Hyperesthesia
Hyperesthesia or hyperaesthesia, is an unusual sensibility to sensory stimuli, such as pain or touch. Hyperesthesia refers to increased sensitivity to cutaneous stimulation due to a diminished threshold or an increased response to stimuli. Frequently described as a chronic burning type pain, it can also manifest as increased sensitivity to touch.
Types of hyperesthesia include:
- Acoustic or auditory hyperesthesia: sensitivity to sound
- Gustatory hyperesthesia: sensitivity to taste
- Muscular hyperesthesia: sensitivity to pain or tiredness
- Optic hyperesthesia: sensitivity to light
- Tactile hyperesthesia: sensitivity to touch
If painful hyperesthesia is the only symptom, the diagnosis of small-fiber neuropathy should be considered. In this type of neuropathy the sensory, often painful, symptoms begin in the feet and progress proximally, eventually involving the hands. Less typical onset of symptoms has been described in patients with demonstrated gain-of-function mutations of the genes SCN 9A or SCN 10A, mutations found in some patients with this type of neuropathy. Difficulties may arise when small-fiber neuropathy is diagnosed on the basis of skin biopsy. In this situation it can be unclear whether loss of nerve fibers occurs as a primary phenomenon or secondary to limb disuse in chronic pain. Paresthesia appears very commonly with many types of chronic pain syndrome, including those where there is a clear organic cause such as herpes zoster, but also those where there is no clear pathology, such as fibromyalgia. Hyperesthesia may be mixed with hyperalgesia and allodynia.
Traumatic brain injury may be accompanied by hyperesthesia to 1:
- Light (Photophobia)
- Sound (Hyperacusis)
- Touch (Sensory Defensiveness)
- Temperature (Sensory Defensiveness)
Excessive consumption of caffeine can temporarily induce hyperesthesia in humans and usually wears off after 3-5 hours, due to excessive stimulaton of the spinal cord, as well as the cortex and medulla in the central nervous system.
Hyperesthesia is a common phenomenon in patients with functional neurologic symptoms 2. Hyperesthesia may be generalized and may occur as hemihyperesthesia. Literature on hyperventilation shows that hemisensory tingling can be induced experimentally in some people during hyperventilation, which may include panic attacks, migraine, and dissociation.
Hyperesthesia causes
The most common cause of hyperesthesia is peripheral neuropathy and there are more than 100 kinds of peripheral nerve disorders. They can affect one nerve or many nerves. Some are the result of other diseases, like diabetic nerve problems, chemo-induced neuropathy, hereditary disorders, inflammatory infections, auto-immune diseases, protein abnormalities, exposure to toxic chemicals (toxic neuropathy), poor nutrition, kidney failure, chronic alcoholism, and certain medications – especially those used to treat cancer and HIV/AIDS. Others, like Guillain-Barre syndrome, happen after a virus infection. Still others are from nerve compression, like carpal tunnel syndrome or thoracic outlet syndrome. In some cases, like complex regional pain syndrome and brachial plexus injuries, the problem begins after an injury. Some people are born with peripheral nerve disorders. In some cases, however, even with extensive evaluation, the causes of peripheral neuropathy in some people remain unknown – this is called idiopathic neuropathy.
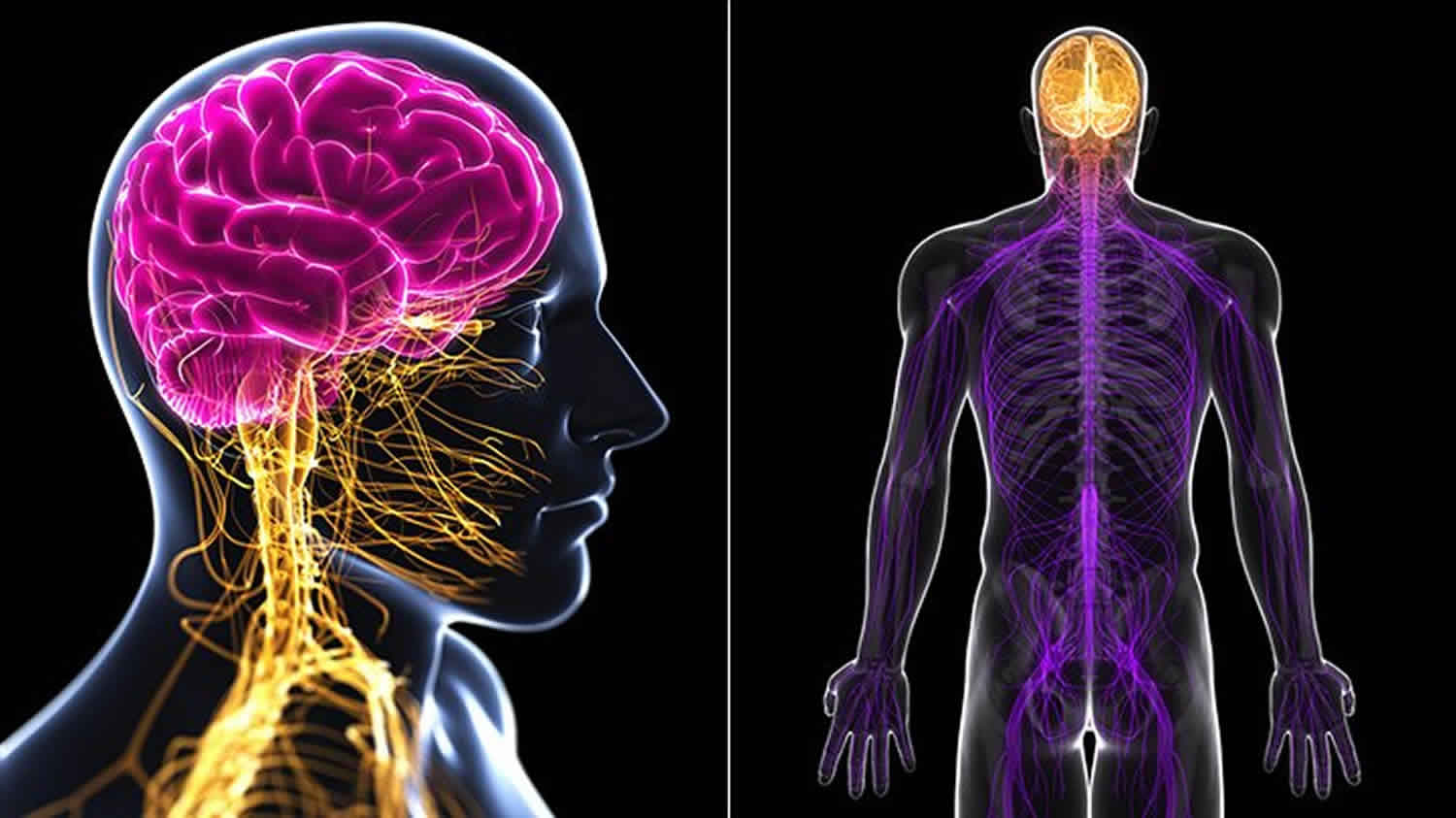
Your peripheral nerves are the ones outside your brain and spinal cord. Like static on a telephone line, peripheral nerve disorders distort or interrupt the messages between the brain and the rest of the body.
Most instances of neuropathy are either acquired, meaning the neuropathy or the inevitability of getting it isn’t present from the beginning of life, or genetic. Acquired neuropathies are either symptomatic (the result of another disorder or condition; see below) or idiopathic (meaning it has no known cause).
Causes of symptomatic acquired peripheral neuropathy include:
- Physical injury (trauma) is the most common cause of acquired single-nerve injury. Injury from automobile accidents, falls, sports, and medical procedures can stretch, crush, or compress nerves, or detach them from the spinal cord. Less severe traumas also can cause serious nerve damage. Broken or dislocated bones can exert damaging pressure on neighboring nerves and slipped disks between vertebrae can compress nerve fibers where they emerge from the spinal cord. Arthritis, prolonged pressure on a nerve (such as by a cast) or repetitive, forceful activities can cause ligaments or tendons to swell, which narrows slender nerve pathways. Ulnar neuropathy and carpal tunnel syndrome are common types of neuropathy from trapped or compressed nerves at the elbow or wrist. In some cases, there are underlying medical causes (such as diabetes) that prevent the nerves from tolerating the stresses of everyday living.
- Diabetes is the leading cause of polyneuropathy in the United States. About 60 – 70 percent of people with diabetes have mild to severe forms of damage to sensory, motor, and autonomic nerves that cause such symptoms as numb, tingling, or burning feet, one-sided bands or pain, and numbness and weakness on the trunk or pelvis.
- Vascular and blood problems that decrease oxygen supply to the peripheral nerves can lead to nerve tissue damage. Diabetes, smoking, and narrowing of the arteries from high blood pressure or atherosclerosis (fatty deposits on the inside of blood vessel walls) can lead to neuropathy. Blood vessel wall thickening and scarring from vasculitis can impede blood flow and cause patchy nerve damage in which isolated nerves in different areas are damaged—called mononeuropathy multiplex or multifocal mononeuropathy.
- Systemic (body-wide) autoimmune diseases, in which the immune system mistakenly attacks a number of the body’s own tissues, can directly target nerves or cause problems when surrounding tissues compress or entrap nerves. Sjögren’s syndrome, lupus, and rheumatoid arthritis are some systemic autoimmune diseases that cause neuropathic pain.
- Autoimmune diseases that attack nerves only are often triggered by recent infections. They can develop quickly or slowly, while others become chronic and fluctuate in severity. Damage to the motor fibers that go to the muscle includes visible weakness and muscle shrinking seen in Guillain-Barré syndrome and chronic inflammatory demyelinating polyneuropathy. Multifocal motor neuropathy is a form of inflammatory neuropathy that affects motor nerves exclusively. In other autoimmune neuropathies the small fibers are attacked, leaving people with unexplained chronic pain and autonomic symptoms.
- Hormonal imbalances can disturb normal metabolic processes, leading to swollen tissues that can press on peripheral nerves.
- Kidney and liver disorders can lead to abnormally high amounts of toxic substances in the blood that can damage nerve tissue. Most individuals on dialysis because of kidney failure develop varying levels of polyneuropathy.
- Nutritional or vitamin imbalances, alcoholism, and exposure to toxins can damage nerves and cause neuropathy. Vitamin B12 deficiency and excess vitamin B6 are the best known vitamin-related causes. Several medications have been shown to occasionally cause neuropathy.
- Certain cancers and benign tumors cause neuropathy in various ways. Tumors sometimes infiltrate or press on nerve fibers. Paraneoplastic syndromes, a group of rare degenerative disorders that are triggered by a person’s immune system response to a cancer, can indirectly cause widespread nerve damage.
- Chemotherapy drugs used to treat cancer cause polyneuropathy in an estimated 30 to 40 percent of users. Only certain chemotherapy drugs cause neuropathy and not all people get it. Chemotherapy-induced peripheral neuropathy may continue long after stopping chemotherapy. Radiation therapy also can cause nerve damage, sometimes starting months or years later.
- Infections can attack nerve tissues and cause neuropathy. Viruses such as varicella-zoster virus (which causes chicken pox and shingles), West Nile virus, cytomegalovirus, and herpes simplex target sensory fibers, causing attacks of sharp, lightning-like pain. Lyme disease, carried by tick bites, can cause a range of neuropathic symptoms, often within a few weeks of being infected. The human immunodeficiency virus (HIV), which causes AIDS, can extensively damage the central and peripheral nervous systems. An estimated 30 percent of people who are HIV-positive develop peripheral neuropathy; 20 percent develop distal (away from the center of the body) neuropathic pain.
Genetically-caused polyneuropathies are rare. Genetic mutations can either be inherited or arise de novo, meaning they are completely new mutations to an individual and are not present in either parent. Some genetic mutations lead to mild neuropathies with symptoms that begin in early adulthood and result in little, if any, significant impairment. More severe hereditary neuropathies often appear in infancy or childhood. Charcot-Marie-Tooth disease, also known as hereditary motor and sensory neuropathy, is one of the most common inherited neurological disorders.
The small-fiber neuropathies that present with pain, itch, and autonomic symptoms also can be genetic. As our understanding of genetic disorders increases, many new genes are being associated with peripheral neuropathy.
Diabetic peripheral neuropathy
Diabetic peripheral neuropathy is the most common type of peripheral neuropathy. Today, it is estimated that 60-70% of diabetics have diabetic peripheral neuropathy. Under managed diabetic peripheral neuropathy is the number one cause of non-traumatic lower limb amputations in the United States.
Chemotherapy-induced peripheral neuropathy
30-40% of all cancer patients have chemotherapy-induced peripheral neuropathy. Chemotherapy-induced peripheral neuropathy is caused by chemotherapy drugs used in cancer treatments. Chemotherapy is hardest on the nervous system due to the fact the nerve cells are more sensitive than other cells. Sensory nerves are at an increased risk to chemotherapy-associated damage compared to motor nerves. The onsets and resolution of symptoms is variable. Some drugs may cause symptoms during or immediately after the first dose and some have a delayed onset of symptoms, up to several weeks, months, or even years, after the last dose.
Idiopathic peripheral neuropathy
Idiopathic peripheral neuropathy has no identifiable known cause and therefore is considered the primary disease. If a cause is detected, then the neuropathy is secondary to that and not idiopathic.
Idiopathic peripheral neuropathies occur typically in middle-aged and elderly individuals. It’s estimated that 23% of all neuropathy patients are diagnosed with idiopathic neuropathy.
Human immunodeficiency virus (HIV) or AIDS
Human immunodeficiency virus (HIV) or AIDS are often accompanied by the development of peripheral neuropathic conditions. Of all HIV/AIDS patients, 33% have peripheral neuropathy.
Immune system disorders
- Guillian-Barré syndrome and Chronic Inflammatory Demyelinating Polyneuropathy (CIDP). Anyone can develop Guillian-Barré syndrome; however, it is more common among older adults. The incidence of Guillian-Barré syndrome increases with age, and people older than 50 years are at greatest risk for developing Guillian-Barré syndrome. In the United States, for example, an estimated 3,000 to 6,000 people develop Guillian-Barré syndrome each year on average.
- Charcot-Marie Tooth. Charcot-Marie Tooth disease is the most common inherited disorder that involves the peripheral nerves, affecting an estimated 150,000 people in the United States. It occurs in populations worldwide with a prevalence of about 1 in 2,500 individuals.
Other autoimmune disorders can include but not limited to:
- Celiac disease
- Lupus
- Rheumatoid arthritis
- Shingles
Repetitive stress
A job or hobby that puts stress on one nerve for long periods of time increases the chances for development of peripheral neuropathy. Playing certain sports or musical instruments and/or using vibrating power tools even crutches can put pressure on peripheral nerves and cause nerve irritation and damage.
Alcohol abuse
Excessive drinking of alcohol can affect the nervous system, causing numbness of the hands and feet.
Vitamin deficiency
A lack of certain vitamins, especially B-1 (thiamin) and B-12 makes peripheral neuropathy more likely. Pernicious anemia, which occurs when the body cannot absorb B-12 properly, often leads to peripheral neuropathy. Learn more
Other health problems
Medical conditions, including certain types of kidney disease and liver disease, or those with family history of genetic diseases that produce peripheral neuropathic pain symptoms and conditions put an individual at risk of developing peripheral nerve damage. Learn more
Toxic substances
Exposure to some toxic substances can make one susceptible to peripheral nerve damage. These substances include heavy metals, such as lead, mercury, arsenic and organic solvents; and certain medications, such as those used to treat cancer or AIDS.
Hyperesthesia symptoms
Hyperesthesia symptoms often start gradually, and then get worse. They include
- Numbness
- Pain
- Burning or tingling
- Muscle weakness
- Sensitivity to touch
From Henry Head, Studies in Neurology(1920), hyperesthesia is described as:
- “Pins and needles.”
- “Unpleasant numb feeling.”
- “something … crawling under the skin.”
- “dreadful burning pain.”
- food always seemed rough and cold on the affected side.
- even hot tea felt unpleasantly cold on the cheek of the affected side.
Peripheral neuropathy symptoms usually start with numbness, prickling or tingling in the toes or fingers. It may spread up to the feet or hands and cause burning, freezing, throbbing and/or shooting pain that is often worse at night.
The pain can be either constant or periodic, but usually the pain is felt equally on both sides of the body—in both hands or in both feet. Some types of peripheral neuropathy develop suddenly, while others progress more slowly over many years.
The symptoms of peripheral neuropathy often include:
- A sensation of wearing an invisible “glove” or “sock”
- Burning sensation or freezing pain
- Sharp, jabbing, shooting, or electric-like pain
- Extreme sensitivity to touch
- Difficulty sleeping because of feet and leg pain
- Loss of balance and coordination
- Muscle weakness
- Muscle cramping/twitching
- Difficulty walking or moving the arms
- Unusual sweating
- Abnormalities in blood pressure or pulse
Symptoms such as experiencing weakness or not being able to hold something, not knowing where your feet are, and experiencing pain that feels as if it is stabbing or burning in your limbs, can be common signs and symptoms of peripheral neuropathy.
The symptoms of peripheral neuropathy may depend on the kind of peripheral nerves that have been damaged. There are three types of peripheral nerves: motor, sensory and autonomic. Some neuropathies affect all three types of nerves, while others involve only one or two.
The majority of people, however, suffer from polyneuropathy, an umbrella term for damage involving many nerves at the same time.
Hyperesthesia diagnosis
The bewildering array and variability of symptoms that neuropathies can cause often makes diagnosis difficult. Before diagnosing peripheral neuropathy, your physician will review your medical history and conduct a physical exam and neurological evaluation.
A neurological evaluation, which consists of a number of simple and painless tests, is usually performed to diagnose peripheral neuropathy. Depending on your symptoms and outcome of the neurological evaluation, you may encounter other tests that can determine what type of peripheral neuropathy you have.
A neurological exam helps doctors to diagnose peripheral neuropathy and may include the following:
- Your history: questions concerning your symptoms and condition
- An evaluation of neurological function
- Diagnostic tests
- Electrodiagnostic tests
- Blood tests
- Other common tests
Medical history
You should be prepared to discuss your symptoms in detail with your doctor. Your doctor will ask you to describe your symptoms, when you experience them, how long the episodes last and the amount of discomfort or pain you experience. The more specific you can be about the tingling, numbness, weakness or other symptoms you are experiencing, the easier it will be for your doctor to understand your condition.
Your doctor may also ask you general health questions that may seem unrelated to your symptoms, but are, in fact, important. These questions could be about whether or not you feel faint, nauseated or tired. The doctor may also ask if your bladder control and sexual function are normal. You will also be asked if you are suffering from any other illnesses and if you are taking medications.
The physician will then perform a physical exam to test for loss of vibratory sensation. He or she will test ankle jerks and other reflexes. Sensations in the feet and hands will be evaluated with a pin.
Since some neuropathies are hereditary, you doctor will ask if other members of your family have suffered from any type of neuropathy or neurological disorder.
Neurological examination tests
A neurological evaluation consists of a physical exam and a number of simple and painless tests. The purpose of these tests is to assess your neurological function, including your muscle strength, how your autonomic nerves are functioning, and your ability to feel different sensations.
Diagnostic testing
The neurologist may recommend certain diagnostic tests, depending on the patient’s symptoms, medical history and physical examination.
Frequently the neurologist will recommend electrodiagnostic testing to measure the electrical activity of muscles and nerves. If necessary, the neurologist may also recommend a nerve biopsy, a spinal tap or magnetic resonance imaging (MRI). However, for some patients with longstanding neuropathy, the cause may not be found in spite of extensive tests and examinations.
Electrodiagnostic test
Electrodiagnostic tests measure the electrical activity of muscles and nerves. By measuring the electrical activity they are able to determine if there is nerve damage, the extent of the damage and potentially the cause of the damage. Frequently the neurologist will recommend common, non-invasive neurological evaluations such as electromyography (EMG) and nerve conduction velocity (NCV) testing.
Blood tests
Blood tests are commonly employed to check for vitamin deficiencies, toxic elements and evidence of an abnormal immune response.
Depending on your individual situation, your doctor may request certain laboratory tests to identify potentially treatable causes for neuropathy. These include tests for:
- Vitamin B12 and folate levels
- Thyroid, liver and kidney functions
- Vasculitis evaluation
- Oral glucose tolerance test
- Antibodies to nerve components (e.g., anti-MAG antibody)
- Antibodies related to celiac disease
- Lyme disease
- HIV/AIDS
- Hepatitis C and B
Other common tests
If your doctor suspects that you have a specific type of neuropathy, an advanced case of neuropathy, or an entirely different condition, it may be suggested that you undergo additional testing. Your doctor may recommend quantitative sensory testing and autonomic testing, or other tests to diagnose a specific disorder.
Hyperesthesia treatment
Hyperesthesia treatment aims to treat any underlying problem, reduce pain and control symptoms. Treatments depend entirely on the type of nerve damage, symptoms, and location. Your doctor will explain how nerve damage is causing specific symptoms and how to minimize and manage them. With proper education, some people may be able to reduce their medication dose or manage their neuropathy without medications. Definitive treatment can permit functional recovery over time, as long as the nerve cell itself has not died. Treatment often involves a number of approaches and aims to restore movement and function of the affected limb. Options may include:
- medication – such as pain-relieving medications. Medications that are usually prescribed for other conditions, such as epilepsy or depression, can sometimes help to manage hyperesthesia, although this does not mean that the person has epilepsy or depression
- physical therapy – such as physiotherapy and occupational therapy. Typically, treatment starts with strategies to reduce pain and swelling. This is followed by gentle movement, then muscle-strengthening exercises to improve the functioning of the limb and, finally, exercises to improve the functioning of the person’s whole body
- counseling and psychological support – for example, to help the person cope with stress, depression and chronic pain
- intervention therapy – such as nerve blocks. The most commonly used is a sympathetic ganglion block, which involves the use of a local anesthetic to stop some of the nerves in the affected limb from working
- implant therapy – an operation to place a device such as an electrode or a medication-delivery system is placed into the person’s body. The device helps to manage symptoms, including pain. However, implant therapy is considered a last resort when all other methods of pain management have failed.
Addressing neuropathy’s causes. Correcting underlying causes can result in the neuropathy resolving on its own as the nerves recover or regenerate. Nerve health and resistance can be improved by healthy lifestyle habits such as maintaining optimal weight, avoiding toxic exposures, eating a balanced diet, and correcting vitamin deficiencies. Smoking cessation is particularly important because smoking constricts the blood vessels that supply nutrients to the peripheral nerves and can worsen neuropathic symptoms. Exercise can deliver more blood, oxygen, and nutrients to far-off nerve endings, improve muscle strength, and limit muscle atrophy. Self-care skills in people with diabetes and others who have an impaired ability to feel pain can alleviate symptoms and often create conditions that encourage nerve regeneration. Strict control of blood glucose levels has been shown to reduce neuropathic symptoms and help people with diabetic neuropathy avoid further nerve damage.
Inflammatory and autoimmune conditions leading to neuropathy can be controlled using immunosuppressive drugs such as prednisone, cyclosporine, or azathioprine. Plasmapheresis—a procedure in which blood is removed, cleansed of immune system cells and antibodies, and then returned to the body—can help reduce inflammation or suppress immune system activity. Agents such as rituximab that target specific inflammatory cells, large intravenously administered doses of immunoglobulins, and antibodies that alter the immune system, also can suppress abnormal immune system activity.
Topical medications
Topical medications are creams, ointments, gels, lotions or patches that you apply directly on your skin to provide relief from nerve pain and inflammation. The active drugs in these medications are absorbed through the skin and provide localized pain relief.
Two types of topical medications used to treat neuropathy pain are:
- Local anesthetics
- Analgesics
Local anesthetics are used to treat localized pain. They work by numbing the area and blocking the pain where they are applied. Some local anesthetics are:
Nonprescription topical pain relievers (analgesics) — which are rubbed on the skin — are available to treat pain from neuropathy. These medications contain capsaicin (Capzasin-P, Dolorac, Zostrix® are brand names). A substance made from the seeds of hot chili peppers, capsaicin may reduce the ability of nerve cells to transmit pain messages to the brain. Capsaicin and other topical pain relievers provide temporary relief from minor pain located close to the skin’s surface.
Transcutaneous Electronic Nerve Stimulation (TENS)
Transcutaneous electronic nerve stimulation (TENS) is a method of therapy that may be used to treat nerve pain. It works by inhibiting pain signals from reaching the brain. It is a drug-free therapy that works by placing very small electrical impulses on specific nerve paths. The electrical impulses are delivered to the nerves through electrodes that are placed on the skin. Although it doesn’t work for everyone or all types of pain, TENS may be prescribed in combination with other treatments, primarily to provide relief from acute forms of nerve pain.
Prescription medications for neuropathy
When over-the-counter pain medications do not relieve the pain associated with peripheral neuropathy, other types of medications and therapies are available, including prescription nonsteroidal anti-inflammatory drugs, narcotics, antidepressants, and topical medications.
Sometimes, drugs developed and used to control other conditions are effective pain relievers. In addition to relieving depression, many antidepressant drugs can relieve chronic pain. These drugs also may improve sleep quality, which may in turn help reduce pain. In some cases, antidepressants work by treating accompanying depression that makes chronic pain more difficult to handle.
- Selective Serotonin Reuptake Inhibitors (SSRIs)
- Serotonin and Norepinephrine Reuptake Inhibitors (SNRIs) (e.g.,Cymbalta®)
- Norepinephrine Reuptake Inhibitors (e.g., Wellbutrin®)
- Serotonin Receptor Modulators (SRM)
Alternative therapies for peripheral neuropathy
Many patients find that complementary and alternative therapies help manage pain caused by peripheral neuropathy. Complementary and alternative therapies are drug-free treatments that are non-invasive and support the idea that the body will work to heal itself. They may be used alone or may be combined with other medications and treatments.
Below are some of the most commonly used therapies. You are strongly encouraged to consult a neurologist with any questions or comments you have regarding your condition. The best care can only be given by a qualified provider who knows you personally.
Acupuncture
Acupuncture is an ancient Chinese treatment that is performed today throughout the United States and Europe. Acupuncture involves inserting very thin needles into the body at specific points. Many people believe that acupuncture is an effective therapy to reduce pain. For some people with peripheral neuropathy, acupuncture acts as a complementary therapy because it may reduce the need to take pain-relieving drugs. Presently, research results are mixed as to whether or not acupuncture reduces chronic pain. A list of doctors that practice acupuncture is available from The American Academy of Medical Acupuncture (https://www.medicalacupuncture.org).
Biofeedback
Biofeedback is a therapy that uses an electrical machine to help you identify, monitor and learn to consciously manage your body’s physiological responses. Biofeedback helps people learn to alter activities usually controlled by the autonomic nervous system such as heart rate, blood pressure, and muscle activity. It also can be used to learn relaxation techniques that can reduce stress, headaches and chronic pain. Biofeedback therapy enables people to learn how to consciously manipulate a body function by using feedback gathered by electronic sensors that measure various body functions such as brain waves, temperature, heart rate and muscle tension. The information provided by the electronic instruments enables a person to learn ways to control, reduce or avert certain physical reactions such as those that increase feelings of stress and pain. Certified biofeedback therapists monitor the electronic equipment and train patients in the most effective techniques to control their specific symptoms.
Ergonomics and Splints
Splints can be helpful for people suffering from muscle weakness as the result of peripheral neuropathy. Also, making ergonomic changes to one’s workplace may reduce the symptoms of carpal tunnel, and help alleviate the pain from peripheral neuropathy.
Relaxation techniques
Relaxation techniques are designed to release tension that could make pain worse. A number of techniques exist including breathing exercises, visualization, meditation, massage and yoga.
Tactile defensiveness
Ayres (1972) recommended a course of sensory stimulation. Designed to stimulate participants’ higher cortical centers. This helped them integrate threatening tactile input with knowledge about the situation and other sensations. Integration let participants recognize seemingly threatening input as harmless.
Occupational therapists use sensory integration treatment. Deep pressure, designed to facilitate habituation, increased tolerance for other types of stimuli. Studies of sensory integration techniques indicate generalized improvements in the sensory modulation abilities of an adult and children.
Hyperacusis treatment
Tinnitus Retraining Therapy may ameliorate hyperacusis and tinnitus.
Distraction in traumatic brain injury client with sensory defensiveness was aggressive in the presence of loud noises. Distracting or redirecting him reduced aggressive responses.
Desensitization for in traumatic brain injury clients: Meyerson and Frank (1987) described a desensitization program for a client with William’s syndrome.
Tape record aversive sounds, then play them back with gradually increasing loudness, to increase a client’s ability to tolerate them.
Feeding aversion treatment
Oral-facial hypersensitivity: Gilmore et al. (2003) and Bahr (2001); Desensitization programs helped clients eat and tolerate oral hygiene.
Tonic biting reflex: in children with cerebral palsy, Alexander (1987) reported using deep pressure to the sides and biting surfaces of gums and teeth.
Photophobia treatment
Tinted lenses, may reduce hypersensitivity to light.
Jackowski et al (1996) found that light filtering lenses improved reading rate by 39%.
This might help clients carry out job or household responsibilities requiring reading.
Modifying the environment
Modify the environment to reduce the frequency and intensity of aversive stimuli. An adult with a traumatic brain injury, was intolerant of touch and noise. His daily routines were changed. Bathing, for example, was facilitated by having him take baths instead of showers (Fluharty and Glassman, 2001).
References- Bohnen N, Twijnstra A, Wijnen G, Jolles J. Recovery from visual and acoustic hyperaesthesia after mild head injury in relation to patterns of behavioural dysfunction. J Neurol Neurosurg Psychiatry. 1992;55(3):222–224. doi:10.1136/jnnp.55.3.222 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1014733/pdf/jnnpsyc00488-0052.pdf
- J. Stone, M. Vermeulen, in Handbook of Clinical Neurology, 2016