Hamate fracture
Hamate fractures can be classified broadly on the basis of the Milch classification into fractures of either the hook or the body. Hamate fractures are rare and underreported. Hamate fractures can pose a diagnostic challenge for the treating physician 1. Hamate fractures are usually misdiagnosed or confused with simple wrist sprains. The rarity of hamate fracture as well as the complex anatomy of the carpal bones can make hamate fracture diagnosis commonly missed 2. Hamate fractures (hook and body) tend to occur in young, active people. Hamate fractures are unusual in children.
The mechanism of injury to the hamate dictates the fracture type and orientation. Fractures of the hamate hook are commonly seen in golfers, baseball players, and racket sport players. Falls and crush injuries are also common injury mechanisms. In comparison, body fractures of the hamate are more associated with the mechanism of a clenched fist striking a wall 3.
Hamate fractures are unfrequent injuries, accounting for 2 to 4% of carpal fractures 4. Distal carpal row fractures are less common than first row fractures.
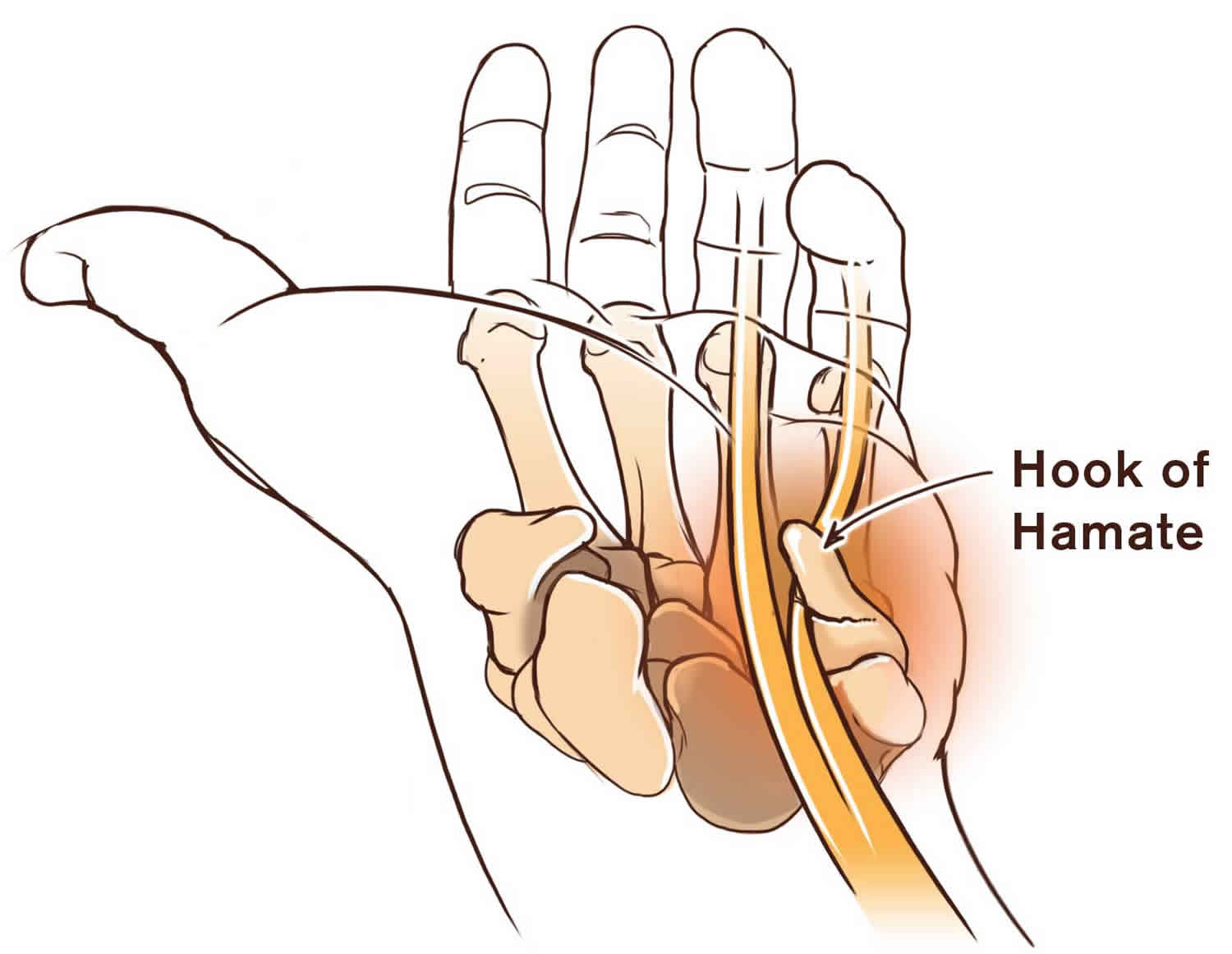
Considering hamate bone unique anatomy (Figure 2), hamate fractures usually get subdivided into two broad groups: hook fractures and body fractures 5.
Classification of hamate fractures 6:
- Type 1: Hook of the hamate fracture. The hook of the hamate fractures are the most common and can occur via several different mechanisms 7. First, repeated microtrauma to the hook during sports involving swinging clubs, bats, or racquets can result in a hook stress fracture. These usually occur in the nondominant hand and account for approximately one third of hamate fractures. Second, direct trauma can be applied during sports when the butt of the club rests on the hamate and the force of the swing is then transmitted directly to the bone. In addition, indirect trauma can be applied to the hook through its muscular and ligamentous attachments. This can occur either when falling on a hyperextended wrist or during power grips.
- Type 2: Body of the hamate fracture. Type 2 fractures involving the body of the hamate are less common than type 1 hook of hamate fractures and always require direct force 8. Most commonly, these fractures occur with a punch-press injury or dorsopalmar compression of the wrist between heavy weights 7.
- 2a: Coronal (may be dorsal oblique or splitting fracture)
- 2b: Transverse fracture
The hook of hamate fracture frequently occurs in sports where a firm grip is required, such as tennis, baseball, and golf 9. Body of the hamate fractures are related to higher energy trauma such as a punch and may be associated with concomitant carpal fractures and carpometacarpal dislocations. Body of hamate fractures are less common 10.
Associated hook of hamate fracture injuries:
- Ulnar artery injury
- Ulnar nerve injury
Associated body of hamate fracture injuries:
- Fourth and fifth metacarpal fracture-dislocation
- Greater arc perilunate fracture-dislocation
Hamate anatomy
The hamate is a triangular shaped bone that forms part of the distal carpal row, articulating with the capitate (radially), triquetrum (proximally) and fifth and fourth metacarpals (distally) (Figures 1 and 2).
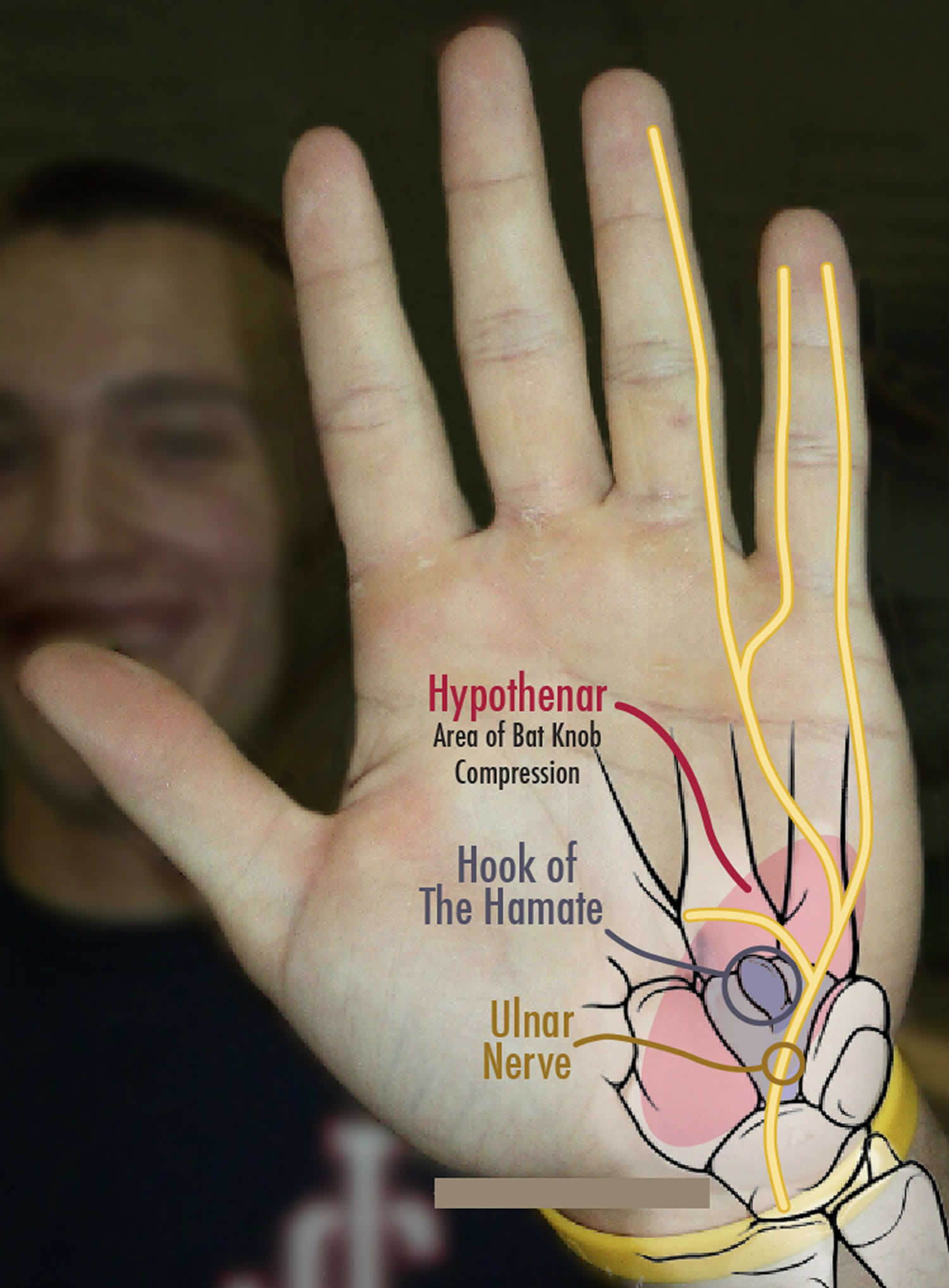
A roughly circular projection or hook on the volar surface of the hamate is the inferolateral border of the Guyon canal. The roof (superficial) of the canal is formed by the palmar carpal ligament, and the floor (deep) is formed by the flexor retinaculum. The canal carries the ulnar artery and nerve, and, for this reason, hook fractures should suggest a high probability of ulnar artery and nerve damage 11. In addition, the hamate hook has a dual blood supply, with vessels entering from both the ulnar tip and radial base. These vessels often have a poor anastomosis, which clinically can result in nonunion due to insufficient blood supply.
Figure 1. Hand bones
Figure 2. Hamate bone in hand
Hamate fracture causes
The hook of hamate injuries are mainly due to repeated impact, usually, a sporting activity (racket, club, bat) exerting a direct force against the hamate 12. The hook of hamate is always at risk because of its peculiar anatomy, protruding from its body into the ulnar aspect of the palm. Avulsion fractures of the hook may also occur, taking into account that this portion of the hamate serves as an attachment point for three tendons (opponens digiti minimi, flexor digiti minimi and flexor carpi ulnaris) 13.
Body of the hamate fracture is a consequence of a direct blow over the hypothenar eminence or a considerably strong dorsopalmar compression 14. A body fracture may also accompany high energy trauma resulting in wrist fracture-dislocations 15. Body of the hamate fractures can lead to axial carpal instability.
Hamate fracture prevention
Having good strength and flexibility of both the wrist flexors and extensors can aid in the prevention of some wrist injuries. If participating in sports activities in which diving or falling is not an uncommon occurrence (eg, rollerblading, skiing, ice skating), a protective wrist guard may be recommended to prevent injury to the wrist and hand. Athletes who golf may have increased risk for fracturing the hook of the hamate secondary to repetitive wrist extension. One good method of prevention in this population is to ensure that a proper length of club is always used.
Hamate fracture symptoms
Hook of hamate fractures are usually seen in individuals who participate in sports involving a racquet, bat, or club or in individuals who have a history of falling on an outstretched hand 16. Because most patients with this injury seek medical advice only after persistent symptoms, they often present weeks to months after the initial injury. Most report palmar pain aggravated by grasp, pain with dorsoulnar deviation, and pain with flexion of the fourth and fifth digits.
Suspicion should be high in young athletes with chronic pain along the ulnar aspect of the wrist. Chronic wrist pain is common with a hook of the hamate fracture, with tenderness and exquisite pain over the hypothenar area. Paresthesias along the ring and small finger are relatively common in chronic disease 17. Delayed medical consultation is not uncommon.
Because of its relation to higher energy trauma and associated injuries, the body of the hamate fracture diagnosis tends to be acute. Swelling and tenderness over the dorsal ulnar wrist frequently present in hamate body fractures.
Weakened grip strength is typical. Grasp maneuvers provoke pain along the ulnar side of the wrist. Fourth and fifth metacarpal pain is related to hamate injuries; even metacarpal deformity may be an indirect sign of the body of the hamate fracture.
Hamate fracture complications
Hamate fracture complications include ulnar nerve compression at the level of the Guyon canal. The hook of the hamate is the distal lateral border of the Guyon canal and is close to the motor branch of the ulnar nerve and ulnar artery as they pass through the canal. The ulnar nerve then turns around the hook of the hamate and travels deep to innervate the intrinsic musculature. When surgical treatment is indicated, care must be taken to prevent damage to the motor branch of the ulnar nerve. Additionally, rupture of the small- and ring-finger flexor tendons may occur if injured by the irregular fracture edges.
The most frequent complication is nonunion 18. This can follow conservative treatment in more than 50% of patients. Often, these patients present with continued palmar pain, especially with grip. Conventional radiographs can miss this diagnosis in 30-50% of patients. Therefore if the clinical suspicion is high and radiographic findings are negative, CT scanning should be performed. The treatment of nonunion involves either excision of the hook of hamate or open reduction and internal fixation (ORIF).
Hamate fracture diagnosis
Initial radiographs include anteroposterior and lateral wrist views. The overlapping of the hook of the hamate and its body is known as the “ring sign,” a normal finding in the anteroposterior view. In some hook fractures, the so-called “ring sign” may be disrupted. Other signs that are visible in the anteroposterior view are loss of cortical density at the base of the hook and even absence of the hook 19. Body fractures are usually visible in standard lateral projection or on CT scan.
Nevertheless, standard radiographs posses a high rate of false negatives, with a 70% sensitivity 20. Specific views include carpal tunnel projection and semisupine oblique radially deviated projection 21. CT scan is often necessary to reach proper diagnosis (100% sensitivity) 22. MRI scan is only necessary for chronic disease (avascular necrosis)
If a surgical procedure is required, routine blood work should be performed based on the patient’s history and physical exam.
Hamate fracture test
Though clinical findings may be vague and unspecific, there are some tests that are useful if a hamate fracture is suspected.
Pull test
In the hook of the hamate fractures, active flexion of distal interphalangeal joints of the ring and small finger may cause pain or resisted distal interphalangeal flexion of the fourth and fifth fingers with the wrist in ulnar deviation causes pain over the fractured hook. This phenomenon is the result of flexor tendons deforming forces attached at the fracture site 23.
Hamate fracture treatment
Hook of hamate fractures:
- Acute, nondisplaced: Immobilization, ulnar gutter cast for six weeks. There is still debate whether patients may profit from initial surgical treatment in this type of fractures. Sport players will usually benefit from early surgical management, returning to sports activities in three months.
- Acute, displaced: Excision of a bony fragment is the gold standard procedure. Open reduction and internal fixation (screws or Kirschner wires) is another proven treatment. Both alternatives showed similar clinical results 24.
- Chronic pain, nonunion: These signs require fracture pinning with bone grafting.
Body of hamate fractures:
- Acute, nondisplaced: Immobilization, six-week cast 25.
- Acute, displaced: Open reduction and internal fixation (Kirschner wires, grid plate, or headless compression screws) 26.
Hamate bone surgery
Surgical indications: displaced fractures, nonunion, ulnar nerve compression, median nerve compression, ulnar artery compression, tendon rupture and metacarpal subluxation.
In the past, hamate hook fractures were treated conservatively with lower arm cast immobilization for 6 weeks, provided the fracture was diagnosed within 1 week of the injury 27. Retrospective analyses have demonstrated nonunion rates greater than 50% and as high as 80-90% with conservative treatment. These nonunions are likely multifactorial, involving poor blood supply, delayed diagnosis, and fragment displacement with continuous movement of the fourth and fifth digits while casted. Therefore, all hamate hook fractures should be referred to a hand surgeon for possible surgical intervention.
Two types of surgeries are commonly performed for hamate hook fractures 27. One involves excision of the hook itself. The other is an open reduction and internal fixation (ORIF) procedure. Of the 2 procedures, the former (excision of the hook) is considered the criterion standard 28.
Complications that may arise from hook excision include decreased grip strength secondary to removal of the attachment for the transverse carpal ligament, pisohamate ligament, and flexor and opponens digiti minimi muscles. Because of this concern, 2 retrospective studies compared grip strength in patients who underwent excision versus those who underwent open reduction and internal fixation (ORIF) 27, 8. Both studies failed to show any statistically significant difference in grip strength up to 3 years post procedure.
Hamate body fractures are commonly associated with dislocation of the fourth and fifth fingers 29. Shearing forces from the metacarpals can cause either a dorsal cortical hamate fracture or a coronal body fracture 30. These fractures can be reapproximated by reduction of the carpometacarpal joint; however, they usually require internal fixation because of the high incidence of instability in these injuries 31.
Surgical tech tips:
- The motor branch of the ulnar nerve must be clearly spotted and retracted before hook excision or drilling.
- After fractured fragment excision, periosteum closure should be over the base of the remaining body to protect the ulnar nerve and tendons.
Rehabilitation
Recovery from injury occurs in 4 stages (ie, wound healing, recovery of motion, recovery of strength and power, and recovery of endurance). Although these divisions are arbitrary, they provide a progressive sequence for management and a target for physical therapy. Early motion, instituted before collagen cross-linking and scarring occur, favors functional recovery. Collagen has more elasticity in the earlier stages of formation; and this elasticity decreases with time and immobilization.
The goals of physical therapy are tailored to the desires of the patient and the demands of his or her occupation or lifestyle. In all phases of recovery, special attention is directed to any development of edema. Fibrin contained in the exudate has the potential to evolve into scar tissue and limit function. For this reason, recommend elevation, compression, and motion in order to mobilize excess fluid from around the wound until maximum medical recovery is achieved.
The ability to begin physical therapy and increase the intensity of exercises varies according to the initial treatment of the hamate fracture. Conservative treatment requires immobilization with casting for 6 weeks, followed by an additional 4-6 weeks of physical therapy. If the injury is treated surgically with hook excision, the patient can start physical therapy immediately, without limitations, and can return to full activity within 6-8 weeks. If the injury is treated surgically with ORIF, the patient requires casting for 2 weeks, followed by an additional 4 weeks of physical therapy without placing strain on the affected wrist, before progressing to full activity in 6-8 weeks 32.
Return to play
Return to full activity depends on the patient’s activity level and desires. Return to full activity is also dependent on the initial fracture treatment. Typically, if treated conservatively, simple fractures of the hamate are unified within 6-8 weeks of injury.
Patient participation in full-contact sports, such as football, usually requires bracing or protection for the wrist until full musculature and flexibility have returned. This improvement should be achieved within 12 weeks with a diligent physical therapy program. In contrast, if the injury is treated surgically with either ORIF or excision, return to play occurs much sooner. Although no evidence-based guidelines have been developed, the general consensus is that return to play takes 6-8 weeks after either surgery, but this is very individualized and often depends on the level of the athlete.
A study by Guss et al that included data from 18 Major League Baseball players with hook of hamate fractures reported no significant change in Wins Above Replacement or isolated power when preinjury and postinjury performance were compared and also reported no significant decline in performance the first season and second season after injury was found 33.
Hamate fracture prognosis
Hamate fractures treated conservatively should generally heal in 8 weeks 6. Non-displaced hook fractures treated conservatively have a 50% rate of nonunion. Symptomatic nonunion will require further surgical treatment. Surgical treatment (fragment excision or open reduction and internal fixation [ORIF]) provides a more rapid return to daily activities and sports 34. The prognosis of hamate fractures depends on the degree of injury encountered and the patient’s effort in the physical therapy program. In a retrospective review of 29 cases, the patient’s functional recovery was indirectly related to the degree of soft-tissue damage at the time of the injury (an increase in soft-tissue damage results in a decrease in functional recovery) 8.
References- Snoap T, Habeck J, Ruiter T. Hamate Fracture. Eplasty. 2015;15:ic28. Published 2015 Jun 4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4462833
- Bishop AT, Beckenbaugh RD. Fracture of the hamate hook. J Hand Surg Am. 1988 Jan;13(1):135-9.
- Classification and treatment of hamate fractures. Hirano K, Inoue G. Hand Surg. 2005; 10(2-3):151-7.
- Devers BN, Douglas KC, Naik RD, Lee DH, Watson JT, Weikert DR. Outcomes of hook of hamate fracture excision in high-level amateur athletes. J Hand Surg Am. 2013 Jan;38(1):72-6.
- Arora S, Goyal A, Mittal S, Singh A, Sural S, Dhal A. Combined intraarticular fracture of the body and the hook of hamate: an unusual injury pattern. J Hand Microsurg. 2013 Dec;5(2):92-5.
- Abrego MO, De Cicco FL. Hamate Fractures. [Updated 2019 Jul 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK544314
- Goliver JA, Adamow JS, Goliver J. Hamate body and capitate fracture in punch injury. Am J Emerg Med. 2014 Oct. 32 (10):1303.e1-2.
- Hirano K, Inoue G. Classification and treatment of hamate fractures. Hand Surg. 2005. 10(2-3):151-7.
- Arora S, Goyal A, Mittal S, Singh A, Sural S, Dhal A. Combined intraarticular fracture of the body and the hook of hamate: an unusual injury pattern. J Hand Microsurg. 2013;5(2):92–95. doi:10.1007/s12593-012-0070-2 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3827647
- Yalcinkaya M, Azar N, Dogan A. A rare wrist injury: simultaneous fractures of the hamate body and scaphoid waist. Orthopedics. 2009 Aug;32, 8.
- Failla JM. Hook of hamate vascularity: vulnerability to osteonecrosis and nonunion. J Hand Surg [Am]. 1993 Nov. 18(6):1075-9.
- Bachoura A, Wroblewski A, Jacoby SM, Osterman AL, Culp RW. Hook of hamate fractures in competitive baseball players. Hand (N Y). 2013 Sep;8(3):302-7.
- Blum AG, Zabel JP, Kohlmann R, Batch T, Barbara K, Zhu X, Dautel G, Dap F. Pathologic conditions of the hypothenar eminence: evaluation with multidetector CT and MR imaging. Radiographics. 2006 Jul-Aug;26(4):1021-44.
- Chen NC, Jupiter JB, Jebson PJ. Sports-related wrist injuries in adults. Sports Health. 2009 Nov;1(6):469-77.
- Walsh JJ, Bishop AT. Diagnosis and management of hamate hook fractures. Hand Clin. 2000 Aug;16(3):397-403, viii.
- Guha AR, Marynissen H. Stress fracture of the hook of the hamate. Br J Sports Med. 2002 Jun. 36(3):224-5.
- Mouzopoulos G, Vlachos C, Karantzalis L, Vlachos K. Fractures of hamate: a clinical overview. Musculoskelet Surg. 2019 Apr;103(1):15-21.
- Scheufler O, Radmer S, Erdmann D, et al. Therapeutic alternatives in nonunion of hamate hook fractures: personal experience in 8 patients and review of literature. Ann Plast Surg. 2005 Aug. 55(2):149-54.
- Cockenpot E, Lefebvre G, Demondion X, Chantelot C, Cotten A. Imaging of Sports-related Hand and Wrist Injuries: Sports Imaging Series. Radiology. 2016 Jun;279(3):674-92.
- Suh N, Ek ET, Wolfe SW. Carpal fractures. J Hand Surg Am. 2014 Apr;39(4):785-91; quiz 791.
- Andresen R, Radmer S, Scheufler O, Adam C, Bogusch G. [Optimization of conventional X-ray images for the detection of hook of hamate fractures]. Rontgenpraxis. 2006;56(2):59-65.
- Andresen R, Radmer S, Sparmann M, Bogusch G, Banzer D. Imaging of hamate bone fractures in conventional X-rays and high-resolution computed tomography. An in vitro study. Invest Radiol. 1999 Jan;34(1):46-50.
- O’Shea K, Weiland AJ. Fractures of the hamate and pisiform bones. Hand Clin. 2012 Aug;28(3):287-300, viii.
- Stark HH, Chao EK, Zemel NP, Rickard TA, Ashworth CR. Fracture of the hook of the hamate. J Bone Joint Surg Am. 1989 Sep;71(8):1202-7.
- Whalen JL, Bishop AT, Linscheid RL. Nonoperative treatment of acute hamate hook fractures. J Hand Surg Am. 1992 May;17(3):507-11.
- Eder C, Scheller A, Schwab N, Krapohl BD. Hamate’s coronal fracture: diagnostic and therapeutic approaches based on a long-term follow-up. GMS Interdiscip Plast Reconstr Surg DGPW. 2019;8:Doc05.
- Scheufler O, Andresen R, Radmer S, et al. Hook of hamate fractures: critical evaluation of different therapeutic procedures. Plast Reconstr Surg. 2005 Feb. 115(2):488-97.
- Tolat AR, Humphrey JA, McGovern PD, Compson J. Surgical excision of ununited hook of hamate fractures via the carpal tunnel approach. Injury. 2014 Oct. 45 (10):1554-6.
- Pajares-López M, Hernández-Cortés P, Robles-Molina MJ. Rupture of small finger flexor tendons secondary to asymptomatic nonunion of the hamate hook. Orthopedics. 2011 Jan 1. 34(2):142.
- Cano Gala C, Pescador Hernández D, Rendón Díaz DA, López Olmedo J, Blanco Blanco J. Fracture of the body of hamate associated with a fracture of the base of fourth metacarpal: A case report and review of literature of the last 20 years. Int J Surg Case Rep. 2013. 4(5):442-5
- Gill NW, Rendeiro DG. Hook of the hamate fracture. J Orthop Sports Phys Ther. 2010 May. 40(5):325.
- Devers BN, Douglas KC, Naik RD, Lee DH, Watson JT, Weikert DR. Outcomes of hook of hamate fracture excision in high-level amateur athletes. J Hand Surg Am. 2013 Jan. 38(1):72-6.
- Guss MS, Begly JP, Ramme AJ, Taormina DP, Rettig ME, Capo JT. Performance Outcomes After Hook of Hamate Fractures in Major League Baseball Players. J Sport Rehabil. 2018 Jul 27. 1-4.
- Tolat AR, Humphrey JA, McGovern PD, Compson J. Surgical excision of ununited hook of hamate fractures via the carpal tunnel approach. Injury. 2014 Oct;45(10):1554-6.