What is hypersensitivity pneumonitis
Hypersensitivity pneumonitis also known as extrinsic allergic alveolitis, bird fancier’s lung, farmer’s lung, hot tub lung or humidifier lung, is a disease of your lungs caused by an allergy to certain dust (allergens) that you breathe in. In hypersensitivity pneumonitis your lungs become inflamed as an allergic reaction to inhaled dust, fungus, molds or chemicals. Commonly, these allergens are naturally occurring (organic). These allergens may be present at home, work or in the environment. These dusts contain fungus spores from moldy hay or bird droppings.
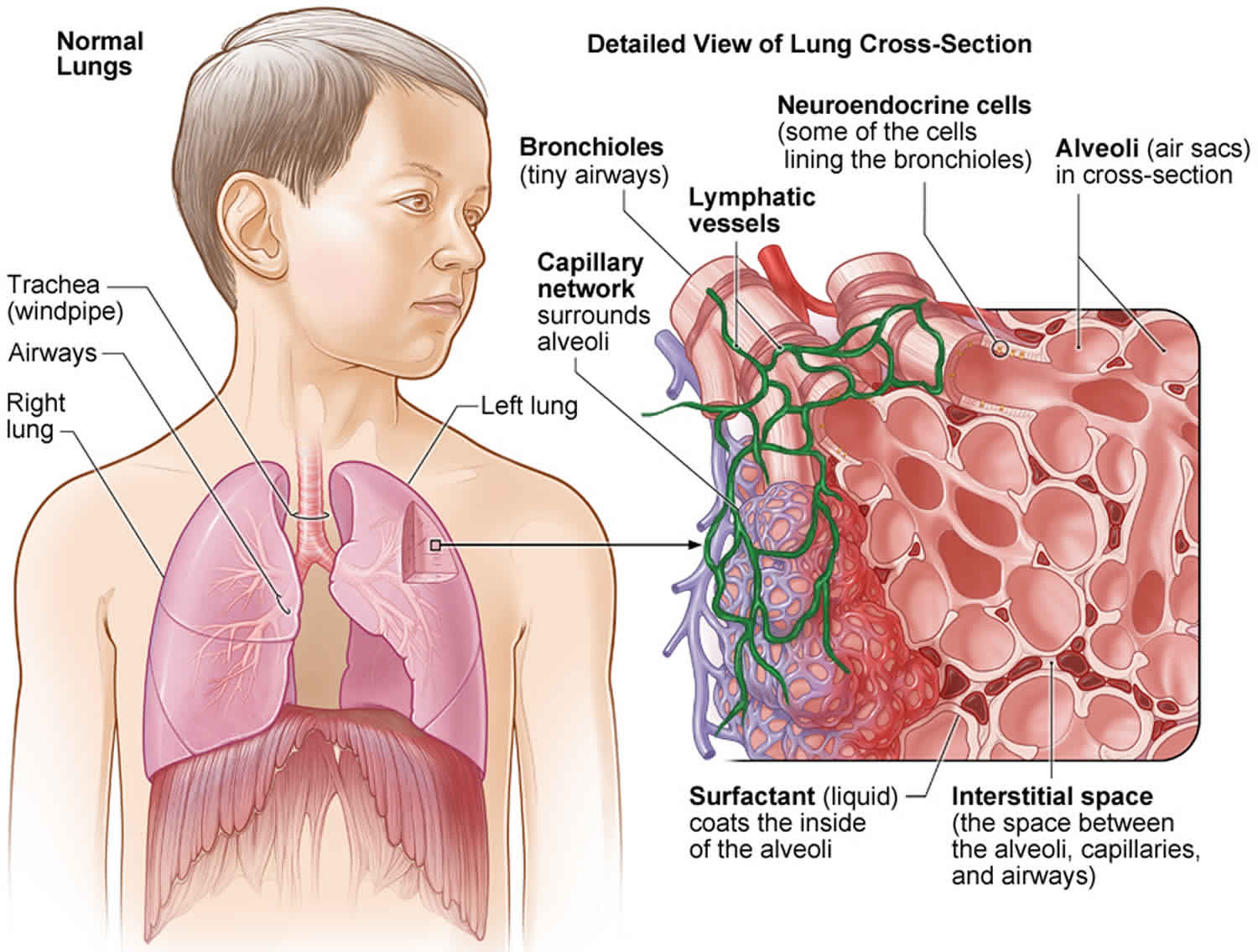
When you breathe in the dust that you are allergic to, you will not notice any problems the first time. Some individuals may develop symptoms after a large exposure to the dust or after repeated smaller exposures. The tiny air sacs in your lungs become inflamed as their walls fill with white blood cells and, occasionally, the air sacs may also fill with fluid. The inflammation gets better within a few days if you no longer breathe in those dusts. If you breathe in those dusts repeatedly, the inflammation in the lung continues. This may lead to some portions of the lung developing scar tissue. When your lungs have scar tissue, you may have trouble breathing normally.
Hypersensitivity pneumonitis can become a serious condition for some individuals whose lungs develop scarring. Lung scarring (also called pulmonary fibrosis) may occur in the later stages of the disease. The lung scarring is permanent. Unfortunately, there is no cure or effective treatment for chronic hypersensitivity pneumonitis or long-standing hypersensitivity pneumonitis. The good news is that if the hypersensitivity pneumonitise is caught in the early stages and if you avoid the dust, then it can be completely reversed. That is why it is very important to catch this disease in the early stages to prevent permanent lung damage.
The single most important thing that you can do is avoid the dust that causes the disease. If you do so, your lungs can return to normal function, as the disease is completely reversible in the early stages. Completely avoiding the dust is sometimes not possible, unless you remove yourself from the dust-causing environment. Your doctor may recommend completely avoiding the dust by relocating to a new home or job. If you have bird fancier’s lung, then it is possible you may have to give up your pet bird.
In patients who have severe cases, treatment may include prescription steroids, such as prednisone. You may be required to take this medication for up to 3 months and sometimes longer. Steroids may help with your symptoms; however, it will not cure the disease. Steroids can also cause certain side effects such as weight gain, thinning of the bones, cataracts, abnormal blood sugar levels and increased pressure in your eyes. Medications that supress immunity such as mycophenolate and azahtioprine show promise as steroid-sparing agents in some individuals to reduce or eliminate steroids. In end stage lung disease with advanced scarring, lung transplantation may be a consideration.
Hypersensitivity pneumonitis key facts:
- Hypersensitivity pneumonitis is caused by an allergy to certain dust (allergens) that you inhale.
- This allergy causes inflammation in your lungs
- If detected early, and you avoid the allergy-producing substance, the inflammation can be reversed.
- Sometimes hypersensitivity pneumonitis can cause lung scarring if it is not detected early and you continue to be exposed to the substances.
Figure 1. Normal lungs
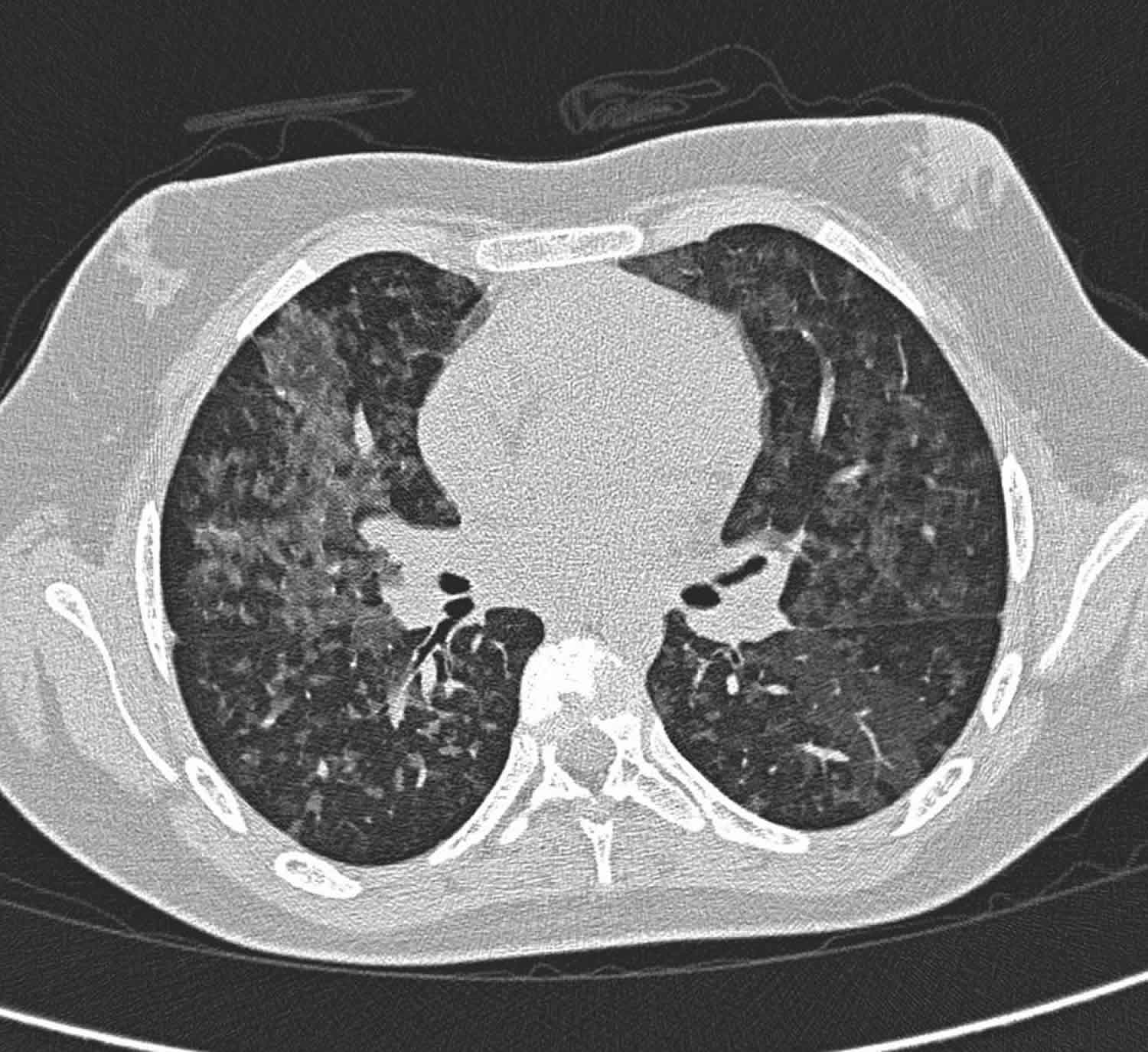
Figure 2. Hypersensitivity pneumonitis CT
Footnote: A 12 year old girl presented with hypoxia and poor expiratory effort with signs of peripheral gas trapping. Her chest X-ray reveals subtle perihilar alveolar infiltrate. Her history reveals she slept with her pet parrot. CT scan shows perihilar ground glass changes.
[Source 1 ]If you develop symptoms of hypersensitivity pneumonitis, contact your doctor. You may feel like you have caught the flu when the acute attack occurs. You may notice a dry cough, shortness of breath, chest tightness, fever, chills, or tiredness about 4 to 6 hours after you inhale the dust. Unlike the common flu, which most commonly occurs during October to May, hypersensitivity pneumonitis symptoms can occur during any time of the year. You may notice dry cough or shortness of breath on activity if you have repeated exposure to the dust. Your coworkers or family members may not have any symptoms but your lungs could still be allergic to some dust at workplace or home respectively.
Why does hypersensitivity pneumonitis only occur in some people?
If you have hypersensitivity pneumonitis, your body’s immune system reacts strongly to certain substances. Differences in the immune systems may explain why some people have strong reactions after breathing in certain substances, while others who breathe those same substances do not.
Acute hypersensitivity pneumonitis
Acute hypersensitivity pneumonitis refers to the acute form of hypersensitivity pneumonitis although this classification system has recently been challenged 2.
Fever, chills, myalgia, headaches, coughing, chest tightness, dyspnea, and leukocytosis can occur in various combinations. This typically occurs 4-12 hours after exposure to the allergens 3. Symptoms may begin after patients return to an environment from which they have been absent for a while (e.g. resuming work following weekends or holidays) but in at times do not develop with uninterrupted, routine contact with the same antigen.
Acute hypersensitivity pneumonitis is histologically characterized by the presence of neutrophilic infiltration of the respiratory bronchioles and alveoli. A pattern of diffuse alveolar damage and temporally uniform, non-specific, chronic interstitial pneumonitis may also be seen.
Subacute hypersensitivity pneumonitis
Subacute hypersensitivity pneumonitis develops when hypersensitivity pneumonitis continues beyond the acute phase (i.e. continues for weeks to months). While some publications suggest the disease to needs to prevail for between 1-4 months to fall into this category 4, it is important to realize that the terms acute, subacute and chronic lie on a continuum.
Symptoms in the subacute phase of hypersensitivity pneumonitis are similar to, but less severe than, those in the acute phase. Symptoms are often prolonged over weeks to months. Patients may experience recurrent episodes of acute symptoms superimposed on a background of deteriorating respiratory function.
Subacute hypersensitivity pneumonitis usually results from intermittent or continuous exposure to low doses of antigen and is histologically characterized by the presence of cellular bronchiolitis, non-caseating granulomas, and bronchiolocentric interstitial pneumonitis with a predominance of lymphocytes.
Chronic hypersensitivity pneumonitis
Chronic hypersensitivity pneumonitis refers to hypersensitivity pneumonitis where there is radiological evidence of fibrosis and represents the end-stage of repeated or persistent pneumonitis 5. The presence of fibrotic changes confers a poor prognosis.
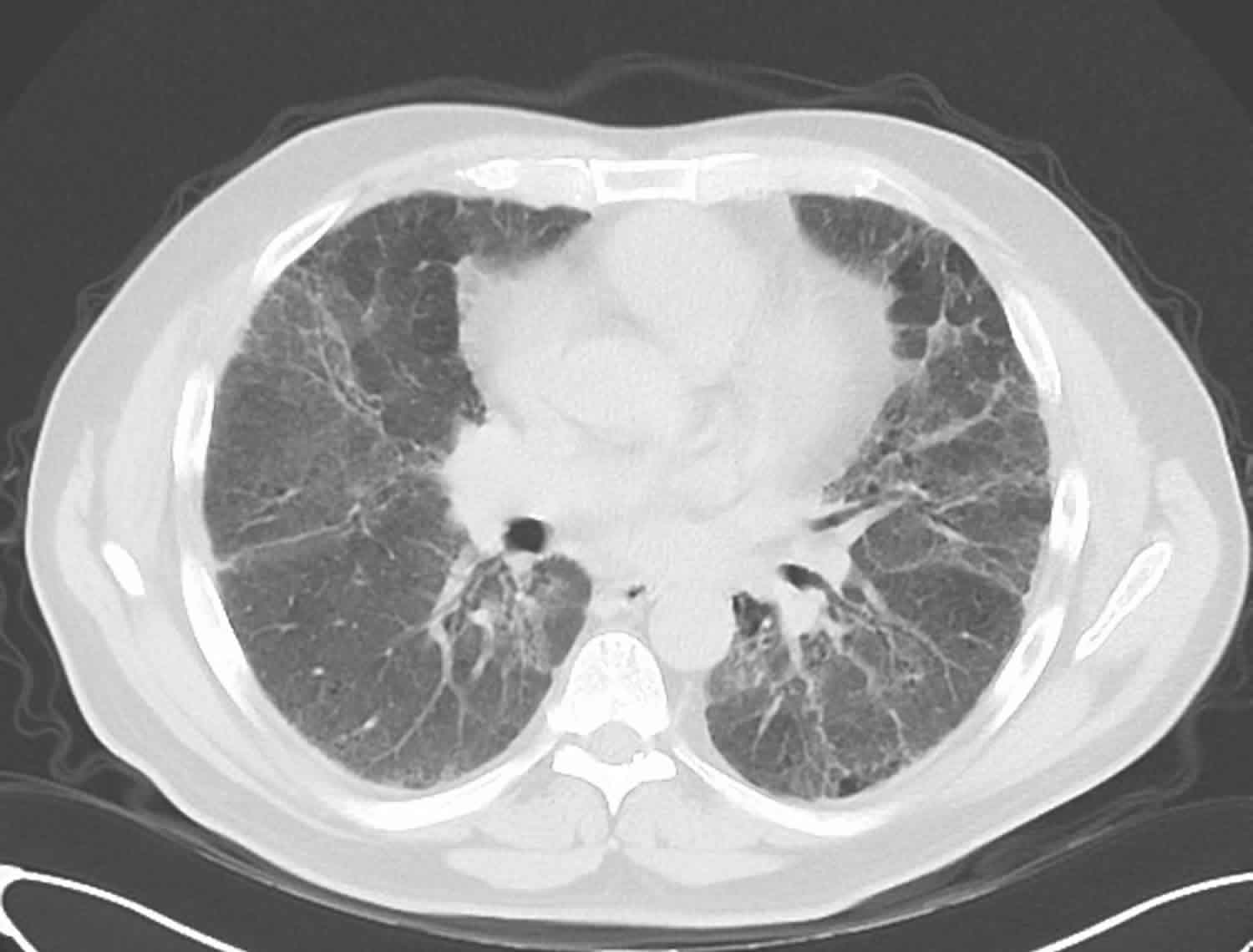
Chronic hypersensitivity pneumonitis CT scan
High-resolution CT of the chest typically reveals indistinct centrilobular peribronchiolar nodular opacities – micronodules) of varying numbers 6. Other features include:
- ground-glass opacities
- lobular areas of hyperlucency (mosaic perfusion) caused by bronchiole obstruction
- areas of pulmonary fibrosis and honeycombing
There is often a middle or upper zone predominance of CT findings with sparing of the lung bases, unlike non-specific interstitial pneumonia or usual interstitial pneumonia, which show a lower zone predominance.
The presence of an extensive reticular pattern, traction bronchiectasis, and honeycombing have been shown to closely correlate with the presence of histologic fibrosis in chronic hypersensitivity pneumonitis 7.
Figure 2. Chronic hypersensitivity pneumonitis CT
Footnote: 60 year man who is non-smoker man with cough for months and increasing shortness of breath. This patient had kept pigeons for many years. CT scan shows reticular opacity and honeycombing in a mainly basal and peripheral distribution. Traction bronchiectasis in the bases. Widespread ground glass opacity. Gas trapping on expiratory images. Emphysematous changes at the lung apices. No pleural effusion. No lymphadenopathy. Lung biopsy shows mild interstitial inflammation and fibrosis with giant cells, consistent with hypersensitivity pneumonitis.
[Source 8 ]Chronic hypersensitivity pneumonitis life expectancy
Among patients with chronic hypersensitivity pneumonitis, the degree of pulmonary function impairment and the extent of fibrosis are known predictors of mortality 5. In a study involving Korean patients with chronic hypersensitivity pneumonitis, showed old age, low levels of bronchoalveolar lavage fluid lymphocyte, and poor lung function mean poor prognosis 9. The median follow-up period was 24.8 months and the mean age of patients was 60.4 years, 60.4% were female and 33.7 % died during follow-up. The 1, 3, and 5-year survival rates were 95 %, 81.2% and 69.3 %, respectively 9. Non-survivors had older age and lower body mass index (BMI), and showed higher forced expiratory volume in 1 second / forced vital capacity ratio (FEV1/FVC), lower diffusing capacity for carbon monoxide (DLco) and the lowest oxygen saturation during 6-minute walk test, shorter 6-minute walk test distance and larger decline in forced vital capacity during 6 months, compared to survivors 9. Multivariate cox proportional analysis showed that older age, lower levels of lymphocytes in bronchoalveolar lavage fluid and lower diffusing capacity for carbon monoxide (DLco) and larger decline in forced vital capacity during 6 months, were independently associated with poor prognosis.
Hypersensitivity pneumonitis causes
Hypersensitivity pneumonitis is a rare immune system disorder that affects the lungs. Hypersensitivity pneumonitis occurs in some people after they breathe in certain substances they encounter in the environment. There are more than 300 known substances which, when inhaled as a fine dust, have been known to cause hypersensitivity pneumonitis. These substances trigger your immune systems, causing short- or long-term inflammation, especially in a part of the lungs called the interstitium. This inflammation makes it harder for the lungs to function properly and may even permanently damage the lungs. It can take several months to a number of years to develop allergy to the dust. Only a small number of people who inhale this dust actually develop hypersensitivity pneumonitis. If diagnosed, some types of hypersensitivity pneumonitis are treatable by avoiding exposure to the environmental substances or with medicines such as corticosteroids that reduce inflammation. If the condition goes untreated or is not well controlled over time, the chronic inflammation can cause irreversible scarring of the lungs that may severely impair their ability to function.
Hypersensitivity pneumonitis is caused by repeated exposure to environmental substances that cause inflammation in the lungs when inhaled. These substances include certain:
- Bacteria and mycobacteria
- Fungi or molds
- Proteins
- Chemicals
Common environmental sources of substances that can cause hypersensitivity pneumonitis are:
- Animal furs
- Air conditioner, humidifier, and ventilation systems
- Bird droppings and feathers
- Contaminated foods such as cheese, grapes, barley, sugarcane
- Contaminated industry products or materials such as sausage casings and corks
- Contaminated metal working fluid
- Hardwood dusts
- Hay or grain animal feed
- Hot tubs
- Organic chemicals such as isocyanates found in paint hardeners
- From immunosuppressant used in organ transplantation: e.g. sirolimus/everolimus 10
Because hypersensitivity pneumonitis is caused by different substances found in many environmental sources, doctors once thought they were treating different lung diseases. Research has helped us understand hypersensitivity pneumonitis is triggered by different causative substances.
Some commonly seen problems are given specific names related to the source of the dust, including:
- Farmer’s lung: seen in farmers and cattle workers, this condition is caused by breathing mold that grows on hay, straw and grain.
- Bird fancier’s lung: also called pigeon fancier’s lung caused by breathing particles from feathers or droppings of many species of birds.
- Cheese worker’s lung
- Bagassosis
- Mushroom worker’s lung
- Malt worker’s lung
- Maple bark disease
- Humidifier lung: can develop by breathing in fungus growing in humidifiers, air conditioners and heating systems, particularly if they are not well maintained.
- Hot tub lung: may develop by breathing in bacteria that may be found in the water vapor coming from indoor hot tubs.
Risk factors for hypersensitivity pneumonitis
Certain factors affect your risk of developing hypersensitivity pneumonitis. These factors include age, environment or occupation, family history and genetics, lifestyle habits, other medical conditions, and sex or gender.
If you work in certain occupations, then you may be at an increased risk of developing hypersensitivity pneumonitis. This includes farmers, vegetable or dairy cattle workers, bird and poultry handlers, veterinary workers and animal handlers, grain and flour processing and loaders, lumber milling, wood stripping and paper and wallboard manufacturers. Another risk factor is inhaling certain chemicals produced in plastic manufacturing, painting, and the electronics industry.
Most individuals who work in such occupations do not develop hypersensitivity pneumonitis. It appears that certain genetic factors determine if you are going to develop hypersensitivity pneumonitis or not. Unfortunately, at this time, there is not much information about the genes that can predispose a person to develop hypersensitivity pneumonitis.
Age
Although hypersensitivity pneumonitis can occur at any age, people tend to be diagnosed with this condition between 50 and 55 years of age. Hypersensitivity pneumonitis is a common type of chronic interstitial lung disease in children.
Environment or occupation
Repeated exposure to certain substances that cause the condition, possibly while working in occupations where environmental sources are common, can increase your risk of developing hypersensitivity pneumonitis. Certain occupations—such as farmers or people who breed animals or birds, cheese washers, woodworkers, and wine makers—have a greater chance of exposure to causative substances. However, you may be exposed to environmental sources in your home or elsewhere. Even having pets such as birds in the home can increase your risk of hypersensitivity pneumonitis.
Alone, environmental exposure to causative substances is not enough to cause hypersensitivity pneumonitis. An estimated 85 to 95 percent of people exposed to causative substances either never develop hypersensitivity pneumonitis or they experience a mild immune reaction with no obvious signs or symptoms or disease.
Family history and genetics
Genetics is thought to predispose some people to have strong immune responses and develop hypersensitivity pneumonitis after repeat exposures to a causative substance. In some populations, family history of pulmonary fibrosis or hypersensitivity pneumonitis may increase the risk of developing hypersensitivity pneumonitis. When hypersensitivity pneumonitis occurs in relatives it is called familial hypersensitivity pneumonitis.
Researchers are beginning to map genetic variations in immune system proteins that may increase the risk for developing hypersensitivity pneumonitis. These differences may explain why immune cells respond differently between people who do or do not develop hypersensitivity pneumonitis after the same exposure to a causative substance.
Lifestyle habits
Smoking is not thought to increase the risk of developing hypersensitivity pneumonitis. However, smoking can worsen chronic hypersensitivity pneumonitis and cause complications. If you have hypersensitivity pneumonitis, learn why doctors recommend quitting smoking.
Other medical conditions
Some viral infections later in life may increase the risk of developing hypersensitivity pneumonitis.
Sex or gender
Men and women can have hypersensitivity pneumonitis. Some small studies found this condition to be slightly more common in women.
Hypersensitivity pneumonitis prevention
Once hypersensitivity pneumonitis is diagnosed, measures should be taken to avoid the dust to which your lungs has developed allergy. Avoiding the dust is important both in early and later stages of hypersensitivity pneumonitis. You can live a normal life and your lungs may become normal if you avoid the dust in the early stages of hypersensitivity pneumonitis.
You can take steps to limit exposure to certain dusts:
- Allergy-causing bacteria and fungus can thrive in stagnant, or still, water. Be sure to remove any standing water inside and outside your home.
- Take efforts to keep the humidity in your home and work below 60 percent.
- Immediately repair any water damage inside your home or work. This includes removing water-damaged carpeting, furnishings and drywall.
- Properly maintain your heating, ventilation and air conditioning systems.
- Make sure that the water in heating, air conditioning and ventilation systems is not recirculated.
- Properly dry and store farm products if you work with them.
If you cannot completely avoid the dusts, there are certain protective devices that can reduce the chances of breathing in the dust. You can consider wearing an air-purifying respirator. Air purifying respirators have been used to prevent acute attacks of farmer’s lung. Wearing such respirators for long periods can be a challenge. Dust respirators are not found to be very helpful. Some engineering controls, such as having an electrostatic dust filter in the return ducts of central air conditioning systems, can also be considered to reduce dust exposure.
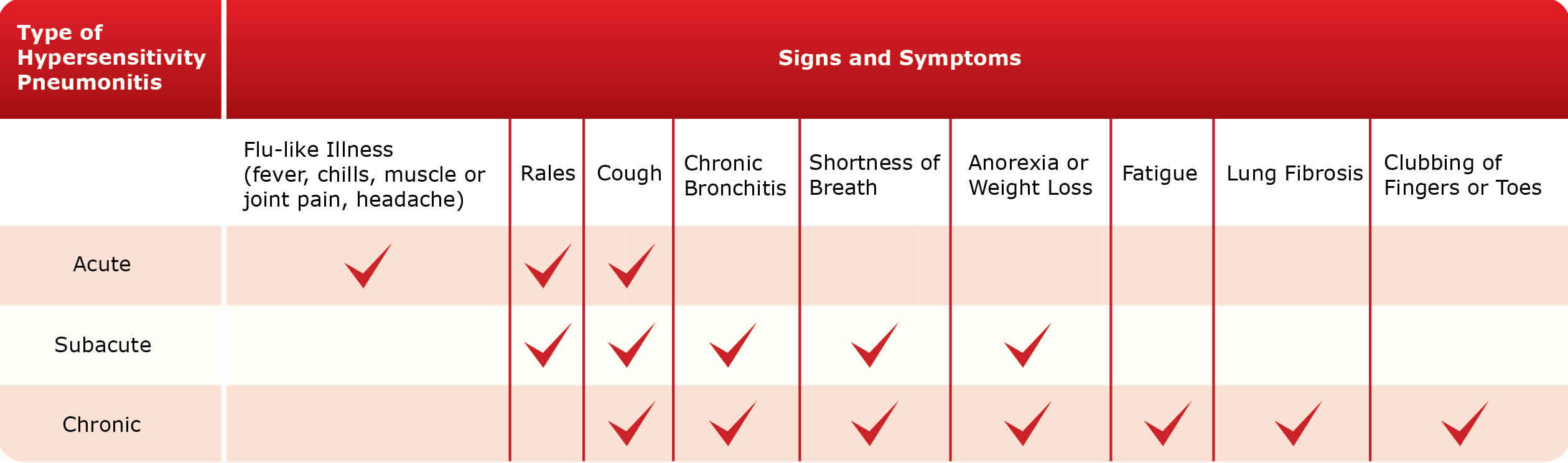
Hypersensitivity pneumonitis signs and symptoms
Hypersensitivity pneumonitis signs and symptoms vary between acute, subacute, and chronic types of hypersensitivity pneumonitis. If your hypersensitivity pneumonitis is not diagnosed or well controlled by treatment, it can lead to irreversible lung damage and other potentially fatal complications.
Acute hypersensitivity pneumonitis is the most common form of this condition. Acute hypersensitivity pneumonitis is thought to occur as a result of a short period of exposure to a large amount of causative substance. Symptoms usually occur within 9 hours of being exposed again to a substance that triggers your immune system. If an additional exposure does not occur, symptoms usually resolve after a few days. Subacute and chronic forms of hypersensitivity pneumonitis occur after multiple or continuous exposures to small amounts of causative substance. Approximately 5 percent of patients develop chronic disease.
Signs and symptoms of acute, subacute, and chronic hypersensitivity pneumonitis may include flu-like illness including fever, chills, muscle or joint pain, or headaches; rales; cough; chronic bronchitis; shortness of breath; anorexia or weight loss; fatigue; fibrosis of the lungs; and clubbing of fingers or toes.
While some signs and symptoms occur in several types of hypersensitivity pneumonitis, they may vary in severity. The exact signs and symptoms you experience also may vary.
The following are common signs and symptoms of acute, subacute, and chronic hypersensitivity pneumonitis.
Hypersensitivity pneumonitis complications
Hypersensitivity pneumonitis may cause the following potentially fatal complications if the condition is not diagnosed or well controlled by treatment.
- Irreversible lung damage and permanently reduced lung function because of severe fibrosis and impaired ability to oxygenate the blood during normal breathing.
- Pulmonary hypertension due to damage of blood vessels in the lungs.
- Heart failure because inflammation makes it harder for the heart to pump blood to and through the lungs.
Hypersensitivity pneumonitis diagnosis
To diagnose hypersensitivity pneumonitis, your doctor will collect your medical history to understand your symptoms and see if you have an exposure history to possible causative substances. Your doctor will perform a physical exam and may order diagnostic tests and procedures. Based on this information, your doctor may able to determine whether you have acute, subacute, or chronic hypersensitivity pneumonitis.
Your doctor will ask if you have exposure to any kind of dust at home or at work. Some specific questions that your doctor may ask are as follows:
- Have you been exposed to any water damage in your house or at work, especially from humidifiers, heating systems, or air conditioners?
- Do you have a hot tub at home?
- Have you have been exposed to bird droppings/ do you have any birds as pets/do you have any feather cushions or down pillows?
You can bring in a family member to the doctor’s visit since they may remember exposure to certain dusts that you may have forgotten or overlooked. Rarely, if no obvious cause for exposure is determined, an industrial hygienist who is trained to detect such dust exposure may have to visit your home or workplace.
It can take months or even years for your doctor to diagnose hypersensitivity pneumonitis in you or your child. Hypersensitivity pneumonitis can be hard to diagnose because:
- There are no clear exposure histories to potential causative substances before having symptoms. This occurs in up to 50 percent of patients who are later diagnosed with hypersensitivity pneumonitis. Despite hypersensitivity pneumonitis being a common childhood interstitial lung disease, children are often diagnosed late after the condition has progressed to chronic disease. This is because children tend to be exposed to small amounts of causative substance over long periods of time, which does not trigger obvious acute symptoms and makes it very difficult to determine their exposure history.
- Other conditions may cause similar signs and symptoms. Before diagnosing hypersensitivity pneumonitis, your doctor must rule out: unintentional effects of medicines such as bleomycin, methotrexate, or nitrofurantoin; lung infections such as pneumonia or the flu (influenza); smoking-related lung disease; connective tissue disease; bleeding in the lungs; idiopathic pulmonary fibrosis; sarcoidosis; and lung cancer.
- Diagnostic features seen in chest x-rays, CT scans, and lung biopsies may differ between children and adults. Even when a person’s exposure history is known or hypersensitivity pneumonitis is suspected, doctors look for diagnostic features in chest x-rays, CT scans, and lung biopsies that are indicators of the disease in adults. More research is needed to help map diagnostic features for children with this condition.
Diagnostic tests and procedures
To diagnose hypersensitivity pneumonitis, your doctor may order:
- Blood tests to detect high levels of white blood cells and other immune cells and factors in your blood that indicate your immune system is activated and causing inflammation somewhere in your body.
- Bronchoalveolar lavage (BAL) to collect fluid from your lungs that can be tested for high levels of white blood cells and other immune cells. High levels of these cells mean your body is making an immune response in your lungs, but low levels do not rule out hypersensitivity pneumonitis.
- Computed tomography (CT) to image the lungs and look for inflammation or damage such as fibrosis. CT scans, particularly high-resolution ones, can help distinguish between types of hypersensitivity pneumonitis.
- Inhalation challenge tests to see if a controlled exposure to a suspected causative substance triggers your immune system and the onset of common signs and symptoms such as an increase in temperature, increase in white blood cell levels, rales that are heard during a physical exam, or reduced lung function. A positive test can confirm an inhaled substance triggers your immune system. A negative test does not rule out that you have hypersensitivity pneumonitis, because it may mean a different untested environmental substance is causing your condition. Before having this test, talk to your doctor about the benefits and possible risks of this procedure.
- Lung biopsies to see if your lung tissue shows signs of inflammation, fibrosis, or other changes known to occur in hypersensitivity pneumonitis. Lung biopsies will reveal inflammation, fibrosis, and possibly granulomas in subacute and chronic hypersensitivity pneumonitis. They are not usually performed for acute hypersensitivity pneumonitis.
- Lung function tests to see if you show signs of restriction such as reduced breathing capacity or abnormal blood oxygen levels and check if you have obstructed airways. These tests help assess the severity of your lung disease and when repeated they can help monitor whether your condition is stable or worsening over time. Lung function tests may be normal between acute flares.
- Precipitin tests to see if you have antibodies in your blood that recognize and bind to a causative substance. While a positive test means that you have been exposed to a substance, it cannot confirm you have hypersensitivity pneumonitis. This is because some people without this condition also have antibodies in their blood to these substances. If you have antibodies to a substance, your doctor may have you perform an inhalation challenge test to see if a new exposure to the same substance can activate your immune system and cause a new acute flare.
- Chest x-rays to image the lungs and look for inflammation or damage such as fibrosis in your lungs.
Plain chest X-ray
In population-based studies, the sensitivity of chest radiography for detection of this disease is relatively low 11. Many patients may indeed have normal radiographs 12.
Abnormal plain radiographic findings may be observed in some patients can include 12:
- numerous poorly defined small (<5 mm) opacities throughout both lungs, sometimes with sparing of the apices and bases
- airspace disease: usually seen as ground-glass opacities (can be patchy or diffuse, resembling pulmonary edema) or, more rarely, as consolidation
- a pattern of fine reticulation may also occur
- zonal distribution is variable from patient to patient and may even show temporal variation within the same patient
Late stages
- when fibrosis develops: there may be a reticular pattern and honeycombing, which sometimes are more severe in the upper lobes than in the lower ones
- volume loss may occur: particularly in the upper lungs, and peribronchial thickening may be visible
- cardiomegaly may develop as a result of cor pulmonale
Hypersensitivity pneumonitis CT
Several features on high resolution CT chest may appear at any stage of the disease and include 12:
- homogeneous ground-glass opacity: bilateral and symmetric but sometimes patchy and concentrated in the middle part and base of the lungs or having a bronchovascular distribution
- ground-glass opacity usually represents chronic interstitial inflammation but occasionally may be caused by fine fibrosis or organizing pneumonia
- numerous round centrilobular opacities: usually <5 mm in diameter (occasionally these opacities have well-defined borders and soft-tissue attenuation)
- hypoattenuation and hypovascularity of scattered secondary lobules: hypoattenuating regions that persist on expiratory CT scans are indicative of air trapping, which is caused by bronchiolar inflammation and obstruction: this may give a mosaic attenuation pattern 13
- head cheese sign: the combination of patchy ground-glass opacities, normal regions, and air trapping
Other associated features include:
- small volume mediastinal lymphadenopathy (generally 10-20 mm in short-axis diameter)
- occasional pulmonary arterial enlargement
- centrilobular emphysema
- with developing fibrosis, there can be reticulation, mainly in the middle portion of the lungs or fairly evenly throughout the lungs but with relative sparing of the extreme apices and bases
Hypersensitivity pneumonitis treatment
Treatments for hypersensitivity pneumonitis usually include avoidance strategies and medicines. Occasionally, lung transplants are used to treat severe chronic disease in some patients.
Treatment is more successful when hypersensitivity pneumonitis is diagnosed in the early stages of the disease, before permanent irreversible lung damage has occurred. As new data emerges, doctors are becoming more aware of the unique treatment needs for children with hypersensitivity pneumonitis.
Avoidance strategies
If your doctor is able to identify the environmental substance that causes your hypersensitivity pneumonitis, he or she will recommend that you adopt the following avoidance strategies.
- Remove the causative substance if possible
- Replace workplace or other products with available alternatives that do not contain the substance responsible for your condition
- Alter work processes so you don’t continue to breathe in the causative substance
- Stay away from known sources of your causative substance
Medicines
If avoidance strategies do not work for your condition, your doctor may prescribe corticosteroids or other immunosuppressive medicines to treat your condition. The choice, dose, and duration of these medicines will depend on your condition and medical history. Acute and subacute types of hypersensitivity pneumonitis usually respond well to these treatments.
Depending on your condition, your doctor also may prescribe some of the following supportive therapies:
- Oxygen therapy as needed for low levels of oxygen in the blood.
- Bronchodilators to relax the muscles in the airways and open your airways to make breathing easier.
- Opioids to control shortness of breath or chronic cough that is resistant to other treatments. Regular (e.g. several times a day, for several weeks or more) or longer use of opioids can lead to physical dependence and possibly addiction.
Lung transplants
If your condition is not adequately controlled by avoidance strategies or medicines and you develop serious complications, you may be a candidate for a lung transplant. During this procedure, healthy donor lung will be transplanted into you to replace the damaged lung. Two important things to know:
- This procedure is not a cure. This is because your immune system will be the same after the procedure. This means that if you are exposed again to the substances that triggers your immune system, new inflammation may damage the transplanted donor lung tissue.
- This procedure is not for everyone. Even if you are a candidate for this procedure, it may be difficult to find a matching organ donor. Lung transplants are serious medical procedures with their own risks. Talk to your doctor about what procedures are right for you.
Hypersensitivity pneumonitis prognosis
Most symptoms go away when you avoid or limit your exposure to the material that caused the problem. If prevention is made in the acute stage, the outlook is good. When it reaches the chronic stage, the disease might continue to progress, even if the offending substance is avoided.
Living with hypersensitivity pneumonitis
If you have hypersensitivity pneumonitis, you can take steps to control the condition and prevent complications by receiving routine follow-up care, monitoring your condition, preventing new acute flares and complications, and learning about and preparing for serious complications.
Receive routine follow-up care
In addition to treatments you are using to control your condition, your doctor may recommend other medical care to improve your quality of life, vaccines to prevent lung infections, and lifestyle changes such as physical activity and quitting smoking to improve overall health and avoid some complications.
- Other medical care: Your doctor may evaluate how your condition is affecting your activity level and mental health. To improve your quality of life, your doctor may recommend other treatments to address pain, fatigue, or mental health concerns that you may have.
- Vaccines: Remember that your condition causes you to have reduced lung function, particularly if you have subacute or chronic hypersensitivity pneumonitis. Your doctor may recommend that you receive routine pneumococcal and flu (influenza) vaccines to avoid lung infections that can further impair your reduced lung function.
- Physical activity: Patients with hypersensitivity pneumonitis benefit from regular exercise. Before starting any exercise program, ask your doctor about what level of physical activity is right for you.
- Quitting smoking: If you smoke, quit. Although smoking does not increase the risk of developing hypersensitivity pneumonitis, some studies suggest smoking can worsen disease and shorten survival for people with chronic hypersensitivity pneumonitis compared to nonsmokers with chronic hypersensitivity pneumonitis. Another study reported lung cancer in patients who smoked and had chronic hypersensitivity pneumonitis.
Monitor your condition
If you have been diagnosed with subacute or chronic hypersensitivity pneumonitis, your doctor may recommend follow-up testing to see how well your treatment is working and if your disease is improving, stable, or worse. To monitor your condition, your doctor may recommend repeating tests used earlier to diagnose hypersensitivity pneumonitis such as chest x-rays, computed tomography (CT) scans, or lung function tests.
Your doctor may determine your disease is worse if you have new or more severe fibrosis or lung function problems. High-resolution CT scans may be more informative than lung function tests at assessing disease progression.
There is a growing recognition that disease tends to be worse, such as greater lung fibrosis, if it starts in childhood or early adult life. Therefore, more careful monitoring may be required for younger patients with hypersensitivity pneumonitis.
Prevent new acute flares and serious complications over your lifetime
To help prevent new acute flares and complications, your doctor may recommend tests to identify the substances causing your condition, as well as additional screening tests to prevent potentially fatal complications.
- Identification of substances causing your condition: If you do not know the environmental substances causing your condition, your doctor may recommend diagnostic precipitin and inhalation challenge tests. Identification can help avoid the environmental sources of the substances causing your condition. Successful avoidance strategies can help you live a longer, prevent new acute flares, and slow or stop progression to chronic disease with serious complications.
- Screening for serious complications: If you have been diagnosed with chronic hypersensitivity pneumonitis, your doctor may recommend echocardiography and right-heart catheterization to evaluate pulmonary artery pressure and screen for pulmonary hypertension. Pulmonary hypertension can occur in people who have chronic hypersensitivity pneumonitis, particularly in patients with more severe disease who have poorer lung function and reduced exercise capacity
Learn the warning signs of serious complications and have a plan
Always notify your doctor if your symptoms suddenly worsen. Your doctor will need to rule out other causes including infection and order repeat chest imaging tests. If these chest imaging tests show new findings without evidence of another cause, your doctor may modify your hypersensitivity pneumonitis treatment plan to better control your condition. Talk to your doctor and agree on a clinical decision plan to help you know when to seek urgent medical care.
References- Hypersensitivity pneumonitis. https://radiopaedia.org/cases/hypersensitivity-pneumonitis-1
- Lacasse Y, Girard M, Cormier Y. Recent advances in hypersensitivity pneumonitis. Chest. 2012;142 (1): 208-17. doi:10.1378/chest.11-2479
- Hirschmann JV, Pipavath SN, Godwin JD. Hypersensitivity pneumonitis: a historical, clinical, and radiologic review. Radiographics. 2009;29 (7): 1921-38.
- Hirschmann JV, Pipavath SN, Godwin JD. Hypersensitivity pneumonitis: a historical, clinical, and radiologic review. Radiographics. 2009;29 (7): 1921-38. Radiographics (full text) – doi:10.1148/rg.297095707
- Pulmonary haemodynamics and mortality in chronic hypersensitivity pneumonitis. Rudolf K.F. Oliveira, Jaquelina S. Ota-Arakaki, Paula S. Gomes, Andrea Gimenez, Carolina M.S. Messina, Roberta P. Ramos, Eloara V.M. Ferreira, David M. Systrom, Carlos A.C. Pereira. European Respiratory Journal Jun 2018, 51 (6) 1800430; DOI: 10.1183/13993003.00430-2018
- Buschman DL, Gamsu G, Waldron JA et-al. Chronic hypersensitivity pneumonitis: use of CT in diagnosis. AJR Am J Roentgenol. 1992;159 (5): 957-60.
- Sahin H, Brown KK, Curran-everett D et-al. Chronic hypersensitivity pneumonitis: CT features comparison with pathologic evidence of fibrosis and survival. Radiology. 2007;244 (2): 591-8. doi:10.1148/radiol.2442060640
- Chronic hypersensitivity pneumonitis. https://radiopaedia.org/cases/chronic-hypersensitivity-pneumonitis-6
- Prognostic factors in Korean patients with chronic hypersensitivity pneumonitis. Yeon joo Kim, Jooae Choe, Eun Jin Chae, Joon Seon Song, Dong Soon Kim, Jin Woo Song. European Respiratory Journal Sep 2018, 52 (suppl 62) PA3663; DOI: 10.1183/13993003.congress-2018.PA3663
- Rodríguez-Moreno A, Ridao N, García-Ledesma P et-al. Sirolimus and everolimus induced pneumonitis in adult renal allograft recipients: experience in a center. Transplant. Proc. 2009;41 (6): 2163-5. doi:10.1016/j.transproceed.2009.06.003
- Lynch DA, Rose CS, Way D et-al. Hypersensitivity pneumonitis: sensitivity of high-resolution CT in a population-based study. AJR Am J Roentgenol. 1992;159 (3): 469-72.
- Hirschmann JV, Pipavath SN, Godwin JD. Hypersensitivity pneumonitis: a historical, clinical, and radiologic review. Radiographics. 2009;29 (7): 1921-38. doi:10.1148/rg.297095707
- Glazer CS, Rose CS, Lynch DA. Clinical and radiologic manifestations of hypersensitivity pneumonitis. J Thorac Imaging. 2002;17 (4): 261-72.