What is a hematoma
A hematoma is a localized collection or pooling of blood in the tissues outside of the blood vessels and it can form virtually anywhere in your body. A hematoma most often form secondary to trauma or surgery but spontaneous hematoma formation is also not uncommon, especially in those with bleeding disorders or on anticoagulant therapy.
Normally, if you get hurt, your body forms a blood clot to stop the bleeding. A hematoma happens when an injury causes blood to collect and pool under the skin. The pooling blood gives the skin a spongy, rubbery, lumpy feel. For blood to clot, your body needs cells called platelets and proteins known as clotting factors. If you have a bleeding disorder, you either do not have enough platelets or clotting factors or they don’t work the way they should.
Bleeding disorders can be the result of other diseases, such as severe liver disease or a lack of vitamin K. They can also be inherited. Hemophilia is an inherited bleeding disorder. Bleeding disorders can also be a side effect of medicines such as blood thinners. Various blood tests can check for a bleeding disorder. You will also have a physical exam and history. Treatments depend on the cause. They may include medicines and transfusions of blood, platelets, or clotting factor.
A hematoma usually is not a cause for concern. A hematoma is not the same thing as a blood clot in a vein (known as deep vein thrombosis or DVT), and it does not cause blood clots.
Follow-up care is a key part of your treatment and safety. Be sure to make and go to all appointments, and call your doctor or nurse call line if you are having problems. It’s also a good idea to know your test results and keep a list of the medicines you take.
Hematomas may be hyperacute to chronic in duration and therefore their internal contents will vary from fresh bleeding to chronic hemoglobin degradation products (e.g. hemosiderin and ferritin) and are often a mixture of different aged components. The physical consistency of the collection may also vary from a hyperacute purely liquid collection to a chronic solidified mass-like state, but often a mixed cystic-solid state.
Hematomas are usually sterile when first formed and the majority remain uninfected. However, superinfection is seen forming a hemorrhagic abscess and is one of the well-recognized complications of draining a hematoma.
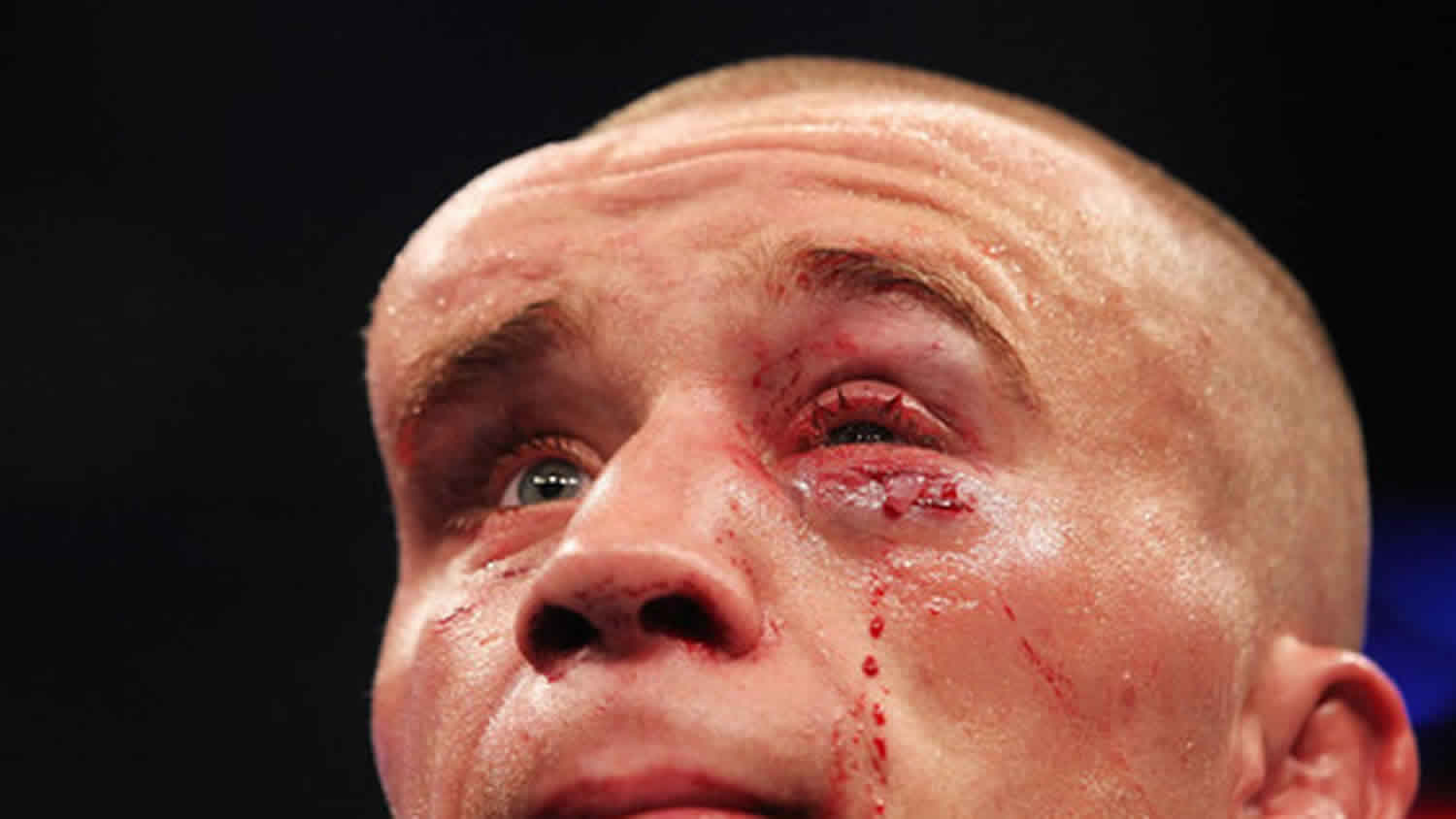
Hematoma vs bruise
A bruise is bleeding under the skin or a collection of blood underneath the skin that is caused by trauma to an area of the body. The trauma causes tiny blood vessels, called capillaries, to break, and then blood leaks from the vessels into the surrounding tissue. Sometimes, enough bleeding occurs so that a lump also forms (this lump is called a hematoma).
A bruise will usually heal on its own. Some general guidelines for treatment may include:
- A cold or ice pack for the first 24 hours after injury may help reduce swelling and discomfort. Never apply ice directly to the skin. Place a towel between the ice and your skin. After one to two days, warm soaks or a warm bath may help the area feel better.
- If the bruise or swelling is on the lips or in the mouth, offer your child an ice cube or ice pop to suck on.
- Avoid putting more pressure on the bruised area or massaging it.
- If the bruise involves a large area on an arm or leg, elevate the limb to help reduce swelling.
When should you see a doctor?
Specific treatment for bruises that require more than minor treatment at home will be determined by your doctor. In general, see your doctor if you:
- Bruise often or have recurring bruises without known trauma or cause
- Have increased pain or swelling
- Are unable to move a joint
- May have broken a bone
- Have injured or bruised an eye
- Have injured or bruised the neck or is having difficulty breathing
See your doctor or seek immediate medical care if:
- You have signs of skin infection, such as:
- Increased pain, swelling, warmth, or redness.
- Red streaks leading from the area.
- Pus draining from the area.
- A fever.
Watch closely for changes in your health, and be sure to contact your doctor if:
- The bruise lasts longer than 4 weeks.
- The bruise gets bigger or becomes more painful.
- You do not get better as expected.
How to treat a hematoma
How can you care for yourself at home:
- Rest and protect the injured area.
- Put ice or a cold pack on the area for 10 to 20 minutes at a time.
- Prop up the bruised area on a pillow when you ice it or anytime you sit or lie down during the next 3 days. Try to keep it above the level of your heart. This will help reduce swelling.
- Wrapping the bruised area with an elastic bandage such as an Ace wrap will help decrease swelling. Don’t wrap it too tightly, as this can cause more swelling below the affected area.
- Take an over-the-counter pain medicine, such as acetaminophen (Tylenol), ibuprofen (Advil, Motrin), or naproxen (Aleve).
- Do not take two or more pain medicines at the same time unless the doctor told you to. Many pain medicines have acetaminophen, which is Tylenol. Too much acetaminophen (Tylenol) can be harmful.
Subdural hematoma
A subdural hematoma is a collection of blood between the surface of the brain and the skull. A subdural hematoma is usually caused by a head injury. A subdural hematoma occurs when blood vessels — usually veins — rupture between your brain and the outermost of three membrane layers that cover your brain (the dura mater). The leaking blood forms a hematoma that presses on the brain tissue. An enlarging hematoma can cause gradual loss of consciousness and possibly death.
A subdural hematoma is an emergency condition that can result from a head injury that ruptures of a blood vessel within the brain. A subdural hematoma is potentially life-threatening. It usually requires immediate treatment, often surgery to remove the blood. If there’s any chance you or someone you care for might have a subdural hematoma, it’s important to speak to your doctor straight away, visit your nearest emergency department or call for an ambulance.
If you’re an older adult — especially if you’re taking an anticoagulant or an antiplatelet drug, such as aspirin — even mild head trauma can cause a subdural hematoma.
You can have a serious injury even if there’s no open wound, bruise or other obvious damage.
Figure 1. Meninges of the brain
Footnote: Altered conscious state following fall. Patient on anticoagulation (warfarin) for atrial fibrillation. A very large acute subdural haemorrhage is present with marked midline shift and right uncal herniation. The left temporal horn is dilated in keeping with obstruction to the outflow of the left lateral ventricle.
[Source 1 ]Subdural hematoma types
Subdural hematomas are classified according to the length of time since the event that caused them. They can be:
- Acute subdural hematoma (less than 2 days). This most dangerous type is generally caused by a severe head injury, and signs and symptoms usually appear immediately.
- Subacute subdural hematoma (2 to 14 days). Signs and symptoms take time to develop, sometimes days or weeks after your injury.
- Chronic subdural hematoma (more than 14 days). The result of less severe head injuries, this type of hematoma can cause slow bleeding, and symptoms can take weeks and even months to appear. You might not recall injuring your head. For example, bumping your head while getting into the car can cause bleeding, especially if you’re on blood-thinning medication.
Some people with chronic subdural hematoma have had only a mild head injury or no head injury that they can recall.
All three types require medical attention as soon as signs and symptoms appear so that permanent brain damage can be prevented.
The risk of subdural hematoma increases as you age. The risk is also greater for people who:
- Take aspirin or other blood-thinning medication daily
- Abuse alcohol
You should always seek emergency medical treatment after a severe head injury.
Go to your nearest accident and emergency department, or dial your local emergency services number to request an ambulance.
If you develop the symptoms listed below any time after a minor head injury, or don’t remember hitting your head, you should also go to your nearest emergency department or call your local emergency services number for an ambulance as soon as possible.
A subdural hematoma can be very serious and needs to be assessed as quickly as possible.
Subdural hematoma causes
A subdural hematoma is usually caused by a head injury, such as a blow to the head in a fall, an assault or a road accident. Minor bumps to the head can also lead to a subdural hematoma in a few cases. The blow causes a blood vessel between the surface of the brain and a layer covering the brain to tear. The blood that flows from this blood vessel can’t escape the skull. As this blood starts to build up in the subdural space, it can place pressure on the brain (intracranial hypertension) and it gradually squashes the brain. This can cause brain injury or brain damage.
Who’s most at risk of subdural hematoma?
Anyone can develop a subdural hematoma after a severe head injury.
Chronic subdural hematomas form gradually a few weeks after a minor head injury.
These are more commonly seen in older people and those who take blood-thinning medication, drink excessively, or have another medical condition.
Increasing age
Most chronic subdural hematomas affect people over 60, and the chances of developing one increase with age. This is thought to be because most people’s brains shrink to some degree as they get older.
This places the brain’s blood vessels under increased tension, like a stretched rubber band, and means they’re more vulnerable to damage from minor injuries.
Alcohol misuse
Drinking too much alcohol over a long period of time can also gradually cause the brain to shrink and make the brain’s blood vessels more vulnerable to damage.
Blood-thinning medication
Taking medication to reduce your risk of blood clots can increase your risk of developing a chronic subdural hematoma. This is because it means your blood clots less easily and any bleeding caused by a head injury is likely to be more severe.
Both anticoagulant medicines, such as warfarin, and antiplatelet medicines, such as aspirin, may increase your risk.
Other medical conditions
An increased risk of chronic subdural hematoma has also been linked with:
- Epilepsy – a condition that causes repeated fits (seizures)
- Hemophilia – a condition that stops your blood clotting properly
- Having a ventriculoperitoneal shunt – a thin tube implanted in the brain to drain away any excess fluid to treat hydrocephalus
- Brain aneurysms – a bulge in one of the brain’s blood vessels that can burst and cause bleeding on the brain
- Cancerous (malignant) brain tumors
Subdural hematoma prevention
Follow these tips to reduce the risk of brain injury:
- Seat belts and airbags. Always wear a seat belt in a motor vehicle. A small child should always sit in the back seat of a car secured in a child safety seat or booster seat that is appropriate for his or her size and weight.
- Protect young children. Always use properly fitted car seats, pad countertops and edges of tables, block stairways, tether heavy furniture or appliances to the wall to prevent tipping, and keep children from climbing on unsafe or unsteady objects.
- Alcohol and drug use. Don’t drive under the influence of alcohol or drugs, including prescription medications that can impair the ability to drive.
- Wear a helmet and make sure your kids wear helmets. Wear an appropriate and properly fitted helmet while riding a bicycle, skateboard, motorcycle, snowmobile or all-terrain vehicle. Also wear appropriate head protection when playing baseball or contact sports, skiing, skating, snowboarding or riding a horse or doing any activity that could result in head injury.
- Avoid dangerous sports and activities.
Preventing falls
The following tips can help older adults avoid falls around the house:
- Install handrails in bathrooms
- Put a nonslip mat in the bathtub or shower
- Remove area rugs
- Install handrails on both sides of staircases
- Improve lighting in the home
- Keep stairs and floors clear of clutter
- Get regular vision checkups
- Get regular exercise
Preventing head injuries in children
The following tips can help children avoid head injuries:
- Install safety gates at the top of a stairway
- Keep stairs clear of clutter
- Install window guards to prevent falls
- Put a nonslip mat in the bathtub or shower
- Use playgrounds that have shock-absorbing materials on the ground
- Make sure area rugs are secure
- Don’t let children play on fire escapes or balconies
Subdural hematoma symptoms
The symptoms can develop soon after a severe head injury (acute subdural hematoma), or very occasionally a few days or weeks after a more minor head injury (subacute or chronic subdural hematoma). Sometimes you may not remember hitting your head at all.
The most common symptom of subdural hematoma is a headache, which can be very painful and keeps getting worse.
Other symptoms include:
- nausea and vomiting
- confusion
- personality changes, such as being unusually aggressive or having rapid mood swings
- loss of consciousness
- problems with your vision, such as double vision
- difficulty speaking or speech problems, such as slurred speech
- difficulty with balance or walking
- weakness and numbness
- paralysis (loss of movement) on one side of the body
- problems walking and frequent falls
- change in behavior
- being lethargic or very drowsy
- seizures
- feeling and being sick
- feeling drowsy and finding it difficult to keep your eyes open.
These symptoms can often be mistaken for other conditions, such as strokes, infections or dementia.
Subdural hematoma prognosis
A subdural hematoma is a serious condition that carries a high risk of death, particularly in older people and those whose brain was severely damaged.
Acute subdural hematomas are the most serious type because they’re often associated with significant damage to the brain.
Those who survive an acute subdural hematoma may take a long time to recover, and may be left with physical and mental disabilities.
The outlook is generally better for subacute and chronic hematomas. Most people who are fit enough to have surgery eventually make a full recovery.
But because many people with these types of hematoma are older, they may be too frail to have treatment.
Subdural hematoma diagnosis
If you have had a head injury, you should seek medical help immediately by calling an ambulance or going to the nearest hospital emergency department.
Your doctor will probably ask you questions and examine you. You might need a brain imaging examination such as a computed tomography (CT) scan.
Checking your medical history
The doctor assessing you in hospital might suspect you have a subdural hematoma if you recently injured your head and have some of the main symptoms of a subdural hematoma, such as confusion or a worsening headache.
It’ll also be helpful to know if you take medication to prevent blood clots, such as warfarin or aspirin, as these can increase your chances of developing a subdural hematoma.
If necessary, a blood test can be carried out to assess your blood’s ability to clot.
Sometimes your doctor will want to find out if you have previously been diagnosed with another condition that can have similar symptoms to a subdural hematoma, such as dementia, Parkinson’s disease or a brain tumor.
Tests may be carried out to rule these conditions out.
Assessing your symptoms
You’ll be examined to see if you have any physical signs of an injury to your head, such as cuts and bruises.
Tests to check how your pupils react to light will be used to check for signs of a brain injury.
The Glasgow Coma Scale (GCS) will also normally be used to check your level of consciousness and help determine the severity of any brain injury.
The GCS scores you on:
- your verbal responses – whether you can speak appropriately or make any sounds at all
- your motor response – whether you can move voluntarily or in response to stimulation
- whether you can open your eyes
Table 1. Glasgow Coma Scale
| Under 4 years of age | Above 4 years of age | ||
| Response | Score | Response | Score |
| Eye opening | Eye opening | ||
| Spontaneously | 4 | Spontaneously | 4 |
| To verbal stimuli | 3 | To verbal stimuli | 3 |
| To painful stimuli | 2 | To painful stimuli | 2 |
| No response to pain | 1 | No response to pain | 1 |
| Best verbal response | Best verbal response | ||
| Orientated and converses | 5 | Appropriate words or social smile, fixes, follows | 5 |
| Confused and converses | 4 | Cries but consolable; less than usual words | 4 |
| Inappropriate words | 3 | Persistently irritable | 3 |
| Incomprehensible sounds | 2 | Moans to pain | 2 |
| No response to pain | 1 | No response to pain | 1 |
| Best motor response | Best motor response | ||
| Obeys verbal commands | 6 | Spontaneous or obeys verbal commands | 6 |
| Localises to stimuli | 5 | Localizes to stimuli | 5 |
| Withdraws to stimuli | 4 | Withdraws to stimuli | 4 |
| Abnormal flexion to pain (decorticate) | 3 | Abnormal flexion to pain (decorticate) | 3 |
| Abnormal extension to pain (decerebrate) | 2 | Abnormal extension to pain (decerebrate) | 2 |
| No response to pain | 1 | No response to pain | 1 |
The Glasgow Coma Scale (GCS), a clinical tool designed to assess coma and impaired consciousness, is one of the most commonly used severity scoring systems 2.
- Glasgow Coma Scale scores of 3 to 8 are classified as a severe traumatic brain injury,
- Glasgow Coma Scale scores of 9 to 12 are classified as a moderate traumatic brain injury,
- Glasgow Coma Scale scores of 13 to 15 are classified as a mild traumatic brain injury.
If your GCS score suggests there may be a problem with your brain, a brain scan will be carried out.
Brain scans
Most people with a suspected subdural hematoma will have a type of brain scan called a CT scan to confirm the diagnosis.
A CT scan uses X-rays and a computer to create detailed images of the inside of your body.
It can show whether any blood has collected between your skull and brain.
In a few cases, an MRI scan may be used to check for a subdural hematoma instead.
This is a type of scan that uses strong magnetic fields and radio waves to produce detailed images of the inside of the body.
Subdural hematoma treatment
Surgery is recommended for most subdural hematomas. Very small subdural hematomas may be carefully monitored first to see if they heal without having an operation.
If surgery is recommended, it’ll be carried out by a neurosurgeon (an expert in surgery of the brain and nervous system).
There are 2 widely used surgical techniques to treat subdural hematomas:
- Craniotomy – a section of the skull is temporarily removed so the surgeon can access and remove the hematoma
- Burr holes – a small hole is drilled into the skull and a tube is inserted through the hole to help drain the hematoma
Craniotomy
A craniotomy is the main treatment for subdural hematomas that develop soon after a severe head injury (acute subdural hematomas). A craniotomy is usually performed under a general anaesthetic, which means you’ll be asleep while it’s carried out.
During the procedure, the surgeon creates a temporary flap in the skull. The hematoma is gently removed using suction and irrigation, where it’s washed away with fluid.
After the procedure, the section of skull is put back in place and secured using metal plates or screws.
Burr holes
Burr hole surgery is the main treatment for subdural hematomas that develop a few days or weeks after a minor head injury (chronic subdural hematomas). Burr hole surgery is often carried out under general anaesthetic, but is sometimes done under local anaesthetic. This means you remain awake during the procedure, but the scalp is numbed so you don’t feel any pain.
During the procedure, one or more small holes are drilled in the skull and a flexible rubber tube is inserted to drain the hematoma.
Sometimes the tube may be left in place for a few days afterwards to drain away any blood and reduce the chances of the hematoma coming back.
Risks of surgery
Like all operations, surgery for a subdural hematoma carries a risk of complications. Most of these complications are uncommon, but they can be serious.
Some of the main problems that can occur after subdural hematoma surgery include:
- further bleeding on the brain
- infection of the wound or skull flap
- a blood clot in a leg vein (deep vein thrombosis)
- fits (seizures)
- a stroke
There’s also a chance that not all of the hematoma can be removed and that some of the symptoms you had before surgery continue. These may get better over time or they may be permanent.
In some cases, the hematoma can come back during the days or weeks after surgery. If this happens, further surgery may be needed to drain it again.
Recovering from surgery
If surgery goes well and you don’t have any complications, you may be well enough to leave hospital after a few days.
If you do develop complications, it may be several weeks before you’re able to go home.
If you have persistent problems after surgery, such as memory problems or weakness in your limbs, you may need further treatment to help you gradually return to your normal activities.
The length of time it takes to recover from a subdural hematoma will vary from person to person.
Some people will feel a lot better after a few weeks, while others may never make a full recovery.
Recovering from subdural hematoma
In some cases, a subdural haematoma can cause damage to the brain that requires further care and recovery time.
How long it takes to recover varies from person to person. Some people may feel better within a few weeks or months, while others may never make a full recovery even after many years.
This will largely depend on how severe the damage to your brain is.
What problems might I have?
Many people are left with some long-lasting problems after treatment for a subdural hematoma. These can include changes to your mood, concentration or memory problems, fits (seizures), speech problems, and weakness in your limbs. There’s also a risk the hematoma could come back after treatment. You may have some follow-up appointments and brain scans to check if it’s returned.
Sometimes surgery to drain the hematoma may need to be repeated.
Contact your doctor or hospital care team as soon as possible if any of the symptoms of a subdural hematoma return, such as a worsening headache or periods of confusion.
Rehabilitation
If you have any persistent problems after treatment for a subdural hematoma, you may need further treatment and support to help you return to your normal everyday activities. This is known as rehabilitation.
A number of different healthcare professionals may be involved in your rehabilitation, depending on the specific problems you’re experiencing:
- physiotherapists can help with movement problems, such as muscle weakness or poor co-ordination
- speech and language therapists can help with speech and communication problems
- occupational therapists can identify everyday tasks you have trouble with and help find ways to make things easier for you
You might also benefit from some psychological support or therapy if you find it difficult adjusting to everyday life after a subdural hematoma.
Returning to your normal activities
While you’re recovering, it’s important to take things easy and not to do too much too soon.
Try to make time every day to completely rest your brain from any kind of distraction, such as the radio or television.
Speak to your specialist for advice before driving, flying or returning to sport as sometimes these can be dangerous while recovering from a subdural hematoma.
How soon you’ll be able to drive will depend on the type of subdural hematoma you had, what treatment you had or continue to have, and whether you have any persistent problems, such as seizures.
Intracranial hematoma
An intracranial hematoma is a collection of blood within the skull, most commonly caused by rupture of a blood vessel within the brain or from trauma such as a car accident or fall. The blood collection can be within the brain tissue or underneath the skull, pressing on the brain.
Although some head injuries — such as one that causes only a brief lapse of consciousness (concussion) — can be minor, an intracranial hematoma is potentially life-threatening. It usually requires immediate treatment, often surgery to remove the blood.
You should always seek emergency medical treatment after a severe head injury.
An intracranial hematoma can be life-threatening, requiring emergency treatment.
Seek immediate medical attention after a blow to the head if you:
- Lose consciousness
- Have a persistent headache
- Have difficulties such as vomiting, weakness, blurred vision, unsteadiness
If signs and symptoms aren’t immediately evident after a blow to the head, watch for physical, mental and emotional changes. For example, if someone seems fine after a blow to the head and can talk but later becomes unconscious, seek immediate medical care.
Also, even if you feel fine, ask someone to keep an eye on you. Memory loss after a blow to your head can make you forget about the blow. Someone you tell might be more likely to recognize the warning signs and get you medical attention.
Intracranial hematoma symptoms
You might develop signs and symptoms of an intracranial hematoma right after a blow to your head, or they may take weeks or longer to appear. You might seem fine after a head injury, a period called the lucid interval.
However, with time, pressure on your brain increases, producing some or all of the following signs and symptoms:
- Increasing headache
- Vomiting
- Drowsiness and progressive loss of consciousness
- Dizziness
- Confusion
- Unequal pupil size
- Slurred speech
As more blood fills your brain or the narrow space between your brain and skull, other signs and symptoms may become apparent, such as:
- Lethargy
- Seizures
- Unconsciousness
Intracranial hematoma causes
Head injury, often from motor vehicle or bicycle accidents, falls, assaults, and sports injuries, is the most common cause of intracranial bleeding (hemorrhage).
If you’re an older adult — especially if you’re taking an anticoagulant or an antiplatelet drug, such as aspirin — even mild head trauma can cause a hematoma.
You can have a serious injury even if there’s no open wound, bruise or other obvious damage.
There are three categories of hematoma — subdural hematoma, epidural hematoma and intraparenchymal hematoma.
- Subdural hematoma (see above)
- Epidural hematoma
- Also called an extradural hematoma, this type occurs when a blood vessel — usually an artery — ruptures between the outer surface of the dura mater and the skull. Blood then leaks between the dura mater and the skull to form a mass that presses on brain tissue. The most common cause of an epidural hematoma is trauma.
- Some people with this type of injury remain conscious, but most become drowsy or go into a coma from the moment of trauma. An epidural hematoma that affects an artery in your brain can be deadly without prompt treatment.
- Intraparenchymal hematoma
- This type of hematoma, also known as intracerebral hematoma, occurs when blood pools in the brain. There are many causes, including trauma, rupture of an aneurysm, vascular malformation, high blood pressure and tumor. There are also diseases that can cause spontaneous leakage of blood into the brain. A head trauma can result in multiple severe intraparenchymal hematomas.
Intracranial hematoma prevention
Follow these tips to reduce the risk of brain injury:
- Seat belts and airbags. Always wear a seat belt in a motor vehicle. A small child should always sit in the back seat of a car secured in a child safety seat or booster seat that is appropriate for his or her size and weight.
- Protect young children. Always use properly fitted car seats, pad countertops and edges of tables, block stairways, tether heavy furniture or appliances to the wall to prevent tipping, and keep children from climbing on unsafe or unsteady objects.
- Alcohol and drug use. Don’t drive under the influence of alcohol or drugs, including prescription medications that can impair the ability to drive.
- Wear a helmet and make sure your kids wear helmets. Wear an appropriate and properly fitted helmet while riding a bicycle, skateboard, motorcycle, snowmobile or all-terrain vehicle. Also wear appropriate head protection when playing baseball or contact sports, skiing, skating, snowboarding or riding a horse or doing any activity that could result in head injury.
- Avoid dangerous sports and activities.
Preventing falls
The following tips can help older adults avoid falls around the house:
- Install handrails in bathrooms
- Put a nonslip mat in the bathtub or shower
- Remove area rugs
- Install handrails on both sides of staircases
- Improve lighting in the home
- Keep stairs and floors clear of clutter
- Get regular vision checkups
- Get regular exercise
Preventing head injuries in children
The following tips can help children avoid head injuries:
- Install safety gates at the top of a stairway
- Keep stairs clear of clutter
- Install window guards to prevent falls
- Put a nonslip mat in the bathtub or shower
- Use playgrounds that have shock-absorbing materials on the ground
- Make sure area rugs are secure
- Don’t let children play on fire escapes or balconies
Intracranial hematoma diagnosis
Diagnosing an intracranial hematoma can be difficult because people with a head injury can seem fine. However, doctors generally assume that a hemorrhage inside the skull is the cause of progressive loss of consciousness after a head injury until proved otherwise.
Imaging techniques are the best ways to determine the position and size of a hematoma. These include:
- CT scan. This uses a sophisticated X-ray machine linked to a computer to produce detailed images of your brain. You lie still on a movable table that’s guided into what looks like a large doughnut where the images are taken. CT is the most commonly used imaging scan to diagnose intracranial hematomas.
- MRI scan. This is done using a large magnet and radio waves to make computerized images. During an MRI scan, you lie on a movable table that’s guided into a tube. MRIs aren’t used as often as CT scans to diagnose intracranial hematomas because MRIs take longer to perform and aren’t as available.
- Angiogram. If there is concern about a possible bulge in a blood vessel (aneurysm) of the brain or other blood vessel problem, an angiogram might be necessary to provide more information. This test uses X-ray and a special dye to produce pictures of the blood flow in the blood vessels in the brain.
Intracranial hematoma treatment
Hematomas that are small and produce no signs or symptoms don’t need to be removed. But because signs and symptoms can appear or worsen days or weeks after the injury, you might have to be watched for neurological changes, have your intracranial pressure monitored and undergo repeated head CT scans.
If you take blood-thinning medication, such as warfarin, you may need therapy to reverse the effects of the medication and reduce the risk of further bleeding. Options for reversing blood thinners include administering vitamin K and fresh frozen plasma.
Surgery
Hematoma treatment often involves surgery. The type of surgery depends on the type of hematoma you have. Options include:
- Surgical drainage. If the blood is localized and isn’t clotting a lot, your doctor might create a burr hole through your skull and use suction to remove the liquid.
- Craniotomy. Large hematomas might require that a section of your skull be opened (craniotomy) to remove the blood.
Recovery
Recovery after an intracranial hematoma can take a long time, and you might not recover completely. The greatest period of recovery is up to three months after the injury, usually with lesser improvement after that. If you continue to have neurological problems after treatment, you might need occupational and physical therapy.
Coping and support
Patience is key to coping with brain injuries. Adults will have the majority of their recovery during the first six months. Then you might have smaller, more-gradual improvements for up to two years after the hematoma.
To aid your recovery:
- Get enough sleep at night, and rest in the daytime when you feel tired.
- Ease back into your normal activities when you feel stronger.
- Don’t participate in contact and recreational sports until you get your doctor’s OK.
- Check with your doctor before you begin driving, playing sports, riding a bicycle or operating heavy machinery. Your reaction times likely will have slowed as a result of your brain injury.
- Check with your doctor before taking medication.
- Don’t drink alcohol until you’ve recovered fully. Alcohol may hinder recovery, and drinking too much can increase your risk of a second injury.
- Write down things you have trouble recalling.
- Talk with someone you trust before making important decisions.