What is giant papillary conjunctivitis
Giant papillary conjunctivitis also called contact lens–induced papillary conjunctivitis, is a type of allergic and irritant conjunctivitis that occurs secondary to direct mechanical irritation/injury and subsequent immune response (a combination of delayed type (type IV) and immediate (type I) hypersensitivity) 1. The foreign object may become coated with different allergens or injury epithelial tissue and allow deeper exposure to allergens and provoke an immunological response 2. In giant papillary conjunctivitis, large bumps appear on the underside of the eyelid. Giant papillary conjunctivitis is associated with the use of all types of contact lenses. However, giant papillary conjunctivitis is seen most commonly in teens and young adults, most likely because of soft contact lens use and is present in approximately 5% of that population 1. Giant papillary conjunctivitis can happen at any time, even after wearing contact lenses for many years. Giant papillary conjunctivitis average onset is one to two years after starting contact lens but varies widely with other ocular foreign bodies 3. Since the advent of disposable contact lenses, the frequency of giant papillary conjunctivitis is low 4. It appears that protein build-up on the surface of contact lenses and irregular edges were the main reason for the close association between contact lenses and giant papillary conjunctivitis 5, by immune or mechanical mechanisms: in particular protein deposits on the surface of the contact lens could become antigenic and stimulate the production of IgE; mechanical trauma and chronic irritation can determine the release of some mediators (CXCL8 and TNF-α) from injured conjunctival epithelial cells 6.
In the United States, the prevalence of giant papillary conjunctivitis is highest among wearers of hydrogel contact lenses—approximately 20%. Rigid gas-permeable contact lens wearers constitute approximately 5% of all cases. One study found that 85% of 221 patients with giant papillary conjunctivitis had been wearing hydrogel lenses, whereas only 15% used rigid lenses 7. With an increased frequency of contact lens replacement from more than four weeks to less than four weeks, the incidence of giant papillary conjunctivitis has dropped from 36% to 4.5% 8. This rate should drop even lower with the greater availability and popularity of one-day disposable contact lenses.
The international prevalence of giant papillary conjunctivitis is similar to that in the United States. Both sexes develop giant papillary conjunctivitis.
Giant papillary conjunctivitis can be more aggressive in children who wear contact lenses 9.
People who do not wear contact lenses can also get giant papillary conjunctivitis. But this is rare, mostly affecting those who have an artificial eye or stitches. Prior to the widespread use of contact lens, giant papillary conjunctivitis was predominantly seen in patients with immunoglobulin E (IgE) mediated ocular allergies including allergic conjunctivitis and vernal keratoconjunctivitis 10. It has also been found in patients with exposed sutures, filtering blebs, scleral buckles, ocular prostheses, corneal foreign bodies, limbal dermoids and tissue adhesives used on the ocular surface 11.
In long-standing, untreated disease, the bumps (papillae) will develop white fibrotic centers. In severe cases, patients will have lid swelling and ptosis (droopy eyelid).
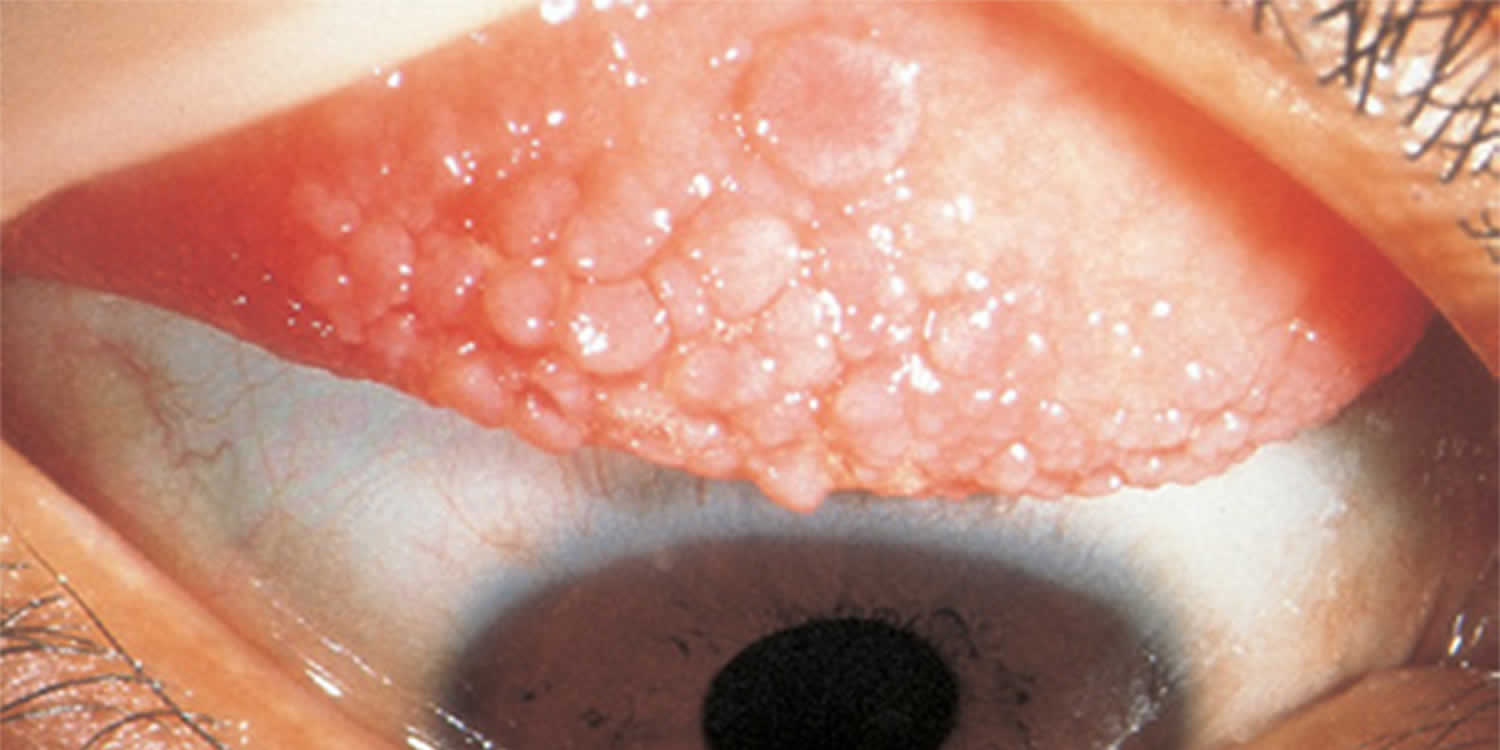
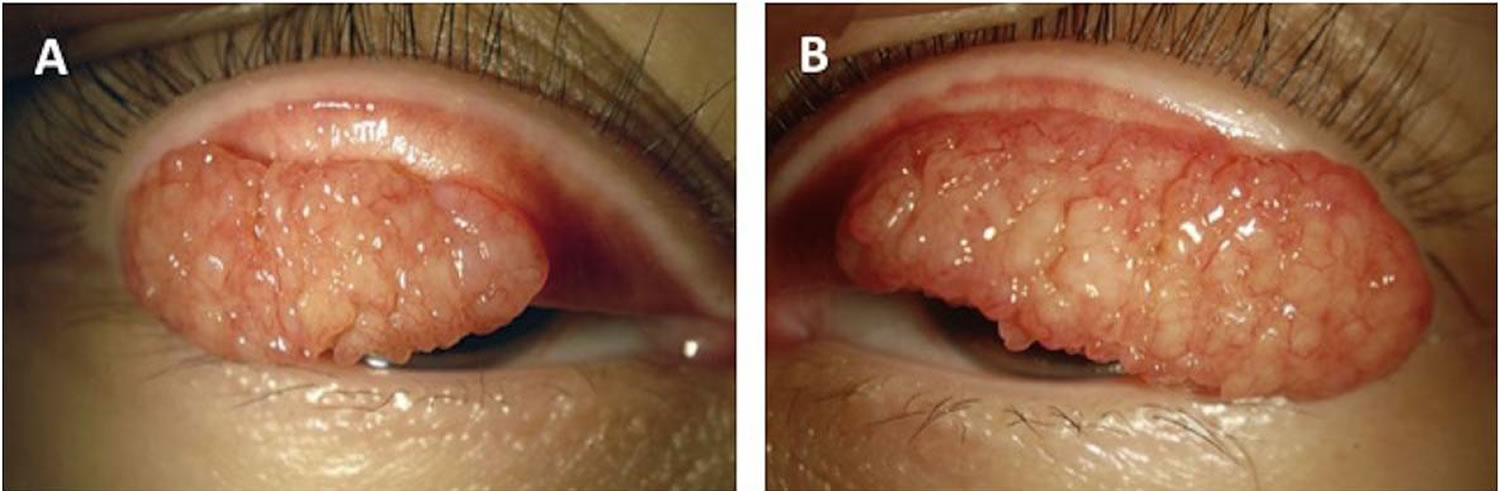
Figure 1. Giant papillary conjunctivitis
Footnote: Giant papillary conjunctivitis before excision A, Giant papillae of the right upper palpebral conjunctiva; B, Giant papillae of the left upper palpebral conjunctiva.
[Source 10 ]Giant papillary conjunctivitis causes
Giant papillary conjunctivitis was once considered an allergic disease similar to other immunoglobulin E (IgE)–mediated ocular allergy such as allergic conjunctivitis and vernal keratoconjunctivitis because of the similar clinical symptoms seen in allergic diseases (eg, itchiness, tearing, mucous hyperproduction, increase in symptoms during allergy season) 9. The mechanical irritation of contact lenses and sutures that causes giant papillary conjunctivitis supports the classification of giant papillary conjunctivitis into a group of nonallergic hypersensitivity disorders 12.
Giant papillary conjunctivitis seems to be caused by the following:
- An allergy, either to contact lenses or the chemicals used to clean them. Contact lens wearers with asthma, hay fever, or other allergies are more likely to get giant papillary conjunctivitis.
- A contact lens, artificial eye, or exposed stitches rubbing against the eyelid
- Deposits of proteins or other substances on the contact lenses
- Chronic eye allergies
The antigen(s) responsible for giant papillary conjunctivitis have yet to be identified 9. From circumstantial evidence, the initiating event is believed to be mechanical irritation and/or antigenic stimulus of the tarsal conjunctiva of the upper lids by a contact lens surface or edge (rigid or flexible) or deposit. Histologic changes in the tissue occur with mast cell degranulation and a secondary inflammatory cascade. This leads to conjunctivitis and further tissue changes with increasing inflammatory markers in the tears.
giant papillary conjunctivitis can be caused by all forms of ocular prostheses, including rigid and hydrogel (soft) contact lenses, prosthetic eyes, extruding scleral buckles, exposed portions of sutures, filters, knots, and even corneal scars 13. Heat sterilization, poor cleaning, thick or rough contact lens edges, and extended wearing times also predispose to the development of giant papillary conjunctivitis.
Lipid and protein deposits from the tears, as well as debris coating the surface of contact lenses, may also lead to a spiral of inflammation. This, in turn, causes even more lens deposits to form, leading to additional inflammation 14. The level of coating on the lenses varies among individuals and the polymer of the contact lenses.
High-water hydrogel (HEMA) contact lenses tend to coat more than lower-water HEMA contact lenses. Silicone contact lenses tend to accumulate more lipid deposits than HEMA lenses. First-generation silicone hydrogel contact lenses may be more prone to giant papillary conjunctivitis development, perhaps because of their mechanical stiffness or their higher propensity for lipid deposition. Silicone hydrogel lenses tend to induce more local giant papillary conjunctivitis (similar to the changes seen with rigid lenses), whereas hydrogel lenses tend to induce more generalized giant papillary conjunctivitis reactions in the palpebral conjunctiva 15.
Millions of people choose to wear contact lenses. However, they are not for everyone. You might not be able to wear them for the following reasons:
- You get a lot of eye infections.
- You have severe allergies or dry eyes that are hard to treat.
- You work or live where it is very dusty.
- You are not able to properly care for your contact lenses.
Your cornea and tear film must be healthy for you to be comfortable and see clearly with contact lenses.
To safely wear contact lenses, you must be committed to caring for them properly and replacing them when needed. Talk with your ophthalmologist or other eye care professional to discuss your vision needs and expectations. They can help you decide if contacts are a good option for you.
Giant papillary conjunctivitis prevention
Increased frequency of contact lens replacement (especially one-day disposables), rigorous cleaning, hydrogen peroxide disinfection, decreased wear times, and appropriate/timely professional supervision appear to reduce the prevalence of giant papillary conjunctivitis among users of hydrogel contact lenses.
Increased enzyme cleaning also appears to be prophylactic for wearers of rigid lenses 14.
Giant papillary conjunctivitis symptoms
At first, the inside of your eyelid gets rough, red, and swollen. Later, you may get papillary hypertrophy especially on the upper eyelid (tarsus) called papillae—that could grow to the size of a pimple. Mucous strands are seen both in the tear film and between the giant papillae.
Other giant papillary conjunctivitis symptoms include:
- Tearing
- Feeling like something is stuck in your eye
- Red, painful, itchy eyes
- Swollen or droopy eyelids (ptosis)
- Excess mucus discharge in the eye, which makes vision blurry
- Feeling like your contact lens is moving up on your eyeball when you blink.
Giant papillary conjunctivitis treatment
You need to take care of giant papillary conjunctivitis right away. If not, it can cause serious damage to your eyelid and to your cornea. The cornea is the clear, front window of your eye. If the cornea is damaged, you cannot see properly.
Here are treatment options for giant papillary conjunctivitis:
- Avoid wearing contact lenses for a few weeks. This gives the inside of your eye time to heal.
- Limit the amount of time you wear contact lenses each day.
- Use eyedrop medicine or ointment prescribed by your ophthalmologist to reduce itching and swelling.
- Change the type of contact lenses you wear.
- Avoid lens solutions with preservatives. Switch to unpreserved salt solutions.
Your ophthalmologist will discuss treatment options for you based on your condition.
Combination mast cell stabilizers/antihistamines and modification of contact lens type/hygiene are the primary treatments for giant papillary conjunctivitis (giant papillary conjunctivitis). Topical steroids can be used in the treatment of severe giant papillary conjunctivitis but are not always necessary, especially in mild cases.
Short-term low-potency topical corticosteroid used concurrently with a combination mast cell stabilizer/antihistamine ophthalmic solution is a more effective treatment for papillary conjunctivitis than mast cell stabilizer/antihistamine monotherapy and topical steroid monotherapy alone 16. However, combination mast cell stabilizers and antihistamine ophthalmic medications generally suffice without exposing the patient to the known risks of topical steroids. Most patients do not require more aggressive treatment.
Long-term use of topical steroid drops, especially for more than a few weeks, is associated with glaucoma, cataracts, and decreased ocular resistance to infection. Topical steroid use is a particular concern in patients with a history of herpetic eye disease. Although topical corticosteroid use is not associated with induction or facilitation of viral recurrence, a fulminant infection could occur if herpes virus infection recurs during topical corticosteroid treatment. Increased concerns exist regarding de novo fungal and other viral infections and potentiating bacterial infections. Contact lenses should not be worn while the patient is being treated with steroids.
Although contact lens cessation is the most effective initial treatment for giant papillary conjunctivitis, some patients may still need to wear contact lenses during treatment (eg, patients with keratoconus). Topical antihistamine/mast cell stabilizer combination solutions are the primary choice of treatment because of the drug efficacy and low frequency of dosing to improve patient compliance.
Topical mast cell stabilizers (eg, sodium cromolyn 0.4%) and antihistamines may also be used.
Topical nonsteroidal anti-inflammatory drugs (NSAIDs) have limited immediate hypersensitivity responses but can be effective in patients with giant papillary conjunctivitis. NSAIDs have rarely been associated with corneal melting.
More recently, immunomodulatory drugs such as tacrolimus 0.05% have been found comparable to fluorometholone 0.1% in efficacy without the adverse effects of steroids in the treatment of giant papillary conjunctivitis. More studies need to be conducted for this recent development. [30]
Cool compresses can be added to improve symptoms.
Surgical care
Surgical care is extremely rare, although there have been limited cases when surgery is used when medical therapy was not effective. giant papillary conjunctivitis is surgically removed and a free autologous conjunctival graft is used to cover the tarsal conjunctival defect 17.
Helpful tips for contact lens users
You must clean and disinfect any contact lens you remove from your eye before you put the lens back in. There are many types of cleansing systems. The choice depends on the type of lens you use, if you have allergies or if your eyes tend to form protein deposits. Ask your eye doctor what kind of cleaning solutions you should use.
Take special care to clean and store your lenses correctly to avoid dangerous eye infections.
Here is what you should do:
- Follow the schedule your eye doctor gives you for wearing and replacing your lenses. You should not wear daily wear lenses while you sleep.
- Remove contact lenses before taking a shower, using a hot tub, swimming, or doing anything where water gets in your eyes.
- Before touching your contact lenses, wash your hands with soap and water and dry them with a lint-free towel.
- Never put contacts in your mouth to wet them. Saliva (spit) is not a sterile solution.
- Do not rinse or store contacts in water (tap or sterile water). Also, never use a homemade saline solution.
- Do not use saline solution or rewetting drops to disinfect your lenses. They are not disinfectants.
- Follow directions from your doctor and from the lens cleaning solution manufacturer to clean and store your lenses.
- No matter what type of lens cleaning solution you buy, use a “rub and rinse” cleaning method. Rub your contact lenses with clean fingers, then rinse the lenses with solution before soaking them. Use this method even if the solution you are using is a “no-rub” type.
- Use new solution each time you clean and disinfect your contact lenses. Never reuse or “top off” with old solution. Also, do not pour contact lens solution into a different bottle. The solution will no longer be sterile.
- Make sure the tip of the solution bottle does not touch any surface. Keep the bottle tightly closed when you are not using it.
- Rinse your contact lens case with sterile contact lens solution (not tap water). Then leave the empty case open to air dry.
- Keep your contact lens case clean. Replace the case at least every 3 months, or right away if it gets cracked or damaged.
- If you store your lenses in the case for a long time, check the contact lens instructions or the lens solution directions to see if you should re-disinfect them before wearing them. Never wear your contact lenses if they have been stored for 30 days or longer without re-disinfecting.
- Contact lenses can warp over time, and your cornea can change shape. To make sure your lenses fit properly and the prescription is right for you, see your eye doctor regularly.
Giant papillary conjunctivitis prognosis
The prognosis of giant papillary conjunctivitis is good. Approximately 80% of patients can return to comfortable contact lens wear with appropriate treatment 8.
giant papillary conjunctivitis has been a common cause of temporary and permanent contact lens intolerance. It can also cause ptosis of the upper lids.
The lids of some patients return to normal appearance following the resolution of giant papillary conjunctivitis, whereas other lids retain small, white, capped scars of the giant papillary lesions for long periods, sometimes indefinitely.
Giant papillary conjunctivitis is not associated with mortality.
References- Baab S, Kinzer EE. Allergic Conjunctivitis. [Updated 2018 Nov 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448118
- Jordakieva G, Jensen-Jarolim E. The impact of allergen exposure and specific immunotherapy on circulating blood cells in allergic rhinitis. World Allergy Organ J. 2018;11(1):19.
- Ojeda P, Sastre J, Olaguibel JM, Chivato T., investigators participating in the National Survey of the Spanish Society of Allergology and Clinical Immunology Alergológica 2015. Alergológica 2015: A National Survey on Allergic Diseases in the Adult Spanish Population. J Investig Allergol Clin Immunol. 2018 Jun;28(3):151-164.
- La Rosa M, Lionetti E, Reibaldi M, et al. Allergic conjunctivitis: a comprehensive review of the literature. Ital J Pediatr. 2013;39:18. Published 2013 Mar 14. doi:10.1186/1824-7288-39-18 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3640929
- Friedlander MH. Ocular Allergy. Curr Opin Allergy Clin Immunol. 2011;11(5):477–482. doi: 10.1097/ACI.0b013e32834a9652
- Wong AH, Barg SS, Leung AK. Seasonal and perennial conjunctivitis. Recent Pat Inflamm Allergy Drug Discov. 2009;3:118–127. doi: 10.2174/187221309788489733
- Porazinski AD, Donshik PC. Giant papillary conjunctivitis in frequent replacement contact lens wearers: a retrospective study. CLAO J. 1999 Jul. 25 (3):142-7.
- Donshik PC, Ballow M, Luistro A, Samartino L. Treatment of contact lens-induced giant papillary conjunctivitis. CLAO J. 1984 Oct-Dec. 10(4):346-50.
- Giant papillary conjunctivitis. https://emedicine.medscape.com/article/1191641-overview
- Lai Y, Sundar G, Ray M. Surgical treatment outcome of medically refractory huge giant papillary conjunctivitis. Am J Ophthalmol Case Rep. 2017;8:22–24. Published 2017 Sep 18. doi:10.1016/j.ajoc.2017.09.002 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5731670
- Donshik P.C. Giant papillary conjunctivitis. Trans Am Ophthalmol Soc. 1994;92:687–744.
- García-Posadas L, Contreras-Ruiz L, Soriano-Romaní L, Dartt DA, Diebold Y. Conjunctival Goblet Cell Function: Effect of Contact Lens Wear and Cytokines. Eye Contact Lens. 2016 Mar. 42 (2):83-90.
- Dunn JP Jr, Weissman BA, Mondino BJ, Arnold AC. Giant papillary conjunctivitis associated with elevated corneal deposits. Cornea. 1990 Oct. 9(4):357-8
- Donshik PC, Ehlers WH, Ballow M. Giant papillary conjunctivitis. Immunol Allergy Clin North Am. 2008 Feb. 28(1):83-103, vi.
- Skotnitsky CC, Naduvilath TJ, Sweeney DF, Sankaridurg PR. Two presentations of contact lens-induced papillary conjunctivitis (CLPC) in hydrogel lens wear: local and general. Optom Vis Sci. 2006 Jan. 83 (1):27-36.
- Diao H, She Z, Cao D, Wang Z, Lin Z. Comparison of tacrolimus, fluorometholone, and saline in mild-to-moderate contact lens-induced papillary conjunctivitis. Adv Ther. 2012 Jul. 29 (7):645-53.
- Lai Y, Sundar G, Ray M. Surgical treatment outcome of medically refractory huge giant papillary conjunctivitis. Am J Ophthalmol Case Rep. 2017 Dec. 8:22-24.