are usually taken once a day in the morning. Take galantamine at around the same time(s) every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take galantamine exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor. You are less likely to experience side effects of galantamine if you follow the exact dosing schedule prescribed by your doctor.
Galantamine is well absorbed with absolute oral bioavailability of about 90%. It has a terminal elimination half-life of about 7 hours and pharmacokinetics are linear over the range of 8-32 mg /day. The maximum inhibition of acetylcholinesterase activity of about 40% was achieved about one hour after a single oral dose of 8 mg galantamine in healthy male subjects.
Galantamine may upset your stomach, especially at the beginning of your treatment. Take galantamine with food and drink 6 to 8 glasses of water every day. This may decrease the chance that you will have an upset stomach during your treatment.
Your doctor will probably start you on a low dose of galantamine and gradually increase your dose, not more often than once every 4 weeks.
Continue to take galantamine even if you feel well. Do not stop taking galantamine without talking to your doctor. If you do stop taking galantamine for a few days or longer, call your doctor before you start to take galantamine again. Your doctor will probably tell you to start with the lowest dose of galantamine and gradually increase your dose to the dose you had been taking.
Before taking galantamine
- tell your doctor and pharmacist if you are allergic to galantamine, any other medications, or any of the inactive ingredients in galantamine tablets, solution, or extended-release capsules. Ask your pharmacist for a list of the inactive ingredients.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention any of the following: ambenonium chloride (Mytelase); amitriptyline (Elavil); anticholinergic medications such as atropine (Atropen, Sal-Tropine), belladonna (in Donnatal, Bellamine, Bel-Tabs, others); benztropine (Cogentin), biperiden (Akineton); clidinium (in Librax), dicyclomine (Bentyl), glycopyrrolate (Robinul), hyoscyamine (Cytospaz-M, Levbid, Levsin), ipratropium (Atrovent, in Combivent), oxybutynin (Ditropan), procyclidine (Kemadrin), propantheline (Pro-Banthine), scopolamine (Scopace, Transderm-Scop), tiotropium (Spiriva), tolterodine (Detrol), and trihexyphenidyl; certain antifungals such as fluconazole (Diflucan), itraconazole (Sporanox), ketoconazole (Nizoral), and voriconazole (Vfend); aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil, Motrin) and naproxen (Aleve, Naprosyn); bethanechol (Urecholine);cevimeline (Evoxac); cimetidine (Tagamet); clarithromycin (Biaxin, in Prevpac); digoxin (Lanoxin); fluoxetine (Prozac, Sarafem); fluvoxamine (Luvox); heart medications; nefazodone; neostigmine (Prostigmin);other medications for Alzheimer’s disease; medications for human immunodeficiency virus (HIV) or acquired immunodeficiency syndrome (AIDS); medications for high blood pressure; paroxetine (Paxil); pyridostigmine (Mestinon); and quinidine (Quinidex). Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you have or have ever had asthma or any other lung disease; an enlarged prostate; ulcers; seizures; irregular heartbeat; or heart, kidney, or liver disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breast-feeding. If you become pregnant while taking galantamine, call your doctor.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking galantamine.
- you should know that galantamine may make you drowsy. Do not drive a car or operate machinery until you know how this medication affects you.
- remember that alcohol can add to the drowsiness caused by galantamine.
Galantamine mechanism of action
Although the etiology of cognitive impairment in Alzheimer’s disease is not fully understood, it has been reported that acetylcholine-producing neurons degenerate in the brains of patients with Alzheimer’s disease. The degree of this cholinergic loss has been correlated with degree of cognitive impairment and density of amyloid plaques (a neuropathological hallmark of Alzheimer’s disease).
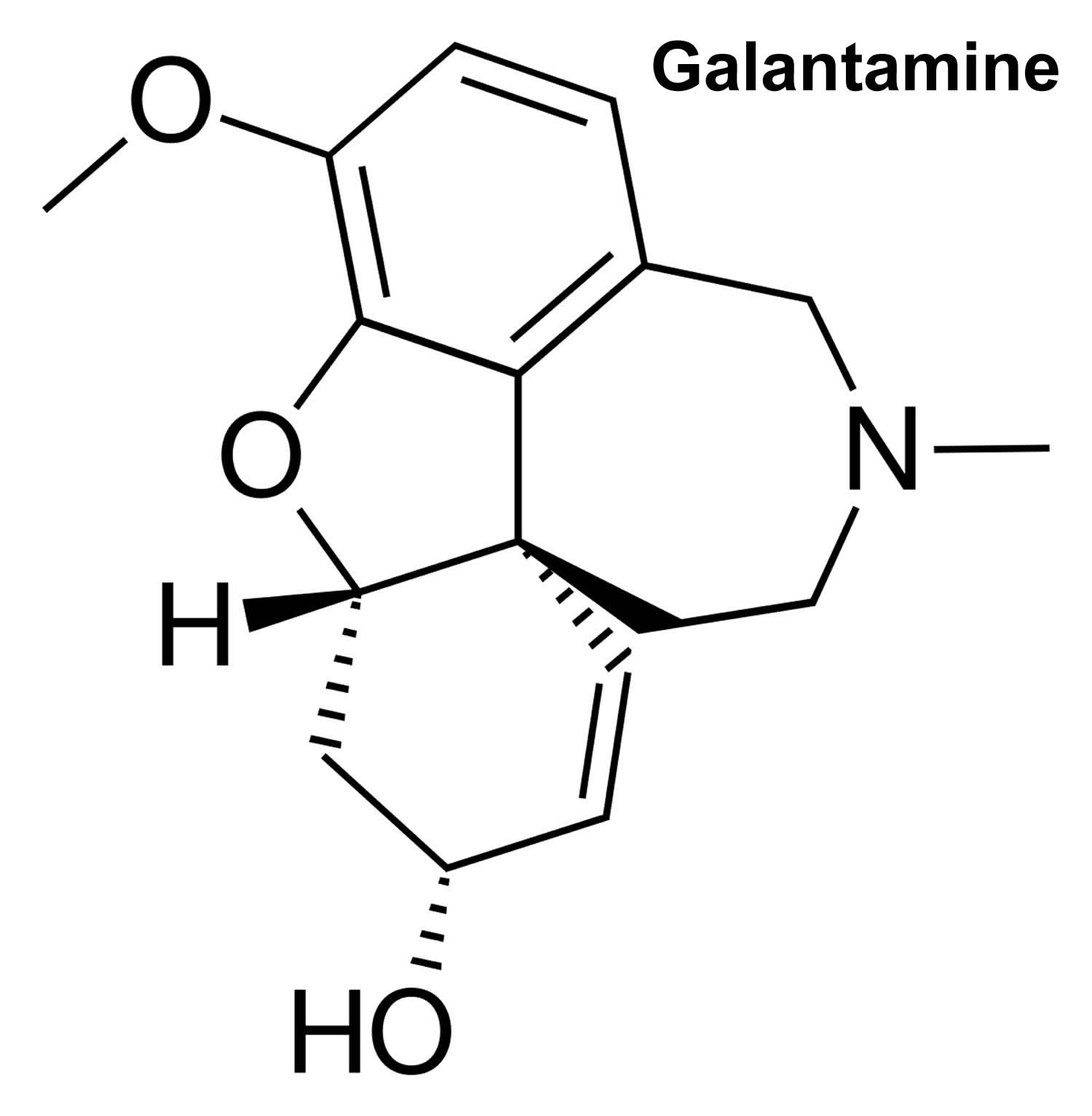
Galantamine, a tertiary alkaloid, is a competitive and reversible inhibitor of acetylcholinesterase. While the precise mechanism of galantamine’s action is unknown, it is postulated to exert its therapeutic effect by enhancing cholinergic function. This is accomplished by increasing the concentration of acetylcholine through reversible inhibition of its hydrolysis by cholinesterase. If this mechanism is correct, galantamine’s effect may lessen as the disease process advances and fewer cholinergic neurons remain functionally intact. There is no evidence that galantamine alters the course of the underlying dementing process.
All of the prescription medications currently approved to treat Alzheimer’s symptoms in early to moderate stages are from a class of drugs called cholinesterase inhibitors (also called inhibitor of acetylcholinesterase). Cholinesterase inhibitors are prescribed to treat symptoms related to memory, thinking, language, judgment and other thought processes.
Additionally, cholinesterase inhibitors:
- Prevent the breakdown of acetylcholine, a chemical messenger important for learning and memory. This supports communication among nerve cells by keeping acetylcholine high.
- Delay or slow worsening of symptoms. Effectiveness varies from person to person.
- Are generally well-tolerated. If side effects occur, they commonly include nausea, vomiting, loss of appetite and increased frequency of bowel movements.
Three cholinesterase inhibitors are commonly prescribed:
- Donepezil (Aricept) is approved to treat all stages of Alzheimer’s.
- Rivastigmate (Exelon) is approved to treat mild to moderate Alzheimer’s.
- Galantamine (Razadyne) is approved to treat mild to moderate Alzheimer’s.
Table 1. Cholinesterase inhibitors for early to moderate stages of Alzheimer’s disease
| Generic | Brand | Approved For | Side Effects |
|---|---|---|---|
| Donepezil | Aricept | All stages | Nausea, vomiting, loss of appetite and increased frequency of bowel movements. |
| Galantamine | Razadyne | Mild to moderate | Nausea, vomiting, loss of appetite and increased frequency of bowel movements. |
| Memantine | Namenda | Moderate to severe | Headache, constipation, confusion and dizziness. |
| Rivastigmine | Exelon | Mild to moderate | Nausea, vomiting, loss of appetite and increased frequency of bowel movements. |
| Memantine + Donepezil | Namzaric | Moderate to severe | Nausea, vomiting, loss of appetite, increased frequency of bowel movements, headache, constipation, confusion and dizzine |
What is galantamine used for
Galantamine is used to treat mild to moderate Alzheimer’s type dementia. Galantamine improves the function of nerve cells in the brain. It works by preventing the breakdown of a chemical called acetylcholine (ACh). People with dementia usually have lower levels of acetylcholine (ACh), which is important for the processes of memory, thinking, and reasoning.
Before taking galantamine
You should not use galantamine if you are allergic to it.
To make sure galantamine is safe for you, tell your doctor if you have:
- urination problems;
- heart disease or a heart rhythm disorder;
- a history of stomach ulcer or bleeding;
- seizures or epilepsy;
- kidney disease;
- liver disease; or
- a history of asthma or chronic obstructive pulmonary disease (COPD).
It is not known whether galantamine will harm an unborn baby. Tell your doctor if you are pregnant or plan to become pregnant.
It is not known whether galantamine passes into breast milk or if it could affect the nursing baby. Tell your doctor if you are breast-feeding.
Galantamine medication
The galantamine extended-release capsule is usually taken once per day in the morning. Follow your doctor’s instructions.
Brand names
- Razadyne® (formerly available as Reminyl®)
- Razadyne® ER (extended-release)
The galantamine short-acting tablet or the oral solution (liquid) are usually given two times per day, with meals. Follow your doctor’s instructions.
The extended-release capsule works best if you take it with food.
Do not crush, chew, break, or open an extended-release capsule. Swallow it whole.
Measure liquid medicine with the dosing syringe provided, or with a special dose-measuring spoon or medicine cup. If you do not have a dose-measuring device, ask your pharmacist for one.
Read all patient information, medication guides, and instruction sheets provided to you. Ask your doctor or pharmacist if you have any questions.
Take galantamine with a full glass of water. Drink 6 to 8 full glasses of water each day to keep from getting dehydrated while taking this medication.
If you need surgery, tell the surgeon ahead of time that you are using galantamine. You may need to stop using the medicine for a short time.
If you have stopped taking galantamine for any reason, talk with your doctor before you start taking it again. You may need to restart the medication at a lower dose.
Store at room temperature away from moisture and heat. Do not allow the liquid medicine to freeze.
Before you take galantamine oral solution for the first time, read the written instructions that come with it. Ask your doctor or pharmacist to show you how to take the oral solution. To take the oral solution, follow these steps:
- Open the child-proof cap by pushing the cap down while turning it to the left. Remove the cap.
- Pull the pipette (the tube that you use to measure the dose of galantamine) out of its case.
- Place the pipette fully into the bottle of galantamine.
- While holding the bottom ring of the pipette, pull the pipette plunger up to the marking that shows the dose your doctor prescribed.
- Hold the bottom ring of the pipette and remove the pipette from the bottle. Be careful not to push the plunger in.
- Prepare 3 to 4 ounces (about 1/2 cup [90 to 120 milliliters]) of any non-alcoholic beverage. Empty all the medicine from the pipette into the beverage by pushing the plunger all the way in.
- Stir the beverage well.
- Drink all of the mixture right away.
- Put the plastic cap back on the bottle of galantamine and turn the cap to the right to close the bottle.
- Rinse the empty pipette by putting its open end into a glass of water, pulling the plunger out, and pushing the plunger in to remove the water.
What other drugs will affect galantamine?
Tell your doctor about all your current medicines and any you start or stop using, especially:
- atropine;
- cold or allergy medicine that contains an antihistamine (Benadryl and others);
- medicine to treat Parkinson’s disease;
- medicine to treat excess stomach acid, stomach ulcer, motion sickness, or irritable bowel syndrome;
- bladder or urinary medicines–darifenacin, fesoterodine, oxybutynin, tolterodine, solifenacin;
- bronchodilators–aclidinium, ipratropium, or tiotropium;
This list is not complete. Other drugs may interact with galantamine, including prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible interactions are listed in this medication guide.
Galantamine dosage
The dosage of galantamine tablets shown to be effective in controlled clinical trials is 16 to 32 mg/day given as twice daily dosing. As the dosage of 32 mg/day is less well tolerated than lower dosages and does not provide increased effectiveness, the recommended dosage range is 16 to 24 mg/day given twice daily. The dosage of 24 mg/day did not provide a statistically significant greater clinical benefit than 16 mg/day. It is possible, however, that a daily dosage of 24 mg of galantamine might provide additional benefit for some patients.
The recommended starting dosage of galantamine tablets is 4 mg twice a day (8 mg/day). The dosage should be increased to the initial maintenance dosage of 8 mg twice a day (16 mg/day) after a minimum of 4 weeks. A further increase to 12 mg twice a day (24 mg/day) should be attempted after a minimum of 4 weeks at 8 mg twice a day (16 mg/day).
Dosage increases should be based upon assessment of clinical benefit and tolerability of the previous dose.
Galantamine tablets should be administered twice a day, preferably with morning and evening meals.
Patients and caregivers should be advised to ensure adequate fluid intake during treatment. If therapy has been interrupted for more than three days, the patient should be restarted at the lowest dosage and the dosage escalated to the current dose.
The abrupt withdrawal of galantamine in those patients who had been receiving dosages in the effective range was not associated with an increased frequency of adverse events in comparison with those continuing to receive the same dosages of that drug. The beneficial effects of galantamine are lost, however, when the drug is discontinued.
Adult Dose for Alzheimer’s Disease
- Immediate release tablet and oral solution:
- Initial dose: 4 mg orally twice a day, preferably with morning and evening meals.
- Maintenance dose: After a minimum of four weeks of treatment, if the initial dosage is well tolerated, it should be increased to 8 mg twice a day. A further increase to 12 mg twice a day should be attempted only after a minimum of 4 weeks at the previous dosage.
- Maximum dose: 16 to 24 mg/day
- Extended release capsule:
- Initial dose: 8 mg orally daily, preferably with the morning meal.
- Maintenance dose: After a minimum of four weeks of treatment, if the initial dosage is well tolerated, it should be increased to 16 mg once a day. A further increase to 24 mg once a day should be attempted only after a minimum of 4 weeks at the previous dosage.
- Maximum dose: 16 to 24 mg/day
Comment:
- Dose increases should be based upon assessment of clinical benefit and tolerability of the previous dose.
- If therapy has been interrupted for more than 3 days, the patient should be restarted at the lowest dosage and the dosage escalated to the current dose.
- Abrupt withdrawal of galantamine was not associated with increased frequency of adverse events
- The beneficial effects of galantamine are lost when the drug is discontinued
Renal dose adjustments
- Moderate renal impairment: The dose should generally not exceed 16 mg/day.
- Severe renal impairment (creatinine clearance less than 9 mL/min): The use of galantamine is not recommended.
Liver dose adjustments
- Moderately Impaired Hepatic Function (Child-Pugh score of 7 to 9): The dose should generally not exceed 16 mg/day.
- Severe Hepatic Impairment (Child-Pugh score of 10 to 15): The use of galantamine is not recommended.
What should I do if I forget a dose?
Take the missed dose as soon as you remember it. However, if it is almost time for the next dose, skip the missed dose and continue your regular dosing schedule. Do not take a double dose to make up for a missed one.
Galantamine side effects
Commonly reported side effects of galantamine include: nausea and vomiting. Other side effects include: dizziness, dyspepsia, fatigue, headache, weight loss, diarrhea, and anorexia. See below for a comprehensive list of side effects.
Galantamine may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- nausea
- vomiting
- diarrhea
- loss of appetite
- stomach pain
- heartburn
- weight loss
- extreme tiredness
- dizziness
- pale skin
- headache
- shaking of a part of your body that you cannot control
- depression
- difficulty falling asleep or staying asleep
- runny nose
Some side effects can be serious. The following symptoms are uncommon, but if you experience any of them, call your doctor immediately:
- difficulty urinating
- blood in the urine
- pain or burning while urinating
- seizures
- slowed heartbeat
- chest pain
- fainting
- shortness of breath
- black and tarry stools
- red blood in the stools
- bloody vomit
- vomit that looks like coffee grounds
- signs of stomach bleeding–bloody or tarry stools, coughing up blood or vomit that looks like coffee grounds
- liver problems–nausea, upper stomach pain, itching, tired feeling, loss of appetite, dark urine, clay-colored stools, jaundice (yellowing of the skin or eyes)
- dehydration symptoms–feeling very thirsty or hot, being unable to urinate, heavy sweating, or hot and dry skin
- a light-headed feeling, like you might pass out
- severe skin reaction–fever, sore throat, swelling in your face or tongue, burning in your eyes, skin pain, followed by a red or purple skin rash that spreads (especially in the face or upper body) and causes blistering and peeling.
Galantamine may cause other side effects. Call your doctor if you have any unusual problems while taking this medication.
Cardiovascular
- Common (1% to 10%): Syncope, bradycardia
- Frequency not reported: First degree atrioventricular (AV) block, palpitations, sinus bradycardia, supraventricular extrasystoles, flushing, hypotension
- Postmarketing reports: Complete AV block, hypertension
Two randomized, placebo controlled trials revealed increased deaths in galantamine-treated patients with mild cognitive impairment. A total of 13 deaths occurred among galantamine-treated patients (n=1026) and 1 patient on placebo (n=1022). The deaths were due to various causes; about half of the galantamine deaths appeared to result from various vascular causes (myocardial infarction, stroke, and sudden death).
Dermatologic
- Frequency not reported: Hyperhidrosis
- Postmarketing reports: Stevens-Johnson syndrome, Acute generalized exanthematous pustulosis, Erythema multiforme
Gastrointestinal
The median duration of nausea in clinical trials was 5 to 7 days. The most commonly occurring adverse reactions associated with discontinuation have include nausea (6.2%), vomiting (3.3%), decreased appetite (1.5%), and dizziness (1.3%).
- Very common (10% or more): Nausea, vomiting
- Common (1% to 10%): Diarrhea, abdominal pain, upper abdominal pain, dyspepsia, stomach discomfort, abdominal discomfort
- Uncommon (0.1% to 1%): Retching
- Postmarketing reports: Upper and lower GI bleeding, stomach discomfort, and abdominal discomfort.
General
The most common side effects associated with discontinuation were nausea, vomiting, decreased appetite, dizziness, diarrhea, headache, and decreased appetite.
Genitourinary
- Common (1% to 10%): Urinary tract infection, hematuria
- Frequency not reported: Increased libido
Hematologic
- Common (1% to 10%): Anemia
Hepatic
- Postmarketing reports: Hepatitis, increased hepatic enzymes
Hypersensitivity
- Postmarketing reports: Hypersensitivity
Metabolic
- Common (1% to 10%): Decreased appetite, decreased weight, anorexia
- Uncommon (0.1% to 1%): Dehydration
Musculoskeletal
- Common (1% to 10%): Muscle spasms
- Uncommon (0.1% to 1%): Muscular weakness
Nervous system
- Common (1% to 10%): Headache, dizziness, tremor, somnolence, lethargy
- Frequency not reported: Dysgeusia, hypersomnia, paresthesia
- Postmarketing reports: Seizures
Ocular
- Uncommon (0.1% to 1%): Blurred vision
Other
- Common (1% to 10%): Fatigue, asthenia, malaise
- Uncommon (0.1% to 1%): Fall
- Postmarketing reports: Tinnitus
Psychiatric
- Common (1% to 10%): Depression
- Frequency not reported: Apathy, paranoia (disagreeable or terrifying dreams), paranoid reaction, increased libido, delirium, suicidal ideation and suicide
- Postmarketing reports: Hallucination, visual hallucination, auditory hallucination
Respiratory
- Common (1% to 10%): Rhinitis
Symptoms of galantamine overdose may include:
- muscle weakness or twitching
- nausea
- vomiting
- stomach cramps
- drooling
- teary eyes
- increased urination
- need to have a bowel movement
- sweating
- slowed, fast, or irregular heartbeat
- lightheadedness
- dizziness
- fainting
- slowed breathing
- collapse
- loss of consciousness
- seizures
- dry mouth
- chest pain
- hallucinations (seeing things or hearing voices that do not exist).
As in any case of overdose, general supportive measures should be utilized. Signs and symptoms of significant overdosing of Galantamine are predicted to be similar to those of overdosing of other cholinomimetics. These effects generally involve the central nervous system, the parasympathetic nervous system, and the neuromuscular junction. In addition to muscle weakness or fasciculations, some or all of the following signs of cholinergic crisis may develop: severe nausea, vomiting, gastrointestinal cramping, salivation, lacrimation, urination, defecation, sweating, bradycardia, hypotension, respiratory depression, collapse and convulsions. Increasing muscle weakness is a possibility and may result in death if respiratory muscles are involved.
Tertiary anticholinergics such as atropine may be used as an antidote for Galantamine hydrobromide overdosage. Intravenous atropine sulfate titrated to effect is recommended at an initial dose of 0.5 to 1 mg i.v. with subsequent doses based upon clinical response. Atypical responses in blood pressure and heart rate have been reported with other cholinomimetics when coadministered with quaternary anticholinergics. It is not known whether Galantamine and/or its metabolites can be removed by dialysis (hemodialysis, peritoneal dialysis, or hemofiltration). Dose-related signs of toxicity in animals included hypoactivity, tremors, clonic convulsions, salivation, lacrimation, chromodacryorrhea, mucoid feces, and dyspnea.
In one postmarketing report, one patient who had been taking 4 mg of Galantamine daily for a week inadvertently ingested eight 4 mg tablets (32 mg total) on a single day. Subsequently, she developed bradycardia, QT prolongation, ventricular tachycardia and torsades de pointes accompanied by a brief loss of consciousness for which she required hospital treatment. Two additional cases of accidental ingestion of 32 mg (nausea, vomiting, and dry mouth; nausea, vomiting, and substernal chest pain) and one of 40 mg (vomiting), resulted in brief hospitalizations for observation with full recovery. One patient, who was prescribed 24 mg/day and had a history of hallucinations over the previous two years, mistakenly received 24 mg twice daily for 34 days and developed hallucinations requiring hospitalization. Another patient, who was prescribed 16 mg/day of oral solution, inadvertently ingested 160 mg (40 mL) and experienced sweating, vomiting, bradycardia, and near-syncope one hour later, which necessitated hospital treatment. His symptoms resolved within 24 hours.
References