What is oculomotor nerve
Oculomotor nerve (oculo- = eye; motor = a mover) is the 3rd cranial nerve (cranial nerve III). Oculomotor nerve nuclei in the midbrain provide motor impulses
that control movements of the eyeball, while accessory oculomotor parasympathetic nucleus (Edinger-Westphal nucleus) provides motor control to the smooth muscles that regulate constriction of the pupil and changes in shape of the lens via the oculomotor nerves.
The oculomotor nerve originates from 2 nuclei in the midbrain:
- Oculomotor nucleus
- Accessory parasympathetic nucleus (Edinger-Westphal nucleus)
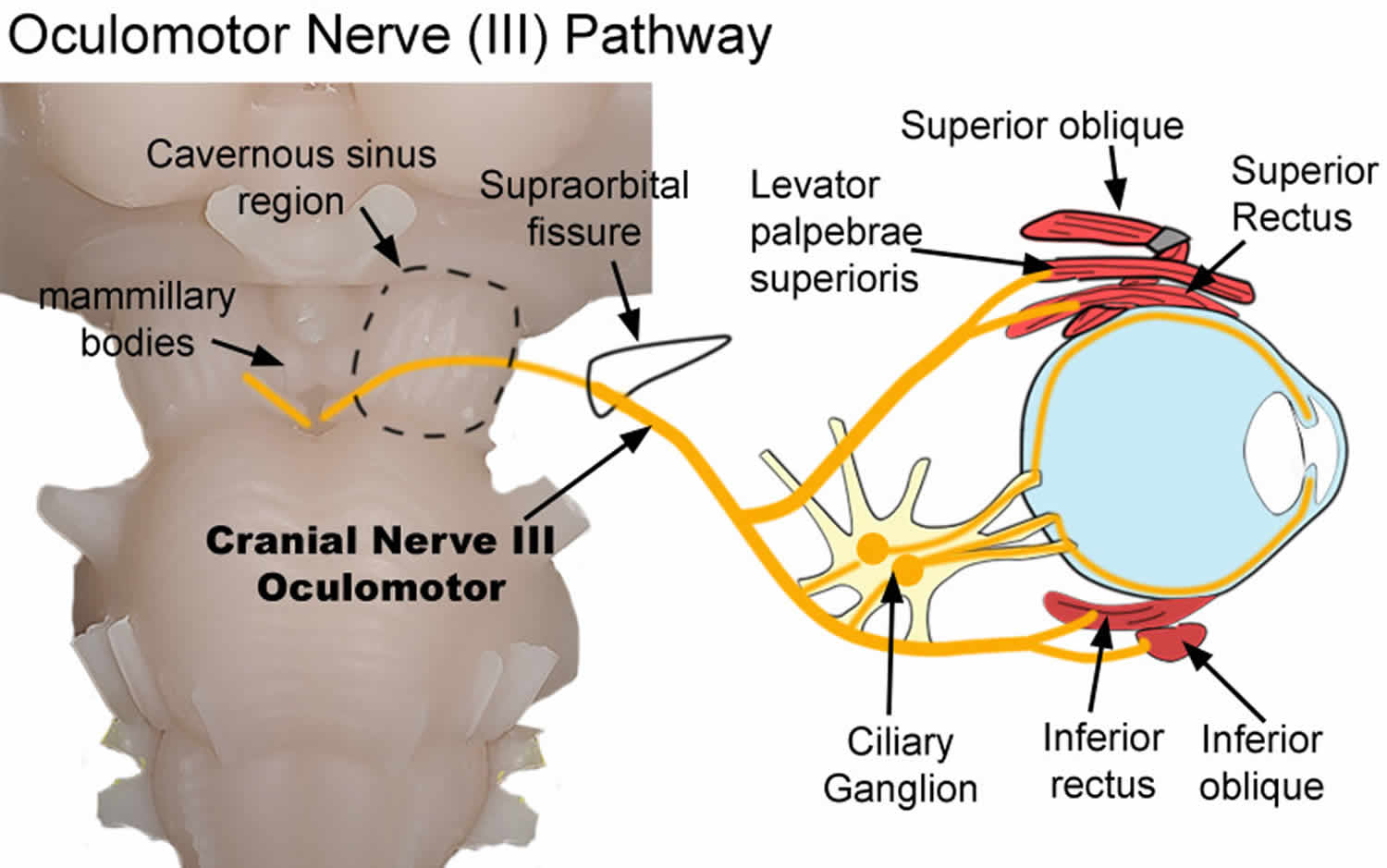
The oculomotor nerve exits the brainstem near midline at the base of the midbrain just caudal to the mammillary bodies. It passes through the cavernous sinus and proceeds through the supraorbital fissure to reach the orbit of the eye (Figures 1 and 2).
The oculomotor nerve (third cranial nerve) has both somatic and autonomic fibers. Somatic (voluntary) nerve fibers are bundled deep inside the nerve, while the autonomic (involuntary) fibers surround the somatic fibers around the outside of the nerve. Knowing the spatial layout of these fibers will help one understand the various forms of presentation in third nerve palsies.
The oculomotor nerve controls several muscles:
- Levator palpebrae superioris – raises the upper eyelid
- Superior rectus muscle – rotates the eyeball backward, “looking up”
- Medial rectus muscle – adducts the eye, “looking towards your nose”
- Inferior rectus muscle – rotates the eyeball forwards, “looking down”
- Inferior oblique muscle – rotates the eyeball backward when the eye is adducted
- Ciliary muscle – controls lens shape to focus on up-close objects
- Sphincter pupillae – constricts the pupil
There are two primary functions of the autonomic parasympathetic (involuntary) oculomotor nerve. It constricts the pupil (miosis) by innervating the smooth muscle (sphincter pupillae) near the pupil. It also innervates the ciliary muscles. These muscles connect the iris to the choroid. Contraction of the muscle alters the curvature of the lens which allows individuals to focus the lens on near objects (Figures 1 and 2) 1.
Control of other eye muscles is by the trochlear (CN IV) and abducens (CN VI) nerves.
The trochlear nerve (4th cranial nerve) controls:
- Superior oblique muscle – rotates the eyeball forward when the eye is adducted
The abducens nerve (6th cranial nerve) controls:
- Lateral rectus muscle – abducts the eye, “looking towards your ear on the same side”
The oculomotor nerve can become impaired in disease states which can lead to lifelong impairment in normal vision. Dysfunction can also be indicative of more serious underlying diseases, such as an aneurysm or a neoplasm.
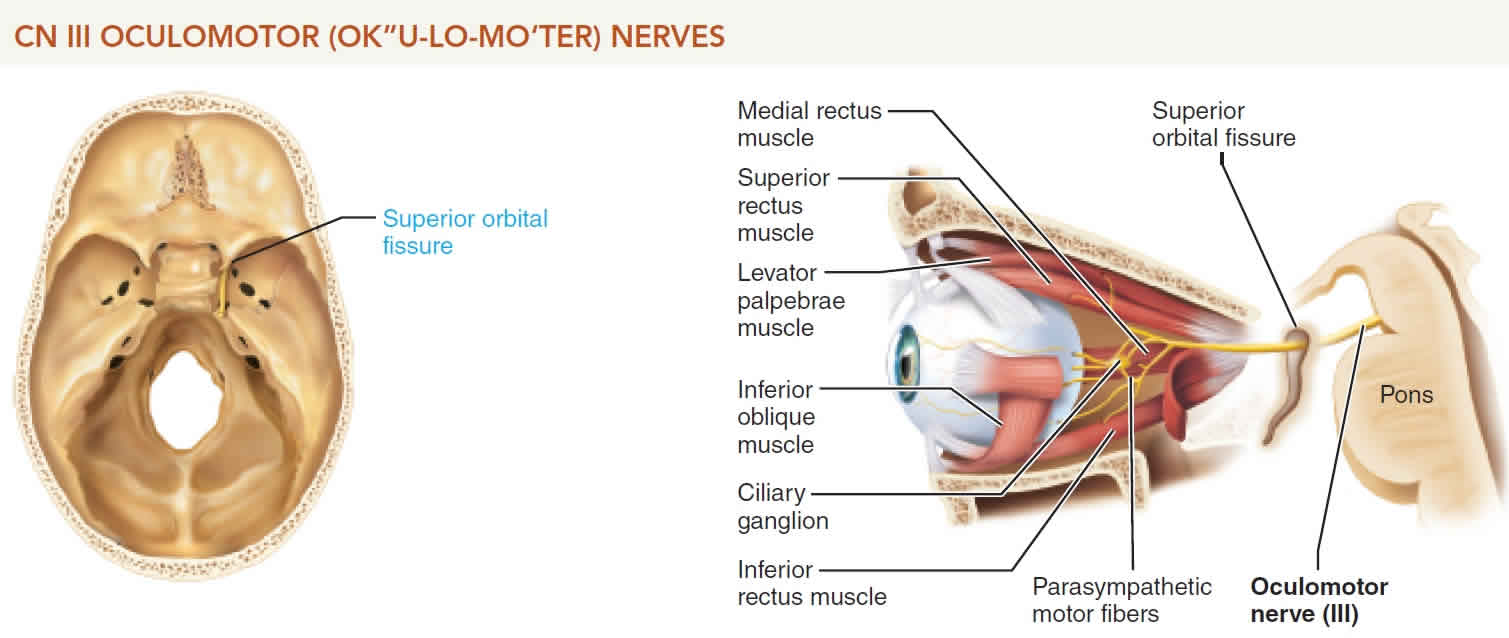
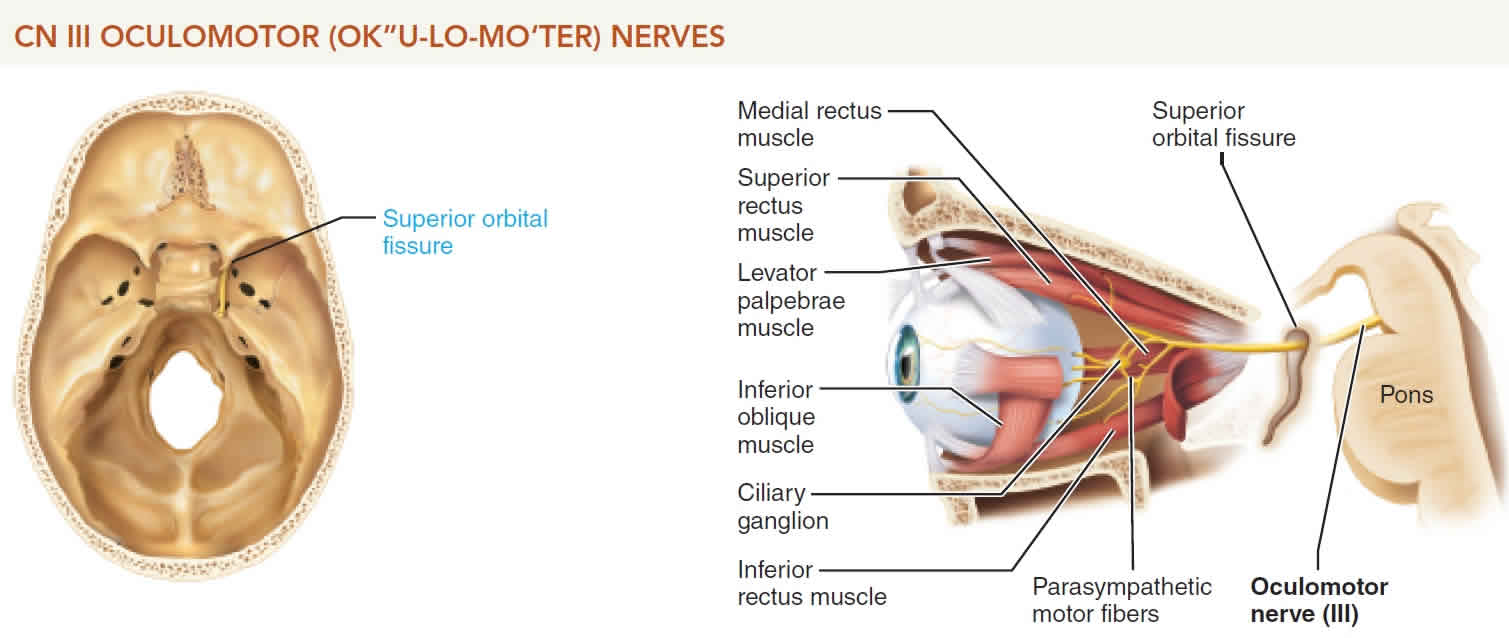
Figure 1. Oculomotor nerve
Figure 2. Oculomotor nerve pathway and function
Footnote: Pathway of the oculomotor nerve (cranial nerve III). Diagram shows the pathway of the oculomotor nerve as it exits the brainstem and terminates within the orbit. After exiting the brainstem, it traverses both the cavernous sinus (dotted line) and supraorbital fissure (black line) before entering the orbit. Parasympathetic nerves synapse within the ciliary ganglion. Postganglionic nerves then innervate the sphincter papillae and ciliary muscles. Somatic nerves innervate the superior oblique, levator palpebrae superioris, superior rectus, inferior rectus, and inferior oblique muscles.
[Source 2 ]Oculomotor nerve function
Oculomotor nerve (cranial nerve III) has smotos and autonomic functions.
The oculomotor nerve (the third cranial nerve; CN III) has three main motor functions:
- Innervation to the pupil and lens (autonomic, parasympathetic)
- Innervation to the upper eyelid (somatic)
- Innervation of the eye muscles that allow for visual tracking and gaze fixation (somatic)
Oculomotor nerve (cranial nerve III) has its motor nucleus in the anterior part of the midbrain. The oculomotor nerve extends anteriorly and divides into superior and inferior branches, both of which pass through the superior orbital fissure into the orbit (Figures 1 and 2). Axons in the superior branch innervate the superior rectus (an extrinsic eyeball muscle) and the levator palpebrae superioris (the muscle of the upper eyelid). Axons in the inferior branch supply the medial rectus, inferior rectus, and inferior oblique muscles—all extrinsic eyeball muscles. These somatic motor neurons control movements of the eyeball and upper eyelid.
Somatic (voluntary) functions of the oculomotor nerve include elevation of the upper eyelid via innervation of the levator palpebrae superioris muscle. Other essential functions include coordination of eye muscles for visual tracking and gaze fixation. These functions of eye movement occur through innervation of four eye muscles:
- Superior rectus muscle – elevates the eye while looking straight ahead (primary position)
- Medial rectus muscle – adducts the eye from a primary position
- Inferior rectus muscle – moves the eye down from a primary position
- Inferior oblique muscle – elevates the eye when the eye is adducted from a primary position
The inferior branch of the oculomotor nerve also supplies parasympathetic motor axons to intrinsic eyeball muscles, which consist of smooth muscle. They include the ciliary muscle of the eyeball and the circular muscles (sphincter pupillae) of the iris. Parasympathetic impulses propagate from a nucleus in the midbrain (accessory oculomotor nucleus) to the ciliary ganglion, a synaptic relay center for the two motor neurons of the parasympathetic nervous system. From the ciliary ganglion, parasympathetic motor axons extend to the ciliary muscle, which adjusts the lens for near vision (accommodation). Other parasympathetic motor axons stimulate the circular muscles of the iris to contract when bright light stimulates the eye, causing a decrease in the size of the pupil (constriction).
Oculomotor nerve damage
A dilated pupil and ptosis is the most common clinical presentation of oculomotor nerve palsy post-neurosurgery, usually after clipping of an intracranial aneurysm 3. Patients who undergo open surgery or a minimally invasive technique on basilar artery aneurysms may develop a third nerve palsy after surgery, although this complication has been shown to be transient 4.
Oculomotor nerve palsy
Recognizing oculomotor nerve palsy is crucial because it can be a sign of underlying or uncontrolled chronic disease states. It is an essential clinical symptom that can be life-saving in certain circumstances.
The cause of oculomotor nerve palsy is most commonly by microvascular diseases including diabetes, hypertension, compression from an intracranial neoplasm or an aneurysm, or trauma 3.
Microvascular disease can affect the vasa vasorum. In these instances, the fibers innervating the upper eyelid and most of the extraocular muscles become ischemic. Compression of the oculomotor nerve can also occur via an aneurysm, intracranial neoplasm, or uncal herniation. These ischemic events can affect the outer pia blood vessels supplying the fibers to the pupil and lens and eventually the inner vasa vasorum.
Oculomotor nerve palsy clinical signs
- Ptosis (droopy eyelid) – due to paralysis of levator palpebrae superioris
- “Down and out” positioning of the affected eye
- Position caused by unopposed action of:
- lateral rectus muscle (eye abduction action): innervation = abducens nerve (cranial nerve VI)
- superior oblique muscle (Adduct and move eye down): innervation = trochlear nerve (cranial nerve IV)
- Position caused by unopposed action of:
- Diplopia (“seeing double”) – due to a misalignment of the eyes (ptosis may block the vision in one eye, resulting in the absence of diplopia)
- Dilated pupil – caused by lack of parasympathetic innervation
- Abnormal swinging flashlight test – if parasympathetic nerve fibers are affected, shining a light into EITHER eye will NOT result in pupillary constriction of the affected eye
- Inability to accommodate – this may be difficult to assess in an older patient because their lens may already be hard and difficult to change shape due to a normal part of the aging process
Labs and Imaging
Evaluation should base its conclusions on the presence or absence of pupil involvement.
If the pupil is spared, obtain:
- Blood pressure measurement
- HbA1C
- CBC
- ESR
If the pupil is involved, compression from the outside should be suspected, and one should obtain 1:
- Prompt referral to a neuro-ophthalmologist
- MRI
- CT angiography (if an aneurysm suspected)
Oculomotor nerve palsy treatment
Conservative management
Treatment is conservative in the acute phase.
If diplopia is present and distressful, an eye patch, opaque contact lens, or a blurred lens in glasses covering the affected eye can be helpful.
Botulinum toxin can be useful in the acute setting of partial third nerve palsy with horizontal deviation; best used with paralysis of only the medial rectus. With injection into the overcompensating lateral rectus in these cases, horizontal deviation in the primary position is correctable. If there is mild vertical deviation remaining, prisms in glasses may be of some help. Botulinum toxin should be avoided in vertical muscle imbalance due to the high rate of complications 5.
Most patient (63%) with an acquired third nerve palsy recover completely with conservative management. Patients with microvascular etiology having the greatest chance of full recovery 3.
Surgical management
Minimal or no improvement after 6 months of conservative therapy warrants strabismus surgery. Strabismus surgery involves fixing the malalignment of the extraocular muscles. Surgery usually involves a combination of a recession (cutting the muscle from the eye and reattaching it posterior to the initial position to WEAKEN the muscle’s function) and resection (removing a section of the muscle to shorten it, STRENGTHENING the muscle’s function). Depending on the pair of muscles involved, the surgeon will typically recess the contracted muscle while resecting on the antagonist muscle 5.
If the pupil is involved, patients should undergo a thorough evaluation by a neurologist 1.
References- Modi P, Arsiwalla T. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Feb 1, 2019. Cranial Nerve III Palsy
- Joyce C, Peterson DC. Neuroanatomy, Cranial Nerve 3 (Oculomotor) [Updated 2019 Jan 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537126
- Fang C, Leavitt JA, Hodge DO, Holmes JM, Mohney BG, Chen JJ. Incidence and Etiologies of Acquired Third Nerve Palsy Using a Population-Based Method. JAMA Ophthalmol. 2017 Jan 01;135(1):23-28
- Seng LB, Yamada Y, Rajagopal N, Mohammad AA, Teranishi T, Miyatani K, Kawase T, Kato Y. Multimodality Techniques in Microsurgical Clipping as the Gold Standard Treatment in the Management of Basilar Tip Aneurysm: A Case Series. Asian J Neurosurg. 2018 Oct-Dec;13(4):1148-1157
- Singh A, Bahuguna C, Nagpal R, Kumar B. Surgical management of third nerve palsy. Oman J Ophthalmol. 2016 May-Aug;9(2):80-6