Anal pain
Anal pain is defined as pain originating from the anal canal or the perianal area that can be caused by variety of medical problems. Anal pain is a common complaint. Although most causes of anal pain aren’t serious, the pain itself can be severe because of the many nerve endings in the perianal region. Many conditions that cause anal pain also may cause rectal bleeding, which is usually more frightening than serious.
Anal pain can have many causes, do not self-diagnose, it’s best that you see a doctor. Your doctor may recommend changes to your diet or arrange for tests to look for a cause of your anal pain.
Sometimes surgery or other treatments may be needed if the pain is caused by severe anal fissures, piles or fistulas.
Non-serious anal pain usually can be treated with nonprescription pain relievers and hot water soaks, also called sitz baths.
See a doctor if you’re in a lot of pain or it does not get better.
Ask for an urgent doctor’s appointment if:
- you have severe anal pain and you have a high temperature or feel hot and shivery
- your poop is black or dark red
Go to your local emergency room or call your local emergency services number for an ambulance if:
- you’re bleeding non-stop from your bottom
- there’s a lot of blood coming from your bottom – for example, the toilet water turns red or you see large blood clots
The anus
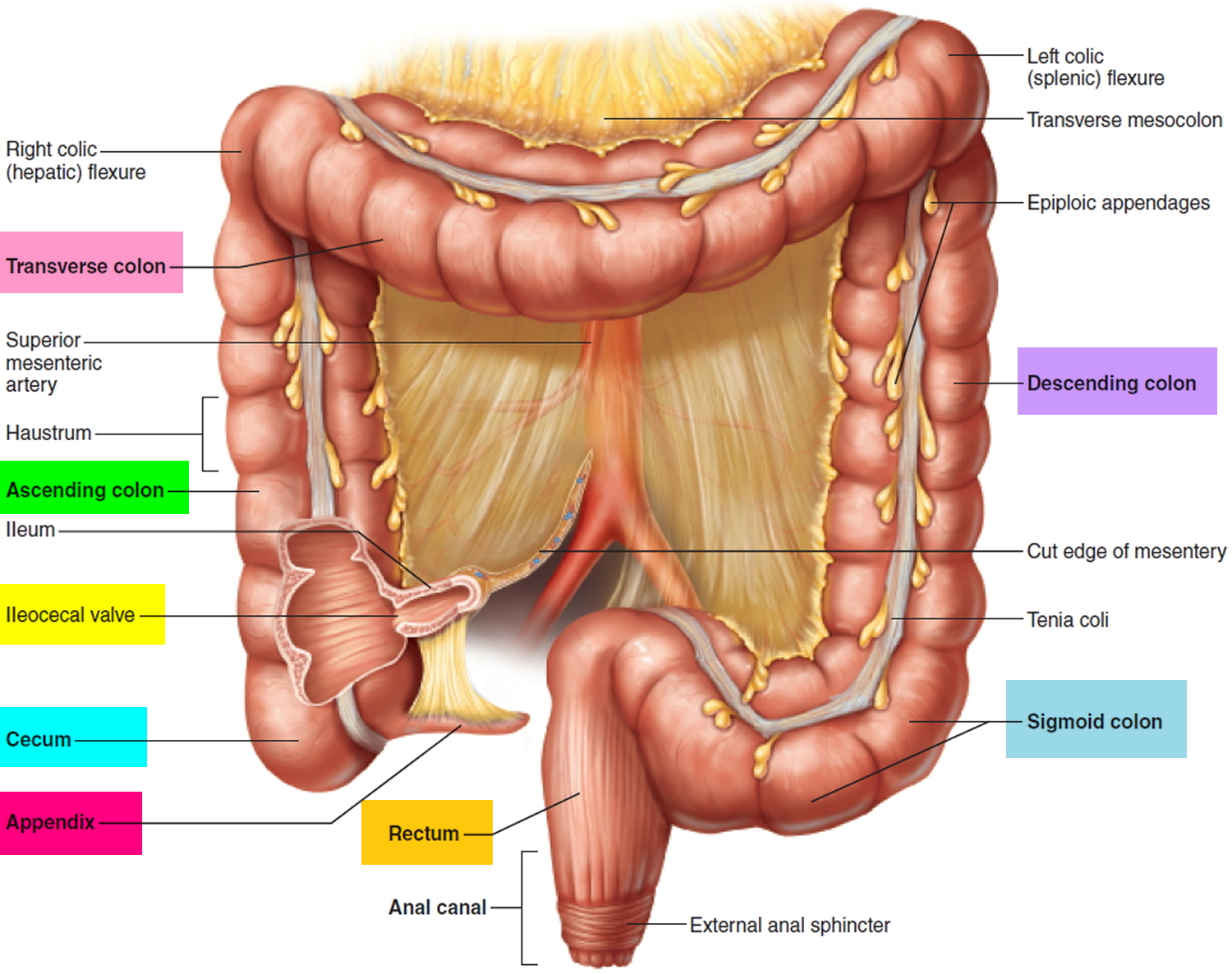
The anus is connected to the rectum by the anal canal. The anus is the continuation of the large intestine (the colon or large bowel) inferior to the rectum. It’s where the end of the intestines connect to the outside of the body.
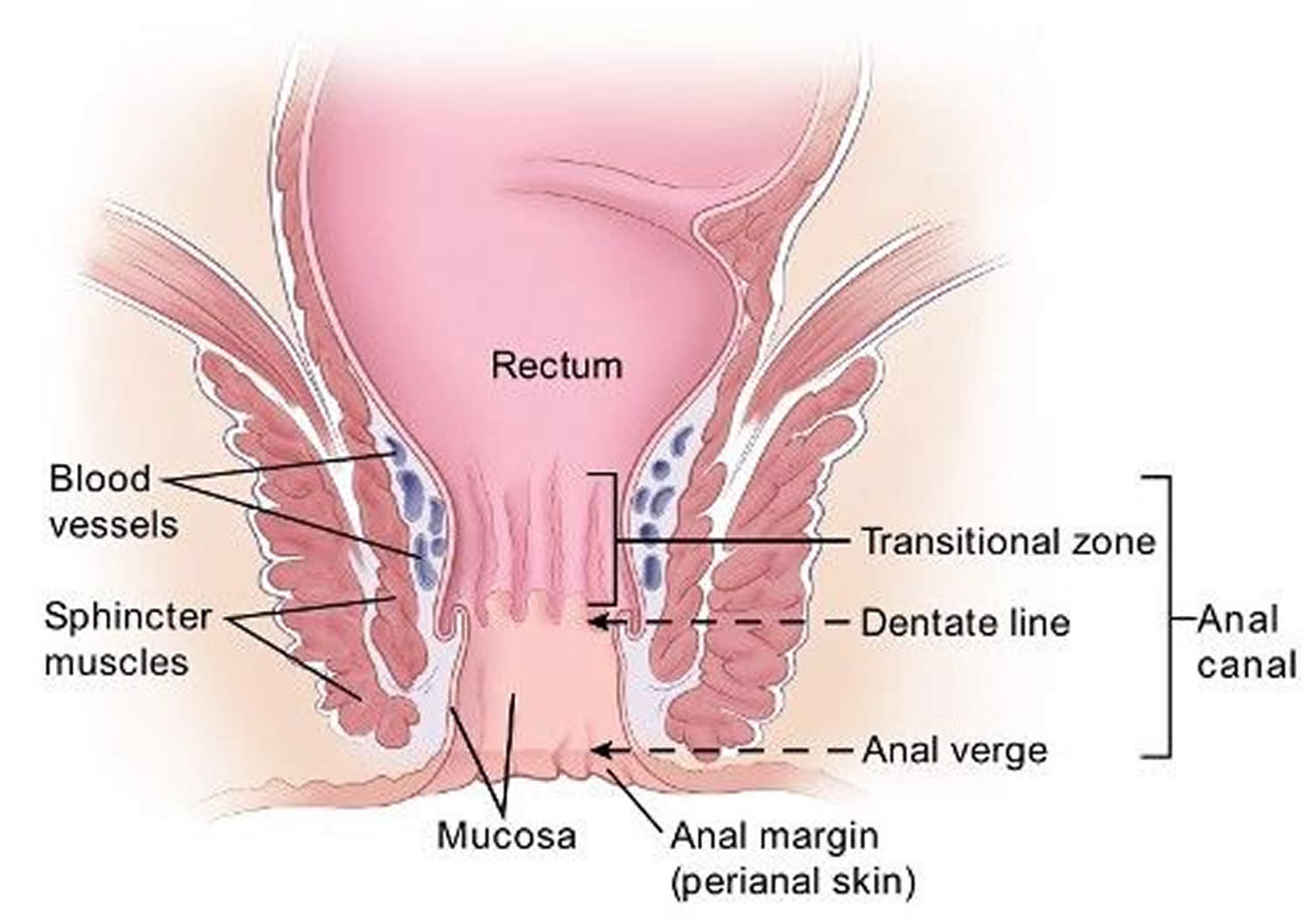
The anal canal is about 1-1/2 inches (about 3 to 5 cm) long, it begins where the rectum passes through the levator ani (the muscle that forms the pelvic floor) and goes to the anal verge. The anal verge is where the anal canal connects to the outside skin at the anus. This skin around the anal verge is called the perianal skin (previously called the anal margin). The anal canal has two ring-shaped muscles (called sphincter muscles – an internal and external anal sphincter) that keep the anus closed and prevent stool from leaking out.
As food is digested, it passes from the stomach to the small intestine. It then moves from the small intestine into the main part of the large intestine (called the colon). The colon absorbs water and salt from the digested food. The waste matter that’s left after going through the colon is known as feces or stool. Stool is stored in the last part of the large intestine, called the rectum. From there, stool is passed out of the body through the anus as a bowel movement.
The inner lining of the anal canal is the mucosa. Most anal cancers start from cells in the mucosa. Glands and ducts (tubes leading from the glands) are found under the mucosa. The glands make mucus, which acts as a lubricating fluid. Anal cancers that start from cells in the glands are called adenocarcinomas.
The anal canal changes as it goes from the rectum to the anal verge. The parts of the anus include the:
- Cells above the anal canal (in the rectum) and in the part of the anal canal close to the rectum are shaped like tiny columns.
- Most cells near the middle of the anal canal are shaped like cubes and are called transitional cells. This area is called the transitional zone – this is where the rectum meets the anal canal.
- About midway down the anal canal is the dentate line, which is where most of the anal glands empty into the anus.
- Below the dentate line are flat (squamous) cells.
- At the anal verge, the squamous cells of the lower anal canal merge with the skin just outside the anus. This skin around the anal verge called the perianal skin or the anal margin, is also made up of squamous cells, but it also contains sweat glands and hair follicles, which are not found in the lining of the lower anal canal. The anal margin is the lower part of the anal canal and it contains muscles called the anal sphincters. You have an internal and external anal sphincter. They are the muscles that control your bowel movements.
Figure 1. Rectum
Figure 2. Anus anatomy
Anal pain causes
Anal pain causes include:
- Anal cancer
- Anal fissure (a small tear in the lining of the anal canal)
- Anal fistula (an abnormal channel between the anus or rectum usually to the skin near the anus)
- Anal incontinence (accidental bowel leakage)
- Anal itching (pruritus ani)
- Anal sex
- Anal or rectal stricture (narrowing that may occur from scarring, severe inflammation or cancer)
- Cancers of the anal margin and perianal skin (e.g., squamous cell carcinoma, Bowen’s disease [nonkeratinizing intraepithelial squamous-cell carcinoma of the perianal skin], basal cell carcinoma, perianal Paget’s disease [intraepithelial adenocarcinoma], large condyloma acuminata) 1
- Constipation
- Crohn’s disease
- Chronic idiopathic anal pain 2
- Diarrhea (causing anal irritation)
- Fecal impaction (a mass of hardened stool in the rectum due to chronic constipation)
- Genital warts
- Hemorrhoids (swollen and inflamed veins in your anus or rectum)
- Levator ani syndrome (spasm in the muscles that surround the anus) 3, 4
- Perianal abscess (pus in the deep tissue around the anus)
- Perianal hematoma (a collection of blood in the perianal tissue caused by a ruptured vein, sometimes called an external hemorrhoid)
- Perianal mantle cell lymphoma 5
- Proctalgia fugax (fleeting pain due to rectal muscle spasm)
- Proctitis (inflammation of the lining of the rectum)
- Several sexually transmitted diseases (STDs) can infect the rectum and cause proctitis, including:
- Other infections in the rectum that can cause proctitis include:
- Infections that cause food poisoning, such as Salmonella, Shigella, and Campylobacter infections
- Clostridioides difficile (C. diff) infection, which most often occurs while a person is taking antibiotics or shortly thereafter
- Solitary rectal ulcer syndrome (ulcer of the rectum)
- Sexually transmitted infection (STI)
- Tailbone pain, also known as coccydynia or coccygodynia
- Thrombosed hemorrhoid (blood clot in a hemorrhoid)
- Trauma
- Ulcerative colitis (a type of inflammatory bowel disease)
- Ulcerative proctitis (a type of ulcerative colitis)
Anal pain diagnosis
Your doctor will likely ask about your medical history including your toilet habits and perform a physical exam, including a gentle inspection of the anal region. Often the tear is visible by gently parting your buttocks.
A digital rectal examination (DRE), where a doctor inserts a lubricated, gloved finger into your bottom to feel for abnormalities, is not usually used to diagnose anal fissures as it’s likely to be painful.
If your doctor thinks you might have anal fistula, they can refer you to a specialist called a colorectal surgeon for further tests to confirm the diagnosis and determine the most suitable treatment.
Your doctor may recommend further testing if he or she thinks you have an underlying condition:
- Anoscopy. An anoscope is a tubular device inserted into the anus to help your doctor visualize the rectum and anus.
- Flexible sigmoidoscopy. Your doctor will insert a thin, flexible tube with a tiny video into the bottom portion of your colon. This test may be done if you’re younger than 50 and have no risk factors for intestinal diseases or colon cancer.
- Colonoscopy. Your doctor will insert a flexible tube into your rectum to inspect the entire colon. This test may be done if you are older than age 50 or you have risk factors for colon cancer, signs of other conditions, or other symptoms such as abdominal pain or diarrhea.
Key point: If a mass is seen on external examination or anoscopy and there is any question of pathology such as malignancy, the area should be evaluated by a physician familiar with diseases of the anus and rectum to further determine whether biopsy is indicated.
Anal pain treatment
There are many causes of anal pain, therefore it’s best that you see your doctor if your anal pain lasts more than a few days and treatments at home aren’t helping. Also make an appointment with your doctor if your anal pain comes with a change in bowel habits or rectal bleeding. See your doctor for rectal bleeding, especially if you’re older than 40, to rule out rare but serious conditions such as colon cancer.
See your doctor if you think you have an anal fissure. Do not let embarrassment stop you seeking help. Anal fissures are a common problem doctors are used to dealing with. Most anal fissures get better without treatment, but your doctor will want to rule out other conditions with similar symptoms, such as piles (hemorrhoids). Your doctor can also tell you about self-help measures and treatments that can relieve your symptoms and reduce the risk of fissures coming back.
A hemorrhoid that develops quickly or is especially painful may have formed a blood clot inside, called a thrombosed hemorrhoid. Removing the clot within the first 48 hours often gives the most relief, so request a timely appointment with your health care team. The blood clot of a thrombosed hemorrhoid, although painful, can’t break loose and travel. It won’t cause any of the complications associated with blood clots that form in other parts of the body, such as stroke.
Rectal pain treatment at home
Depending on the cause of your anal pain, there are some measures you can try at home to get relief. They include:
- Drink lots of fluid and eat high-fiber foods to keep your poop soft. Eating more fruits, vegetables and whole grains.
- Daily exercise.
- Taking stool softeners, if needed, to help with bowel movements, reduce straining and ease pain.
- Sitting in a tub of hot water up to your hips, known as a sitz bath, for 10 to 15 minutes two or three times a day. This helps ease the pain of hemorrhoids, anal fissures or rectal muscle spasms.
- Applying nonprescription hemorrhoid cream for hemorrhoids or hydrocortisone cream for anal fissures.
- Taking a nonprescription pain reliever such as acetaminophen (Tylenol, others), aspirin or ibuprofen (Advil, Motrin IB, others).
Dietary Fiber
Dietary fiber is a type of carbohydrate made up of many sugar molecules linked together. But unlike other carbohydrates, dietary fiber is bound together in such a way that it cannot be easily digested in the small intestine.
There are two types of dietary fiber:
- Soluble dietary fiber dissolves in water to form a thick gel-like substance in the stomach. It is broken down by bacteria in the large intestine and provides some calories. Soluble dietary fiber can interfere with the absorption of dietary fat and cholesterol. This, in turn, can help lower low-density lipoprotein (LDL or “bad”) cholesterol levels in the blood. Soluble fiber can also slow digestion and the rate at which carbohydrates and other nutrients are absorbed into the bloodstream. This can help control the level of blood glucose (often referred to as blood sugar) by preventing rapid rises in blood glucose following a meal.
- Insoluble dietary fiber does not dissolve in water and may pass through the gastrointestinal tract relatively intact and, therefore, is not a source of calories. Insoluble dietary fiber can speed up the movement of food and waste through the digestive system.
Both soluble and insoluble dietary fiber can make you feel full, which may lower your calorie intake by helping you eat less and yet stay satisfied longer.
Diets higher in dietary fiber can increase the frequency of bowel movements and can reduce the risk of developing cardiovascular disease.
The US Department of Agriculture and US Department of Health and Human Services recommend that you eat 25 g to 40 g of fiber daily, but most people get less than half this recommendation 7. Adequate fiber intake is important for many reasons:
- Fiber helps regulate bowel movements by softening hard stool to reduce constipation and adding bulk to loose stool to reduce diarrhea
- Common anal problems such as anal fissures and hemorrhoids are caused by inadequate fiber and water intake
- Adequate fiber will reduce the risk of developing colorectal cancer, diverticulosis, and complications of diverticulitis
- Adequate fiber will reduce cholesterol.
Table 1. Food Sources of Dietary Fiber
| FOOD ab | STANDARD PORTION c | CALORIES | FIBER (g) | |
|---|---|---|---|---|
| Grains | ||||
| Ready-to-eat cereal, high fiber, unsweetened | 1/2 cup | 62 | 14 | |
| Ready-to-eat cereal, whole grain kernels | 1/2 cup | 209 | 7.5 | |
| Ready-to-eat cereal, wheat, shredded | 1 cup | 172 | 6.2 | |
| Popcorn | 3 cups | 169 | 5.8 | |
| Ready-to-eat cereal, bran flakes | 3/4 cup | 98 | 5.5 | |
| Bulgur, cooked | 1/2 cup | 76 | 4.1 | |
| Spelt, cooked | 1/2 cup | 123 | 3.8 | |
| Teff, cooked | 1/2 cup | 128 | 3.6 | |
| Barley, pearled, cooked | 1/2 cup | 97 | 3 | |
| Ready-to-eat cereal, toasted oat | 1 cup | 111 | 3 | |
| Oat bran | 1/2 cup | 44 | 2.9 | |
| Crackers, whole wheat | 1 ounce | 122 | 2.9 | |
| Chapati or roti, whole wheat | 1 ounce | 85 | 2.8 | |
| Tortillas, whole wheat | 1 ounce | 88 | 2.8 | |
| Vegetables | ||||
| Artichoke, cooked | 1 cup | 89 | 9.6 | |
| Navy beans, cooked | 1/2 cup | 128 | 9.6 | |
| Small white beans, cooked | 1/2 cup | 127 | 9.3 | |
| Yellow beans, cooked | 1/2 cup | 128 | 9.2 | |
| Lima beans, cooked | 1 cup | 209 | 9.2 | |
| Green peas, cooked | 1 cup | 134 | 8.8 | |
| Adzuki beans, cooked | 1/2 cup | 147 | 8.4 | |
| French beans, cooked | 1/2 cup | 114 | 8.3 | |
| Split peas, cooked | 1/2 cup | 116 | 8.2 | |
| Breadfruit, cooked | 1 cup | 170 | 8 | |
| Lentils, cooked | 1/2 cup | 115 | 7.8 | |
| Lupini beans, cooked | 1/2 cup | 115 | 7.8 | |
| Mung beans, cooked | 1/2 cup | 106 | 7.7 | |
| Black turtle beans, cooked | 1/2 cup | 120 | 7.7 | |
| Pinto beans, cooked | 1/2 cup | 123 | 7.7 | |
| Cranberry (roman) beans, cooked | 1/2 cup | 121 | 7.6 | |
| Black beans, cooked | 1/2 cup | 114 | 7.5 | |
| Fufu, cooked | 1 cup | 398 | 7.4 | |
| Pumpkin, canned | 1 cup | 83 | 7.1 | |
| Taro root (dasheen or yautia), cooked | 1 cup | 187 | 6.7 | |
| Brussels sprouts, cooked | 1 cup | 65 | 6.4 | |
| Chickpeas (garbanzo beans), cooked | 1/2 cup | 135 | 6.3 | |
| Sweet potato, cooked | 1 cup | 190 | 6.3 | |
| Great northern beans, cooked | 1/2 cup | 105 | 6.2 | |
| Parsnips, cooked | 1 cup | 110 | 6.2 | |
| Nettles, cooked | 1 cup | 37 | 6.1 | |
| Jicama, raw | 1 cup | 46 | 5.9 | |
| Winter squash, cooked | 1 cup | 76 | 5.7 | |
| Pigeon peas, cooked | 1/2 cup | 102 | 5.7 | |
| Kidney beans, cooked | 1/2 cup | 113 | 5.7 | |
| White beans, cooked | 1/2 cup | 125 | 5.7 | |
| Black-eyed peas, dried and cooked | 1/2 cup | 99 | 5.6 | |
| Cowpeas, dried and cooked | 1/2 cup | 99 | 5.6 | |
| Yam, cooked | 1 cup | 158 | 5.3 | |
| Broccoli, cooked | 1 cup | 54 | 5.2 | |
| Tree fern, cooked | 1 cup | 56 | 5.2 | |
| Luffa gourd, cooked | 1 cup | 100 | 5.2 | |
| Soybeans, cooked | 1/2 cup | 148 | 5.2 | |
| Turnip greens, cooked | 1 cup | 29 | 5 | |
| Drumstick pods (moringa), cooked | 1 cup | 42 | 5 | |
| Avocado | 1/2 cup | 120 | 5 | |
| Cauliflower, cooked | 1 cup | 34 | 4.9 | |
| Kohlrabi, raw | 1 cup | 36 | 4.9 | |
| Carrots, cooked | 1 cup | 54 | 4.8 | |
| Collard greens, cooked | 1 cup | 63 | 4.8 | |
| Kale, cooked | 1 cup | 43 | 4.7 | |
| Fava beans, cooked | 1/2 cup | 94 | 4.6 | |
| Chayote (mirliton), cooked | 1 cup | 38 | 4.5 | |
| Snow peas, cooked | 1 cup | 67 | 4.5 | |
| Pink beans, cooked | 1/2 cup | 126 | 4.5 | |
| Spinach, cooked | 1 cup | 41 | 4.3 | |
| Escarole, cooked | 1 cup | 22 | 4.2 | |
| Beet greens, cooked | 1 cup | 39 | 4.2 | |
| Salsify, cooked | 1 cup | 92 | 4.2 | |
| Cabbage, savoy, cooked | 1 cup | 35 | 4.1 | |
| Cabbage, red, cooked | 1 cup | 41 | 4.1 | |
| Wax beans, snap, cooked | 1 cup | 44 | 4.1 | |
| Edamame, cooked | 1/2 cup | 94 | 4.1 | |
| Okra, cooked | 1 cup | 36 | 4 | |
| Green beans, snap, cooked | 1 cup | 44 | 4 | |
| Hominy, canned | 1 cup | 115 | 4 | |
| Corn, cooked | 1 cup | 134 | 4 | |
| Potato, baked, with skin | 1 medium | 161 | 3.9 | |
| Lambsquarters, cooked | 1 cup | 58 | 3.8 | |
| Lotus root, cooked | 1 cup | 108 | 3.8 | |
| Swiss chard, cooked | 1 cup | 35 | 3.7 | |
| Mustard spinach, cooked | 1 cup | 29 | 3.6 | |
| Carrots, raw | 1 cup | 52 | 3.6 | |
| Hearts of palm, canned | 1 cup | 41 | 3.5 | |
| Mushrooms, cooked | 1 cup | 44 | 3.4 | |
| Bamboo shoots, raw | 1 cup | 41 | 3.3 | |
| Yardlong beans, cooked | 1/2 cup | 101 | 3.3 | |
| Turnip, cooked | 1 cup | 34 | 3.1 | |
| Red bell pepper, raw | 1 cup | 39 | 3.1 | |
| Rutabaga, cooked | 1 cup | 51 | 3.1 | |
| Plantains, cooked | 1 cup | 215 | 3.1 | |
| Nopales, cooked | 1 cup | 22 | 3 | |
| Dandelion greens, cooked | 1 cup | 35 | 3 | |
| Cassava (yuca), cooked | 1 cup | 267 | 3 | |
| Asparagus, cooked | 1 cup | 32 | 2.9 | |
| Taro leaves, cooked | 1 cup | 35 | 2.9 | |
| Onions, cooked | 1 cup | 92 | 2.9 | |
| Cabbage, cooked | 1 cup | 34 | 2.8 | |
| Mustard greens, cooked | 1 cup | 36 | 2.8 | |
| Beets, cooked | 1 cup | 49 | 2.8 | |
| Celeriac, raw | 1 cup | 66 | 2.8 | |
| Fruits | ||||
| Sapote or Sapodilla | 1 cup | 217 | 9.5 | |
| Durian | 1 cup | 357 | 9.2 | |
| Guava | 1 cup | 112 | 8.9 | |
| Nance | 1 cup | 82 | 8.4 | |
| Raspberries | 1 cup | 64 | 8 | |
| Loganberries | 1 cup | 81 | 7.8 | |
| Blackberries | 1 cup | 62 | 7.6 | |
| Soursop | 1 cup | 148 | 7.4 | |
| Boysenberries | 1 cup | 66 | 7 | |
| Gooseberries | 1 cup | 66 | 6.5 | |
| Pear, Asian | 1 medium | 75 | 6.5 | |
| Blueberries, wild | 1 cup | 80 | 6.2 | |
| Passion fruit | 1/4 cup | 57 | 6.1 | |
| Persimmon | 1 fruit | 118 | 6 | |
| Pear | 1 medium | 103 | 5.5 | |
| Kiwifruit | 1 cup | 110 | 5.4 | |
| Grapefruit | 1 fruit | 130 | 5 | |
| Apple, with skin | 1 medium | 104 | 4.8 | |
| Cherimoya | 1 cup | 120 | 4.8 | |
| Durian | 1/2 cup | 179 | 4.6 | |
| Starfruit | 1 cup | 41 | 3.7 | |
| Orange | 1 medium | 73 | 3.7 | |
| Figs, dried | 1/4 cup | 93 | 3.7 | |
| Blueberries | 1 cup | 84 | 3.6 | |
| Pomegranate seeds | 1/2 cup | 72 | 3.5 | |
| Mandarin orange | 1 cup | 103 | 3.5 | |
| Tangerine (tangelo) | 1 cup | 103 | 3.5 | |
| Pears, dried | 1/4 cup | 118 | 3.4 | |
| Peaches, dried | 1/4 cup | 96 | 3.3 | |
| Banana | 1 medium | 112 | 3.2 | |
| Apricots | 1 cup | 74 | 3.1 | |
| Prunes or dried plum | 1/4 cup | 105 | 3.1 | |
| Strawberries | 1 cup | 49 | 3 | |
| Dates | 1/4 cup | 104 | 3 | |
| Blueberries, dried | 1/4 cup | 127 | 3 | |
| Cherries | 1 cup | 87 | 2.9 | |
| Protein Foods | ||||
| Wocas, yellow pond lily seeds | 1 ounce | 102 | 5.4 | |
| Pumpkin seeds, whole | 1 ounce | 126 | 5.2 | |
| Coconut | 1 ounce | 187 | 4.6 | |
| Chia seeds | 1 Tbsp | 58 | 4.1 | |
| Almonds | 1 ounce | 164 | 3.5 | |
| Chestnuts | 1 ounce | 106 | 3.3 | |
| Sunflower seeds | 1 ounce | 165 | 3.1 | |
| Pine nuts | 1 ounce | 178 | 3 | |
| Pistachio nuts | 1 ounce | 162 | 2.9 | |
| Flax seeds | 1 Tbsp | 55 | 2.8 | |
| Hazelnuts (filberts) | 1 ounce | 178 | 2.8 | |
Footnotes:
a Some fortified foods and beverages are included. Other fortified options may exist on the market, but not all fortified foods are nutrient-dense. For example, some foods with added sugars may be fortified and would not be examples in the lists provided here.
b Some foods or beverages are not appropriate for all ages, (e.g., nuts, popcorn), particularly young children for whom some foods could be a choking hazard.
c Portions listed are not recommended serving sizes. Two lists—in ‘standard’ and ‘smaller’ portions–are provided for each dietary component. Standard portions provide at least 2.8 g of dietary fiber. Smaller portions are generally one half of a standard portion.
[Source 8 ]Table 2. Fiber supplementation instructions
| My daily fiber intake goal | 25–40 g daily |
|---|---|
| The US Department of Agriculture and US Department of Health and Human Services recommend that I eat 25 g to 40 g of fiber DAILY | Adequate fiber will regulate my bowel movements by softening hard stool and reducing the frequency of constipation adding bulk to loose stool and reducing the frequency of diarrhea. Adequate fiber will improve my anal problems and bleeding by softening hard stool and making bowel movements less traumatic thickening loose stool and making bowel movements less traumatic. Adequate fiber will reduce my risk of developing colon and rectal cancer diverticulosis complications of diverticulitis: Perforation, infection, emergency surgery. Adequate fiber will reduce my cholesterol |
| How much fiber is in the food I eat? | The fiber content in foods that you eat can be found on the “Nutrition Facts” label for processed foods. For fresh foods, fruits, and vegetables, there are a variety of Web sites that can give you the amount of fiber per serving. |
| Go slow and keep it up | Gradually work your way up to taking 20 g of fiber daily in the form of a fiber supplement AND increase fiber in your diet so that you are eating at least 10 g to 20 g of dietary fiber daily. Fiber supplementa: 20 g daily Dietary fiber: + 10–20 g daily Total fiber intake: 25–40 g daily |
| Slow and steady fiber supplement ramp-up plan | Week 1: Start counting the amount of fiber you consume in your diet on a daily basis. Purchase a fiber product that you will be able to take every day for the rest of your life. Read the label to check the fiber content. Many fiber products, especially fiber pills, have very small amounts of fiber. Choose a fiber product with 5 g or more of fiber per serving. Start drinking 8 to 10 glasses of water daily. |
| Week 2: Supplement your diet with 5 g of additional fiber daily. Drink 8 to 10 eight-oz. glasses of water daily. | |
| Week 3: Supplement your diet with 10 g of additional fiber daily. Drink 8 to 10 glasses of water daily. | |
| Week 4 and beyond: Continue to increase the amount of additional fiber daily by 5 g per week until you reach your goal of 25 g to 40 g of fiber daily for life. TIP: If you feel bloated or develop excessive gas, you are increasing your daily fiber too quickly. You may need to increase your daily fiber over a longer period of time. |
Footnotes: a Common fiber supplements: Metamucil, Konsyl, Citrucel, Fiber One. Choose the fiber supplement that works best for you. Be sure to calculate the fiber amount per serving size. Choose a fiber supplement that you would be willing to take every day as a 20-g dose (goal at the end of the ramp-up period). If you experience diarrhea with a natural fiber supplement or fiber supplement that claims “easy to take/dissolves in water,” consider changing to one of the above brand names because some natural fiber supplements contain natural laxatives as well.
Warning: If you take Coumadin (warfarin), please be sure to speak with your primary care physician or cardiologist before starting a fiber supplement because fiber may interfere with your Coumadin international normalized ratio levels.
[Source 9 ] References- Wietfeldt ED, Thiele J. Malignancies of the anal margin and perianal skin. Clin Colon Rectal Surg. 2009 May;22(2):127-35. doi: 10.1055/s-0029-1223845
- Mao W, Liao X, Wu W, Yu Y, Yang G. The Clinical Characteristics of Patients with Chronic Idiopathic Anal Pain. Open Med (Wars). 2017 May 4;12:92-98. doi: 10.1515/med-2017-0015
- Whitehead WE, Wald A, Diamant NE, Enck P, Pemberton JH, Rao SSC. Functional disorders of the anus and rectum. In: Drossman DA, Corazziari E, Talley NJ, Thompson WG, Whitehead WE, editors. Rome II: The Functional Gastrointestinal Disorders. 2. McLean, VA: Degnon Associates; 2000. pp. 483–501.
- Mastragostino P, Lee AD, Battaglia PJ. Perianal abscess mimicking levator ani syndrome: a case report and approach to the differential diagnosis of anorectal pain. J Can Chiropr Assoc. 2017 Aug;61(2):145-152. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5596975
- Gulcu B, Ozer A, Nazlioglu HO, Ozturk E, Yilmazlar T. Perianal mantle cell lymphoma mimicking an external thrombosed hemorrhoid: a case report. J Med Case Rep. 2014 Feb 5;8:40. doi: 10.1186/1752-1947-8-40
- Pfäfflin F, Wendisch D, Scherer R, Jürgens L, Godzick-Njomgang G, Tranter E, Tober-Lau P, Stegemann MS, Corman VM, Kurth F, Schürmann D. Monkeypox in-patients with severe anal pain. Infection. 2023 Apr;51(2):483-487. doi: 10.1007/s15010-022-01896-7
- Dietary Guidelines for Americans. https://www.dietaryguidelines.gov
- Food Sources of Dietary Fiber. https://www.dietaryguidelines.gov/resources/2020-2025-dietary-guidelines-online-materials/food-sources-select-nutrients/food-0
- Chang J, Mclemore E, Tejirian T. Anal Health Care Basics. Perm J. 2016 Fall;20(4):15-222. doi: 10.7812/TPP/15-222