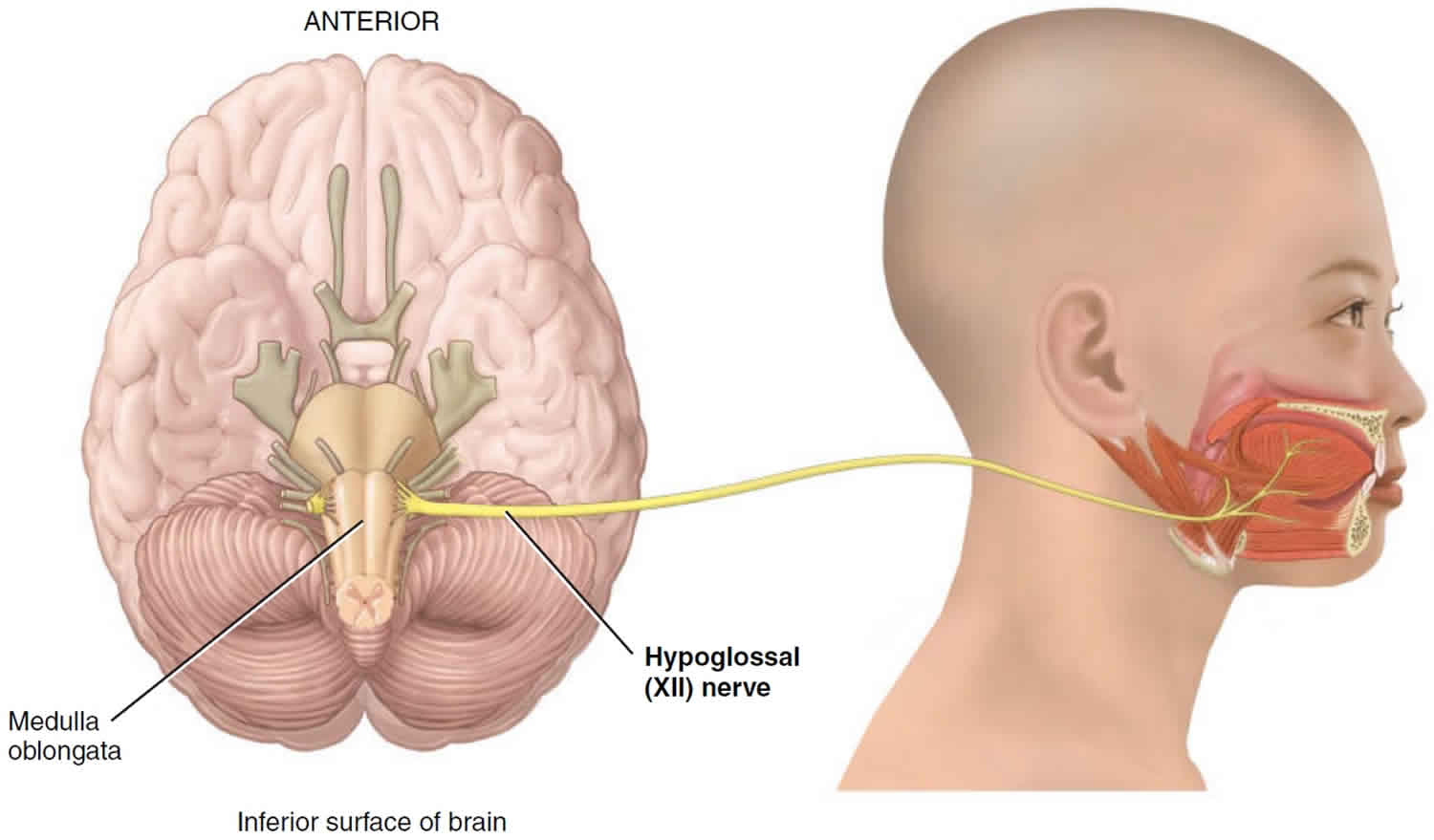
Hypoglossal nerve
Hypoglossal nerve (hypo- = below; -glossal= tongue) is the 12th cranial nerve (cranial nerve XII). Hypoglossal nerve is mainly a motor cranial nerve for the tongue musculature. Hypoglossal nerve originates in a nucleus in the medulla oblongata (hypoglossal nucleus) and exit the medulla on its anterior surface, and pass through the hypoglossal canal to supply the muscles of the tongue 1.
The hypoglossal nerve motor nerve fibers conduct nerve impulses for speech and swallowing. The sensory axons do not return to the brain in the hypoglossal nerve. Instead, sensory axons that originate from proprioceptors in the tongue muscles begin their course toward the brain in the hypoglossal nerve but leave the nerve to join cervical spinal nerves and end in the medulla oblongata, again entering the central nervous system via posterior roots of cervical spinal nerves.
Hypoglossal nerve also contains some sympathetic postganglionic fibers from the cervical ganglia, which innervates tongue vessels and some small glands in the oral mucosa.
The hypoglossal nerve’s course starts from the hypoglossal nuclei pair in the lower medulla. The two nerves travel laterally and ventrally from the respective nucleus. The nerve splits in two before exiting the medulla and passes through the hypoglossal canal in the occipital bone of the skull. The nerve reforms and descends through the neck to the angle of the mandible and travels underneath the tongue to innervate the tongue muscles.
At the early portion of the course, the nerve is below the internal carotid artery and internal jugular vein and near the vagus nerve. Then the nerve travels above the hyoid bone and in between the mylohyoid and hyoglossus muscles before branching to the various parts of the tongue musculature 1.
The hypoglossal nerve consists of four branches: the meningeal, descending, thyrothyroid, and muscular. However, only the muscular branch is considered part of the real hypoglossal nerve originating from the hypoglossal nucleus. Other branches originate from spinal nerves (mainly C1/C2) or the cervical ganglia. The meningeal branch arises from C1 and C2 nerves to the posterior cranial fossa. The descending branch carries information from C1 and then C2/C3 to innervate the neck muscles (omohyoid, sternohyoid, and sternothyroid). The thyrothyroid branches innervate the thyrohyoid muscle of the neck. The descending and thyrohyoid branches mostly originate from the cervical plexus.
The muscular/lingual branch is a general somatic efferent branch and innervates all the muscles of the tongue (both intrinsic and extrinsic), except for the palatoglossus, which receives motor innervation from the vagal nerve (CN X). The muscular branch controls most actions of the tongue including, protruding, retracting, depressing the tongue, and changing the tongue’s shape 1.
Figure 1. Hypoglossal nerve anatomy and function
[Source 2 ]Hypoglossal nerve function
The Hypoglossal nerve innervates all the intrinsic muscles and all but one of the extrinsic muscles (genioglossus, styloglossus, and hyoglossus) of the tongue. The hypoglossal nerve controls most actions of the tongue including protruding, retracting, depressing the tongue, and changing the tongue’s shape. Hypoglossal nerves control tongue movements during speech and swallowing.
The function of each muscle/muscle group is as follows:
- Genioglossus- Draw the tongue forward from the root
- Hyoglossus- Retracts the tongue and depresses its side
- Styloglossus- Draws the tongue upward
- Intrinsic muscles (superior/inferior longitudinales, transversus, verticalis)- Changes the shape of the tongue such as shortening, narrowing, curving the tongue
Hypoglossal nerve injury
Injury to the hypoglossal nerve results in difficulty in chewing; dysarthria or difficulty in speaking; and dysphagia or difficulty in swallowing. The tongue, when protruded, curls toward the affected side, and the affected side atrophies. The hypoglossal nerve may be injured as a result of conditions such as trauma, lesions, stroke, amyotrophic lateral sclerosis (ALS or Lou Gehrig’s disease), or infections in the brainstem.
The hypoglossal nerve can be damaged at the hypoglossal nucleus (nuclear), above the hypoglossal nucleus (supranuclear) or interrupted at the motor axons (infranuclear). Such damage causes paralysis, fasciculations (as noted by a scalloped appearance of the tongue), and eventual atrophy of the tongue muscles. When one of the two nerves is damaged, then the tongue, when protruded will deviate towards the damaged nerve because of the overaction of the strong genioglossus muscles.
Hypoglossal nerve damage
Supranuclear lesions occur at the cerebral cortex, the corticobulbar tract of the internal capsule, cerebral peduncles, or the pons. Supranuclear lesions cause the tongue to protrude away from the nerve because of predominant neural crossing for upper motor neurons. Supranuclear lesions do not tend to cause atrophy but can lead to an uncoordinated tongue with slow but spastic tongue movements. Supranuclear lesions commonly result from strokes, but can also be caused by pseudobulbar palsy.
Infranuclear and nuclear lesions cause weakness of the tongue but additionally cause ipsilateral atrophy. Lower motor neuron disease can also cause fasciculation when localized to the lower motor neurons.
Unilateral lesions are not typically a serious problem for patients as any impediments are compensated partly by the remaining hypoglossal nerve. However, bilateral lesions can cause profound difficulty with speech and swallowing as the patient cannot protrude the tongue for these necessary functions.
Hypoglossal nerves can be damaged unilaterally by a multitude of causes especially, tumors, infection, or trauma. The concept of trauma includes surgical trauma as with carotid endarterectomy (surgery to remove the plaques from the carotid artery). Rare bilateral lesions can be the result of radiation therapy 3.
Hypoglossal nerve in neurologic disorders
Progressive bulbar palsy and advanced amyotrophic lateral sclerosis (ALS) can cause severe tongue atrophy and an inability for the tongue to be protruded leading to inertia of the tongue (glossoplegia). Fasciculations frequently occur with atrophy in the case of motor neuron disease. Tremors can also occur on the tongue in the case of alcoholism, parkinsonism, and in paresis 4.
Neck-tongue syndrome
Neck-tongue syndrome is a pain on one side of upper neck or back of the head, usually involved with rapid rotation of the neck. The syndrome also typically involves the tongue, causing the ipsilateral side of the tongue to feel the pain as well. The cause of the syndrome is unknown although two theories have been suggested, and both involve strain/pressure on the C2 nerve. As the C2 nerve route is involved with hypoglossal nerve route, tongue pain can result 5.
Obstructive Sleep Apnea and Hypoglossal Nerve Stimulation
In obstructive sleep apnea (OSA), the decrease in muscle tone of the genioglossus muscle causes the tongue to retract and impede airflow into the trachea. One possible treatment if the patient is refractory to continuous positive airway pressure (CPAP), oral devices, or surgery is the hypoglossal nerve stimulator. Mild stimulation of the hypoglossal nerve causes the nerve to pull the tongue forward enabling better airflow 6.
Hypoglossal nerve test
Examining the hypoglossal nerve involves observation of the primary innervation target of the nerve; the tongue. The three observable aspects of the tongue are strength, bulk, and dexterity. Special attention is given when the tongue is weak, atrophied, moving abnormally, or impaired.
The tongue is first observed for position and appearance while it is at rest. Then the patient is asked to protrude the tongue, move it in and out, side to side, and up and down. The patient does each movement twice: once slowly and the next rapidly. Dexterity is tested by having the patient repeat sounds involving the tongue, such as saying “la la la” or use words with “t” or “d” sounds. Testing strength consists of the patient forcing the tongue to the side against the patient’s cheek, while the examiner tries to dislodge the tongue using his/her finger. The tongue’s strength can be checked more accurately using the tongue blade. Strength test is especially useful in testing for unilateral weakness caused by ipsilateral hypoglossal nerve damage.
References- Lin HC, Barkhaus PE. Cranial nerve XII: the hypoglossal nerve. Semin Neurol. 2009 Feb;29(1):45-52
- Kim SY, Naqvi IA. Neuroanatomy, Cranial Nerve 12 (Hypoglossal) [Updated 2018 Dec 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532869
- Lin HC, Barkhaus PE. Cranial nerve XII: the hypoglossal nerve. Semin Neurol. 2009 Feb;29(1):45-52.
- Orrell RW, Marsden CD. The neck-tongue syndrome. J. Neurol. Neurosurg. Psychiatry. 1994 Mar;57(3):348-52.
- Fleury Curado T, Oliven A, Sennes LU, Polotsky VY, Eisele D, Schwartz AR. Neurostimulation Treatment of OSA. Chest. 2018 Dec;154(6):1435-1447
- Finsterer J, Grisold W. Disorders of the lower cranial nerves. J Neurosci Rural Pract. 2015 Jul-Sep;6(3):377-91