What is lymphangitis
Lymphangitis is an infection or inflammation of the lymph vessels (channels). Lymphangitis is a complication of some bacterial infections.
The lymphatic system encompasses a network of lymph nodes, lymph ducts, lymph vessels, and organs located throughout the body that produce and move a fluid called lymph from tissues to the bloodstream. Functioning as part of the immune system, it also transports fluids, fats, proteins, and other substances in the body. Lymph nodes, or glands, filter the lymph fluid. Foreign bodies such as bacteria and viruses are processed in the lymph nodes to generate an immune response to fight infection.
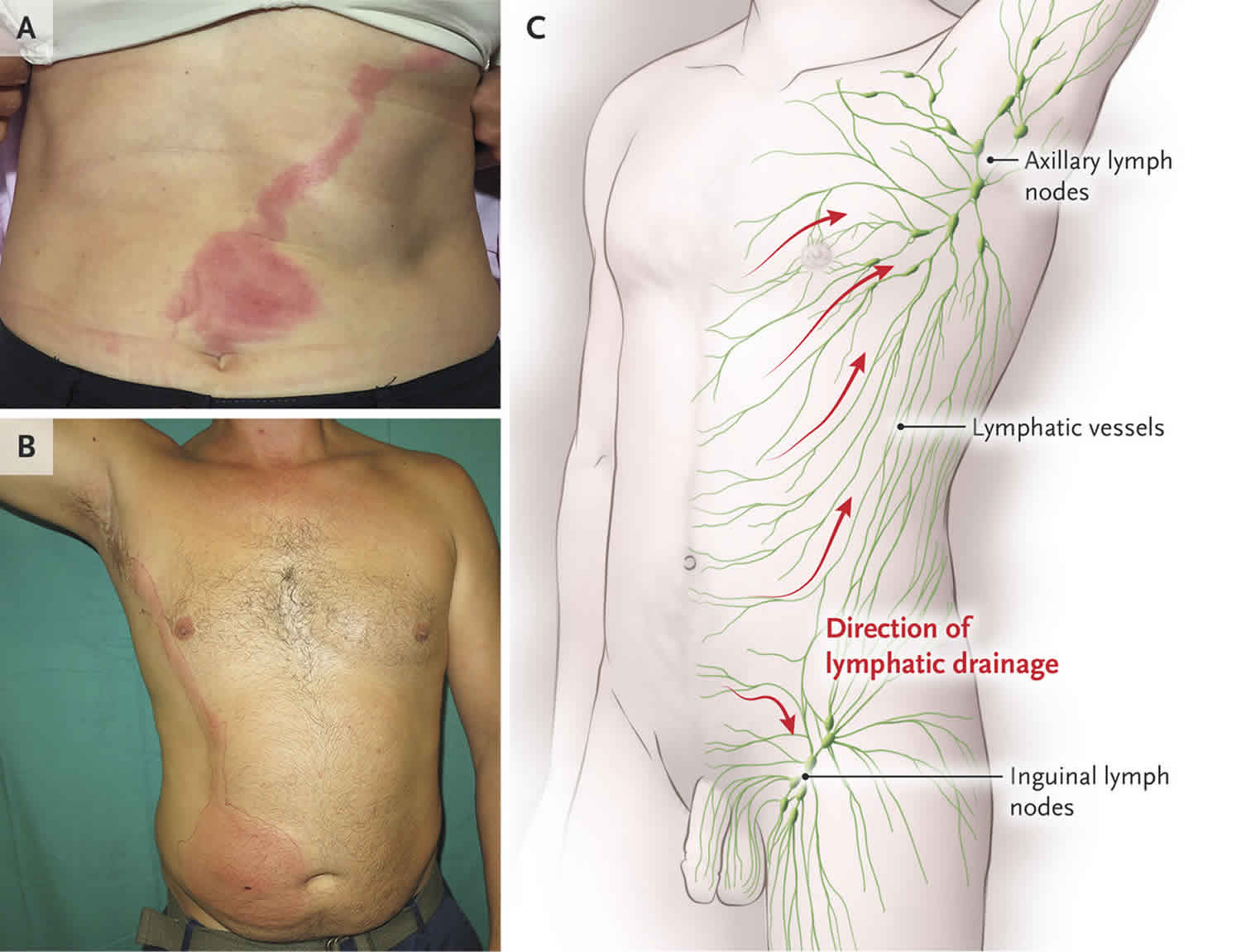
However, when pathogenic organisms enter the lymphatic channels, invading directly through an abrasion or wound or as a complication of infection, local inflammation and subsequent infection ensue, manifesting as red streaks on the skin. The inflammation or infection then extends proximally toward regional lymph nodes. Bacteria can grow rapidly in the lymphatic system.
Although no specific data regarding sex-related demographics are available for lymphangitis, two thirds of patients with cellulitis (a complication of lymphangitis occurring in the absence of appropriate antimicrobial therapy) are reported to be male.
Nodular lymphangitis is a distinct clinical entity, separate from lymphangitis. This disorder is characterized by inflammatory nodules along the lymphatics draining a primary skin infection.
Figure 1. Lymphangitis arm
Footnote: Erythematous patch with central bulla on the ventral forearm, with a lymphangitic streak extending to the antecubital fossa in a patient with herpes simplex virus infection versus a reaction to an arthropod bite.
[Source 1 ]Figure 2. Lymphangitis bug bite
Footnote: Two annular patches with surrounding erythema associated with lymphangitic streaks that developed after insect bites on the medial thigh of a patient with chronic lymphocytic leukemia.
[Source 1 ]Lymphangitis causes
Lymphangitis most often results from an acute streptococcal infection of the skin. Group A beta-hemolytic streptococci are the most common causes of lymphangitis 2. These organisms elaborate fibrinolysins and hyaluronidase, which aid their invasion of lymphatic channels. Lymphangitis caused by group A beta-hemolytic streptococci can rapidly progress and has been associated with serious complications. Less often, lymphangitis is caused by a Staphylococcus aureus infection. The infection causes the lymph vessels to become inflamed.
Lymphangitis may be a sign that a skin infection is getting worse. The bacteria can spread into the blood, and cause life-threatening problems.
Other organisms that can cause lymphangitis include the following:
- Pseudomonas species
- Streptococcus pneumoniae – A relatively uncommon cause of lymphangitis
- Pasteurella multocida – Associated with dog and cat bites; can cause cellulitis and lymphangitis
- Gram-negative rods, gram-negative bacilli, and fungi – May cause cellulitis and resultant lymphangitis in immunocompromised hosts
- Aeromonas hydrophila – Can contaminate wounds that occur in freshwater
- Wuchereria bancrofti – This filarial nematode is a major cause of acute lymphangitis worldwide; signs and symptoms of lymphangitis caused by Wuchereria bancrofti are indistinguishable from those of bacterial lymphangitis 3
In addition, individuals with diabetes, immunodeficiency, varicella, chronic steroid use, or other systemic illnesses have increased risk of developing serious or rapidly spreading lymphangitis.
A literature review by Cohen et al indicated that nonbacterial etiologies of lymphangitis with lymphangitic streaking include viral and fungal infections, insect and spider bites, and noninfectious, iatrogenic causes, with the latter reportedly including treatment with bacillus Calmette-Guérin vaccine, purified protein derivative placement, and topical treatment of verrucae vulgaris with cantharidin 4.
Lymphangitis symptoms
Lymphangitis symptoms may include:
- Fever and chills
- Enlarged and tender lymph nodes (glands) — usually in the elbow, armpit, or groin
- General ill feeling (malaise)
- Headache
- Loss of appetite
- Muscle aches
- Red streaks from the infected area to the armpit or groin (may be faint or obvious)
- Throbbing pain along the affected area
Lymphangitis possible complications
Health problems that may occur include:
- Abscess (collection of pus)
- Cellulitis (a skin infection)
- Sepsis (a general or bloodstream infection)
Lymphangitis diagnosis
The doctor will perform a physical exam, which includes feeling your lymph nodes and examining your skin. The doctor may look for signs of injury around swollen lymph nodes.
A biopsy and culture of the affected area may reveal the cause of the inflammation. A blood culture may be done to see if the infection has spread to the blood.
Lymphangitis treatment
Lymphangitis may spread within hours. Treatment should begin right away.
Treatment may include:
- Antibiotics by mouth or IV (vein) to treat any infection
- Pain medicine to control pain
- Anti-inflammatory medicines to reduce inflammation and swelling
- Warm, moist compresses to reduce inflammation and pain
Surgery may be needed to drain an abscess.
Lymphangitis prognosis
The prognosis for patients with uncomplicated lymphangitis is good. Prompt treatment with antibiotics usually leads to a complete recovery. It may take weeks, or even months, for swelling to disappear. The amount of time it takes to recover depends on the cause of your lymphangitis.
Without appropriate antimicrobial therapy, however, cellulitis may develop or extend along the channels; necrosis and ulceration may occur.
Morbidity and mortality
Lymphangitis may spread within hours. The morbidity and mortality associated with the disease is related to the underlying infection. Although no specific data are available regarding complications and mortality associated with lymphangitis alone, lymphangitis caused by group A beta-hemolytic streptococci can lead to bacteremia, sepsis, and death.
References- Nonbacterial Causes of Lymphangitis with Streaking. J Am Board Fam Med November 2016, 29 (6) 808-812; DOI: https://doi.org/10.3122/jabfm.2016.06.160015
- Lymphangitis. https://emedicine.medscape.com/article/966003-overview
- Akogun OB, Akogun MK, Apake E, Kale OO. Rapid community identification, pain and distress associated with lymphoedema and adenolymphangitis due to lymphatic filariasis in resource-limited communities of North-eastern Nigeria. Acta Trop. 2011 Sep. 120 Suppl 1:S62-8
- Cohen BE, Nagler AR, Keltz Pomeranz M. Nonbacterial causes of lymphangitis with streaking. JABFM. 2016 Nov-Dec. 29(6):808-12