What is kyphoplasty
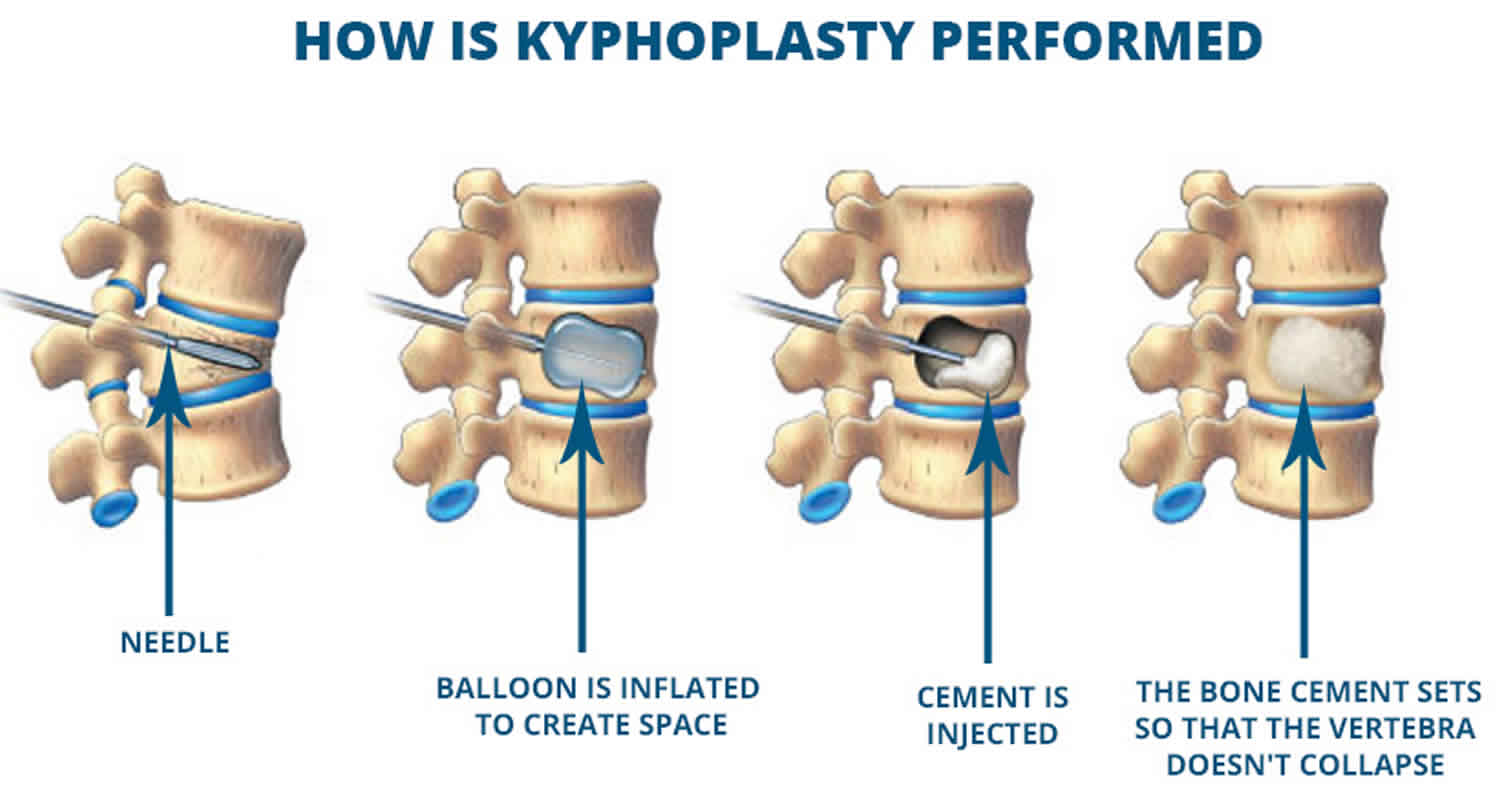
Kyphoplasty is used to treat painful compression fractures in the spine 1. In a compression fracture, all or part of a spine bone collapses. The procedure is also called balloon kyphoplasty. In a kyphoplasty, a needle is inserted into the fractured vertebra using an x-ray for guidance. A small device called a balloon tamp is then inserted through the needle and into the fractured vertebra 2. The balloon tamp is inflated from within the vertebra, which restores the height and shape of the vertebral body. When the balloon tamp is removed, it leaves a cavity that is filled with a special bone cement that strengthens the vertebra.
Kyphoplasty is generally recommended in the treatment of osteoporotic or osteolytic painful progressive vertebral compression fractures. Kyphoplasty has been shown to provide symptomatic relief in patients with vertebral compression fractures from primary spinal tumors or metastatic spine tumors. Kyphoplasty is typically useful in patients who are bedridden and unable to mobilize because of the pain associated with vertebral compression fractures. Early pain relief and mobility are crucial in avoiding complications associated with prolonged recumbency, like pneumonia, deep vein thrombosis, pulmonary embolism, or decubiti.
Kyphoplasty can be performed using general anesthesia (which puts you to sleep) or with a local anesthesia (which numbs your body around the fracture). In this procedure, the patient lies face down on the operating table and the surgeon accesses the spine from the back.
After surgery, patients can go back to all their normal activities of daily living as soon as possible with no restrictions.
A common cause of compression fractures of the spine is thinning of your bones, or osteoporosis. Your provider may recommend this procedure if you have severe and disabling pain for 2 months or more that does not get better with bed rest, pain medicines, and physical therapy.
Your doctor may also recommend kyphoplasty procedure if you have a painful compression fracture of the spine due to:
- Cancer, including multiple myeloma
- Injury that caused broken bones in the spine
Vertebroplasty vs Kyphoplasty
Vertebroplasty and kyphoplasty are minimally invasive procedures used to treat painful vertebral compression fractures in the spinal column, which are a common result of osteoporosis.
Vertebroplasty is a technique similar to kyphoplasty, but a balloon tamp is not used to create a space for the cement. Instead, bone cement is injected directly into into back bones (vertebrae) that have cracked or broken, often because of osteoporosis. Like kyphoplasty, this procedure is performed while the patient is lying face down so that the surgeon can access the fractured vertebra from the back. The cement hardens, stabilizing the fractures and supporting your spine.
For people with severe, disabling pain caused by a compression fracture, vertebroplasty can relieve pain, increase mobility and reduce the use of pain medication.
After vertebroplasty surgery, patients are encouraged to return to their normal, day-to-day activities as soon as possible.
Kyphoplasty is similar to vertebroplasty, but uses special balloons to create spaces within the vertebra that are then filled with bone cement. Kyphoplasty can correct spinal deformity and restore lost height.
Several reports have been published on the results of vertebral augmentation procedures. In two large studies, the benefit of vertebroplasty was found to be very short term. In contrast, studies indicate that kyphoplasty may increase function and decrease pain more quickly than nonoperative treatment.
The American Academy of Orthopaedic Surgeons has reviewed the current research on osteoporotic spinal compression fractures and developed a Clinical Practice Guideline that provides evidence-based information about vertebral augmentation procedures.
Typically, vertebroplasty and kyphoplasty are recommended after less invasive treatments, such as bed rest, a back brace or pain medication, have been ineffective. Vertebroplasty and kyphoplasty can be performed immediately in patients with problematic pain requiring hospitalization or for conditions that limit bed rest and pain medications.
Vertebroplasty and kyphoplasty are also performed on patients who:
- are elderly or frail and will likely have impaired bone healing after a fracture
- have vertebral compression due to a malignant tumor
- suffer from osteoporosis due to long-term steroid treatment or a metabolic disorder
Vertebroplasty and kyphoplasty should be completed within eight weeks of the acute fracture for the highest probability of successful treatment.
Vertebroplasty and kyphoplasty benefits
- Vertebroplasty and kyphoplasty can increase a patient’s functional abilities and allow return to the previous level of activity without any form of physical therapy or rehabilitation.
- These procedures are usually successful at alleviating the pain caused by a vertebral compression fracture; many patients feel significant relief almost immediately or within a few days. Many patients become symptom-free.
- Following vertebroplasty, about 75 percent of patients regain lost mobility and become more active, which helps combat osteoporosis. After the procedure, patients who had been immobile can get out of bed, and this can help reduce their risk of pneumonia. Increased activity builds more muscle strength, further encouraging mobility.
- Usually, vertebroplasty and kyphoplasty are safe and effective procedures.
- No surgical incision is needed—only a small nick in the skin that does not have to be stitched.
Table 1. Summary of published articles about the effect of kyphoplasty on mortality rates in vertebral compression fractures patients.
| Source | Study Design | Number of patients | Comparisons | Conclusion |
| Lavelle et al 3 | Retrospective | 184 | Conservative; kyphoplasty | Mortality rate was not significantly different between kyphoplasty and conservative cohorts. |
| Edidin et al 4 | Retrospective | 858,978 | Nonoperative; kyphoplasty; vertebroplasty | The 4-year survival rates were 62.8% for kyphoplasty and 57.3% for vertebroplasty. Operated patients were 37% less likely to die compared with nonoperated patients at 4-year follow-up. |
| Chen et al, 5 | Retrospective | 72,693 | Nonoperative; kyphoplasty; vertebroplasty | The 3-year survival rates were 59.9%, 49.7%, and 42.3% for kyphoplasty, vertebroplasty, and nonoperated cohorts, respectively. |
| Edidin et al 6 | Retrospective | 858,978 | Nonoperative; kyphoplasty; vertebroplasty | Adjusted life expectancy was 85% higher in operated patients compared with nonoperated patients. Kyphoplasty patients had 115% and 34% greater adjusted life expectancy compared with nonoperated and vertebroplasty groups, respectively. |
| Lange et al 7 | Retrospective | 3605 | Nonoperative; kyphoplasty; vertebroplasty | At 5-year follow-up, the operated patients were 43% less likely to die compared with the nonoperated patients. Mortality rate was not significantly different between kyphoplasty and vertebroplasty. |
| Edidin et al 8 | Retrospective | 1,038,956 | Nonoperative; kyphoplasty; vertebroplasty | The 4-year adjusted mortality risk was 74% higher in the nonoperated cohort compared with kyphoplasty, and 17% lower in kyphoplasty compared with vertebroplasty. |
Kyphoplasty precautions
Kyphoplasty is usually contraindicated in patients who have posterior wall disruption as a result of extension of the fracture or by infiltrative process in the case of metastatic lesions 1.
Absolute contraindications to vertebroplasty and kyphoplasty are 9:
- Unmanageable bleeding disorder
- Improvement of the symptoms of the patient with conservative management
- Asymptomatic vertebral body fracture,
- Local or generalized infection
- Allergy to bone cement
- Tumour mass with involvement of the spinal canal.
Vertebroplasty and kyphoplasty are NOT:
- used for herniated disks or arthritic back pain.
- generally recommended for otherwise healthy younger patients, mostly because there is limited experience with cement in a vertebral body for longer time periods. These patients also tend to heal faster than elderly patients or those with osteoporosis.
- a preventive treatment to help patients with osteoporosis avoid future fractures. It is used only to repair a known, non-healing compression fracture if it is due to a recent fracture.
- used to correct an osteoporosis-induced curvature of the spine, but it may keep the curvature from worsening if it is due to a recent fracture.
- ideal for someone with severe emphysema or other lung disease because it may be difficult for such individuals to lie facedown for the one to two hours vertebroplasty requires. Special accommodations may be made for patients with these conditions.
- for patients with a healed (chronic) vertebral fracture.
- appropriate for patients with young healthy bones or those who have suffered a fractured vertebra in an accident.
- suitable for patients with spinal curvature such as scoliosis or kyphosis that results from causes other than osteoporosis.
- applicable for patients who suffer from spinal stenosis or herniated disk with nerve or spinal cord compression and loss of neurologic function.
Kyphoplasty procedure
Before the kyphoplasty procedure
A clinical evaluation will be performed to confirm the presence of a compression fracture that may benefit from treatment with vertebroplasty or kyphoplasty. The evaluation may include:
- diagnostic imaging
- blood tests
- a physical exam
- spine x-rays
- radioisotope bone scan
- magnetic resonance imaging (MRI)
- computed tomography (CT)
Before kyphoplasty procedure, always tell your doctor:
- If you could be pregnant
- Which drugs you are taking, even those you bought without a prescription
- If you have been drinking a lot of alcohol
You may be given bone-strengthening medication during treatment.
You should report to your doctor all medications that you are taking, including herbal supplements, and if you have any allergies, especially to local anesthetic medications, general anesthesia or to contrast materials containing iodine (sometimes referred to as “dye” or “x-ray dye”). Your physician may advise you to stop taking aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs) or blood thinners for a specified period of time before your procedure.
Women should always inform their physician and x-ray technologist if there is any possibility that they are pregnant. Many imaging tests are not performed during pregnancy so as not to expose the fetus to radiation. If an x-ray is necessary, precautions will be taken to minimize radiation exposure to the baby. See the Safety page for more information about pregnancy and x-rays.
You will need to have blood drawn for tests prior to the procedure to determine if your blood clots normally.
During the days before the kyphoplasty procedure:
- You may be asked to stop taking aspirin, ibuprofen, coumadin (warfarin), and other drugs that make it hard for your blood to clot.
- Ask which drugs you should still take on the day of the surgery.
- If you smoke, try to stop.
On the day of the kyphoplasty procedure:
- You will most often be told not to drink or eat anything for several hours before the test.
- Take the drugs your provider told you to take with a small sip of water.
- You will be told when to arrive.
During the kyphoplasty procedure
Kyphoplasty is done in a hospital or outpatient clinic. However, some patients may require admission following the procedure. Please consult with your physician as to whether or not you will be admitted.
- You may be connected to monitors that track your heart rate, blood pressure and pulse during the procedure.
- A nurse or technologist will insert an intravenous (IV) line into a vein in your hand or arm so that sedative medication can be given intravenously. Moderate sedation may be used. As an alternative, you may receive general anesthesia.
- You may be given medications to help prevent nausea and pain, and antibiotics to help prevent infection. You will be positioned lying face down for the procedure.
- You lie face down on a table. The health care provider cleans the area of your back and applies medicine to numb the area.
- The area through which the hollow needle, or trocar, will be inserted will be shaved, sterilized with a cleaning solution and covered with a surgical drape.
- You may have local anesthesia (awake and unable to feel pain) injected into your skin and deep tissues, near the fracture. You will likely also receive medicine to help you relax and feel sleepy.
- Or you may receive general anesthesia. You will be asleep and unable to feel pain.
- A very small skin incision is made at the site.
- Using real-time x-ray images, a hollow needle or trocar is passed through the spinal muscles until its tip is precisely positioned within the fractured vertebra. You may feel a tapping sensation during the procedure as the trocar is advanced into the bone.
- A balloon is placed through the needle, into the bone, and then inflated. This restores the height of the vertebrae.
- Cement is then injected into the space to make sure it does not collapse again. The orthopedic cement includes an ingredient called polymethylmethacrylate (PMMA). Its physical appearance resembles toothpaste, which hardens soon after placement in the body.
- X-rays and/or a CT scan may be performed at the end of the procedure to check the distribution of the cement.
- Pressure will be applied to prevent any bleeding and the opening in the skin is covered with a bandage. No sutures are needed.
- This procedure is usually completed within one hour. It may take longer if more than one vertebral body level is being treated.
- Your intravenous line will be removed.
Kyphoplasty recovery
You will probably go home on the same day of the kyphoplasty procedure. You should not drive, unless your doctor says it is OK.
You will be advised to increase your activity gradually and resume all your regular medications. At home, patients may return to their normal daily activities, although strenuous exertion, such as heavy lifting, should be avoided for at least six weeks.
If you take blood thinners, check with your doctor about restarting this medication the day after your procedure.
Pain relief is immediate for some patients. In others, pain is eliminated or reduced within two days. Pain resulting from the procedure will typically diminish within two to three days.
For two or three days afterward, you may feel a bit sore at the point of the needle insertion. You can use an icepack to relieve any discomfort but be sure to protect your skin from the ice with a cloth and ice the area for only 15 minutes per hour. Your bandage should remain in place for 48 hours. Do not immerse the bandage in water for 48 hours. This is to prevent infection. Taking showers is allowed.
Kyphoplasty recovery time
- Approximately one hour after the procedure, you should be able to walk. However, it is best to stay in bed for the first 24 hours, except to use the bathroom.
- After 24 hours, slowly return to your regular activities.
- Avoid heavy lifting and strenuous activities for at least 6 weeks.
- Apply ice to the wound area if you have pain where the needle was inserted.
Your interventional radiologist may recommend a follow-up visit after your procedure or treatment is complete.
The visit may include a physical check-up, imaging procedure(s) and blood or other lab tests. During your follow-up visit, you may discuss with your doctor any changes or side effects you have experienced since your procedure or treatment.
Kyphoplasty prognosis
People who have kyphoplasty surgery often have less pain and a better quality of life after the surgery. They often need fewer pain medicines, and can move better than before.
Kyphoplasty complications
Kyphoplasty is generally safe.
Kyphoplasty complications may include:
- Bleeding
- Infection
- Allergic reactions to medicines
- Breathing or heart problems if you have general anesthesia
- Nerve injuries
- Leakage of the bone cement into surrounding area (this can cause pain if it affects the spinal cord or nerves). Leakage can lead to other treatments to remove the cement.
Cement extravasation is one of the possible complications of vertebroplasty 9. The reported incidence is up to 40% in patients with osteoporotic fractures. Paravertebral soft tissue, intervertebral disc, needle tract, epidural and paravertebral veins, the spinal canal and the neuroforamen can be invaded. The clinical relevance of this complication will be different in relation to the anatomical structure which is invaded from the cement. Cement invasion into the vena cava, lungs, heart and even the kidneys have been described 10. These major adverse events only occur in less than 1% of the patients 11, and require immediate management.
Kyphoplasty risks
- Any procedure where the skin is penetrated carries a risk of infection. The chance of infection requiring antibiotic treatment appears to be less than one in 1,000.
- A small amount of orthopedic cement can leak out of the vertebral body. This does not usually cause a serious problem, unless the leakage moves into a potentially dangerous location such as the spinal canal or the blood vessels of the lungs.
- Other possible complications include infection, bleeding, increased back pain and neurological symptoms such as numbness or tingling. Paralysis is extremely rare.
- Approximately 10 percent of patients may develop additional compression fractures after vertebroplasty or kyphoplasty. When this occurs, patients usually have relief from the procedure for a few days but develop recurrent pain soon thereafter.
- There is a low risk of allergic reaction to the medications.
- Kurra S, Metkar U, Lieberman IH, Lavelle WF. The Effect of Kyphoplasty on Mortality in Symptomatic Vertebral Compression Fractures: A Review. Int J Spine Surg. 2018;12(5):543-548. Published 2018 Oct 15. doi:10.14444/5066 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6198625/
- Initial outcome and efficacy of “kyphoplasty” in the treatment of painful osteoporotic vertebral compression fractures. Lieberman IH, Dudeney S, Reinhardt MK, Bell G. Spine (Phila Pa 1976). 2001 Jul 15; 26(14):1631-8.
- Lavelle WF, Khaleel MA, Cheney R, Demers E, Carl AL. Effect of kyphoplasty on survival after vertebral compression fractures. Spine J. 2008;8(5):763–769.
- Edidin AA, Ong KL, Lau E, Kurtz SM. Mortality risk for operated and nonoperated vertebral fracture patients in the Medicare population. J Bone Miner Res. 2011;26(7):1617–1626.
- Chen AT, Cohen DB, Skolasky RL. Impact of nonoperative treatment, vertebroplasty, and kyphoplasty on survival and morbidity after vertebral compression fracture in the Medicare population. J Bone Joint Surg Am. 2013;95(19):1729–1736.
- Edidin AA, Ong KL, Lau E, Kurtz SM. Life expectancy following diagnosis of a vertebral compression fracture. Osteoporos Int. 2013;24(2):451–458.
- Lange A, Kasperk C, Alvares L, Sauermann S, Braun S. Survival and cost comparison of kyphoplasty and percutaneous vertebroplasty using German claims data. Spine (Phila Pa 1976) 2014;39(4):318–326.
- Edidin AA, Ong KL, Laue E, Kurtz SM. Morbidity and mortality after vertebral fractures: comparison of vertebral augmentation and nonoperative management in the Medicare population. Spine (Phila Pa 1976) 2015;40(15):1228–1241.
- Denaro V, Longo UG, Maffulli N, Denaro L. Vertebroplasty and kyphoplasty. Clin Cases Miner Bone Metab. 2009;6(2):125-30. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2781232/
- Quesada N, Mutlu GM. Images in cardiovascular medicine. Pulmonary embolization of acrylic cement during vertebroplasty. Circulation. 2006;113:e295–296.
- Nussbaum DA, Gailloud P, Murphy K. A review of complications associated with vertebroplasty and kyphoplasty as reported to the Food and Drug Administration medical device related web site. J Vasc Interv Radiol. 2004;15:1185–1192.