What are causes of lump in armpit
A lump in armpit is a swelling or bump under the arm. A lump in the armpit can have many causes. These include swollen lymph nodes, infections, or cysts. Lymph nodes (or lymph glands) are part of the body’s immune system. Lymph nodes filter harmful substances like bacteria and cancer cells from your body, and help fight infections. Lymph nodes also play an important role in cancer diagnosis, treatment and prognosis. Swollen lymph glands are a sign your body is fighting an infection. They usually get better by themselves in 2 to 3 weeks. Rarely lump in the armpit is caused by anything more serious, like cancer of the blood system (leukemia) or lymph system (lymphoma). However, see your doctor if you have an unexplained armpit lump. Do not try to diagnose lumps by yourself. An armpit lump in a woman may be a sign of breast cancer, and it should be checked by a health care provider right away.
Reasons lymph nodes in the armpit area may be enlarged are:
- Arm or breast infection
- Some bodywide infections, such as mono, AIDS, or herpes
- Cancers, such as lymphomas or breast cancer
Cysts or abscesses under the skin may also produce large, painful lumps in the armpit. These may be caused by shaving or use of antiperspirants (not deodorants). This is most often seen in teens just beginning to shave.
Other causes of armpit lumps may include:
- Cat scratch disease
- Lipomas (harmless fatty growths)
- Use of certain medicines or vaccinations
Hidradenitis suppurativa is rare, long-term skin condition that features small, painful lumps under the skin in the armpit. Hidradenitis suppurativa typically develop where the skin rubs together, such as the armpits, the groin, between the buttocks and under the breasts. The lumps may break open and smell or cause tunnels under the skin.
Signs and symptoms of hidradenitis suppurativa include:
- Blackheads. Small pitted areas of skin containing blackheads — often appearing in pairs or a “double-barreled” pattern — are a common feature.
- Red, tender bumps. These bumps often enlarge, break open and drain pus. The drainage may have an odor. Itching and burning may accompany the bumps. They usually appear in areas where skin rubs against skin.
- Painful, pea-sized lumps. These hard lumps, which develop under the skin, may persist for years, enlarge and become inflamed.
- Tunnels. Over time, tracts connecting the lumps may form under the skin. These wounds heal very slowly, if at all, and can leak pus.
Hidradenitis suppurativa tends to start after puberty. It can persist for many years and worsen over time, with serious effects on your daily life and emotional well-being. Early diagnosis and treatment can help manage the symptoms, keep new lumps from forming and prevent complications, such as scarring or depression.
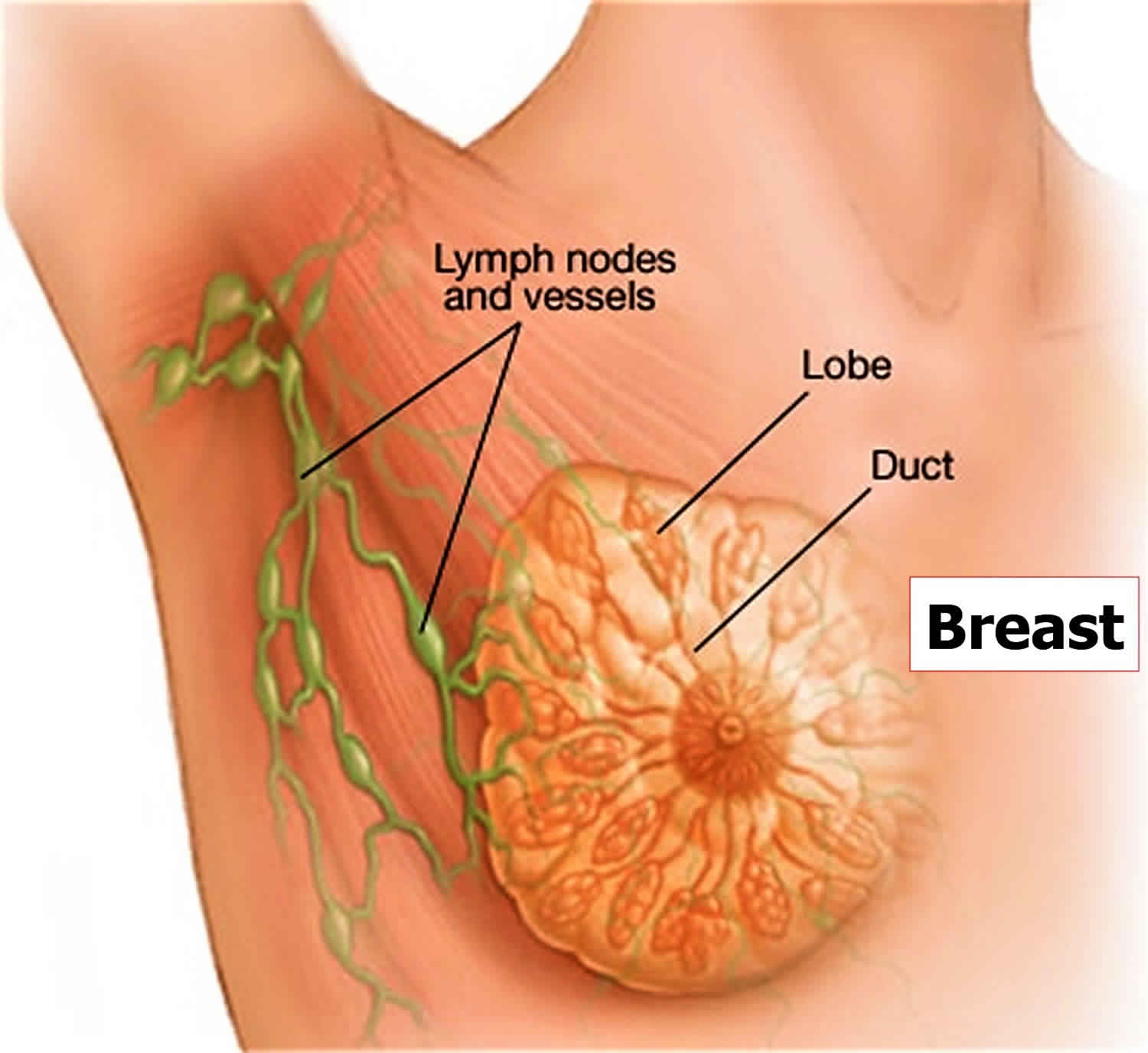
In women, enlarging painless lumps in the armpit could mean breast cancer. After skin cancer, breast cancer is the most common cancer diagnosed in women in the United States. Breast cancer can occur in both men and women, but it’s far more common in women.
Signs and symptoms of breast cancer may include:
- A breast lump or thickening that feels different from the surrounding tissue
- Change in the size, shape or appearance of a breast
- Changes to the skin over the breast, such as dimpling
- A newly inverted nipple
- Peeling, scaling, crusting or flaking of the pigmented area of skin surrounding the nipple (areola) or breast skin
- Redness or pitting of the skin over your breast, like the skin of an orange
Given the many causes of lump in the armpit, it’s important you see your health care provider to determine the cause.
An armpit lump in a woman may be a sign of breast cancer, and it should be checked by your healthcare provider right away.
See your doctor if you have an unexplained armpit lump. Do not try to diagnose lumps by yourself.
- your swollen glands are getting bigger or they haven’t gone down within 3 weeks
- the armpit lump(s) feel hard or don’t move when you press them
- you’re having night sweats or have a very high temperature (you feel hot and shivery) for more than 3 or 4 days
- you have swollen glands and no other signs of illness or infection
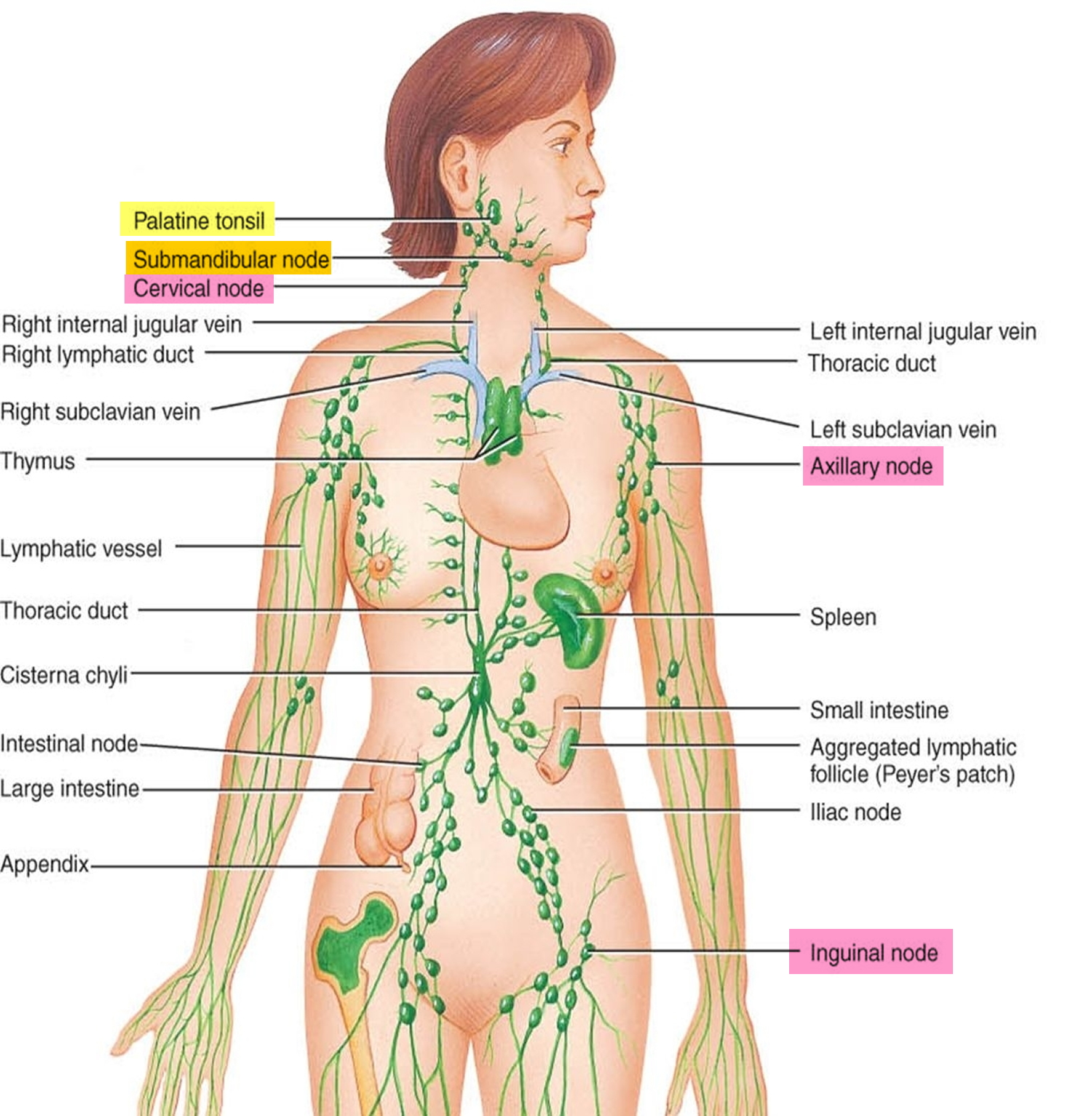
What are lymph nodes?
Lymph nodes are small lumps of tissue that contain white blood cells, which fight infection. They filter lymph fluid, which is composed of fluid and waste products from your body tissues. Lymph nodes also help activate your immune system if you have an infection.
Where are lymph nodes located?
Lymph nodes are located throughout your body, including your neck, armpits, groin, around your gut, and between your lungs. Lymph nodes drain lymph fluid from nearby organs or areas of your body.
How lymph nodes filter lymph fluid
Lymph fluid is carried to your lymph nodes by lymphatic vessels. Your lymph nodes filter out harmful substances and waste products. They also contain immune cells that destroy cancer cells and bacteria.
The filtered fluid is then returned to your blood circulation.
If you have an infection or cancer, a lymph node may become swollen. If you are concerned about your lymph nodes, speak to your doctor.
Lymph nodes and cancer
Sometimes cancer can start in the lymph nodes (such as in lymphoma), but cancer can also spread from one part of the body to another through lymph nodes.
If a person has cancer, doctors examine lymph nodes carefully to see whether or not they are affected by cancer. They can do this by:
- feeling all the nodes in the body
- getting scans, for example a CT scan
- removing nodes near the cancer, then examining them under a microscope
- taking a biopsy of the lymph nodes near the cancer, then examining them under a microscope.
This is done to see if the cancer has spread or not. This helps doctors work out the best treatment for the cancer.
Figure 1. Locations of major lymph nodes
Figure 2. Breast and armpit lymph nodes
Lump in armpit causes
Lumps in the armpit may have many causes.
Lymph nodes act as filters that can catch germs or cancerous tumor cells. When they do, lymph nodes increase in size and are easily felt. Reasons lymph nodes in the armpit area may be enlarged are:
- Arm or breast infection
- Some bodywide infections, such as mono, AIDS, or herpes
- Cancers, such as lymphomas or breast cancer
Cysts or abscesses under the skin may also produce large, painful lumps in the armpit. These may be caused by shaving or use of antiperspirants (not deodorants). This is most often seen in teens just beginning to shave.
Other causes of armpit lumps may include:
- Cat scratch disease
- Lipomas (harmless fatty growths)
- Use of certain medicines or vaccinations
Painful lump in armpit
Hidradenitis suppurativa also known as acne inversa, is a chronic painful inflammatory disease of the apocrine sweat glands in your armpits, groin, under the breasts and/or anogenital regions of the body, although other sites may be involved 1. The sweat glands become clogged due to a variety of reasons, leading to enlargement (dilatation) of the ducts behind them. This dilatation predisposes the area to inflammation and infection by a variety of bacteria. Those with hidradenitis suppurativa typically have multiple large, recurrent boil-like nodules (red bumps) and abscesses on the buttocks, breasts, groin, and armpits. The bumps gradually get larger and drain pus. After multiple bouts of this cycle of plugging, enlargement, drainage and difficult-to-heal open wounds (sinuses), there may be scarring.
Hidradenitis suppurativa onset is generally after puberty and most common between 20-24 years of age. Onset before puberty is uncommon, but does correlate with a greater severity later in life and a positive family history 2.
Potential complications of hidradenitis suppurativa include keloid scars, fistulas, lymphedema, squamous cell carcinoma (SCC), anemia of chronic disease, amyloid of the skin and/or kidney with the development of nephrotic syndrome, scarring, and limb contractures 3. Cancer, in particular squamous cell carcinoma (SCC) may rarely occur 4. Patients may die. The typical patient is one with long term, severe disease who develops a very painful nodule or lesion, often in the perianal or perineal area.
Hidradenitis suppurativa also has significant psychological impact and many patients suffer from impairment of body image, depression and anxiety.
While there is no cure for hidradenitis suppurativa, you can work with your doctor to treat existing lesions and prevent new ones.
Hidradenitis suppurativa treatment:
- Weight loss
- Smoking cessation
- Topical or oral antibiotics
- Intralesional steroids
- Low-dose prednisone
- 1064 nm nd:YAG Laser
- Laser hair removal
- Adalimumab
- Diabetic agents (e.g. metformin)
- Surgery
Figure 3. Hidradenitis suppurativa armpit
Who’s at risk of hidradenitis suppurativa?
Hidradenitis suppurativa usually starts soon after puberty and continues into adult life. Hidradenitis suppurativa is most active between the ages of 20 and 40 years. Hidradenitis suppurativa is three times more common in females than in males and and in women, it can resolve at menopause. Hidradenitis suppurativa is also common in African Americans. Hair removal from shaving or using depilatories, deodorants, and irritation from anything rubbing against the affected area can worsen the condition. Hidradenitis suppurativa is often associated with smoking, obesity, and increased hormones. Additionally, it often runs in families.
Risk factors for developing hidradenitis suppurativa include:
- Other family members with hidradenitis suppurativa
- Obesity and insulin resistance/metabolic syndrome
- Cigarette smoking
- Follicular occlusion disorders: acne conglobata, dissecting cellulitis, pilonidal sinus
- Inflammatory bowel disease (Crohn disease)
- Diabetes
- Polycystic Ovarian Syndrome (PCOS)
- Spondyloarthrothopies
- Heart Disease
- Rare autoinflammatory syndromes associated with abnormalities of PSTPIP1 gene. PAPA syndrome (pyogenic arthritis, pyoderma gangrenosum and acne), PASH syndrome (pyoderma gangrenosum, acne, suppurative hidradenitis) and PAPASH syndrome (pyogenic arthritis, pyoderma gangrenosum, acne, suppurative hidradenitis).
Hidradenitis suppurativa stages
The severity and extent of hidradenitis suppurativa should be recorded at assessment and when determining the impact of a treatment. Two scoring systems are in common use: Hurley Stages and Sartorius Hidradenitis Suppurativa Score.
The Hurley system describes three distinct clinical stages 5:
- Stage 1: Solitary or multiple, isolated abscess formation without scarring or sinus tracts
- Stage 2: Recurrent abscesses, single or multiple widely separated lesions, with sinus tract formation
- Stage 3: Diffuse or broad involvement, with multiple interconnected sinus tracts and abscesses.
- Severe hidradenitis (Hurley Stage 3) has been associated with:
- Male gender
- Armpit and perianal involvement
- Obesity
- Smoking
- Disease duration.
- Severe hidradenitis (Hurley Stage 3) has been associated with:
Hurley Staging allows medical professionals to assign a severity level to hidradenitis suppurativa, but it does not account for disease activity, measure pain, or quality of life impact.
Sartorius Hidradenitis Suppurativa Score
The Sartorius Hidradenitis Suppurativa Score is made by counting involved regions, nodules and sinus tracts 6:
- Anatomic region involved (axilla, groin, genital, gluteal, or other inflammatory region left and/or right): 3 points per region involved
- Number and scores of lesions (abscesses, nodules, fistulas, scars): 2 points for each nodule, 4 points for each fistula, 1 point for each scar, 1 point each for “other”
- Longest distance between 2 relevant lesions (ie, nodules and fistulas, in each region, or size if only 1 lesion): Less than 5 cm, 2 points; less than 10 cm, 4 points; more than 10 cm, 8 points
- Lesions clearly separated by normal skin in each region: If yes, 0 points; if no, 6 points.
Hidradenitis suppurativa symptoms
Hidradenitis can affect a single or multiple areas in the armpits, neck, submammary area, and inner thighs. Anogenital involvement most commonly affects the groin, mons pubis, vulva (in females), sides of the scrotum (in males), perineum, buttocks and perianal folds.
Signs of hidradenitis suppurativa include:
- Open and closed comedones
- Painful firm papules, larger nodules and pleated ridges
- Pustules, fluctuant pseudocysts and abscesses
- Pyogenic granulomas
- Draining sinuses linking inflammatory lesions
- Hypertrophic and atrophic scars.
Many patients with hidradenitis suppurativa also suffer from other skin disorders, including acne, hirsutism and psoriasis.
The severity and extent of hidradenitis suppurativa is recorded at assessment and when determining the impact of a treatment.
Hidradenitis suppurativa causes
The cause of hidradenitis suppurativa is unknown. It is thought that there is an exaggerated inflammatory response to the presence of bacteria trapped in obstructed hair follicles in the skin. In some cases there does seem to be a genetic component. Bacteria seem to play some role, which is why antibiotics may be used in treatment. However, bacteria are not the primary cause of hidradenitis suppurativa. Other factors such as obesity, smoking and stress also play a role.
Contributing factors include:
- Friction from clothing and body folds
- Aberrant immune response to commensal bacteria
- Abnormal cutaneous or follicular microbiome
- Follicular occlusion
- Release of pro-inflammatory cytokines
- Inflammation causing rupture of the follicular wall and destroying apocrine glands and ducts
- Secondary bacterial infection
- Certain drugs.
Follicular Occlusion
Hidradenitis suppurativa was originally thought to be caused by a defect of the sweat gland, but this view has changed and it is now widely accepted to be a problem with the hair follicle. Build-up of keratin (a type of protein) within the hair follicle eventually plugs the hair follicle, causing further build up, and eventually the hair follicle ruptures and releases this material into the surrounding skin resulting in an intense inflammatory response 7.
Bacteria
Sometimes bacteria can be isolated from hidradenitis suppurativa lesions, while other times cultures from hidradenitis suppurativa lesions are sterile (no bacteria found) 8. Those affected by hidradenitis suppurativa frequently experience the characteristic symptoms of an infection, such as pain, tenderness, warmth, and purulent drainage. It may be reasonable to assume that since symptoms tend to improve after antibiotics, that hidradenitis suppurativa is caused primarily by bacteria, however this is not the case.
Biofilms
Recently, hidradenitis suppurativa has been described as a biofilm disease. When numerous bacteria secrete a sticky material known as a polysaccharide matrix and bind to a surface they now exist in what is known as a biofilm. When bacteria exist in a biofilm they become highly resistant to antibiotics. A recent study looking at biopsy samples (pieces of skin) from patients with hidradenitis suppurativa, demonstrated that biofilms were associated with chronic hidradenitis suppurativa 9. Although, biofilms likely don’t form primarily, this may be the reason that hidradenitis suppurativa become very resistant to medical management as it becomes more severe.
Aberrant Immunity
Several markers of inflammation exist in the blood and skin and can be used to assess the inflammatory state of the body. Abnormal levels of these markers have been implicated in the development of several diseases and similarly found to be abnormal in hidradenitis suppurativa. Additional research is needed to determine the implications of these abnormal levels, but these findings have led to the use of biologic medications, such as adalimumab and infliximab for the treatment of hidradenitis suppurativa.
Diet
Nutrition is an understudied and notoriously difficult topic to research in medicine. The majority of evidence is based on individual experience with few published articles in the literature, but the impact of diet on hidradenitis suppurativa infiltrates through social media and online message boards with reports of improvement that ranges from minimal or no effect to complete resolution. In one survey study involving 47 patients who followed dairy free diets, no patients experienced disease progression and 83% improved to various degrees 10. In another study, 12 subjects underwent surgical excision followed by diet modification with no wheat or brewers yeast consumption with immediate disease stabilization during a 12 month period of follow up 11.
Additional research is needed in order to allow for comprehensive diet counseling. Some patients have reported improvement after exclusion of nightshades, simple carbohydrates, and dairy, but the impact of diet modification appears to be highly individual and should be discussed with your physician or nutritionist. Dieticians can provide individualized meal plans to make sure that you are getting all of the required nutrients.
Other Factors
Several other factors have been implicated in the development of hidradenitis suppurativa. Smoking is more common among people with hidradenitis suppurativa than among the general population, and the components of smoke are known to promote hyperkeratosis (causing follicular occlusion) and also increases inflammation potentially worsening hidradenitis suppurativa 12. Mechanical factors caused by skin to skin contact and obesity may also contribute to the overall inflammatory state of hidradenitis suppurativa and the development or progression of hidradenitis suppurativa.
Lastly, hormones are potentially implicated in hidradenitis suppurativa. It is known that more women are affected by hidradenitis suppurativa than men and therefore a hormonal component has been hypothesized. Androgens, a type of hormone, can increase proliferation of the keratinocytes (skin cells), however the hormonal profile of patients with hidradenitis suppurativa is usually found to be normal 12.
With numerous factors implicated in the development of hidradenitis suppurativa, it is clear that additional research is needed and the trigger for one patient may not be consistent across the entire population.
Hidradenitis suppurativa treatment
General measures
Friction and moisture in the affected areas should be reduced as much as possible. Weight loss can greatly improve the condition if the patient is overweight 13. Topical clindamycin may be helpful (or benzoyl peroxide 10% wash). Bleach baths and Hibiclens may have some benefit. Smokers should stop. Bacterial cultures may occasionally be done to rule out other causes or secondary infection.
- Weight loss; follow an anti-inflammatory, low-sugar, low-grain, low-dairy diet (mainly plants)
- Smoking cessation: this can lead to improvement within a few months
- Loose fitting clothing
- Daily unfragranced antiperspirants
- If prone to secondary infection, wash with antiseptics or take bleach baths
- Apply hydrogen peroxide solution or medical grade honey to reduce malodour
- Use peeling agents such as resorcinol 15% cream to de-roof nodules
- Apply simple dressings to draining sinuses
- Analgesics, such as paracetamol (acetaminophen), for pain control
- Seek help to manage anxiety and depression.
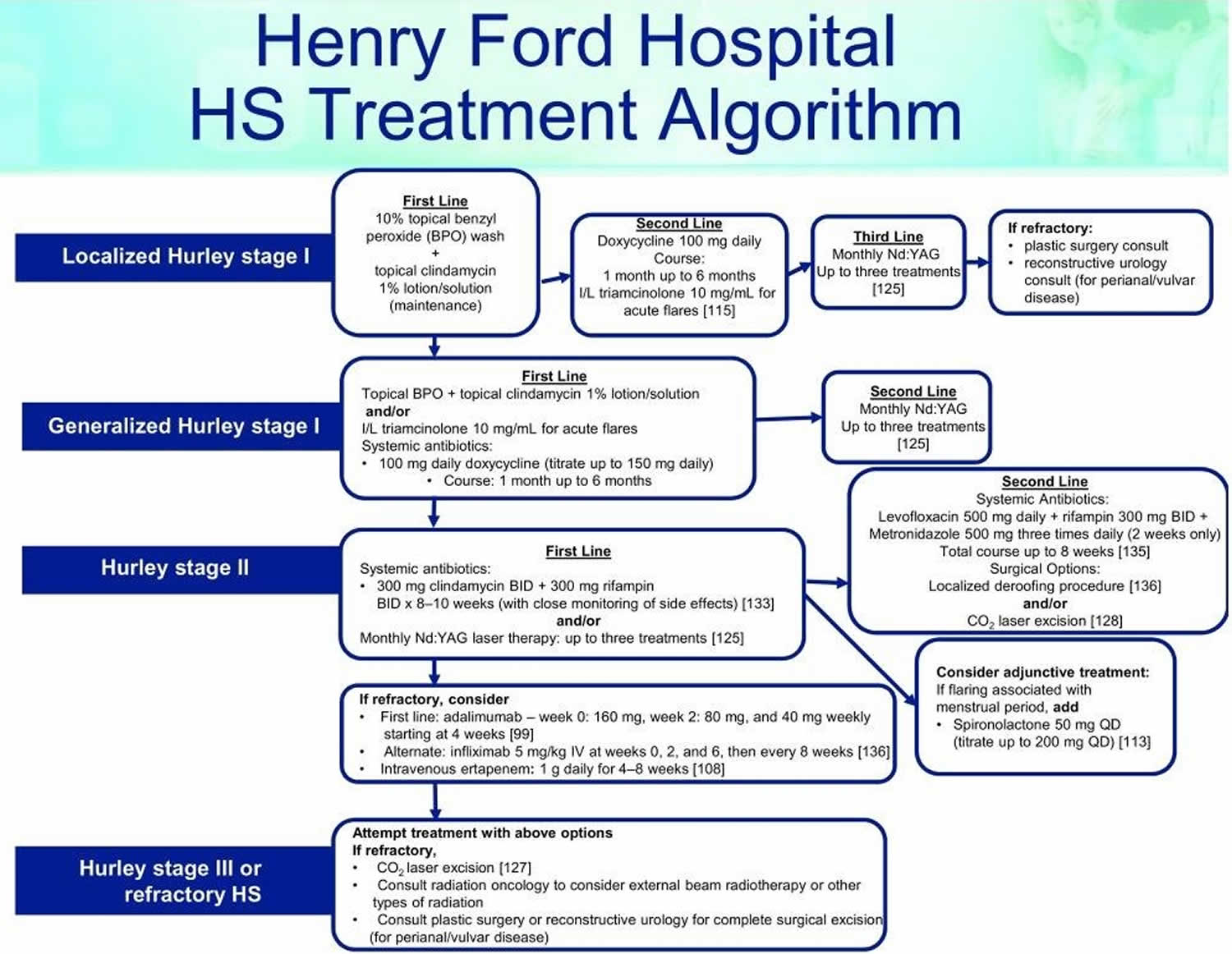
Figure 2. Hidradenitis suppurativa treatment algorithm
Footnote: This treatment algorithm is used in the Henry Ford Dermatology Clinic, which provides care to more than 1,000 patients with HS. The algorithm is based on a combination of evidence-based research and provider experience.
Abbreivations: HS = hidradenitis suppurativa; BID = bis in die (twice daily); I/L = intralesional; IV = intravenously; Nd:YAG = neodymium-doped yttrium aluminum garnet; QD = quaque die (once daily)
[Source 1]Medical management of hidradenitis suppurativa
Medical management of hidradenitis suppurativa is difficult. Treatment is required long term. Effective options are listed below.
Antibiotics
- Topical clindamycin, with benzoyl peroxide to reduce bacterial resistance
- Short course of oral antibiotics for acute staphylococcal abscesses, eg flucloxacillin
- Oral antibiotics can be very helpful. Prolonged courses (minimum 3 months) of tetracycline, metronidazole, trimethoprim + sulphamethoxazole, fluoroquinolones, ertapenem or dapsone for their anti-inflammatory action.
- Doxycycline 100 mg oral twice daily ongoing can be beneficial.
- Dapsone, 5-200 mg/day, may be helpful.
- 6–12 week courses of the combination of clindamycin (or doxycycline) and rifampicin for severe disease.
- Several experts recommend treatment for more severe, unstable hidradenitis suppurativa, with the combination of clindamycin 300 mg and rifampicin 300 mg both twice daily for 10 weeks. On the plus side, rifampicin acts against Clostridium difficule infections, decreasing the risk of colitis. On the down side, rifampicin can inactivate birth control pills. Also, it can turn bodily secretions orange, e.g. tears, sweat and urine.
- Other options include amoxicillin with clavulanic acid or fluoroquinolones (e.g., ciprofloxacin). Trimethoprim with sulfamethoxazole may also be beneficial. One study showed Staphylococcus epidermidis, Proteus mirabilis, and Staphylococcus aureus to be the most common isolates 14.
Antiandrogens
- Long-term oral contraceptive pill; antiandrogenic progesterones drospirenone or cyproterone acetate may be more effective than standard combined pills. These are more suitable than progesterone-only pills or devices.
- Spironolactone. Some women experience a premenstrual flare. For them, antiandrogen therapy (e.g., spironolactone) may be helpful.
- Finasteride has been used in children with hidradenitis suppurativa with success 15, 16. Three female patients, ages six, seven, and 15 who had failed standard therapy including isotretinoin, were treated with finasteride 1.25-10 mg/day for up to six years. Adjunctive birth control pills were given if the patient was a menstruating female. Treatment resulted in decreased frequency and severity of disease flares with no significant adverse effects.
- Response takes 6 months or longer.
Immunomodulatory treatments for severe disease
- Intralesional corticosteroids into nodules (e.g., Triamcinolone 5-10 mg/mL) can give the patient great relief. In one study utilizing triamcinolone 10 mg/mL 17, pain was reduced after 1 day and signs of inflammation after 7 days.
- Systemic corticosteroids short-term for flares. In one report 18, 13 patients were treated initially with prednisone 10 mg/day (ultimate dose varied from 5-15 mg/day). This was given in addition to existing therapy when that was not sufficient for control (e.g., acitretin, adalimumab, dapsone, clindamycin, doxycycline). All patients received calcium (1200 mg/day) and vitamin D (1000 IU/day) and monthly glucose monitoring. Overall, 11/13 patients showed a clinical response with the addition of low-dose prednisone. Side effects were minor and included hyperglycemia, sleep disturbance, and mild psychomotor agitation.
- Methotrexate, cyclosporin, and azathioprine. A few case reports highlight the benefit of cyclosporin. One patient did well on long-term cyclosporin 5 mg/kg/day, then 3 mg/kg/day 19.
- If oral and topical antibiotics plus general measures are not sufficient, a biologic agent is often added. TNF-α inhibitors adalimumab and infliximab, used in higher dose than required for psoriasis, are the most successful treatments to date. Note that paradoxically, they may sometimes induce new-onset hidradenitis suppurativa
- Other biologics are under investigation, such as the IL-1β antagonist, canakinumab
Adalimumab
Adalimumab is FDA-approved for moderate to severe hidradenitis suppurativa that is resistant to conventional therapies, but the dosing is weekly (for psoriasis, it is every other week). Adalimumab for hidradenitis suppurativa is given as a subcutaneous injection as follows: 160 mg day 1; 80 mg day 15; 40 mg day 29; and then weekly ongoing. Combining adalimumab with oral antibiotics, e.g., doxycycline increases efficacy. Interestingly, the incidence of serious infections is not higher than placebo.
In one randomized double blind controlled trial, adalimumab weekly was superior to both adalimumab every other week and placebo 20.
Other biologic agents
In comparing all the biologic agents, one review put the percent responders at 89% infliximab, 79% adalimumab, and 56% for etanercept 21. Ustekinumab has also been used in a few patients. Infliximab seems to be most effective but in one study 22% experienced serious adverse events, the most common being infusion reactions, and one patient died of pneumococcal sepsis. In one study 22 of 11 patients with severe hidradenitis suppurativa unresponsive to more than three prior therapies, infliximab 5 mg/kg every four weeks was given. Nine of the 11 patients remain well-controlled on this regimen. Secukinumab has been helpful anecdotally.
Canakinumab is a human IgGk monoclonal antibody targeting IL-1B. It was beneficial in two patients with severe hidradenitis suppurativa 23.
Other medical treatments
- Metformin in patients with insulin resistance. Metformin 24 and more recently liragutide 25 have shown benefit in difficult to control hidradenitis suppurativa. In overweight or obese patients with recalcitrant disease, these agents may be beneficial.
- Acitretin (unsuitable for females of childbearing potential). Acitretin in one study of 12 patients did incredibly well 26. The average dose was 0.67 mg/kg/day. Nine patients achieved marked or complete remission after one course. The improvement generally started within two months and further improvement was achieved within the first six months of therapy. Isotretinoin has not shown analogous results.
- Isotretinoin — effective for acne but appears unhelpful for most cases of hidradenitis suppurativa
- Colchicine
- Anakinra (IL-1 receptor antagonist) showed benefit in a study of five patients 27. Another study randomized 20 patients to receive either anakinra or placebo for 12 weeks. The disease activity score was decreased at the end of treatment in 20% (2 of 10) of the placebo arm compared with 67% (6 of 9) of the anakinra arm 28
- Medical management of anxiety and depression
- Nd:YAG laser hair removal. For axillary involvement, laser hair removal can be quite helpful. In addition, the 1064 nm nd:YAG laser has been used ongoing with benefit in uncontrolled studies 29.
Hidradenitis suppurativa surgery
If medical therapy is not successful and the patient desires a “cure,” a surgical approach may be considered 30. This usually consists of excision of all diseased tissue in the area. Limited excisions usually result in recurrence adjacent to the scar. In one study, limited excision of diseased tissue had a 43% recurrence rate whereas radical excision had only a 27% recurrence rate 31. With appropriate patient selection, patient satisfaction with surgery is high 32.
There are both localized and extensive surgical interventions. Although there is no consensus on the best approach, procedures are carried out based on disease severity and location, with the overall goal of removing lesional tissue and sparing healthy skin to optimize outcomes.
- Incision and drainage of acute abscesses
- Curettage and deroofing of nodules, abscesses and sinuses. Incision and drainage is usually not helpful as lesions invariably recur. Deroofing an inflammatory nodule, curetting the base, and letting it heal by secondary intention is recommended 33.
- Laser ablation of nodules, abscesses and sinuses
- Wide local excision of persistent nodules
- Radical excisional surgery of entire affected area
Many approaches exist to manage hidradenitis suppurativa, including local destruction, incision and drainage, standard unroofing, and wide excision techniques 34. Local destruction is used to ablate hidradenitis suppurativa lesions and may be carried out with electrosurgery, cryotherapy, or laser removal. Incision and drainage may be used for decompression in acute episodes of unbearable pain. However, incision and drainage does not assist in the long-term resolution of disease, as the inflamed tissue remains and infection is almost certain to recur 35. Unroofing techniques are effective for both small and large lesional units and are carried out by opening the surface of all connected abscesses and tracts within an hidradenitis suppurativa lesion. The contents are removed by curettage, often leaving the site open to heal by secondary intention 36. Unroofing techniques are preferred for Hurley stage I/II, whereas skin-tissue-saving excision with electrosurgical peeling (STEEP) is preferred for Hurley stage II/III. Skin-tissue-saving excision with electrosurgical peeling (STEEP) similarly removes diseased, fibrotic tissue via electrosurgical loop while sparing healthy skin to decrease sequelae following the surgical procedure 37. Lesions that cannot be unroofed may be excised, which includes the removal of the entire diseased area up to the margins of normal-appearing subcutaneous tissue 34.
The best surgical approach for long-term outcomes is controversial and is dependent on the patient’s disease severity and location of the lesions. A recent systematic review and meta-analysis assessed for recurrence rates with varying methods of surgical management. The lowest rates of recurrence occurred following wide excision therapy when compared to local excision and deroofing procedures. This study also indicated that recurrence rates were lowest with skin grafts and skin flaps compared to primary closure, although this was limited by retrospective analysis and lack of randomization of closures 38. Wide excision followed by secondary intention healing was also shown to be functional and aesthetically acceptable to patients 39. Bias may exist in the discrepancy between recurrence rates and type of closure owing to the fact that primary closure is possible only with smaller wound sizes compared to larger excisions that simply cannot be closed by primary intention. Although this has not been formally assessed, the size of the wound may play a role.
The use of lasers in hidradenitis suppurativa management has gained recent popularity. The 1064 nm neodymium-doped yttrium aluminum garnet (Nd:YAG) laser appears to be an effective, novel modality in hidradenitis suppurativa management. After a series of treatments, two trials reported decreases in hidradenitis suppurativa-associated inflammation, scarring, and fibrosis, indicating successful, selective photothermolysis to manage the disease 40. It is best used in recalcitrant Hurley stage I and II patients.
Another type of laser used in the treatment of hidradenitis suppurativa is the carbon dioxide (CO2) laser, which is used to excise hidradenitis suppurativa lesions and ablate pathologic tissues. CO2 laser has been used since the late 1980s for hidradenitis suppurativa, although it is now increasing in popularity. Laser excision followed by marsupialization has been shown to be effective for the management of persistent or late-stage cases of hidradenitis suppurativa, with overall patient satisfaction in post-operative quality of life and pain measures 41. Additionally, a retrospective study (n = 58) of CO 2 laser evaporation techniques reported a 29% recurrence rate of disease within 12.2 months of the procedure (noted around the borders of treated regions), while 95% of patients reported some or great improvement in disease status 42. A reported complication of CO2 excision is scar contracture, restricted range of motion, and delayed wound healing. Nicholson et al. determined that fractional CO 2 therapy could be a helpful adjunct in these cases 43.
Painless lump under armpit
Non-Hodgkin lymphoma is another possible cause of a painless swelling in a lymph node, usually in the neck, armpit or groin.
Some people with non-Hodgkin lymphoma also have other, more general symptoms.
Non-Hodgkin lymphoma symptoms can include:
- night sweats
- unintentional weight loss
- a high temperature (fever)
- feelings of breathlessness
- persistent itching of the skin all over the body
Other symptoms depend on where in the body the enlarged lymph glands are (for example, swollen tonsils, a lump in the tummy, or skin rashes).
A few people with lymphoma have abnormal cells in their bone marrow when they’re diagnosed.
This may lead to:
- persistent tiredness or fatigue
- an increased risk of infections
- excessive bleeding, such as nosebleeds, heavy periods and spots of blood under the skin
How non-Hodgkin lymphoma is diagnosed?
The only way to confirm a diagnosis of non-Hodgkin lymphoma is by carrying out a biopsy.
This is a minor surgical procedure where a sample of affected lymph node tissue is removed and studied in a laboratory.
Further testing
If a biopsy confirms a diagnosis of non-Hodgkin lymphoma, further testing will be required to check how far the lymphoma has spread.
This allows a doctor to diagnose the stage of your lymphoma.
Further tests may include:
- blood tests – samples of blood will be taken throughout your diagnosis and treatment to check your general health, the levels of red and white cells and platelets in your blood, and how well organs such as your liver and kidney are working
- chest X-ray – this can check whether the cancer has spread to your chest or lungs
- bone marrow sample – another biopsy may be carried out to see if the lymphoma has spread to your bone marrow; this involves using a long needle to remove a sample of bone marrow from your pelvis and can be done using a local anaesthetic
- CT scan – this scan takes a series of X-rays that build up a 3D picture of the inside of the body to check the spread of the cancer
- MRI scan – this scan uses strong magnetic fields to build up a detailed picture of areas of your body to check the spread of the cancer
- PET scan – this scan measures the activity of cells in different parts of the body, and can check the spread of the cancer and the impact of treatment; it’s usually taken at the same time as a CT scan to show precisely how the tissues of different sites of the body are working
- lumbar puncture – using a thin needle, a sample of spinal fluid is taken and examined to see if it contains any lymphoma cells
Stages of non-Hodgkin lymphoma
When the testing is complete, it should be possible to determine the stage of your lymphoma. “Staging” means scoring the cancer by how far it’s spread.
The main stages of non-Hodgkin lymphoma are:
- Stage 1 – the cancer is limited to 1 group of lymph nodes, such as your neck, armpit or groin nodes, either above or below your diaphragm (the sheet of muscle underneath the lungs)
- Stage 2 – 2 or more lymph node groups are affected, both either above or below, but just on one side of, the diaphragm
- Stage 3 – the cancer has spread to lymph node groups on both sides of the diaphragm, above and below
- Stage 4 – the lymphoma has spread beyond the lymphatic system and is now present in both lymph nodes and organs or bone marrow
Health professionals also add the letter “A” or “B” to your stage to indicate whether or not you have certain symptoms.
- “A” is put after your stage if you have no additional symptoms other than swollen lymph nodes.
- “B” is put after your stage if you have additional symptoms of weight loss, fever or night sweats.
In some cases, health professionals also use additional letters to indicate where the cancer first developed.
For example, “E” (extranodal) means the cancer developed outside the lymphatic system.
Non-Hodgkin lymphoma treatment
There are many subtypes of non-Hodgkin lymphoma, but they can generally be put into 1 of 2 broad categories:
- High-grade or aggressive non-Hodgkin lymphoma – where the cancer grows quickly and aggressively
- Low-grade or indolent non-Hodgkin lymphoma – where the cancer grows slowly and you may not experience any symptoms for many years
The outlook and treatment for non-Hodgkin lymphoma varies greatly, depending on the exact type, grade and extent of the lymphoma, and the person’s age.
Low-grade tumours don’t necessarily require immediate medical treatment, but are harder to completely cure.
High-grade lymphomas need to be treated straight away, but tend to respond much better to treatment and can often be cured.
The main treatments used for non-Hodgkin lymphoma are:
- chemotherapy
- radiotherapy
- a type of targeted treatment called monoclonal antibody therapy
Overall, most cases of non-Hodgkin lymphoma are considered very treatable.
But there’s a risk of long-term problems after treatment, including infertility and an increased risk of developing another type of cancer in the future.
Armpit lump treatment
Armpit lump treatment depends on what is causing the lump.
References- Smith MK, Nicholson CL, Parks-Miller A, Hamzavi IH. Hidradenitis suppurativa: an update on connecting the tracts. F1000Research. 2017;6:1272. doi:10.12688/f1000research.11337.1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5538037/
- JAAD 2015;72;485
- JEADV 2016;230;174
- Ann R Coll Surg Engl. 2007 Oct; 89: 709–712
- Hurley H. Axillary hyperhidrosis, apocrine bromhidrosis, hidradenitis suppurativa, and familial benign pemphigus: surgical approach. In: Roenigh R, Roenigh H, eds. Dermatologic surgery. New York: Marcel Dekker; 1989:729-739.
- Sartorius K, Emtestam L, Jemec GB et al. Objective scoring of hidradenitis suppurativa reflecting the role of tobacco smoking and obesity. Br J Dermatol 2009; 161: 831–839.
- Jemec GB, Hansen U. Histology of hidradenitis suppurativa. J Am Acad Dermatol. 1996;34(6):994-999.
- Ring HC, Riis Mikkelsen P, Miller IM, et al. The bacteriology of hidradenitis suppurativa: a systematic review. Exp Dermatol. 2015;24(10):727-731.
- Ring HC, Bay L, Nilsson M, et al. Bacterial Biofilm in Chronic Lesions of Hidradenitis Suppurativa. Br J Dermatol. 2016.
- Danby FW. Diet in the prevention of hidradenitis suppurativa (acne inversa). J Am Acad Dermatol. 2015;73(5 Suppl 1):S52-54.
- Cannistra C, Finocchi V, Trivisonno A, Tambasco D. New perspectives in the treatment of hidradenitis suppurativa: surgery and brewer’s yeast-exclusion diet. Surgery. 2013;154(5):1126-1130.
- Prens E, Deckers I. Pathophysiology of hidradenitis suppurativa: An update. J Am Acad Dermatol. 2015;73(5 Suppl 1):S8-11.
- Acta Derm Vener 2014;94;553
- Acta Derm Venereol 2014; 94: 699–702
- JAMA Derm 2013;149(6):732-35
- PD 2017;34;578
- JAAD 2016;75;1151
- JAAD 2016;75;1061
- JAAD Dec 2012
- J Drugs Dermatol 2016;15;1192
- BJD 2013;168;243-52
- BJD April 2014
- JAMA Derm 2017;153;1195
- JEADV 2012;27;1101
- Br J Dermatol 2017;177;858
- Br J Dermatol Jan 2011
- J Am Acad Dermatol. 2014;70:243-51
- JAMA Derm 2016;152;52
- Semin Cutan Med Surg. 2017;36:67-74
- Dermatol Surg. 2016 Sep;42(9):1030-40
- Int J Colorectal Dis 1998;13;164
- Dermatol Surg. 2017 Jan;43(1):125-133
- BJD July 2012
- Danby FW, Hazen PG, Boer J: New and traditional surgical approaches to hidradenitis suppurativa. J Am Acad Dermatol. 2015;73(5 Suppl 1):S62–5. 10.1016/j.jaad.2015.07.043
- Jemec GB: Clinical practice. Hidradenitis suppurativa. N Engl J Med. 2012;366(2):158–64. 10.1056/NEJMcp1014163
- Danby FW: Commentary: unroofing for hidradenitis suppurativa, why and how. J Am Acad Dermatol. 2010;63(3):481.e1–3. 10.1016/j.jaad.2010.01.033
- Blok JL, Spoo JR, Leeman FW, et al. : Skin-Tissue-sparing Excision with Electrosurgical Peeling (STEEP): a surgical treatment option for severe hidradenitis suppurativa Hurley stage II/III. J Eur Acad Dermatol Venereol. 2015;29(2):379–82. 10.1111/jdv.12376
- Mehdizadeh A, Hazen PG, Bechara FG, et al. : Recurrence of hidradenitis suppurativa after surgical management: A systematic review and meta-analysis. J Am Acad Dermatol. 2015;73(5 Suppl 1):S70–7. 10.1016/j.jaad.2015.07.044
- Humphries LS, Kueberuwa E, Beederman M, et al. : Wide excision and healing by secondary intent for the surgical treatment of hidradenitis suppurativa: A single-center experience. J Plast Reconstr Aesthet Surg. 2016;69(4):554–66. 10.1016/j.bjps.2015.12.004
- Xu LY, Wright DR, Mahmoud BH, et al. : Histopathologic study of hidradenitis suppurativa following long-pulsed 1064-nm Nd:YAG laser treatment. Arch Dermatol. 2011;147(1):21–8. 10.1001/archdermatol.2010.245
- Hazen PG, Hazen BP: Hidradenitis suppurativa: successful treatment using carbon dioxide laser excision and marsupialization. Dermatol Surg. 2010;36(2):208–13. 10.1111/j.1524-4725.2009.01427.x
- Mikkelsen PR, Dufour DN, Zarchi K, et al. : Recurrence rate and patient satisfaction of CO2 laser evaporation of lesions in patients with hidradenitis suppurativa: a retrospective study. Dermatol Surg. 2015;41(2):255–60. 10.1097/DSS.0000000000000264
- Nicholson CL, Hamzavi I, Ozog DM: Rapid healing of chronic ulcerations and improvement in range of motion after fractional carbon dioxide (CO 2) treatment after CO 2 excision of hidradenitis suppurativa axillary lesions: A case report. JAAD Case Rep. 2016;2(1):4–6. 10.1016/j.jdcr.2015.11.001