What is laryngomalacia
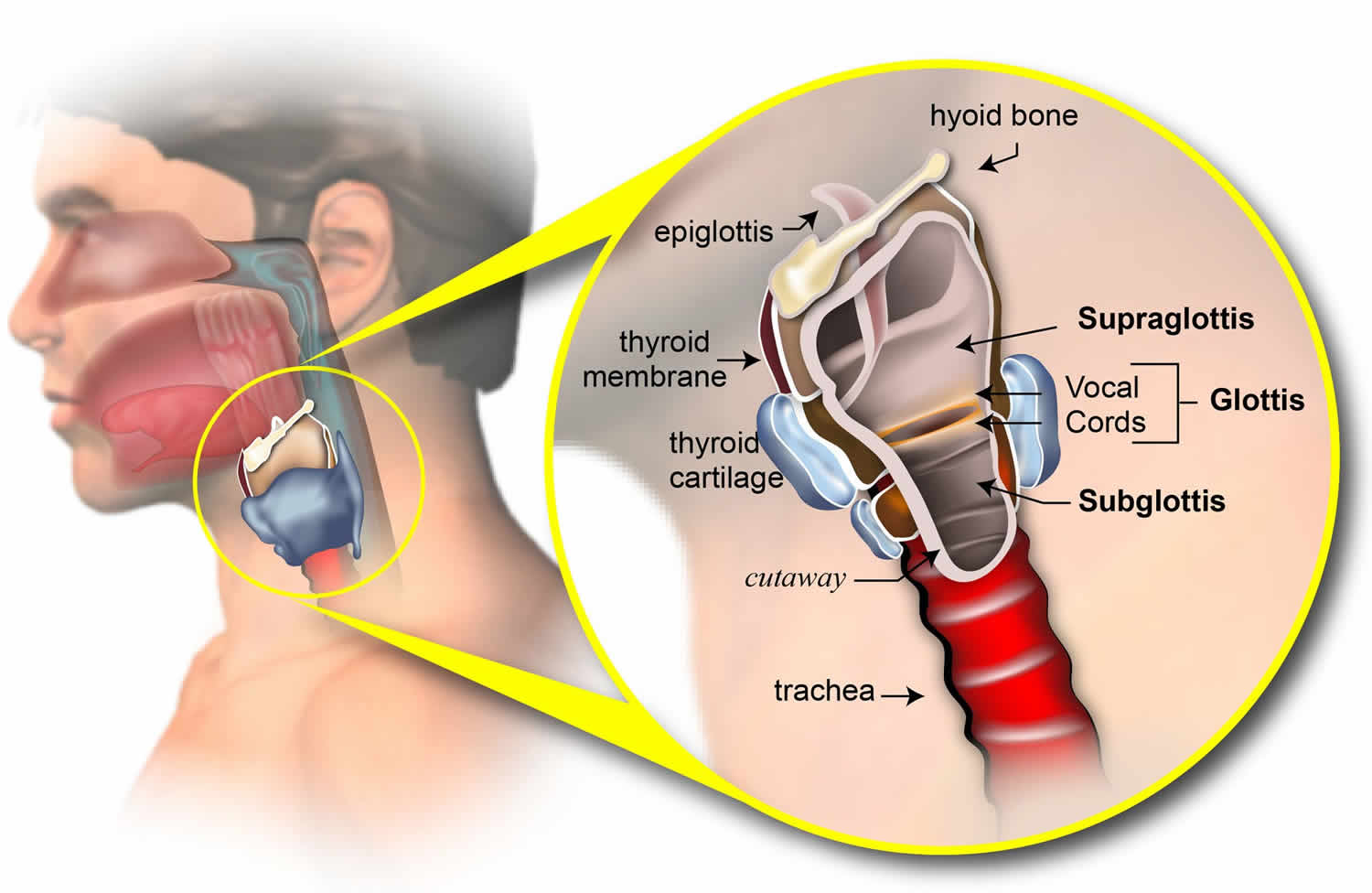
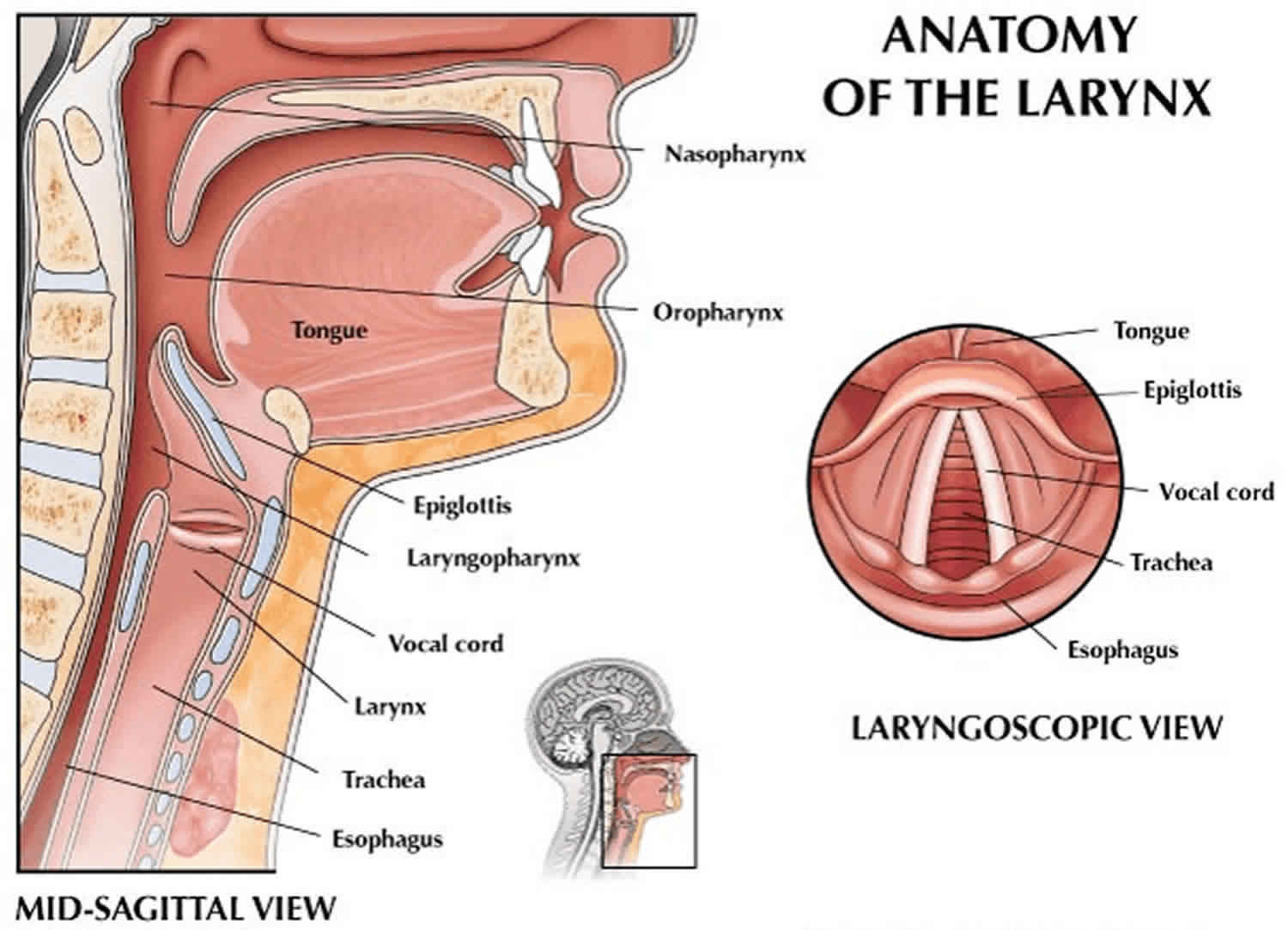
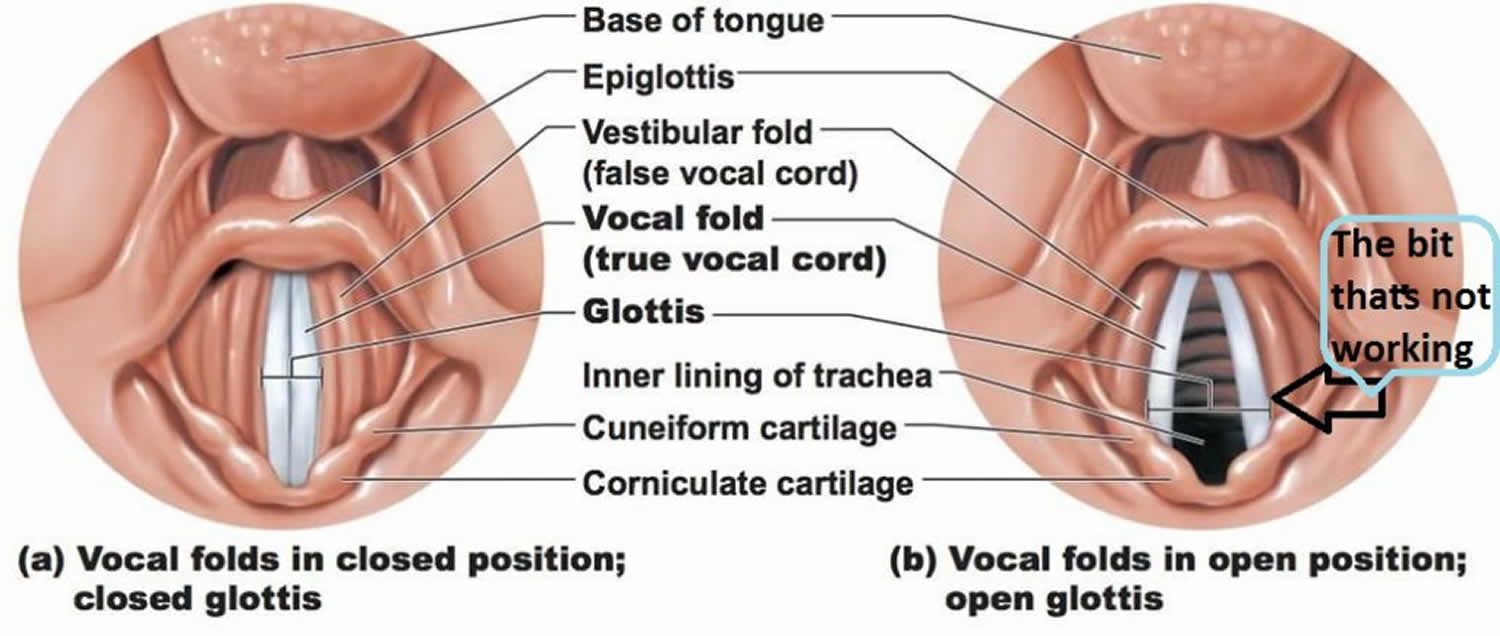
Laryngomalacia also known as “floppy airway” or laryngealmalacia, is a congenital (present at birth) softening of the tissues of the larynx (voice box) above the vocal cords. Laryngomalacia is best described as floppy tissue above the vocal cords that falls into the airway when a child breathes in and partially block it. Laryngomalacia is defined as a supraglottic collapse of the glottis, resulting in intermittent airflow obstruction and associated wheezing 1. Laryngomalacia is the most common cause of stridor in babies 2. Stridor results from upper airway obstruction caused by collapse of supraglottic tissue into the airway. The laryngeal structure is malformed and floppy, causing the tissues to fall over the airway opening and partially block it. Most cases of laryngomalacia are mild and self-resolve, but severe symptoms require investigation and intervention. There is a strong association with gastroesophageal reflux disease (GERD) in patients with laryngomalacia, and thus medical treatment with antireflux medications may be indicated.
Most infants with laryngomalacia are born without complication and are discharged home before symptoms develop. Over the first few weeks of life, most infants with laryngomalacia will develop a characteristic high-pitched inspiratory stridor. The sound can be alarming to parents and others, but in most cases infants are otherwise happy and developing well. Symptoms may become worse with agitation, crying, excitement, during feeding or position / sleeping on their back. The cry is invariably normal and sleep is usually uneventful. However, noisy breathing may be present in babies up to 1 year of age. Symptoms will often increase or get worse over the first few months after diagnosis, usually between 4-8 months of age. Most children outgrow the noisy breathing (stridor) by 12-18 months of age.
In a series of 88 children with confirmed laryngomalacia, most patients presented with stridor alone, but atypical presentations of snoring or obstructive sleep apnea syndrome occurred in 25%, and swallowing dysfunction occurred in 11% 3. Laryngomalacia has also been recognized as a cause of obstructive sleep apnea syndrome in older children and may occur alone or in concert with additional dynamic or fixed lesions to cause obstructive sleep apnea syndrome 3. Acquired laryngomalacia has been reported in a few cases following adenotonsillectomy 3.
In most cases, laryngomalacia in infants is not a serious condition — they have noisy breathing, but are able to eat and grow. For these infants, laryngomalacia will resolve without surgery by the time they are 18 to 24 months old. However, a small percentage of babies with laryngomalacia do struggle with breathing, eating and gaining weight. These symptoms require prompt attention. Proper identification of those patients who require medical and surgical intervention is key to providing treatment with successful outcomes. Supraglottoplasty is the preferred surgical treatment of laryngomalacia, reserved only for severe cases.
Cases of laryngomalacia fall into the “moderate” category when there are feeding and weight gain issues and sleep disruption. In these cases, laryngeal sensation may be blunted, leading to a discoordination of the suck-swallow-breath mechanics. Due to the coexistence of gastroesophageal reflux and laryngomalacia, these symptomatic patients should be managed with anti-reflux therapy and closely monitored.
About 5% of infants with laryngomalacia will fall into the severe range with failure to thrive, obstructive sleep apnea, and/or signs of respiratory distress including tachypnea and retractions. These children require supraglottoplasty surgery to relieve the obstruction.
Most infants with laryngomalacia will have mild to moderate symptoms, have minimal impairment of feeding with normal weight gain and no significant increase in the work of breathing and not require surgical intervention. More than 90% of laryngomalacia babies will have resolution of their symptoms from 18 months to 2 years of age 4. Those with gastroesophageal reflux disease (GERD) or laryngopharyngeal reflux have symptoms improvement from acid suppression therapy 5. In approximately 10%, the laryngomalacia symptoms will extend beyond stridor to include respiratory distress with retractions and cyanosis and failure to thrive as a result of the inability to coordinate breathing with swallowing and maintain adequate caloric reserves 4. Supraglottoplasty has proved to be successful for surgical management in this small subset of infants with severe symptoms 6. Surgical correction (supraglottoplasty) is directed to the surgical division of the aryepiglottic folds and the removal of excess mucosa and cartilage that are prolapsing into the airway. Those with severe laryngomalacia to require supraglottoplasty will have minimal complications and good outcomes if multiple medical co-morbidities are not present. Those with multiple medical co-morbidities could be offered supraglottoplasty as the first intervention but counseled that tracheostomy may be required 5.
Figure 1. Larynx
Figure 2. Vocal cords
Figure 3. Congenital laryngomalacia
Go to the hospital immediately if your baby:
- Stops breathing for more than 10 seconds
- Turns blue around the lips while breathing noisily
- Pulls in the neck or chest without relief after being repositioned or awakened
See your child’s doctor about:
- Child has difficulty keeping food down and constantly spits it up
- Child is losing weight or is not gaining weight
- Child begins to feed less and tires easily in the middle of feeding
- Child begins to choke on food
- Child struggles between eating and breathing
As a rule of thumb, all babies with suspected laryngomalacia should be evaluated by a pediatric otolaryngologist. In most cases, pediatric otolaryngologists perform in-office flexible laryngoscopy to confirm the diagnosis and rule out other pathology, including cysts or neurologic conditions. Patients with more severe presentations (failure to thrive, retractions, aspiration, comorbidities) may be best served by an evaluation in Center for Pediatric Airway Disorders, staffed by airway surgeons and pulmonologist, gastroenterologist, and speech therapist.
Laryngomalacia severity
Mild Laryngomalacia
Infants in this category have non-complicated laryngomalacia with typical noisy breathing when breathing in without significant airway obstructive events, feeding issues or other symptoms associated with laryngomalacia. These infants have noisy breathing that is annoying to the caregivers but does not cause other healthcare problems. These patients will usually outgrow the stridor by 12-18 months of age.
Even though your child may have mild laryngomalacia, it is still important to watch for signs or symptoms of it worsening.
Moderate Laryngomalacia
Infants in this category have the following symptoms:
- Noisy breathing when breathing in
- Vomiting or spitting up
- Airway obstruction (from floppy voice box tissue)
- Feeding difficulties without poor weight gain
- History of airway symptoms severe enough to warrant multiple visits to an emergency department or hospital
- Gastroesophageal reflux disease (GERD). These patients also will typically outgrow the stridor by 12-18 months of age but may require treatment for GERD.
Even though your child may have moderate laryngomalacia, it is still important to watch for signs and symptoms of it worsening.
Severe Laryngomalacia
Patients in this category often require surgery for treatment and to lessen the degree of symptoms. Your doctor may recommend surgery if your child has any of the following symptoms:
- Life-threatening apnea
- Significant blue spells
- Failure to thrive with feeding difficulty
- Significant chest wall and neck retractions with breathing
- Requires oxygen to breathe
- Heart or lung problems as a result of chronic oxygen depravation
Laryngomalacia sound
Laryngomalacia can result in stridor — a high-pitched sound that is heard when your child inhales. Laryngomalacia is sometimes referred to as congenital laryngeal stridor and is the most common cause of noisy breathing in infants.
How common is laryngomalacia?
It is estimated that 70% of infant stridor is attributable to laryngomalacia, although that number is probably an underestimate given that many patients are probably not referred for evaluation of mild symptoms 7.
How to get laryngomalacia to heal in babies?
Many infants with laryngomalacia are able to eat and grow normally, and the condition will resolve without surgery by the time they are around 20 months old. However, a small percentage of babies do struggle with breathing, eating and weight again, and their symptoms require immediate treatment.
Laryngomalacia causes
The exact cause of laryngomalacia is not known. Relaxation or a lack of muscle tone in the upper airway may be a factor. The malformation is usually present at birth or appears within the first month of life. Gastroesophageal reflux may contribute to the severity of the symptoms. The noisy breathing is often worse when the infant is on his back or when crying.
Various theories regarding laryngomalacia cause have been proposed, including anatomic abnormalities, impaired neuromuscular coordination or low muscle tone of laryngeal structures, pharyngo-laryngeal reflux (when stomach acid travels up through the esophagus and reaches the larynx), and abnormalities in the amount of air displaced when breathing (tidal volume) 8.
The development of symptoms of laryngomalacia may result from variable combinations of these factors in each infant. Regardless of the underlying causes(s), the symptoms are due to the cartilage being “floppy,” and prolapsing (collapsing) over the larynx when inhaling. This in turn causes the noises generated when breathing 9.
Laryngomalacia inheritance
Laryngomalacia may be inherited in some instances. Only a few cases of familial laryngomalacia (occurring in more than one family member) have been described in the literature 10. In some of these cases, autosomal dominant inheritance has been suggested 10.
Laryngomalacia has also been reported as being associated with various syndromes 10. In cases where these specific syndromes are inherited, a predisposition to being born with laryngomalacia may be present. However, even within a family, not all people affected with one of these syndromes will have the exact same signs and symptoms (including laryngomalacia). Syndromes that have been associated with laryngomalacia include diastrophic dysplasia, alopecia universalis congenital, XY gonadal dysgenesis, Costello syndrome, DiGeorge syndrome, and acrocallosal syndrome 10. The inheritance pattern depends upon the specific syndrome present.
Laryngomalacia symptoms
If your child is born with laryngomalacia, symptoms may be present at birth, and can become more obvious within the first few weeks of life. The primary symptom is noisy breathing, known as stridor. This is a wheezing sound your baby makes when inhaling. It is often worse when your baby is on his or her back, because the floppy tissues can fall over the airway opening more easily in this position. Stridor may also get worse before it improves.
It is not uncommon for the noisy breathing to get worse before it improves, usually around 4 to 8 months of age. Most children outgrow laryngomalacia by 18 to 20 months of age.
Laryngomalacia symptoms include:
- Noisy breathing (stridor) — An audible wheeze when your baby inhales (breathes in). It is often worse when the baby is agitated, feeding, crying or sleeping on his back.
- High pitched sound
- Difficulty feeding
- Poor weight gain
- Choking while feeding
- Apnea (breathing stoppage)
- Pulling in neck and chest with each breath
- Cyanosis (turning blue)
- Gastroesophageal reflux (spitting, vomiting and regurgitation)
- Aspiration (inhalation of food into the lungs)
Laryngomalacia diagnosis
A diagnosis of laryngomalacia is often suspected based on the presence of characteristic signs and symptoms. Additional testing can then be ordered to confirm the diagnosis, evaluate the severity of the condition, and rule out other disorders that can be associated with similar features.
Your doctor will ask you some questions about your baby’s health problems and may recommend a test called a nasopharyngolaryngoscopy (flexible fiberoptic laryngoscopy) to further evaluate your baby’s condition. Nasopharyngolaryngoscopy test is required to confirm a diagnosis.
During this test, done in your doctor’s office, a tiny camera that looks like a strand of spaghetti with a light on the end is passed through your baby’s nostril and into the lower part of the throat where the larynx is. This allows your doctor to see your baby’s voice box. The doctor looks at the position of the tissue above the voice box to determine if it is floppy. At the same time, they will look for any other throat / voice box problems that may contribute to the noisy breathing.
If laryngomalacia is diagnosed, the doctor may want to do other diagnostic tests to evaluate the extent of your child’s problems and to see whether the lower airway is affected. These tests may include:
- X-ray of the neck. Some children may have an additional problem that may contribute to the noisy breathing. The X-rays can screen for other possible causes of noisy breathing in the upper airway, windpipe, chest and lungs. Your doctor may recommend more studies if these tests are abnormal.
- Airway fluoroscopy
- Microlaryngoscopy and bronchoscopy. This test is done in the operating room under general anesthesia by the ENT surgeon. The doctor looks at the voice box and windpipe with telescopes. Your doctor may recommend this test if the X-ray test shows something abnormal or if your doctor suspects additional airway problems.
- Esophagogastroduodenoscopy (EGD) and pH probe. An esophagogastroduodenoscopy is a diagnostic test done in the operating room under general anesthesia. The gastroenterologist looks at your child’s esophagus and stomach with a lighted tube. During an esophagogastroduodenoscopy, the doctor looks for signs of chronic inflammation from acid irritation that can occur in the stomach or the esophagus. Your doctor may recommend this if the pH probe is significantly abnormal or there is strong suspicion of significant GERD based on history and clinical examination.
- The Gastric Reflux Test (Multichannel Intraluminal Impedance Test)
- There is a strong link between GERD and laryngomalacia. All babies reflux, but children with laryngomalacia may have more than other babies. Acid reflux, if it reaches the upper portion of the swallowing tube (esophagus) and voice box region, can cause additional swelling of the floppy tissue seen in laryngomalacia. The Gastric Reflux Test (Multichannel Intraluminal Impedance Test) is performed to detect and record the number of times stomach contents come back into the esophagus and the relation of these episodes to symptoms (for example, when a child cries, arches, coughs, gags, vomits, has chest pain). It also determines if the contents are acidic or not and how long they stay in the esophagus. A thin light wire with an acid sensor as well as six to seven metal sensors is inserted through the nose into the lower part of the esophagus. The impedance probe is connected to a recorder box that the patient will carry with them for the duration of the study. Child life staff may be a useful resource to aid the patient and staff during placement of the probe, as this can be an uncomfortable procedure while awake.
- Functional endoscopic evaluation of the swallow (FEES)
- CT scan (CAT) with 3‐D reconstruction
- Echocardiogram
Laryngomalacia treatment
In 90 percent of cases, laryngomalacia resolves without treatment by the time your child is 18 to 24 months old. However, if the laryngomalacia is severe, your child’s treatment may include medication or surgery called supraglottoplasty. This surgery involves cutting the folds of tissue to open the supraglottic airway (the area above the vocal chords). During supraglottoplasty procedure, your child will be under general anesthesia. After surgery, your child will be admitted to the hospital for a 24-hour observation period.
Medication
Your child’s doctor may prescribe an anti-reflux medication to help manage the gastroesophageal reflux (GERD). This is important because your child’s chronic neck and chest retractions from the laryngomalacia can worsen reflux. Also, the acid reflux can cause swelling above the vocal cords and worsen the noisy breathing.
Laryngomalacia surgery
A surgery called supraglottoplasty is the treatment of choice if your child’s condition is severe. Symptoms that signal the need for laryngomalacia surgery include:
- Life-threatening apneas (stoppages of breathing)
- Significant blue spells
- Failure to gain weight with feeding
- Significant chest and neck retractions
- Need for extra oxygen to breathe
- Heart or lung issues related to your child’s inability to get enough oxygen
This surgery may not completely eliminate the noisy breathing but it should help to:
- Reduce the severity of the symptoms
- Lessen the apneas (breathing stoppages)
- Reduce the extra oxygen requirements
- Improve swallowing
- Help your child gain weight
The safety of your child’s swallow should be reevaluated after the surgical procedure.
Supraglottoplasty
Supraglottoplasty is a microscopic surgical procedure to alter malformed structures of the upper larynx. This allows a child with certain conditions (such as severe laryngomalacia) to breathe more easily.
Supraglottoplasty procedure is done through the mouth. A laser or surgical instruments may be used to conservatively remove obstructive tissue in the upper larynx. Supraglottoplasty surgery generally takes about one hour, and the child may or may not require a breathing tube overnight following the procedure. Photos of the airway will be taken to document the exam.
References- [Research progress of laryngomalacia in children]. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2017 Jan 20;31(2):162-166. doi: 10.13201/j.issn.1001-1781.2017.02.023. https://www.ncbi.nlm.nih.gov/pubmed/29871214
- Zoumalan R, Maddalozzo J, Holinger LD. Etiology of stridor in infants. Ann. Otol. Rhinol. Laryngol. 2007 May;116(5):329-34
- Case 46 – A 6-month-old with laryngomalacia and stridor in sleep. Pediatric Sleep Pearls 2017, Pages 146-150. https://doi.org/10.1016/B978-0-323-39277-8.00046-4
- Gaudreau P, Fordham MT, Dong T, et al. Visualization of the Supraglottis in Laryngomalacia With 3-Dimensional Pediatric Endoscopy. JAMA Otolaryngol Head Neck Surg. 2016;142(3):258–262. doi:10.1001/jamaoto.2015.3370
- Laryngomalacia: factors that influence disease severity and outcomes of management. Curr Opin Otolaryngol Head Neck Surg. 2010 Dec;18(6):564-70. doi: 10.1097/MOO.0b013e3283405e48 https://www.ncbi.nlm.nih.gov/pubmed/20962644
- Laryngomalacia. Semin Pediatr Surg. 2016 Jun;25(3):119-22. doi: 10.1053/j.sempedsurg.2016.02.004. Epub 2016 Feb 18. https://doi.org/10.1053/j.sempedsurg.2016.02.004
- Relative imbalance as etiology of laryngomalacia – A new theory. Med Hypotheses. 2017 Jan;98:38-41. doi: 10.1016/j.mehy.2016.11.004. Epub 2016 Nov 23. https://doi.org/10.1016/j.mehy.2016.11.004
- Rathi A, Rathi S.. Relative imbalance as etiology of laryngomalacia – A new theory.. Med Hypotheses. January, 2017; 98:38-41. https://www.ncbi.nlm.nih.gov/pubmed/28012601
- Ayari S, Aubertin G, Girschig H, Van Den Abbeele T, Mondain M. Pathophysiology and diagnostic approach to laryngomalacia in infants. Eur Ann Otorhinolaryngol Head Neck Dis. October, 2012; 129(5):257-263. https://www.ncbi.nlm.nih.gov/pubmed/23078980
- Chen JL, Messner AH, Chang KW. Familial laryngomalacia in two siblings with syndromic features. Int J Pediatr Otorhinolaryngol. September 2006; 70(9):1651-1655