What is hay fever
Hay fever also known as seasonal allergic rhinitis, is an allergic reaction to allergens like molds, pollens, dust mites, insects and animal dander. Hay fever affects millions of people worldwide. Symptoms of hay fever are seasonal. You will feel worse when the pollens that affect you are at their highest levels. Symptoms include sneezing, stuffiness, a runny nose and itchiness in your nose, the roof of your mouth, throat, eyes or ears. These allergic reactions are most commonly caused by pollen and mold spores in the air, which start a chain reaction in your immune system.Sometimes symptoms are caused by molds or flakes of animal skin (dander) from pets. If pollen is the cause, you will feel worse when pollen levels are high.
Pollen comes from flowering trees, grass, and weeds. If you are allergic to pollen, you will notice your symptoms are worse on hot, dry days when wind carries the pollen. On rainy days, pollen often is washed to the ground, which means you are less likely to breathe it.
- Allergies that occur in the spring (late April and May) are often due to tree pollen.
- Allergies that occur in the summer (late May to mid-July) are often due to grass and weed pollen.
- Allergies that occur in the fall (late August to the first frost) are often due to ragweed.
Allergens that can cause perennial (year-round) allergic rhinitis include:
- Mold. Mold is common where water tends to collect, such as shower curtains and damp basements. It can also be found in rotting logs, hay, and mulch. This allergy is usually worse during humid and rainy weather.
- Animal dander.Proteins found in the skin, saliva, and urine of furry pets such as cats and dogs are allergens. You can be exposed to dander when handling an animal or from house dust that contains dander.
- Dust. Many allergens, including dust mites, are in dust. Dust mites are tiny living creatures found in bedding, mattresses, carpeting, and upholstered furniture. They live on dead skin cells and other things found in house dust.
Is hay fever contagious?
Hay fever, also called allergic rhinitis, causes cold-like signs and symptoms, such as a runny nose, itchy eyes, congestion, sneezing and sinus pressure. But unlike a cold, hay fever isn’t caused by a virus. Hay fever is caused by an allergic response to outdoor or indoor allergens, such as pollen, dust mites or tiny flecks of skin and saliva shed by cats, dogs and other animals with fur or feathers (pet dander).
Hay fever lasts longer than a cold or the flu—up to several weeks—and does not cause fever. With hay fever, the fluid from your nose is thin, watery, and clear. With a cold or the flu, the fluid tends to be thicker. Itching (mostly eyes, nose, mouth, throat, and skin) is common with hay fever but not with a cold or the flu. Sneezing happens more with hay fever. Hay fever does not cause fever.
Besides making you miserable, hay fever can affect your performance at work or school and generally interfere with your life. But you don’t have to put up with annoying symptoms. You can learn to avoid triggers and find the right treatment.
Figure 1. Hay fever rash
What causes hay fever?
Allergens cause your body to respond with an allergic reaction. When you are exposed to something you are allergic to, your body releases chemicals. One of theses chemicals is histamine, which is your body’s defense against the allergen. The release of histamine causes swelling, itching, sneezing, runny nose, and watery eyes.
If you are allergic to pollen, you will notice that your symptoms are worse on hot, dry days when wind carries the pollen. On rainy days, pollen often is washed to the ground, which means you are less likely to breathe it.
Hay fever symptoms are most often triggered by tree pollen in the early spring. Grasses are often the culprit during the late spring and early summer. Weeds are most often the cause of late summer and fall hay fever symptoms.
What is pollen?
The word pollen is derived from the Greek word meaning ‘fine flour’. Pollen is the male fertilizing agent (male gametes or sperm cells) of flowering plants, trees, grasses and weeds and the role of the pollen grain is to fertilize the female flower to reproduce plant species. Pollen is also a major allergen that causes symptoms of seasonal allergic rhinitis (hay fever).
Pollen from plants with colorful flowers, like roses, usually do not cause allergies. These plants large, waxy pollen are carried from plant to plant by bees and other insects for fertilization. On the other hand, many trees, grasses and low-growing weeds have small, light, dry powdery pollen that are easily spread by wind. These are the pollen that trigger allergy symptoms.
Each plant has a period of pollination that does not vary much from year to year. However, weather conditions affect pollen levels. For instance, wind and humidity may affect pollen counts. Because pollen are small, light and dry, they can be easily spread by wind, which keeps pollen airborne and carries it over long distances. When the air is humid, such as during or after it rains, pollen becomes damp and heavy with moisture, keeping it still and on the ground. Seasonal allergic rhinitis is often caused by tree pollen in the early spring. During the late spring and early summer, grass pollen often cause symptoms. Late summer and fall hay fever is caused by weed pollen. In warmer places, pollination can be year-round.
Allergy symptoms are often minimal on days that are rainy, cloudy or windless, because pollen does not move about during these conditions. Hot, dry and windy weather signals greater pollen and mold distribution and therefore, increased allergy symptoms.
Pollen grains can be spread by birds, bees or wind:
- Some plants (such as flowering plants, including wattle trees) produce small amounts of pollen which are distributed by birds and bees from one plant to another.
- Other plants (such as pasture grasses and weeds) rely on the wind to spread their pollen. These pollen are produced in vast quantities, blow long distances and cause allergies in people, even if they live a long way from the source.
Most of the pollen that cause seasonal allergies is produced by airborne pollen from grasses, trees and weeds:
- Improved pasture grasses are more allergenic than native grasses.
- Pollen from exotic trees, which are planted for their autumn colors, is more allergenic than pollen from native trees.
How long does hay fever last?
Pollen seasons can last for several months. For more information you may want to visit the American Academy of Allergy, Asthma & Immunology’s National Allergy Bureau (NAB™) to find information on the current pollen and mold spore levels in your area: http://www.aaaai.org/global/nab-pollen-counts
The National Allergy Bureau currently provides the most accurate and reliable pollen and mold levels from approximately 84 counting stations throughout the United States, one counting station in Canada, and six counting stations in Argentina. The stations use air sampling equipment to collect airborne pollen and spores which are then examined microscopically. This information is also used for research to aid in the diagnosis, treatment and management of allergic diseases.
Pollen counts from the National Allergy Bureau stations are based on actual counts, which reflect the real day to day weather events. Predicted counts reported on many websites may be based on pollen data from previous years and general weather forecasts.
Ragweed Pollen
Ragweed and other weeds such as curly dock, lambs quarters, pigweed, plantain, sheep sorrel and sagebrush are some of the most prolific producers of pollen allergens.
Although the ragweed pollen season runs from August to November, ragweed pollen levels usually peak in mid-September in many areas in the country.
In addition, pollen counts are highest between 5:00 a.m. – 10:00 a.m. and on dry, hot and windy days.
Preventive Strategies
- Avoid the outdoors between 5:00 a.m. – 10:00 a.m. Save outside activities for late afternoon or after a heavy rain, when pollen levels are lower.
- Keep windows in your home and car closed to lower exposure to pollen. To keep cool, use air conditioners and avoid using window and attic fans.
- Be aware that pollen can also be transported indoors on people and pets.
- Dry your clothes in an automatic dryer rather than hanging them outside. Otherwise pollen can collect on clothing and be carried indoors.
Grass Pollen
As with tree pollen, grass pollen is regional as well as seasonal. In addition, grass pollen levels can be affected by temperature, time of day and rain.
Of the 1,200 species of grass that grow in North America, only a small percentage of these cause allergies. The most common grasses that can cause allergies are:
- Bermuda grass
- Johnson grass
- Kentucky bluegrass
- Orchard grass
- Sweet vernal grass
- Timothy grass
Preventive Strategies:
- If you have a grass lawn, have someone else do the mowing. If you must mow the lawn yourself, wear a mask.
- Keep grass cut short.
- Choose ground covers that don’t produce much pollen, such as Irish moss, bunch, and dichondra.
- Avoid the outdoors between 5:00 a.m. – 10:00 a.m. Save outside activities for late afternoon or after a heavy rain, when pollen levels are lower.
- Keep windows in your home and car closed to lower exposure to pollen. To keep cool, use air conditioners and avoid using window and attic fans.
- Be aware that pollen can also be transported indoors on people and pets.
- Dry your clothes in an automatic dryer rather than hanging them outside. Otherwise pollen can collect on clothing and be carried indoors.
Tree Pollen
Trees can aggravate your allergy whether or not they are on your property, since trees release large amounts of pollen that can be distributed miles away from the original source.
Trees are the earliest pollen producers, releasing their pollen as early as January in the Southern states and as late as May or June in the Northern states.
Most allergies are specific to one type of tree such as:
- catalpa
- elm
- hickory
- olive
- pecan
- sycamore
- walnut
or to the male cultivar of certain trees. The female of these species are totally pollen-free:
- ash
- box elder
- cottonwood
- date palm
- maple (red)
- maple (silver)
- Phoenix palm
- poplar
- willow
Some people, though, do show cross-reactivity among trees in the alder, beech, birch and oak family, and the juniper and cedar family.
Preventive Strategies
- If you buy trees for your yard, look for species that do not aggravate allergies such as crape myrtle, dogwood, fig, fir, palm, pear, plum, redbud and redwood trees or the female cultivars of ash, box elder, cottonwood, maple, palm, poplar or willow trees.
- Avoid the outdoors between 5:00 a.m. – 10:00 a.m. Save outside activities for late afternoon or after a heavy rain, when pollen levels are lower.
- Keep windows in your home and car closed to lower exposure to pollen. To keep cool, use air conditioners and avoid using window and attic fans.
- Be aware that pollen can also be transported indoors on people and pets.
- Dry your clothes in an automatic dryer rather than hanging them outside. Otherwise pollen can collect on clothing and be carried indoors.
Hay fever causes
Your immune system controls how your body defends itself. For instance, if you have an allergy to pollen, your immune system identifies pollen as an invader or allergen. Your immune system overreacts by producing antibodies called Immunoglobulin E (IgE) 1. These antibodies travel to mast cells that release histamine and other chemicals, causing an allergic reaction that leads to the signs and symptoms of hay fever — such as sneezing, stuffiness, a runny nose, itching and post-nasal drip.
Oversensitive immune system
If you have allergic rhinitis, your immune system – your natural defence against infection and illness – will react to an allergen as if it were harmful.
If your immune system is oversensitive, it will react to allergens by producing antibodies to fight them off. Antibodies are special proteins in the blood that are usually produced to fight viruses and infections.
Allergic reactions don’t occur the first time you come into contact with an allergen. The immune system has to recognize and “memorize” it before producing antibodies to fight it. This process is known as sensitization.
After you develop sensitivity to an allergen, it will be detected by antibodies called immunoglobulin E (IgE) whenever it comes into contact with the inside of your nose and throat.
These antibodies cause cells to release a number of chemicals, including histamine, which can cause the inside layer of your nose (the mucous membrane) to become inflamed and produce excess mucus. This is what causes the typical symptoms of sneezing and a blocked or runny nose.
Common allergens
Allergic rhinitis is triggered by breathing in tiny particles of allergens. The most common airborne allergens that cause rhinitis are described below.
House dust mites
House dust mites are tiny insects that feed on the dead flakes of human skin. They can be found in mattresses, carpets, soft furniture, pillows and beds.
Rhinitis isn’t caused by the dust mites themselves, but by a chemical found in their excrement. Dust mites are present all year round, although their numbers tend to peak during the winter.
Pollen and spores
Tiny particles of pollen produced by trees and grasses can sometimes cause allergic rhinitis. Most trees pollinate from early to mid-spring, whereas grasses pollinate at the end of spring and beginning of summer.
Rhinitis can also be caused by spores produced by mold and fungi.
Animals
Many people are allergic to animals, such as cats and dogs. The allergic reaction isn’t caused by animal fur, but flakes of dead animal skin and their urine and saliva.
Dogs and cats are the most common culprits, although some people are affected by horses, cattle, rabbits and rodents, such as guinea pigs and hamsters.
However, being around dogs from an early age can help protect against allergies, and there’s some evidence to suggest that this might also be the case with cats.
Some people are affected by allergens found in their work environment, such as wood dust, flour dust or latex.
Risk factors for developing hay fever
The following can increase your risk of developing hay fever:
- Having other allergies or asthma
- Having atopic dermatitis (eczema)
- Having a blood relative (such as a parent or sibling) with allergies or asthma
- Living or working in an environment that constantly exposes you to allergens — such as animal dander
- Having a mother who smoked during your first year of life
Complications of hay fever
Problems that may be associated with hay fever include:
- Reduced quality of life. Hay fever can interfere with your enjoyment of activities and cause you to be less productive. For many people, hay fever symptoms lead to absences from work or school.
- Poor sleep. Hay fever symptoms can keep you awake or make it hard to stay asleep, which can lead to fatigue and a general feeling of being unwell (malaise).
- Worsening asthma. Hay fever can worsen signs and symptoms of asthma, such as coughing and wheezing.
- Sinusitis. Prolonged sinus congestion due to hay fever may increase your susceptibility to sinusitis — an infection or inflammation of the membrane that lines the sinuses.
- Ear infection. In children, hay fever often is a factor in middle ear infection (otitis media).
Some people with allergic rhinitis also have asthma. Better control of allergic rhinitis has been shown to result in better asthma control in both adults and children. Emerging evidence shows that untreated allergic rhinitis can also increase the risk of developing asthma.
Nasal polyps
Nasal polyps are swellings that grow in the lining inside your nose or sinuses, the small cavities above and behind your nose.
They’re caused by inflammation of the membranes of the nose and sometimes develop as a result of rhinitis.
Nasal polyps are shaped like teardrops when they’re growing and look like a grape on a stem when fully grown.
They vary in size and can be yellow, grey or pink. They can grow on their own or in clusters, and usually affect both nostrils.
If nasal polyps grow large enough, or in clusters, they can interfere with your breathing, reduce your sense of smell and block your sinuses, which can lead to sinusitis.
Small nasal polyps can be shrunk using steroid nasal sprays so they don’t cause an obstruction in your nose. Large polyps may need to be surgically removed.
Sinusitis
Sinusitis is a common complication of allergic rhinitis. It’s where the sinuses become inflamed or infected.
The sinuses naturally produce mucus, which usually drains into your nose through small channels.
However, if the drainage channels are inflamed or blocked – for example, because of allergic rhinitis or nasal polyps – the mucus can’t drain away and it may become infected.
Sinusitis is common and usually clears up on its own within 2 to 3 weeks. But medicines can help if it’s taking a long time to go away.
Common symptoms of sinusitis include:
- a blocked nose, making it difficult to breathe through your nose
- a runny nose
- mucus that drips from the back of your nose down your throat (post-nasal drip)
- a reduced sense of smell or taste
- a feeling of fullness, pressure or pain in the face
- snoring
- obstructive sleep apnea (OSA) – your airways become temporarily blocked while you’re asleep, which can disturb your sleep
Over-the-counter painkillers, such as paracetamol, ibuprofen or aspirin, can be used to help reduce any pain and discomfort in your face.
However, these medications aren’t suitable for everyone, so check the leaflet that comes with them before using them.
For example, children under the age of 16 shouldn’t take aspirin, and ibuprofen isn’t recommended for people with asthma or a history of stomach ulcers. Speak to your doctor or pharmacist if you’re unsure.
Antibiotics may also be recommended if your sinuses become infected with bacteria. If you have long-term (chronic) sinusitis, surgery may be needed to improve the drainage of your sinuses.
Sinusitis treatment
How you can treat sinusitis yourself
You can often treat mild sinusitis without seeing a doctor by:
- getting plenty of rest
- drinking plenty of fluids
- taking painkillers, such as paracetamol or ibuprofen – don’t give aspirin to children under 16
- holding a warm clean flannel over your face for a few minutes several times a day
- inhaling steam from a bowl of hot water – don’t let children do this because of the risk of scalding
- cleaning your nose with a salt water solution to ease congestion
How to clean your nose with a salt water solution
- Boil a pint of water, then leave it to cool
- Mix a teaspoon of salt and a teaspoon of bicarbonate of soda into the water
- Wash your hands
- Stand over a sink, cup the palm of one hand and pour a small amount of the solution into it
- Sniff the water into one nostril at a time
- Repeat these steps until your nose feels more comfortable
You don’t need to use all of the solution, but use a fresh one each day.
A pharmacist can advise you about medicines that can help, such as:
- decongestant nasal sprays, drops or tablets to unblock your nose
- salt water nasal sprays or solutions to rinse out the inside of your nose
You can buy nasal sprays without a prescription, but they shouldn’t be used for more than a week.
Some decongestant tablets also contain paracetamol or ibuprofen. If you’re taking painkillers as well as a decongestant, be careful not to take more than the recommended dose.
Treatment from a doctor
Your doctor may be able to recommend other medicines to help with your symptoms, such as:
- steroid nasal sprays or drops – to reduce the swelling in your sinuses
- antihistamines – if an allergy is causing your symptoms
- antibiotics – if a bacterial infection is causing your symptoms and you’re very unwell or at risk of complications (more rare)
You might need to take steroid nasal sprays or drops for a few months. They sometimes cause irritation, sore throats or nosebleeds.
Your doctor may refer you to an ear, nose and throat (ENT) specialist if:
- these medicines don’t help with your sinusitis
- your sinusitis has lasted longer than 3 months (chronic sinusitis)
- you keep getting sinusitis
They may also recommend surgery in some cases.
Surgery for sinusitis
Surgery to treat chronic sinusitis is called functional endoscopic sinus surgery.
Functional endoscopic sinus surgery is carried out under general anaesthetic (where you’re asleep).
The surgeon can widen your sinuses by either:
- removing some of the blocked skin tissue
- inflating a tiny balloon in the blocked sinuses, then removing it
You should be able to have functional endoscopic sinus surgery within 18 weeks of your doctor appointment.
Middle ear infections
Middle ear infections (otitis media) can also develop as a complication of nasal problems, including allergic rhinitis.
These infections can occur if rhinitis causes a problem with the Eustachian tube, which connects the back of the nose and middle ear, at the back of the nose.
If this tube doesn’t function properly, fluid can build up in the middle ear behind the ear drum and can become infected.
There’s also the possibility of infection at the back of the nose spreading to the ear through the Eustachian tube.
The main symptoms of a middle ear infection usually start quickly and include:
- pain inside the ear
- a high temperature of 100.4 °F (38 °C) or above
- being sick
- a lack of energy
- difficulty hearing
- discharge running out of the ear
- feeling of pressure or fullness inside the ear
- itching and irritation in and around the ear
- scaly skin in and around the ear
Young children and babies with a middle ear infection may also:
- rub or pull their ear
- not react to some sounds
- be irritable or restless
- be off their food
- keep losing their balance
Most middle ear infections clear up within 3 days, although sometimes symptoms can last up to a week, but paracetamol (acetaminophen) or ibuprofen can be used to help relieve fever and pain. Antibiotics may also be prescribed if the symptoms persist or are particularly severe.
Middle ear infection treatment
If your child is older than 6 months of age and only has mild symptoms, the best treatment is to let the fluid go away on its own. You can give your child an over-the-counter pain reliever, such as acetaminophen, (one brand: Children’s Tylenol) if he or she is uncomfortable. A warm, moist cloth placed over the ear may also help.
Usually the fluid goes away in 2 to 3 months, and hearing returns to normal. Your doctor may want to check your child again at some point to see if fluid is still present. If it is, he or she may give your child antibiotics.
One treatment your doctor may suggest is a nasal balloon. A nasal balloon can help clear the fluid from the middle ear. You can easily use a nasal balloon at home. Your child will simply insert the balloon nozzle in one nostril while blocking the other nostril with a finger. Then, he or she will inflate the balloon with their nose.
If the fluid does not go away after a certain amount of time and treatment, your child may need ear tubes. These small tubes are inserted through the ear drum. They allow the doctor to suction out the fluid behind the ear. They also allow air to get into the middle ear, which helps prevent fluid build-up. Any hearing loss experienced by your child should be restored after the fluid is drained.
How to treat a middle ear infection yourself
To help relieve any pain and discomfort from a middle ear infection:
DO
- use painkillers such as paracetamol or ibuprofen (children under 16 shouldn’t take aspirin)
- place a warm or cold flannel on the ear
DON’T
- put anything inside your ear to remove earwax, such as cotton buds or your finger
- let water or shampoo get in your ear
- use decongestants or antihistamines – there’s no evidence they help with ear infections
FDA Warning
The. U.S. Food and Drug Administration (FDA) advise against the use of ear candles. Ear candles can cause serious injuries and there is no evidence to support their effectiveness 2.
Treatment from a doctor
Your doctor may prescribe medicine for your ear infection, depending on what’s caused it.
Antibiotics aren’t usually offered because middle ear infections often clear up on their own, and antibiotics make little difference to symptoms, including pain.
Antibiotics might be prescribed if:
- an ear infection doesn’t start to get better after 3 days
- you or your child has any fluid coming out of their ear
- you or your child has an illness that means there’s a risk of complications, such as cystic fibrosis
They may also be prescribed if your child is less than 2 years old and has an infection in both ears.
Prevention of hay fever
There’s no way to avoid getting hay fever. If you have hay fever, the best thing to do is to lessen your exposure to the allergens that cause your symptoms. Take allergy medications before you’re exposed to allergens, as directed by your doctor.
You can help your symptoms by avoiding the things that you are allergic, including:
- Keeping windows closed. This is especially important during high-pollen seasons.
- Washing your hands after petting animals.
- Using dust- and mite-proof bedding and mattress covers.
- Wearing glasses outside to protect your eyes.
- Showering before bed to wash off allergens from hair and skin.
You can also avoid things that can make your symptoms worse, such as:
- aerosol sprays
- air pollution
- cold temperatures
- humidity
- irritating fumes
- tobacco smoke
- wind
- wood smoke.
House dust mites
Dust mites are one of the biggest causes of allergies. They’re microscopic insects that breed in household dust.
To help limit the number of mites in your house, you should:
- consider buying an air-permeable occlusive mattress and bedding covers – this type of bedding acts as a barrier to dust mites and their droppings
- choose wood or hard vinyl floor coverings instead of carpet
- fit roller blinds that can be easily wiped clean
- regularly clean cushions, soft toys, curtains and upholstered furniture, either by washing or vacuuming them
- use synthetic pillows and acrylic duvets instead of woollen blankets or feather bedding
- use a vacuum cleaner fitted with a high efficiency particulate air (HEPA) filter – it can remove more dust than ordinary vacuum cleaners
- use a clean damp cloth to wipe surfaces – dry dusting can spread allergens further
Concentrate your efforts on controlling dust mites in the areas of your home where you spend most time, such as the bedroom and living room.
Pets
It isn’t pet fur that causes an allergic reaction, but exposure to flakes of their dead skin, saliva and dried urine.
If you can’t permanently remove a pet from the house, you may find the following tips useful:
- keep pets outside as much as possible or limit them to one room, preferably one without carpet
- don’t allow pets in bedrooms
- wash pets at least once a fortnight
- groom dogs regularly outside
- regularly wash bedding and soft furnishings your pet has been on
If you’re visiting a friend or relative with a pet, ask them not to dust or vacuum on the day you’re visiting because it will disturb allergens into the air.
Taking an antihistamine medicine one hour before you enter a house with a pet can help reduce your symptoms.
Pollen
Different plants and trees pollinate at different times of the year, so when you get allergic rhinitis will depend on what sort of pollen(s) you’re allergic to.
Most people are affected during the spring and summer months because this is when most trees and plants pollinate.
To avoid exposure to pollen, you may find the following tips useful:
- check weather reports for the pollen count and stay indoors when it’s high
- avoid line-drying clothes and bedding when the pollen count is high
- wear wraparound sunglasses to protect your eyes from pollen
- keep doors and windows shut during mid-morning and early evening, when there’s most pollen in the air
- shower, wash your hair and change your clothes after being outside
- avoid grassy areas, such as parks and fields, when possible
- if you have a lawn, consider asking someone else to cut the grass for you
Mold spores
Molds can grow on any decaying matter, both in and outside the house. The molds themselves aren’t allergens, but the spores they release are.
Spores are released when there’s a sudden rise in temperature in a moist environment, such as when central heating is turned on in a damp house or wet clothes are dried next to a fireplace.
To help prevent mold spores, you should:
- keep your home dry and well ventilated
- when showering or cooking, open windows but keep internal doors closed to prevent damp air spreading through the house, and use extractor fans
- avoid drying clothes indoors, storing clothes in damp cupboards and packing clothes too tightly in wardrobes
- deal with any damp and condensation in your home.
Hay fever symptoms
They vary depending on how bad your allergies are.
Symptoms of hay fever include:
- Sneezing and coughing
- A runny or blocked nose
- Itchy, red, swollen or watery eyes
- Itchy throat, mouth, nose and ears
- Loss of smell
- Pain around your temples and forehead
- Headache
- Earache
- Feeling tired
- Dark circles under your eyes
- Sore throat
If you have asthma, you might also:
- have a tight feeling in your chest
- be short of breath
- wheeze and cough
Hay fever will last for weeks or months, unlike a cold, which usually goes away after 1 to 2 weeks.
Hay fever season
Your hay fever signs and symptoms may start or worsen at a particular time of year. Triggers include:
- Tree pollen, which is common in early spring.
- Grass pollen, which is common in late spring and summer.
- Ragweed pollen, which is common in fall.
- Dust mites, cockroaches and dander from pets can occur year-round (perennial). Symptoms to indoor allergens might worsen in winter, when houses are closed up.
- Spoors from indoor and outdoor fungi and molds are considered both seasonal and perennial.
Hay fever diagnosis
If your symptoms interfere with your daily life, see your family doctor. Your doctor will ask you questions about your symptoms and medical history and perform a physical exam. Keeping a record of your symptoms over a period of time can help your doctor determine what triggers your allergies.
Your doctor may want to do an allergy skin test to help determine exactly what you are allergic to. During an allergy skin test, tiny amounts of allergens are applied to your skin. Your doctor will observe and record the way your skin reacts to each allergen.
Your doctor may also decide to do a blood test, such as the radioallergosorbent test (RAST). This test identifies antibodies in your blood that determine what you’re allergic to. Once your allergens are identified, you and your doctor can decide the best treatment.
Your doctor will possibly recommend one or both of the following tests:
- Skin prick test – where the allergen is placed on your arm and the surface of the skin is pricked with a needle to introduce the allergen to your immune system; if you’re allergic to the substance, a small itchy spot (welt or bump) will appear. Allergy specialists usually are best equipped to perform allergy skin tests.
- Blood test also called the radioallergosorbent test (RAST) – to check for the immunoglobulin E (IgE) antibody in your blood; your immune system produces this antibody in response to a suspected allergen.
Commercial allergy testing kits aren’t recommended because the testing is often of a lower standard than that provided by the allergy specialist or an accredited private clinic.
It’s also important that the test results are interpreted by a qualified healthcare professional with detailed knowledge of your symptoms and medical history.
Further tests
In some cases further hospital tests may be needed to check for complications, such as nasal polyps or sinusitis.
For example, you may need:
- a nasal endoscopy – where a thin tube with a light source and video camera at one end (endoscope) is inserted up your nose so your doctor can see inside your nose
- a nasal inspiratory flow test – where a small device is placed over your mouth and nose to measure the air flow when you inhale through your nose
- a computerized tomography (CT) scan – a scan that uses X-rays and a computer to create detailed images of the inside of the body.
Hay fever treatment
There’s currently no cure for hay fever and you can’t prevent it. But you can do things to ease your symptoms when the pollen count is high.
It’s best to limit your exposure to substances that cause your hay fever as much as possible. If your hay fever isn’t too severe, over-the-counter medications may be enough to relieve symptoms. For worse symptoms, you may need prescription medications.
Many people get the best relief from a combination of allergy medications. You might need to try a few before you find what works best.
If your child has hay fever, talk with your doctor about treatment. Not all medications are approved for use in children. Read labels carefully.
In addition, hay fever and asthma appear to represent a combined airway inflammatory disease and, therefore, treatment of asthma is also an important consideration in patients with hay fever.
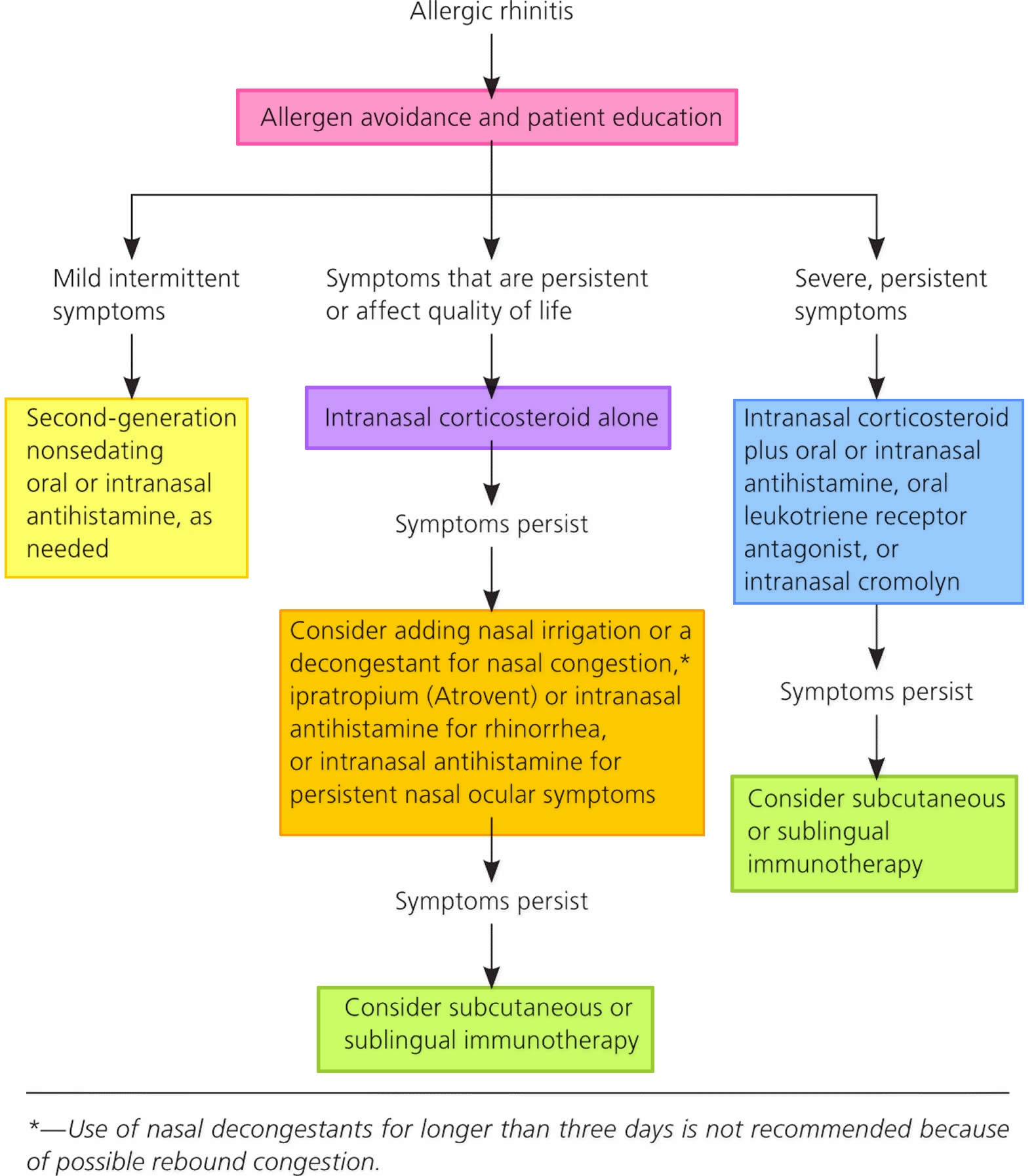
Figure 2. Hay fever treatment algorithm
Table 1. Pharmacotherapy and Immunotherapy for hay fever
| Type of Symptoms | Recommended Treatment Options |
|---|---|
| Episodic symptoms | Oral or nasal H1-antihistamine, with oral or nasal decongestant if needed |
| Mild symptoms, seasonal or perennial | Intranasal glucocorticoid,† oral or nasal H1-antihistamine, or leukotriene- receptor antagonist (e.g., montelukast) |
| Moderate-to-severe symptoms‡ | Intranasal glucocorticoid,§ intranasal glucocorticoid plus nasal H1-antihistamine, ¶ or allergen immunotherapy administered subcutaneously or sublingually (the latter for grass or ragweed only)∥ |
Footnotes:
*Common or severe adverse effects are as follows: for oral antihistamines, sedation and dry mouth (predominantly with older agents); for nasal antihistamines, bitter taste, sedation, and nasal irritation; for oral decongestants, palpitations, insomnia, jitteriness, and dry mouth; for nasal decongestants, rebound nasal congestion and the potential for severe central nervous system and cardiac side effects in small children; for leukotriene-receptor antagonists, bad dreams and irritability; for nasal glucocorticoids, nasal irritation, nosebleeds, and sore throat; for sublingual immunotherapy, oral pruritus and edema, systemic allergic reactions (epinephrine auto-injectors are advised per the package insert), and eosinophilic esophagitis; and for subcutaneous immunotherapy, local and systemic allergic reactions (therapy should be administered only in a setting where emergency treatment is available).
†Intranasal glucocorticoids are more efficacious than oral antihistamines or montelukast, but the difference may not be as evident if the symptoms are mild.
‡Moderate-to-severe allergic rhinitis is defined by the presence of one or more of the following: sleep disturbance, im- pairment of usual activities or exercise, impairment of school or work performance, or troublesome symptoms.
§An oral H1-antihistamine plus montelukast is an alternative for patients for whom nasal glucocorticoids are associated with unacceptable side effects or for those who do not wish to use them; the efficacy of this combination is not unequivo- cally inferior to that of an intranasal glucocorticoid.
¶This combination is more efficacious than an intranasal glucocorticoid alone.
∥Allergen immunotherapy should be used in patients who do not have adequate control with pharmacotherapy or who prefer allergen immunotherapy.
[Source 4 ]Hay fever medications
Medication won’t cure your allergy, but it can be used to treat the common symptoms.
If your symptoms are caused by seasonal allergens, such as pollen, you should be able to stop taking your medication after the risk of exposure has passed.
Visit your doctor if your symptoms don’t respond to medication after two weeks.
Intranasal corticosteroids
If you have frequent or persistent symptoms and you have a nasal blockage or nasal polyps, your doctor may recommend a nasal spray or drops containing corticosteroids. Intranasal corticosteroids are also first-line therapeutic options for patients with mild persistent or moderate/severe symptoms and they can be used alone or in combination with oral antihistamines. For many people intranasal corticosteroids are the most effective hay fever (allergic rhinitis) medications, and they’re often the first type of medication prescribed. Studies and meta-analyses have shown that intranasal corticosteroids are superior to antihistamines and leukotriene receptor antagonists in controlling the symptoms of hay fever, including nasal congestion, and rhinorrhea 5. Intranasal corticosteroids have also been shown to improve ocular symptoms and reduce lower airway symptoms in patients with concurrent asthma and hay fever 6.
Nasal corticosteroid sprays (e.g., Budesonide [Rhinocort], Mometasone furoate [Nasonex]) are the most effective treatment. Many brands are available. You can buy some brands without a prescription. For other brands, you need a prescription.
Nasal corticosteroids are a safe, long-term treatment for most people. Side effects can include an unpleasant smell or taste and nose irritation and stinging. These side effects can usually be prevented by aiming the spray slightly away from the nasal septum 7. Steroid side effects are rare. Evidence suggests that intranasal beclomethasone and triamcinolone, but not other intranasal corticosteroids, may slow growth in children compared to placebo. However, long-term studies examining the impact of usual doses of intranasal beclomethasone on growth are lacking 8.
- Nasal corticosteroid sprays work best when you use them every day.
- It may take 2 or more weeks of steady use for your symptoms to improve.
- Nasal corticosteroid sprays are safe for children and adults.
Corticosteroids help reduce inflammation and swelling. They take longer to work than antihistamines, but their effects last longer. Side effects from inhaled corticosteroids are rare, but can include nasal dryness, irritation and nosebleeds.
Intranasal corticosteroids are cheaper than antihistamines and provide better relief of nasal symptoms, however the two can be used together for optimal symptom control.
Combination intranasal corticosteroid and antihistamine nasal spray
If intranasal corticosteroids are not effective, a combination corticosteroid/antihistamine spray can be tried. Combination fluticasone propionate/azelastine hydrochloride (Dymista) is now available. This combination spray has been shown to be more effective than the individual components with a safety profile similar to intranasal corticosteroids 9.
Oral corticosteroids
Corticosteroid pills such as prednisone sometimes are used to relieve severe allergy symptoms. Because the long-term use of corticosteroids can cause serious side effects such as cataracts, osteoporosis and muscle weakness, they’re usually prescribed for only short periods of time.
If you have a particularly severe bout of symptoms and need rapid relief, your doctor may prescribe a short course of oral corticosteroid tablets such as prednisone lasting 5 to 10 days.
Antihistamines
Antihistamines (e.g., Cetirizine hydrochloride [Zyrtec], Fexofenadine hydrochloride [Telfast]) relieve symptoms of hay fever by blocking the action of a chemical called histamine, which the body releases when it thinks it’s under attack from an allergen.
Antihistamines are often used when symptoms do not occur very often or do not last very long.
- Antihistamines can be bought as a pill, capsule, or liquid without a prescription.
- Over-the-counter pills include loratadine (Claritin, Alavert), cetirizine (Zyrtec Allergy) and fexofenadine (Allegra Allergy).
- The prescription antihistamine nasal sprays azelastine (Astelin, Astepro) and olopatadine (Patanase) can relieve nasal symptoms.
- Antihistamine eyedrops such as ketotifen fumarate (Alaway) help relieve eye itchiness and eye irritation caused by hay fever.
- Older antihistamines can cause sleepiness. They may affect a child’s ability to learn and make it unsafe for adults to drive or use machinery.
- Newer antihistamines cause little or no sleepiness or learning problems.
- Antihistamine nasal sprays work well for treating hay fever. They are only available with a prescription.
You can buy antihistamine tablets over the counter from your pharmacist without a prescription, but antihistamine nasal sprays are only available with a prescription.
Antihistamines can sometimes cause drowsiness. If you’re taking them for the first time, see how you react to them before driving or operating heavy machinery. In particular, antihistamines can cause drowsiness if you drink alcohol while taking them.
Intranasal antihistamines
Histamine is the most studied mediator in early allergic response. Histamine causes smooth muscle constriction, mucus secretion, vascular permeability, and sensory nerve stimulation, resulting in the symptoms of hay fever.
Compared with oral antihistamines, intranasal antihistamines have the advantage of delivering a higher concentration of medication to a targeted area, resulting in fewer adverse effects and an onset of action within 15 minutes 10. Intranasal antihistamines FDA-approved for the treatment of hay fever are azelastine (Astelin; for patients five years and older) and olopatadine (Patanol; for patients six years and older). They have been shown to be similar or superior to oral antihistamines in treating symptoms of conjunctivitis and rhinitis, and may improve congestion 11. Adverse effects include a bitter aftertaste, headache, nasal irritation, epistaxis, and sedation. Although intranasal antihistamines are an option if symptoms do not improve with nonsedating oral antihistamines, their use as first- or second-line therapy is limited by adverse effects, twice daily dosing, cost, and decreased effectiveness compared with intranasal corticosteroids 11.
Oral antihistamines
First-generation antihistamines, including brompheniramine, chlorpheniramine, clemastine, and diphenhydramine (Benadryl), may cause sedation, fatigue, and impaired mental status. These adverse effects occur because the older antihistamines are more lipid soluble and more readily cross the blood-brain barrier than second-generation antihistamines. The use of first-generation sedating antihistamines has been associated with poor school performance, impaired driving, and increased automobile collisions and work injuries 12.
Compared with first-generation antihistamines, second-generation drugs have a better adverse effect profile and cause less sedation, with the exception of cetirizine (Zyrtec) 13. Second-generation nonsedating oral antihistamines include loratadine (Claritin), desloratadine (Clarinex), levocetirizine (Xyzal), and fexofenadine (Allegra). Second-generation antihistamines have more complex chemical structures that decrease their movement across the blood-brain barrier, reducing central nervous system adverse effects such as sedation. Although cetirizine is generally classified as a second-generation antihistamine and a more potent histamine antagonist, it does not have the benefit of decreased sedation.
In general, oral antihistamines have been shown to effectively relieve the histamine-mediated symptoms associated with hay fever (e.g., sneezing, pruritus, rhinorrhea), but they are less effective than intranasal corticosteroids at treating nasal congestion and ocular symptoms. Because their onset of action is typically within 15 to 30 minutes and they are considered safe for children older than two years, second-generation antihistamines are useful for many patients with mild symptoms requiring as-needed treatment 14.
Decongestants
Oral and intranasal decongestants (e.g., Phenylephrine hydrochloride [Sudafed], oxymetazoline [Afrin] and pseudoephedrine) are medicines that help dry up a runny or stuffy nose associated with hay fever by acting on adrenergic receptors, which causes vasoconstriction in the nasal mucosa, decreasing inflammation 15, 10. Decongestants come as pills, liquids, capsules, or nasal sprays. You can buy them over-the-counter (OTC), without a prescription. Over-the-counter oral decongestants include pseudoephedrine (Sudafed, Afrinol, others). Nasal sprays include phenylephrine hydrochloride (Neo-Synephrine) and oxymetazoline (Afrin).
Oral decongestants can cause a number of side effects, including increased blood pressure, elevated intraocular pressure, insomnia, irritability, tremor, urinary retention, dizziness, tachycardia, and headache; therefore, these medications should be used with caution in patients with underlying cardiovascular conditions, glaucoma, or hyperthyroidism 10. Common adverse effects of intranasal decongestants are sneezing and nasal dryness.
- Decongestants may be considered for short-term use in patients without improvement in congestion with intranasal corticosteroids 16.
- You can use decongestants along with antihistamine pills or liquids.
- DO NOT use nasal spray decongestants for more than 3 days in a row because it can actually worsen symptoms when used continuously (rebound congestion or rhinitis medicamentosa) 16.
- The abuse potential for pseudoephedrine should be weighed against its benefits.
- Talk to your child’s health care provider before giving decongestants to your child.
Eye drops
Eye drops containing anti-histamine or steroids may be used to control symptoms such as itchy or watery eyes e.g., Ketotifen fumarate (Zaditen), Hydrocortisone acetate (Hycor).
Leukotriene modifier (leukotriene receptor antagonists)
Montelukast and zafirlukast is a prescription tablet taken to block the action of leukotrienes — immune system chemicals that cause allergy symptoms such as excess mucus production, however, they do not appear to be as effective as intranasal corticosteroids 17. They’re especially effective in treating allergy-induced asthma. Leukotriene receptor antagonist is often used when nasal sprays can’t be tolerated or for mild asthma.
Montelukast can cause headaches. In rare cases, it has been linked to psychological reactions such as agitation, aggression, hallucinations, depression and suicidal thinking. Seek medical advice right away for any unusual psychological reaction.
Cromolyn sodium
Intranasal sodium cromoglycate (Cromolyn) is available as an over-the-counter nasal spray that must be used several times a day. It’s also available in eye-drop form with a prescription. It helps relieve hay fever symptoms by preventing the release of histamine 1. Intranasal sodium cromoglycate (Cromolyn) has been shown to reduce sneezing, rhinorrhea and nasal itching and is, therefore, a reasonable therapeutic option for some patients. Most effective when you start using it before you have symptoms. Although safe for general use, it is not considered first-line therapy for hay fever because it is less effective than antihistamines and intranasal corticosteroids and is given three or four times daily 18.
Nasal ipratropium
Available in a prescription nasal spray, intranasal ipratropium (Atrovent) helps relieve severe runny nose (severe rhinorrhea) by preventing the glands in your nose from producing excess fluid. The recommended administration is two to three times daily 1. Intranasal ipratropium (Atrovent) is not effective for treating congestion, sneezing or postnasal drip than intranasal corticosteroids 19.
Mild side effects include nasal dryness, nosebleeds, sore throat and headache. Rarely, it can cause more-severe side effects, such as blurred vision, dizziness and difficult urination. The drug is not recommended for people with glaucoma or men with an enlarged prostate.
Add-on treatments
If your hay fever doesn’t respond to treatment, your doctor may choose to add to your original treatment.
Your doctor may suggest:
- increasing the dose of your corticosteroid nasal spray
- using a short-term course of a decongestant nasal spray to take with your other medication
- combining antihistamine tablets with corticosteroid nasal sprays, and possibly decongestants
- using a nasal spray that contains a medicine called ipratropium, which will help reduce excessive nasal discharge
- using a leukotriene receptor antagonist medication – medication that blocks the effects of chemicals called leukotrienes, which are released during an allergic reaction
If you don’t respond to the add-on treatments, you may be referred to a specialist for further assessment and treatment.
Allergen immunotherapy
Immunotherapy also known as hyposensitisation, desensitisation or allergy shot, is another type of treatment used for some allergies. Allergen immunotherapy is only suitable for people with certain types of allergies, such as hay fever, and is usually only considered if your symptoms are severe. Immunotherapy involves gradually introducing more and more of the allergen into your body to make your immune system less sensitive to it. The allergen is often injected under the skin of your upper arm. Injections are given at weekly intervals, with a slightly increased dose each time.
Immunotherapy can also be carried out using tablets that contain an allergen, such as grass pollen, which are placed under your tongue.
When a dose is reached that’s effective in reducing your allergic reaction (the maintenance dose), you’ll need to continue with the injections or tablets for up to three years.
Immunotherapy should only be carried out under the close supervision of a specially trained doctor as there’s a risk it may cause a serious allergic reaction.
The appropriate use, timing of initiation, and duration of immunotherapy remain uncertain. The general recommendation in the United States has been to start immunotherapy only for patients in whom symptom control is not adequate with pharmacotherapy or those who prefer immunotherapy to pharmacotherapy 20. However, the Preventive Allergy Treatment Study, in which children with hay fever but without asthma were randomly assigned to subcutaneous immunotherapy or a pharmacotherapy control, showed that fewer children had new allergies or asthma after 3 years of immunotherapy, and this preventive effect persisted 7 years after therapy was discontinued 21. A similar large trial using sublingual immunotherapy is ongoing 22.
With subcutaneous immunotherapy, the standard practice in the United States is to administer multiple allergens (on average, eight allergens simultaneously in a single injection or multiple injections) because most patients are sensitized and symptomatic on exposure to multiple allergens. It is not known whether multi-allergen therapy results in better outcomes than single-allergen therapy. Although some older studies suggest a benefit of multi-allergen immunotherapy, most trials showing the efficacy of immunotherapy involve a single allergen.
The role of allergen avoidance in the prevention of hay fever is controversial. Avoidance of seasonal inhalant allergens is universally recommended on the basis of empirical evidence, but the efficacy of strategies to avoid exposure to perennial allergens, including dust mites, pest allergens (cockroach and mouse), and molds, has been questioned. For abatement strategies to be successful, allergens need to be reduced to very low levels, which are difficult to achieve. Abatement usually requires a multifaceted and continuous approach, raising feasibility problems. Multifaceted programs have been effective in the management of asthma but have not been studied in hay fever.
Hay fever home remedies
It’s not possible to completely avoid allergens, but you can reduce your symptoms by limiting your exposure to them. If you know what you’re allergic to, you can avoid your triggers.
Use over-the-counter hay fever medicines:
- antihistamines may ease mild symptoms
- a steroid nasal spray may ease a blocked or runny nose
- eye drops may help relieve itchy or watery eyes.
Pollen or molds
- Close doors and windows during pollen season.
- Don’t hang laundry outside — pollen can stick to sheets and towels.
- Shower and change your clothes after you’ve been outside to wash pollen off.
- Wash your hands, then bathe your eyes with cold water if they are itchy or sore
- Avoid smoking or breathing in other people’s smoke, as it can make symptoms worse – see our other article on quitting smoking,
- Use air conditioning in your house and car.
- Use an allergy-grade filter in your home ventilation system and change it regularly.
- Avoid outdoor activity in the early morning, when pollen counts are highest.
- Stay indoors on dry, windy days.
- Use a dehumidifier to reduce indoor humidity.
- Use a high-efficiency particulate air (HEPA) filter in your bedroom and other rooms where you spend a lot of time.
- Avoid mowing the lawn or raking leaves.
- Wear a dust mask when cleaning house or gardening.
- Wear wraparound sunglasses to stop pollen getting into your eyes
- Put Vaseline around your nostrils to trap pollen
Dust mites
- Use allergy-proof covers on mattresses, box springs and pillows.
- Wash sheets and blankets in water heated to at least 130 F (54 C).
- Use a dehumidifier or air conditioner to reduce indoor humidity.
- Vacuum carpets weekly with a vacuum cleaner equipped with a small-particle or HEPA filter.
- Spray insecticide designed to kill dust mites (acaricides) and approved for indoor use on carpets, furniture and bedding.
- Consider removing carpeting, especially where you sleep, if you’re highly sensitive to dust mites.
Cockroaches
- Block cracks and crevices where roaches can enter.
- Fix leaky faucets and pipes.
- Wash dishes and empty garbage daily.
- Sweep food crumbs from counters and floors.
- Store food, including pet food, in sealed containers.
- Consider professional pest extermination.
Pet dander
- Keep pets out of your home, if possible.
- Bathe dogs twice a week, if possible. The benefit of bathing cats hasn’t been proven.
- Keep pets out of the bedroom and off furniture.
Hay fever prognosis
The belief is that the prevalence of hay fever peaks in adolescence and gradually decreases with advancing age 23. In a longitudinal study, at the time of the 23-year follow-up, 54.9% of patients showed improvement in symptoms, with 41.6% of those being symptom-free 24. Patients who had an onset of symptoms at a younger age were more likely to show improvement. The severity of hay fever can vary over time and depends on various factors such as location and season 24. Approximately 50% of patients receiving grass allergy immunotherapy noted improvement in symptoms that continued 3 years after discontinuation of therapy 25.
References- Nelson HS, Rachelefsky GS, Bernick J. The Allergy Report. Milwaukee, Wis.: American Academy of Allergy, Asthma, and Immunology; 2000.
- Don’t Get Burned: Stay Away From Ear Candles. https://www.fda.gov/ForConsumers/ConsumerUpdates/ucm200277.htm
- Sur DK, Scandale S. Treatment of allergic rhinitis. Am Fam Physician. 2010;81(12):1440–1446. https://www.aafp.org/afp/2010/0615/p1440.html
- Wheatley LM, Togias A. Allergic Rhinitis. The New England journal of medicine. 2015;372(5):456-463. doi:10.1056/NEJMcp1412282. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4324099/
- Wilson AM, O’Byrne PM, Parameswaran K. Leukotriene receptor antagonists for allergic rhinitis: a systematic review and meta-analysis. Am J Med. 2004;116(5):338–344. doi: 10.1016/j.amjmed.2003.10.030
- Bernstein DI, Levy AL, Hampel FC, Baidoo CA, Cook CK, Philpot EE, Rickard KA. Treatment with intranasal fluticasone propionate significantly improves ocular symptoms in patients with seasonal allergic rhinitis. Clin Exp Allergy. 2004;34(6):952–957. doi: 10.1111/j.1365-2222.2004.01952.x
- Small P, Frenkiel S, Becker A, Boisvert P, Bouchard J, Carr S, Cockcroft D, Denburg J, Desrosiers M, Gall R, Hamid Q, Hébert J, Javer A, Keith P, Kim H, Lavigne F, Lemièr C, Massoud E, Payton K, Schellenberg B, Sussman G, Tannenbaum D, Watson W, Witterick I, Wright E, The Canadian Rhinitis Working Group Rhinitis: a practical and comprehensive approach to assessment and therapy. J Otolaryngol. 2007;36(Suppl 1):S5–S27. doi: 10.2310/7070.2006.X002
- Allen DB, Meltzer EO, Lemanske RF Jr, Philpot EE, Faris MA, Kral KM, Prillaman BA, Rickard KA. No growth suppression in children treated with the maximum recommended dose of fluticasone propionate aqueous nasal spray for one year. Allergy Asthma Proc. 2002 Nov-Dec;23(6):407-13.
- Berger WE, Shah S, Lieberman P, Hadley J, Price D, Munzel U, Bhatia S. Long-term, randomized safety study of MP29-02 (a novel intranasal formulation of azelastine hydrochloride and fluticasone propionate in an advanced delivery system) in subjects with chronic rhinitis. J Allergy Clin Immunol Pract. 2014;2(2):179–185. doi: 10.1016/j.jaip.2013.09.019
- Brozek JL, Bousquet J, Baena-Cagnani CE, et al.; Global Allergy and Asthma European Network; Grading of Recommendations Assessment, Development and Evaluation Working Group. Allergic rhinitis and its impact on asthma (ARIA) guidelines: 2010 revision. J Allergy Clin Immunol. 2010;126(3):466–476.
- Tran NP, Vickery J, Blaiss MS. Management of rhinitis: allergic and non-allergic. Allergy Asthma Immunol Res. 2011;3(3):148–156.
- Robb G, Sultana S, Ameratunga S, Jackson R. A systematic review of epidemiological studies investigating risk factors for work-related road traffic crashes and injuries. Inj Prev. 2008;14(1):51–58.
- Bender BG, Berning S, Dudden R, Milgrom H, Tran ZV. Sedation and performance impairment of diphenhydramine and second-generation antihistamines: a meta-analysis. J Allergy Clin Immunol. 2003;111(4):770–776.
- Barr JG, Al-Reefy H, Fox AT, Hopkins C. Allergic rhinitis in children [published correction appears in BMJ. 2014;349:4923]. BMJ. 2014;349:g4153.
- Scadding GK, Durham SR, Mirakian R, et al.; British Society for Allergy and Clinical Immunology. BSACI guidelines for the management of allergic and non-allergic rhinitis. Clin Exp Allergy. 2008;38(1):19–42.
- Seidman MD, Gurgel RK, Lin SY, et al. Clinical practice guideline: allergic rhinitis executive summary. Otolaryngol Head Neck Surg. 2015;152(2):197–206.
- Ratner PH, Howland WC, 3rd, Arastu R, Philpot EE, Klein KC, Baidoo CA, Faris MA, Rickard KA. Fluticasone propionate aqueous nasal spray provided significantly greater improvement in daytime and nighttime nasal symptoms of seasonal allergic rhinitis compared with montelukast. Ann Allergy Asthma Immunol. 2003;90(5):536–542. doi: 10.1016/S1081-1206(10)61847-9
- Jurado-Palomo J, Bobolea ID, Belver, González MT, et al. Treatment of allergic rhinitis: ARIA document, nasal lavage, antihistamines, cromones and vasoconstrictors. In: Gendeh BS, ed. Otolaryngology. New York, NY: InTech; 2012:61–82.
- Milgrom H, Biondi R, Georgitis JW, et al. Comparison of ipratropium bromide 0.03% with beclomethasone dipropionate in the treatment of perennial rhinitis in children. Ann Allergy Asthma Immunol. 1999;83(2):105–111.
- The diagnosis and management of rhinitis: an updated practice parameter. Wallace DV, Dykewicz MS, Bernstein DI, Blessing-Moore J, Cox L, Khan DA, Lang DM, Nicklas RA, Oppenheimer J, Portnoy JM, Randolph CC, Schuller D, Spector SL, Tilles SA, Joint Task Force on Practice., American Academy of Allergy., Asthma & Immunology., American College of Allergy., Asthma and Immunology., Joint Council of Allergy, Asthma and Immunology. J Allergy Clin Immunol. 2008 Aug; 122(2 Suppl):S1-84. https://www.jacionline.org/article/S0091-6749(08)01123-8/fulltext
- Jacobsen L, Niggemann B, Dreborg S, et al. Specific immunotherapy has long-term preventive effect of seasonal and perennial asthma: 10-year follow-up on the PAT study. Allergy. 2007;62:943–8
- https://clinicaltrials.gov/ct2/show/results/NCT01061203
- Akhouri S, House SA. Allergic Rhinitis. [Updated 2021 Mar 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538186
- Greisner WA 3rd, Settipane RJ, Settipane GA. Natural history of hay fever: a 23-year follow-up of college students. Allergy Asthma Proc. 1998 Sep-Oct;19(5):271-5. doi: 10.2500/108854198778557728
- Durham SR, Emminger W, Kapp A, Colombo G, de Monchy JG, Rak S, Scadding GK, Andersen JS, Riis B, Dahl R. Long-term clinical efficacy in grass pollen-induced rhinoconjunctivitis after treatment with SQ-standardized grass allergy immunotherapy tablet. J Allergy Clin Immunol. 2010 Jan;125(1):131-8.e1-7. doi: 10.1016/j.jaci.2009.10.035