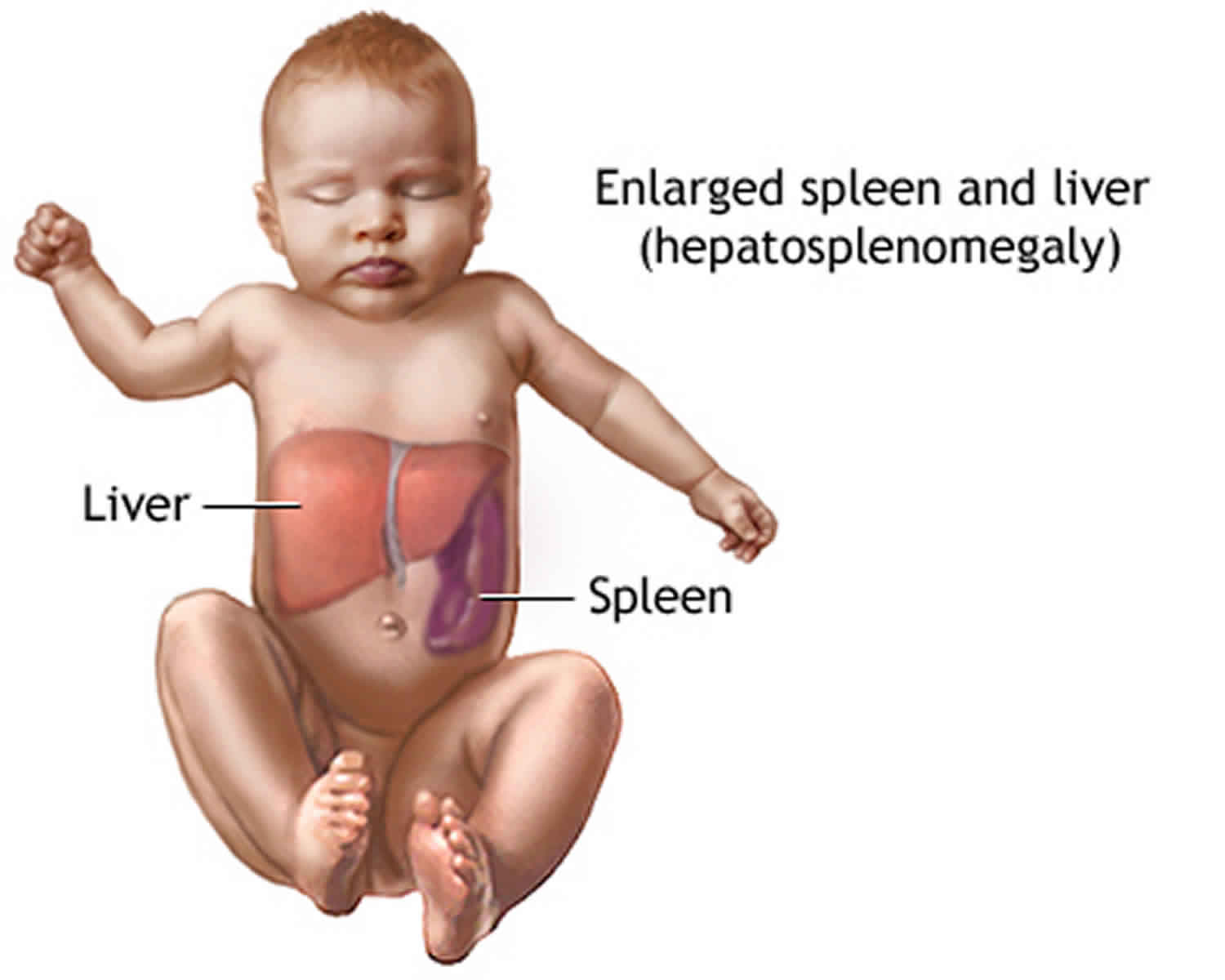
Hepatosplenomegaly
Hepatosplenomegaly is defined as an abnormal enlargement of both the liver (hepatomegaly) and the spleen (splenomegaly). There are many causes of hepatosplenomegaly. Because hepatosplenomegaly has many possible causes, doctors may take a while to diagnose it. However, this is an important part of the process. Doctors need to find out the precise cause. This is because the treatment of the underlying cause is the first step in managing hepatosplenomegaly. For example, in Gaucher disease, hepatosplenomegaly (liver and spleen enlargement) can occur as the result of the liver not processing glucocerebroside properly. The buildup of this substance in body tissues can also lead to severe damage to the central nervous system in infants.
Hepatosplenomegaly causes
Infection
Many, many infections can produce a mild concurrent enlargement of the liver and spleen. This list is by no means exhaustive.
- viral
- EBV (infectious mononucleosis) (common)
- AIDS with Mycobacterial avium complex infection
- CMV
- rubella
- bacterial
- tuberculosis (miliary)
- subacute bacterial endocarditis
- typhoid fever
- brucellosis
- syphilis
- abscess
- fungal
- histoplasmosis
- candidiasis
- parasitic disease
- malaria
- schistosomiasis
- hydatid disease
- leishmaniasis (kala-azar)
Cancer
- lymphoma
- leukemia 1
- multiple metastases: primaries: melanoma, pancreatic, breast, hepatic angiosarcoma
- splenic metastases not usually seen unless advanced metastatic disease
Blood disorders
- extramedullary hematopoiesis
- thalassemia
- sickle cell disease: normal/atrophic spleen more common
- systemic mastocytosis
- myelofibrosis
- myeloproliferative disease
- hemochromatosis
- hemophagocytic lymphohistiocytosis
- hemolytic anemias:
- Hemoglobinopathies: Thalassaemia, sickle cell disease (eventually leads to splenic atrophy)
- Red cell structure: Spherocytosis/elliptocytosis
- Enzyme: G6PD deficiency, pyruvate kinase deficiency
Storage diseases/metabolic/infiltrative disorders
- lysosomal storage disorders 2
- Gaucher disease 3
- mucopolysaccharidoses 4
- Niemann-Pick disease
- Wolman disease 1
- alpha-mannosidosis 2
- glycogen storage diseases
- porphyria
- amyloidosis
- sarcoidosis
- hypervitaminosis A
Connective tissue disorders
- rheumatoid arthritis
- Felty syndrome
- juvenile rheumatoid arthritis
- Still disease
- systemic lupus erythematosus (SLE)
Others
- cirrhosis (early)
- chronic liver disease and portal hypertension
- portal hypertension (non-cirrhotic)
- Graves disease 5.
Hepatosplenomegaly differential diagnosis
Hepatosplenomegaly differential diagnosis:
- Abdominal typhoid fever
- Amebiasis
- Amyloidosis
- Bang’s Disease
- Banti’s Disease
- Bilharziosis
- Brucellosis
- Budd-Chiari Syndrome
- Chronic myelogenous leukemia
- Chronic myelosis
- Cirrhosis
- Congested liver
- Cystic Fibrosis
- Cystic liver
- Cytomegalovirus
- Dengue
- Drug-induced jaundice
- Echinococcosis
- Extrahepatic cholestasis
- Familial hypercholesterolemia
- Fatty liver
- Felty’s Syndrome
- Galactosemia
- Gaucher’s Disease
- Glucose-6 phosphate deficiency
- Hemochromatosis
- Histiocytosis X
- Histoplasmosis
- Hodgkin’s Lymphoma
- Idiopathic thrombocythemia
- Immune-hemolytic anemia
- Infectious mononucleosis (Glandular fever) due to Epstein-Barr virus
- Juvenile myelomonocytic leukemia
- Leishmaniais
- Leptospirosis
- Letterer-Siwe Disease
- Leukemia
- Lymphoma
- Malaria
- Miliary tuberculosis
- Morbus haemolyticus neonatorum
- Moschcowitz microangiopathy
- Multiple liver metastases
- Neimann-Pick Disease
- Neuroblastoma
- Pfaundler-Hurler Syndrome
- Polycythemia
- Primary biliary cirrhosis
- Osler’s Disease
- Osteomyelosclerosis
- Primary/acute HIV infection
- Recurrent pulmonary embolism
- Relapsing fever
- Sarcoidosis
- Schistosomiasis
- Sickle Cell Anemia
- Sideroblastic anemia
- Still’s Disease
- Stones
- Systemic Juvenile Idiopathic Arthritis
- Thalassemia
- Type IV glycogenesis
- Venous thrombosis
- Viral hepatitis
- Visceral leishmaniasis
- Wilson’s Disease
Hepatosplenomegaly symptoms
Hepatosplenomegaly symptoms depend on the underlying cause of hepatosplenomegaly. They often experience fatigue and pain in and around the affected organs.
Patients with severe cases of hepatosplenomegaly often suffer from pain in the upper-right quadrant of the abdomen. Vomiting and nausea, as well as jaundice and fever, are also common symptoms.
Patients can also experience abdominal swelling as well as dark-colored urine and stool.
Hepatosplenomegaly diagnosis
History in hepatosplenomegaly:
- Presenting complaint
- Abdominal swelling
- History of presenting complaint
- Abdominal pain
- Bloating
- Abnormal bruising/bleeding
- Pruritus
- Constitutional symptoms: weight loss, night sweats, fever
- Past medical history
- Previous EBV infection
- Medications
- Hepatotoxic medications
- Family history
- Malignancy
- Connective tissue disease
- Metabolic disorders
- Social history
- Travel history
- Alcohol consumption
- Smoking
Your doctor will examine you and ask questions such as:
- Did you notice fullness or a lump in the abdomen?
- What other symptoms do you have?
- Is there any abdominal pain?
- Is there any yellowing of the skin (jaundice)?
- Is there any vomiting?
- Is there any unusual-colored or pale-colored stools?
- Has your urine appeared to be darker than usual (brownish)?
- Have you had a fever?
- What medicines are you taking including over-the-counter and herbal medicines?
- How much alcohol do you drink?
Tests to determine the cause of hepatosplenomegaly vary, depending on the suspected cause, but may include:
- Abdominal x-ray
- Abdominal ultrasound (may be done to confirm the condition if your doctor thinks your liver feels enlarged during a physical exam)
- CT scan of the abdomen
- MRI scan of the abdomen
- Routine blood tests – CBC, BUN, LFTs, CRP, ESR, HIV, TSH, autoimmune screen, including blood clotting tests
- Plain chest X-ray
- Stool cultures may be relevant. If infective diarrhea is syspected, you may require three samples on three separate days to increase the likelihood of catching the infection
Hepatosplenomegaly treatment
Hepatosplenomegaly treatment will largely depend on the cause of the hepatosplenomegaly.
References- Gopakumar KG, Thankamony P, Nampoothiri S, Bali D, Raj J, A Vasudevan J, K Nair R. Wolman Disease: A Mimic of Infant Leukemia. (2017) Journal of pediatric hematology/oncology. 39 (8): e489-e492. doi:10.1097/MPH.0000000000000861
- Futerman AH, van Meer G. The cell biology of lysosomal storage disorders. (2004) Nature reviews. Molecular cell biology. 5 (7): 554-65. doi:10.1038/nrm1423
- Tseng SY, Niu DM, Chu TH, Yeh YC, Huang MH, Yang TF, Liao HC, Chiang CC, Ho HC, Soong WJ, Yang CF. Very rare condition of multiple Gaucheroma: A case report and review of the literature. (2019) Molecular genetics and metabolism reports. 20: 100473. doi:10.1016/j.ymgmr.2019.100473
- Cheema HA, Malik HS, Hashmi MA, Fayyaz Z, Mushtaq I, Shahzadi N. Mucopolysaccharidoses – Clinical Spectrum and Frequency of Different Types. J Coll Physicians Surg Pak. 2017 Feb;27(2):80-83. https://www.ncbi.nlm.nih.gov/pubmed/28292383
- WALLERSTEIN RS, WALKER WJ. Hepatosplenomegaly and liver damage in Graves’ disease. (1949) Annals of internal medicine. 31 (5): 904-12. doi:10.7326/0003-4819-31-5-904