Jugular vein
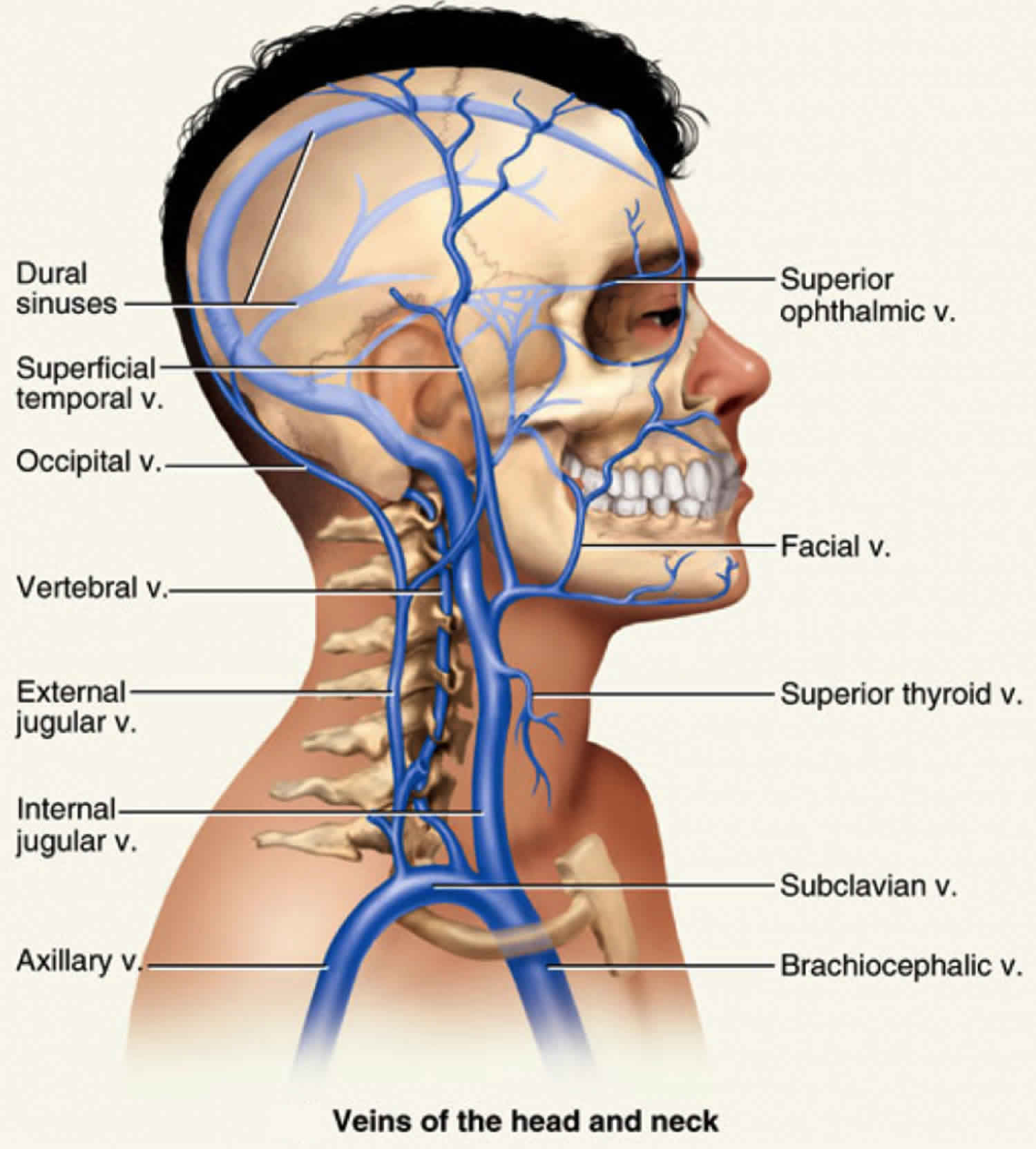
Most blood draining from the head passes into three pairs of veins: the internal jugular, external jugular, and vertebral veins.
Internal jugular vein
The internal jugular vein is a paired venous structure that collects blood from the brain, superficial regions of the face, and neck, and delivers it to the right atrium. The internal jugular vein is a run-off of the sigmoid sinus. The sigmoid sinus arises in the posterior cranial fossa and exits the cranium through the jugular foramen, located at the base of the skull. As the internal jugular vein runs down the lateral neck, it drains the branches of the facial, retromandibular, and the lingual veins. The course of the internal jugular vein is directed caudally in the carotid sheath and is accompanied by the vagus nerve posteriorly and the common carotid artery anteromedially. It lies just lateral and anterior to the internal and common carotid arteries. At the junction of the neck and thorax, the internal jugular vein combines with the subclavian vein to form the brachiocephalic or innominate vein. The left internal jugular vein is slightly smaller than the right internal jugular vein. Both veins contain valves that are located a few centimeters before the vessels drain into the subclavian vein 1.
Like many veins in the body, the internal jugular can have many anatomical variations. Some of the more clinically significant variations include a vein that is significantly smaller than expected or absent altogether.
The internal jugular vein is a preferred initial access site for a central venous catheter. Ultrasound (US) guidance is typically used for assessing cervical anatomy, patency of the vessel, the presence of a thrombus in the lumen, and the internal jugular veins relationship to the common carotid artery. The right internal jugular vein has a relatively straight course into the subclavian vein and right atrium. When cannulating the internal jugular without ultrasound guidance, the main external landmark is the division of the medial and lateral heads of the sternocleidomastoid muscle. The patient is placed in Trendelenburg positioning with their head rotated away from the side of cannulation. Under ultrasound visualization, the skin above the internal jugular vein is anesthetized with lidocaine. A 16-gauge multipurpose introducer needle is introduced and directed inferiorly toward the ipsilateral nipple. Backward pressure should be applied to the syringe as the needle is advanced. Observe the needle puncture the anterior wall of the vein with ultrasound. Once the vein is cannulated, there should be dark red, non-pulsatile blood aspirated back into the syringe. The syringe is removed, and a guidewire is advanced through the introducer needle about 5 to 10 cm. There should be no resistance felt during this step. If the patient is on telemetry, monitor the ECG for ectopy. The needle can be withdrawn over the guidewire, and a small skin incision is made using an 11-blade scalpel at its entry point. A dilator(s) is then advanced over the wire to create a subcutaneous tract. The dilator is removed, and the central venous catheter can be advanced over the wire. The guidewire is then withdrawn. Each port should be aspirated, noting adequate blood return, and then flushed with sterile saline. The catheter can then be sutured to the skin surface and dressed in a sterile fashion. A stat chest x-ray should be evaluated for appropriate placement of the catheter tip at the atriocaval junction and absence of the pneumothorax 2.
Internal jugular vein function
The function of the internal jugular vein is to collect blood from the skull, brain, superficial parts of the face, and the majority of the neck. The tributaries of the internal jugular include the inferior petrosal sinus, facial, lingual, pharyngeal, superior and middle thyroid, and, occasionally, the occipital vein. The blood collected from these vessels then drains to the brachiocephalic vein and into the right atrium.
Internal jugular vein trauma
The internal jugular vein has a superficial course in the neck and is not protected by bone or cartilage. It is beneath the sternocleidomastoid muscle and easily prone to blunt or penetrating trauma. Injury to the vein can result in significant hemorrhage as well as a risk of air embolism. Digital compression is the simplest way to control bleeding from a lacerated internal jugular vein. Surgical exploration may be necessary. If possible, the internal jugular vein should be repaired, with care take to limit narrowing the vessel. In severe cases the internal jugular vein may need to be ligated. At the time of exploration care should also be taken to assess other structures such as vagus nerve and carotid artery, as well as the nearby aerodigestive structures.
Distended internal jugular vein
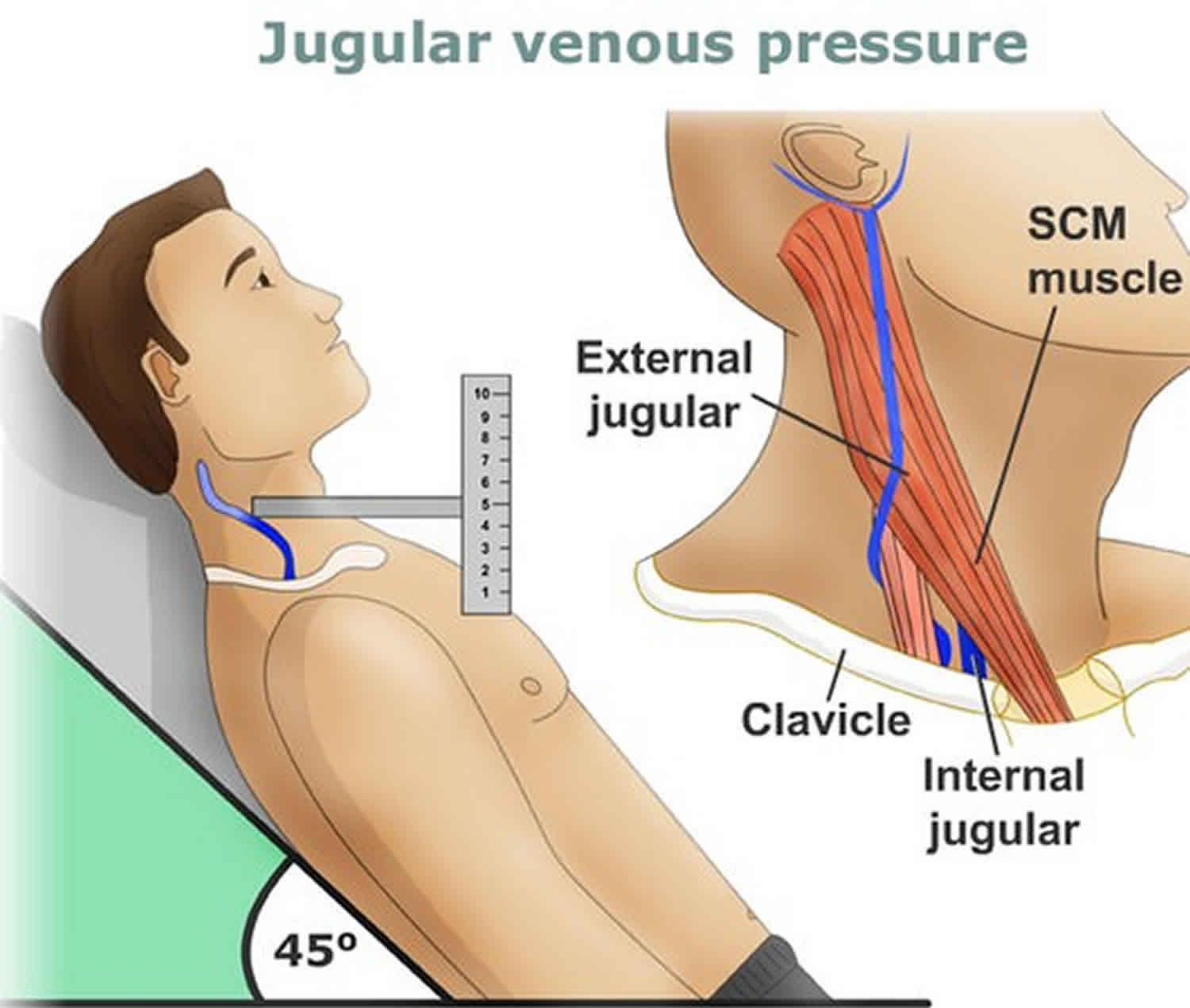
The internal jugular vein is widely used to assess the jugular venous pressure. One can roughly estimate the pressure in the right atrium by looking at the pulsations and their height in the internal jugular vein. For a professional to measure jugular venous pressure, the patient must be seated at 45 degrees with the head slightly turned to the contralateral side.
When the jugular venous pressure is low, it usually signifies low blood volume or dehydration. An important thing to note is that the pulse in the jugular vein is not palpable.
Figure 1. Jugular vein distention
Internal jugular vein distention causes
Elevations of the jugular venous pressure may be seen in cardiac tamponade, tricuspid regurgitation, right heart failure, and tricuspid stenosis. One can also raise the pressure in the jugular vein by applying manual pressure on the liver.
There are several reasons why jugular vein distention may occur, including:
- Right-sided heart failure. The right ventricle of the heart is responsible for pumping blood to the lungs to collect oxygen. The left ventricle is responsible for pumping the blood out to the rest of the body. People with right-sided heart failure have usually already experienced left-sided heart failure. The blood accumulation in the lungs caused by left ventricle failure means the right ventricle has to work harder and becomes weakened until it cannot pump effectively anymore. This failure causes the veins to bulge as blood accumulates.
- Pulmonary hypertension. This condition occurs when the pressure in blood vessels becomes dangerously high, causing their walls to thicken and stiffen, meaning less blood can pass through. This can damage the right side of the heart and increase pressure in the superior vena cava.
- Tricuspid valve stenosis. This is caused by a stiffening of the valve that separates the right atrium and the right ventricle of the heart. This results in blood backing up in the veins.
- Superior vena cava obstruction. Superior vena cava obstruction can occur if a tumor growing in the chest or a clot in the superior vena cava restricts blood flow in the vein.
- Constrictive pericarditis. If the pericardium or the fluid-filled sac around the heart becomes stiff, it can prevent the chambers of the hearts from filling up with blood properly. This situation can cause the blood to back up in the veins.
- Cardiac tamponade. This is a condition that occurs when the sac around the heart fills up with fluid and no longer allows the heart to fill with blood properly. This can happen for a variety of reasons, including infection and bleeding. It causes heart failure as well as jugular vein distention.
Distended internal jugular cannulation
The internal jugular vein is used for cannulation since it is large, superficial in location, and usually does not vary in its course along the neck. This can be the preferred initial access site for central venous catheterization. The central line may be placed to monitor jugular venous pressure, administer fluids and medications, nutrition, or resuscitate a patient. The most common complication following placement of the internal jugular vein via the neck is puncture of the carotid artery. Pneumothorax can occur if the needle is penetrated deep into the neck. However, the risk is lower when compared to subclavian access. In rare cases, the vagus nerve may also be injured.
Internal jugular vein thrombosis
Thrombosis of the internal jugular vein is usually iatrogenic as a result of an internal jugular central venous catheter. Recently, there has been an increased incidence due to intravenous drug users injecting directly into their internal jugular veins. The most common clinical manifestations of thrombosis include neck pain, fever, leukocytosis, and swelling. The swelling may also extend into the ipsilateral upper extremity. Urschel sign is occasionally appreciated in which there is distention in the lower neck and anterior chest veins as a result of the impedance of drainage from the internal jugular. Diagnosis can be made with venous duplex ultrasonography of the neck. US findings include incompressible vein, the presence of a clot, and no response to Valsalva maneuver. Contrast CT may also be used for diagnosis. Sequelae of thrombosis can include an extension of the thrombus or pulmonary embolism. Therefore, internal jugular thrombosis is viewed as a deep vein thrombosis. Treatment for thrombosis may include a need for anticoagulation.
Lemierre Syndrome
Internal jugular thrombosis as a result of pharyngeal infection is known as Lemierre Syndrome. This can occur when a pharyngeal infection, such as an abscess, extends into the internal jugular vein. A deadly complication of this process includes an extension of a septic thromboembolus into the lungs. Treatment is antibiotics and perhaps anticoagulation.
External jugular vein
The external jugular vein, located in the anterior neck, receives blood from the deeper parts of the face as well as the scalp — the external jugular vein forms from the combination of the posterior auricular and retromandibular vein. The external jugular vein starts in the parotid at the level of the angle of the mandible and runs vertically down the neck along the posterior border of the sternocleidomastoid muscle. At its distal end, the external jugular vein perforates the deep neck fascia and terminates in the subclavian vein. Throughout its course in the neck, the vein is superficial and covered by the platysma muscle. During its course from the mandible, it runs parallel with the greater auricular nerve. Like most veins, the external jugular vein also has valves at the terminal end before it enters the subclavian vein. In patients with obstruction or occlusion of the subclavian vein, the external jugular vein will appear dilated. The vein is not always visible to the naked eye. The size of the external jugular vein does vary with body habitus and size of the neck. In rare cases, there may be two small external jugular veins. The vein often has a tortuous course as it descends into the neck. Awareness of its location is essential during head and neck surgery, and the vein can be cannulated to provide fluids and medications during resuscitation.
There are many structural variants of the external jugular vein, mostly without clinical significance. They are important to be aware of for head and neck surgeons operating near the external jugular vein. A documented variant of the origin of the external jugular vein shows the vein forming from the union of retromandibular veins, the anterior jugular vein, and the facial vein 3. There can be significant variation in the connections along the external jugular vein. It is common for the facial vein to drain directly into the external jugular vein anywhere along its course. The facial vein typically drains into the internal jugular vein. Suspicions are that this abnormal anastomosis is related to persistence of the primitive linguofacial vein 4. There have also been documented cases of anastomosis between the external jugular vein and internal jugular vein, with normal venous function 5. There is a case of a persistent jugulocephalic vein with connection superficial to the clavicle. This vein had valves only allowing blood flow from the cephalic vein into the external jugular vein 6. The external jugular vein can be absent or duplicated ipsilaterally or bilaterally. The duplication does not necessarily need to be the entire length of the vein. Duplication has been observed while exiting the parotid gland or in other sections of the vein 7.
A related vein is called the vein of Kocher, or the posterior external jugular vein. It originates in the occipital region and is a tributary of the common facial vein. It travels anterior to the sternocleidomastoid muscle, in a similar fashion to the external jugular vein and can be larger than the external jugular vein in some instances. It is important to be aware of this variant for surgical purposes 7.
External jugular vein function
The external jugular vein derives from the union of the posterior auricular vein and the posterior division of the retromandibular vein, which occurs in the substance of the parotid gland at the level of the angle of the mandible. It also receives blood from the transverse cervical vein, the suprascapular vein, the superficial cervical vein, and the anterior jugular vein in some instances. The retromandibular vein anterior division joins with the facial vein to form the common facial vein. The anterior jugular vein is a related vein which is formed from submandibular veins and can drain into the external jugular vein or the subclavian vein 7. The external jugular vein most commonly drains into the subclavian vein near the middle third of the clavicle. Like most veins, the external jugular vein has a valve at the terminal end before entering the subclavian vein. The function of this valve is to inhibit the regurgitation of blood from the subclavian vein into the external jugular vein. The function of the external jugular vein is to drain blood from the superficial structures of the cranium and the deep portions of the face.
External jugular vein clinical significance
The external jugular vein is sometimes used to obtain vascular access to administer medications or IV fluids. It is a vein that is cannulated during emergency resuscitation or in patients with otherwise difficult peripheral IV access. The external jugular vein is not the first choice for venous cannulation as it is tortuous and can be challenging to cannulate in people with thick, short necks. Unlike the internal jugular vein, the risk of complications from cannulation of the external jugular vein is much less. The external jugular vein is only used for short periods of hydration. Its short course limits its use for long periods as dislodgement of the cannula is common. The patient should be asked not to rotate the neck while the external jugular vein is in use. Because of its tortuous course, the external jugular vein cannot be reliably used to assess jugular venous pressure.
To access the external jugular vein, the patient is first placed in Trendelenburg position to facilitate filling of the vein. Since a tourniquet cannot be applied, the patient can be asked to perform the Valsalva maneuver, or direct pressure can be applied just superior to the middle portion of the clavicle. Standard infection control practices are utilized by cleansing the skin with a chlorhexidine wipe and wearing gloves throughout the procedure. Needle insertion should be at a shallow angle to the skin with the tip of the needle pointing obliquely from the midline along the course of the external jugular vein. Gentle manual traction can be applied to the skin overlying or just adjacent to a more distal portion of the vein to stabilize the vein for cannulation. Once you have achieved a flash of blood in the needle, the plastic catheter can be advanced into the vessel and secured. A challenge with external jugular vein cannulation is that there may not be an appreciable flash of blood into your needle, or it may occur more slowly than in other peripheral veins due to the lower pressure in the external jugular vein. One technique that can assist the practitioner is to attach a small syringe to the needle and hold gentle negative pressure on the syringe while advancing the needle; this will allow you to see blood return into the syringe and confirm entry into the external jugular vein.
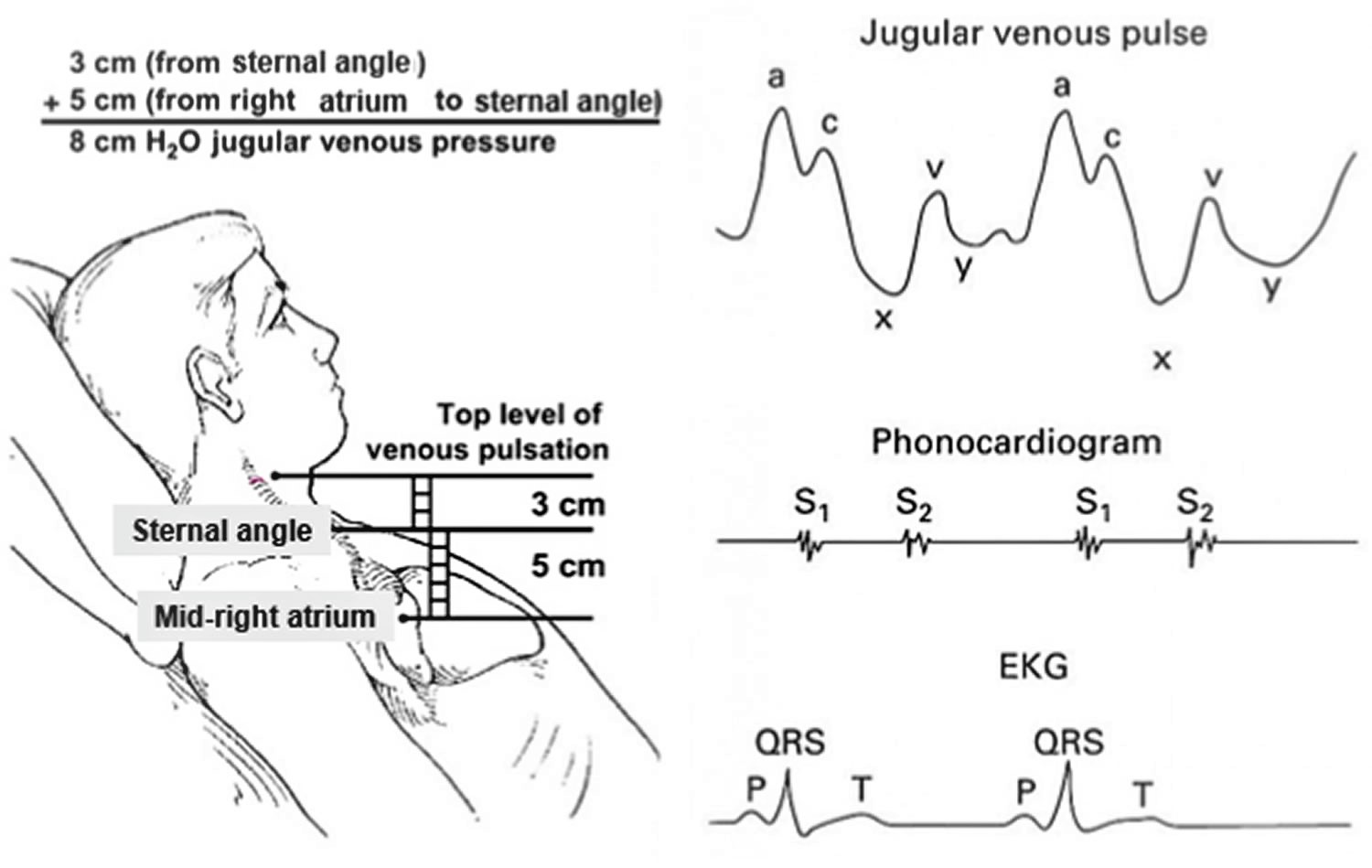
Jugular vein pulsation
Jugular venous pulse is defined as the oscillating top of vertical column of blood in the right Internal Jugular Vein that reflects the pressure changes in the right atrium in cardiac cycle. Jugular venous pressure (JVP) is the vertical height of oscillating column of blood. The anatomic relationships of the right internal and external jugular veins to the right atrium are important to an understanding of the clinical evaluation of the venous pulse. The right internal jugular vein communicates directly with the right atrium via the superior vena cava. There is a functional valve at the junction of the internal jugular vein and the superior vena cava. Usually, however, this valve does not impede the phasic flow of blood to the right atrium. Thus the wave form generated by phasic flow to the right atrium is accurately reflected in the internal jugular vein. The external jugular vein descends from the angle of the mandible to the middle of the clavicle at the posterior border of the sternocleidomastoid muscle. The external jugular vein possesses valves that are occasionally visible. The relatively direct line between the right external and internal jugular veins, as compared to the left external and internal jugular veins, make the right jugular vein the preferred system for assessing the venous pressure and pulse contour. While it has been suggested that blood flow within the external jugular vein is nonpulsatile and thus cannot be used to assess the contour of the jugular venous pulse, my exerience is contrary to this view. Thus, either the external or internal jugular vein may be useful in the assessment of mean venous pressure and pulse contour.
The jugular venous pressure is usually assessed by observing the right side of the patient’s neck. The normal mean jugular venous pressure (JVP), determined as the vertical distance above the midpoint of the right atrium, is 6 to 8 cm H2O 8. Deviations from this normal range reflect either hypovolemia (i.e., mean venous pressure less than 5 cm H2O) or impaired cardiac filling (i.e., mean venous pressure greater than 9 cm H2O). The normal jugular venous pulse contains three positive waves. By convention these are labeled “a,” “c”, and “v” (Figure 2). These positive deflections occur, respectively, before the carotid upstroke and just after the P wave of the ECG (a wave); simultaneous with the upstroke of the carotid pulse (c wave); and during ventricular systole until the tricuspid valve opens (v wave). The a wave is generated by atrial contraction, which actively fills the right ventricle in end-diastole. The c wave is caused either by transmission of the carotid arterial impulse through the external and internal jugular veins or by the bulging of the tricuspid valve into the right atrium in early systole. The v wave reflects the passive increase in pressure and volume of the right atrium as it fills in late systole and early diastole. Normally the crests of the a and v waves are approximately equal in amplitude. The descents or troughs (Figure 2) of the jugular venous pulse occur between the “a” and “c” wave (“x” descent), between the “c” and “v” wave (“x” descent), and between the “v” and “a” wave (“y” descent). The x and x′ descents reflect movement of the lower portion of the right atrium toward the right ventricle during the final phases of ventricular systole. The y descent represents the abrupt termination of the downstroke of the v wave during early diastole after the tricuspid valve opens and the right ventricle begins to fill passively. Normally the y descent is neither as brisk nor as deep as the x descent.
In determining mean jugular venous pressure, one assumes that the filling pressure of the right atrium and right ventricle mirror that of the left atrium and left ventricle. This relationship is usually correct. Thus, a mean jugular venous pressure greater than 10 cm H2O usually indicates volume overload, while a low jugular venous pressure (i.e., less than 5 cm H2O) usually indicates hypovolemia. But there are important, notable exceptions to this relationship. First, acute left ventricular failure (as may be caused by a myocardial infarction) may significantly raise the pulmonary capillary wedge pressure without raising the mean right atrial and jugular venous pressures. Second, pulmonary hypertension, tricuspid insufficiency, or stenosis may be associated with elevated mean right atrial and jugular venous pressures while leaving the left heart pressures unaffected. In using the mean jugular venous pressure in clinical practice, the physician must correlate this bedside measurement with the other information gained from the history and physical examination.
Figure 2. Jugular vein pulsation
Abnormalities in the jugular venous pulse may be reflected in either the mean pressure, amplitude, or configuration of the positive waves or negative troughs, or in the sequence or absence of the positive waves. In this chapter emphasis is placed on measurement of the jugular venous pressure, use of the venous pulse to determine cardiac rhythm, and the more common cardiac problems of pulmonary hypertension, tricuspid regurgitation, and constrictive pericarditis.
Jugular venous pulse measurement technique
Evaluation of the jugular venous pulse is perhaps one of the most misunderstood and difficult to master physical diagnosis techniques. Once understood and practiced in a repetitive manner during each physical examination, the mysticism surrounding assessment of the jugular venous pulse disappears. Nevertheless, attention to a few basic points is crucial for proper examination of the venous pulse.
First, the patient must be positioned in a manner so that the physician can observe the venous pulse. Thus, the neck and chest must be bared to permit an unobstructed view from the midportion of the sternum to the antihelix of the ears. This requires that the dressing gown (preferrably opening to the patient’s back) be positioned at the level of the nipples. Moreover, a woman’s long hair should be tucked out of the way behind her head. Second, the patient should be reclining in a comfortable position. Except for patient comfort, the exact angle of inclination from horizontal is relatively unimportant. Indeed, this angle does not even need to be reported in the physical examination, since the mean venous pressure can be given in units of “centimeters of water,” which is an absolute number. In general, patients who are dyspneic will not tolerate reclining at angles of less than 45 to 60 degrees from horizontal, and thus this should be the initial position of the head of the bed. Third, the examining table (or hospital bed) should be raised to a comfortable height for the physician. The cardiac examination—if performed properly—is time-consuming and must not be hurried; physical discomfort on the physician’s part will detract from the adeptness of his bedside skills. Fourth, an adequate light source with a strong beam must be readily available. This source may be either a pocket flashlight (with a strong battery) or a bedside lamp that the physician can direct. Ambient room or window lighting is not usually as good as directed artificial lighting.
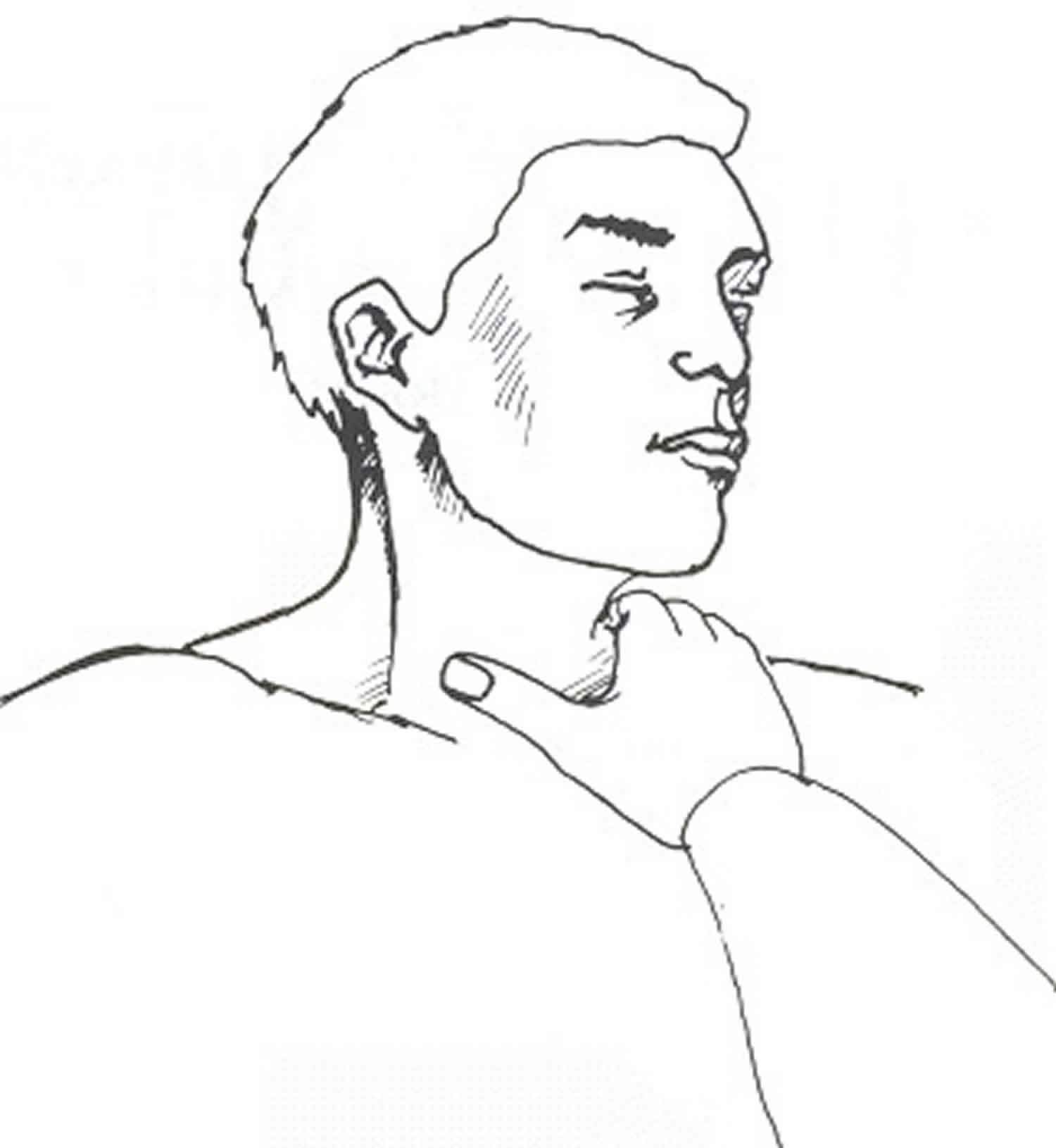
The light source is directed tangentially at approximately a 45-degree angle to the saggital plane from behind the right midscapular area across the right side of the neck toward the midline (Figure 3). The examiner should locate, by direct observation, the venous pulsations in the right side of the neck. Usually the patient’s chin must be extended to enhance this observation. But care should be exercised so that the sternocleidomastoid muscle is not excessively tensed, thus compressing the external and internal jugular veins and obliterating their pulsations. It is crucial that the examiner be certain to distinguish between venous and arterial pulsations, and that the top of the venous column is recognized. The former is accomplished by seeking the three crests in the venous pulse and comparing them to the carotid arterial pulse. It is easiest to observe the pulsations in the right side of the neck while timing the carotid pulse in the left side of the patient’s neck using your right third finger (Figure 3). If you’re still uncertain as to whether or not you’re observing the venous pulse, try to obliterate the venous pulse by placing your right thumb or index finger across the base of the patient’s right neck (Figure 4). By compressing this area with a force of approximately 10 to 20 mm Hg, the venous pulse can be obliterated. Movement that remains will then be observed to have the characteristic monophasic contour of the carotid pulse. During this maneuver, it is important to continue to cast a tangential light across the right side of the neck in order to observe the contour of the various pulses.
Figure 3. Jugular venous pressure measurement
Figure 4. Jugular venous pressure obliteration
The next step is to determine the height of the mean jugular venous pressure, measured in centimeters of water, above the midpoint of the right atrium. The latter position is chosen because it is the standard reference point for all hemodynamic measurements in the catheterization laboratory. Moreover, the midpoint of the right atrium is at a constant fixed relationship (i.e., 5 cm) below the sternal angle of Louis regardless of the patient’s anatomic position. Thus, whether the patient is lying flat or sitting erect, this anatomic relationship holds true. To determine the mean jugular venous pressure, the examiner should observe the nadir of the venous column on inspiration and then the crest of this column on expiration. Next, the midpoint of the excursion of the venous pulse during normal respiratory cycles is estimated visually. Exaggerated breathing or breath holding distorts the normal mean venous pressure and should be avoided. A horizontal line is drawn from this estimated point to intersect a vertical line, which is erected perpendicular to the ground through the sternal angle of Louis. The distance between the sternal angle and this intercept is measured (Figure 2). The sum of this distance—plus the obligatory 5-cm fixed relationship to the midpoint of the right atrium—represents the mean jugular venous pressure (JVP).
Assuming that the top of the venous column has been observed, the degree of the patient’s inclination from horizontal does not have to be stated. While a ruler may be used to measure the distance between the intercept and the sternal angle of Louis, this appliance may not always be readily available. If the width of the observer’s fingers is known, these may serve the same purpose.
Next, the examiner observes the rise and fall of the venous pressure during normal inspiration and expiration. Normally, the mean venous pressure falls during inspiration. It is especially important that the patient does not perform a Valsalva maneuver or hold his breath during this procedure. Finally, the examiner applies firm but persistent pressure over the liver for 10 seconds while observing the mean jugular venous pressure. Normally there is either no rise or only a transient (i.e., 2 to 3 sec) rise in mean jugular venous pressure. A sustained increase in the mean venous pressure until abdominal compression is released is abnormal and indicates impaired right heart function. This abnormal response is called hepatojugular reflux. After determining the mean jugular venous pressure, the venous pulse contour should be examined by simultaneously observing the venous pulse in the right side of the neck while palpating the left carotid artery (Figure 2). A crest in the jugular venous pulse immediately preceding the carotid impulse is an “a” wave; that occurring with the carotid upstroke is the “c” wave; and that occurring after the carotid impulse has peaked is the “v” wave. The “a” wave and “c” waves occur relatively close together, while the “v” wave is observed to be separated from them by a longer interval.
References- Mumtaz S, Singh M. Surgical review of the anatomical variations of the internal jugular vein: an update for head and neck surgeons. Ann R Coll Surg Engl. 2019 Jan;101(1):2-6
- Cheng S, Xu S, Guo J, He Q, Li A, Huang L, Liu Z, Li S. Risk Factors of Central Venous Catheter-Related Bloodstream Infection for Continuous Renal Replacement Therapy in Kidney Intensive Care Unit Patients. Blood Purif. 2018 Nov 28;:1-8
- Chauhan NK, Rani A, Chopra J, Rani A, Srivastava AK, Kumar V. Anomalous formation of external jugular vein and its clinical implication. Natl J Maxillofac Surg. 2011 Jan;2(1):51-3
- Choudhry R, Tuli A, Choudhry S. Facial vein terminating in the external jugular vein. An embryologic interpretation. Surg Radiol Anat. 1997;19(2):73-7
- Karapantzos I, Zarogoulidis P, Charalampidis C, Karapantzou C, Kioumis I, Tsakiridis K, Mpakas A, Sachpekidis N, Organtzis J, Porpodis K, Zarogoulidis K, Pitsiou G, Zissimopoulos A, Kosmidis C, Fouka E, Demetriou T. A rare case of anastomosis between the external and internal jugular veins. Int Med Case Rep J. 2016;9:73-5
- Wysiadecki G, Polguj M, Topol M. Persistent jugulocephalic vein: case report including commentaries on distribution of valves, blood flow direction and embryology. Folia Morphol. (Warsz). 2016;75(2):271-274
- Dalip D, Iwanaga J, Loukas M, Oskouian RJ, Tubbs RS. Review of the Variations of the Superficial Veins of the Neck. Cureus. 2018 Jun 18;10(6):e2826
- Applefeld MM. The Jugular Venous Pressure and Pulse Contour. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 19. Available from: https://www.ncbi.nlm.nih.gov/books/NBK300