Magnesium deficiency
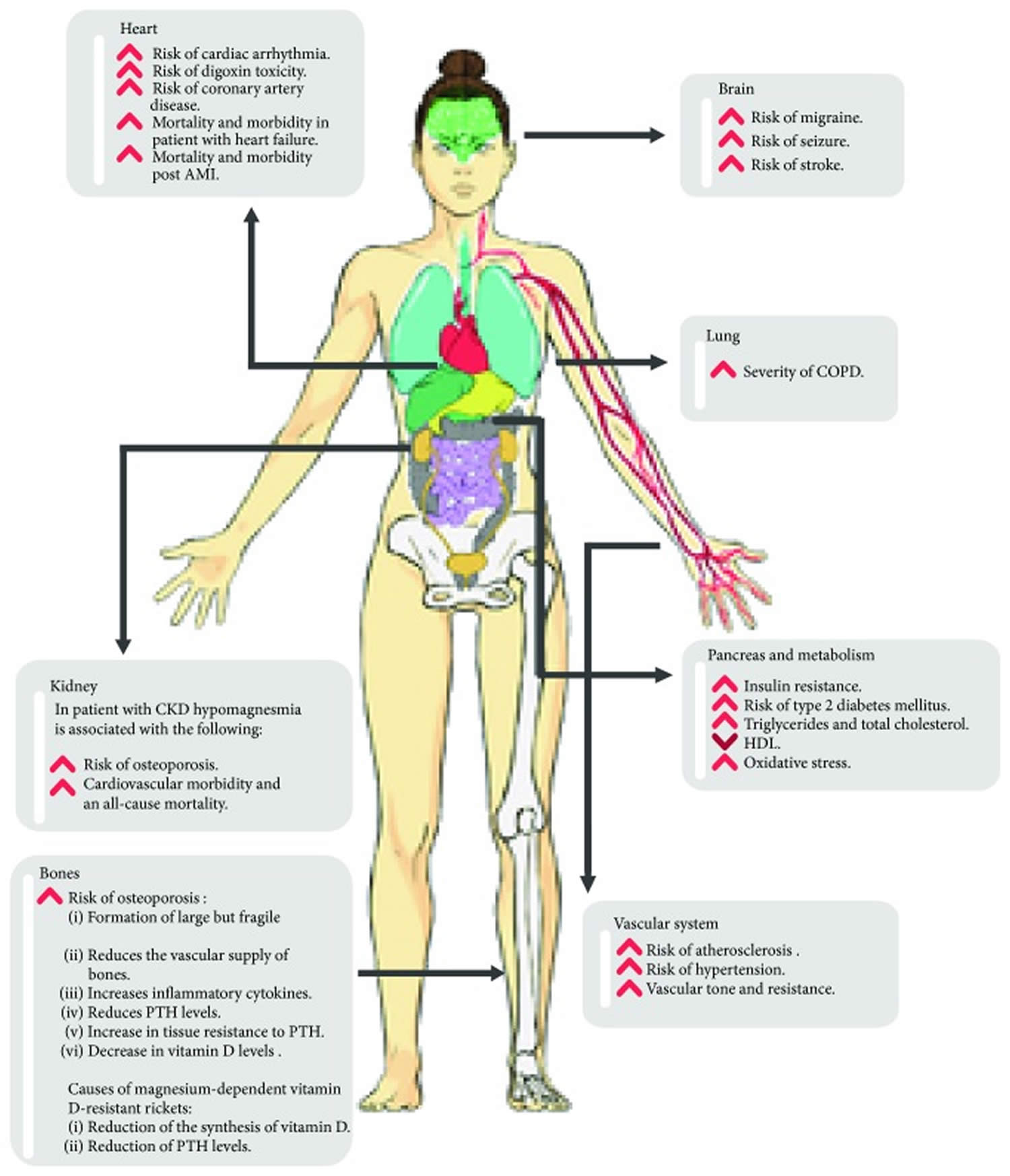
Magnesium deficiency also called hypomagnesemia or low magnesium is a condition in which the amount of magnesium in your blood (plasma) is lower than normal. Normal serum magnesium levels are between 0.6 millimoles/liter (mmol/L) and 1.1 mmol/L (1.46 mg/dL to 2.68 mg/dL) 1. Magnesium deficiency or hypomagnesemia is an electrolyte disturbance caused by a low serum magnesium level less than 0.6 mmol/L (less than 1.46 mg/dL) in the blood 1. When the level of magnesium in your body drops below normal, symptoms develop due to low magnesium. However, it is typically asymptomatic until serum magnesium concentration is less than 0.5 mmol/L (1.22 mg/dL) 2. While mild magnesium deficiency may not elicit clinical symptoms, it may be associated with an increased risk of developing chronic diseases (see Figure 6 below) 3.
Magnesium deficiency in healthy individuals who are consuming a balanced diet is quite rare because magnesium is abundant in both plant and animal foods and because the kidneys are able to limit urinary excretion of magnesium when intake is low. During low intakes of magnesium, the magnesium absorbed from the diet is increased, the amount in urine is decreased, and body magnesium reserves (bone is the major reserve) are used 4. When the dietary intake of magnesium is adequate, the opposite occurs. Magnesium homeostasis involves the kidney (primarily through the proximal tubule, the thick ascending loop of Henle, and the distal tubule), small bowel (primarily through the jejunum and ileum), and bone. Hypomagnesemia occurs when something, whether a drug or a disease condition, alters the homeostasis of magnesium 1.
Low magnesium levels or hypomagnesemia can occur secondary to kidney and gastrointestinal losses 5, 6.
Common causes of magnesium deficiency or hypomagnesemia include 7:
- Alcohol use disorder
- Burns that affect a large area of the body
- Chronic diarrhea
- Excessive urination (polyuria), such as in uncontrolled diabetes and during recovery from acute kidney failure
- Hyperaldosteronism (disorder in which the adrenal gland releases too much of the hormone aldosterone into the blood)
- Kidney tubule disorders
- Malabsorption syndromes, such as celiac disease and inflammatory bowel disease
- Malnutrition
- Medicines
- Diuretics (furosemide, thiazide)
- Epidermal growth factor (EGF) receptor inhibitors (cetuximab)
- Proton pump inhibitors (all, such as omeprazole)
- Calcineurin inhibitors (cyclosporin A, tacrolimus)
- Platinum derivatives (cisplatin, carboplatin)
- Antimicrobials (aminoglycosides, pentimidine, rapamycin, amphotericin B, foscarnet)
- Pancreatitis (swelling and inflammation of the pancreas)
- Excessive sweating
- Genetic causes 8
- Hypercalciuric hypomagnesemias
- Bartter syndrome
- Gitelman syndrome
- EAST (epilepsy, ataxia, sensorineural deafness and tubulopathy) syndrome
- Mitochondrial hypomagnesemias
- Autosomal dominant tubulointerstitial kidney disease
- Autosomal dominant hypocalcemia with hypocalciuria
- Episodic ataxia type 1
- Familial hypomagnesemia with hypocalcemia and nephrocalcinosis
- Hypertension, hypercholesterolemia and hypomagnesemia
- Hyperphenylalaninemia BH4-deficient
- Hypomagnesemia with secondary hypocalcemia
- Hypomagnesemia with seizures and mental retardation
- Hyperuricemia, pulmonary hypertension, renal failure and alkalotic syndrome (HUPRAS)
- Kenny−Chaffey syndrome type 2
- Kearns-Sayre syndrome
- Neonatal inflammatory skin and bowel disease type 2 (NISBD2)
- Renal cysts and diabetes
Figure 1. Factors associated with magnesium deficiency
[Source 9 ]Signs and symptoms of of magnesium deficiency can be nonspecific and usually overlap with symptoms of other electrolyte imbalances 10. The severity of symptoms and signs depends on the degree of magnesium depletion, rate, extent and duration of magnesium decline 10. Low magnesium symptoms usually occur when serum magnesium levels fall below 0.5 mmol/L (1.2 mg/dL) 11. The signs and symptoms of hypomagnesemia may affect every system including neuromuscular, cardiovascular, renal, and gastrointestinal systems 12, 13. The signs and symptoms of hypomagnesemia may include 14, 15, 16:
- Neuromuscular
- Tremors, muscle fasciculation, muscle spasms and cramps, muscle contractions, numbness, tingling, generalized weakness and tiredness.
- Central nervous system
- Agitation, depression, sudden change in behavior, encephalopathy, and seizures.
- Cardiovascular
- Cardiac arrhythmia, ECG changes and cardiac ischemia.
- Gastrointestinal
- Loss of appetite, nausea, and vomiting.
- Metabolic
- Low serum potassium concentrations (hypokalemia) and low serum calcium concentrations (hypocalcemia). Magnesium deficiency also can cause hypocalcemia (low blood calcium), as the two are interrelated. Decreased magnesium causes impaired magnesium-dependent adenyl cyclase generation of cyclic adenosine monophosphate (cAMP), decreasing parathyroid hormone (PTH) release. Hypocalcemia persisted despite increased secretion of parathyroid hormone (PTH), which regulates calcium homeostasis. Usually, increased parathyroid hormone (PTH) secretion quickly results in the mobilization of calcium from bone and normalization of blood calcium concentration. As the magnesium depletion progressed, parathyroid hormone (PTH) secretion diminished to low concentrations. In addition to hypomagnesemia, signs of severe magnesium deficiency included hypocalcemia, low serum potassium concentrations (hypokalemia), retention of sodium, low circulating parathyroid hormone (PTH) concentrations, neurological and muscular symptoms (tremor, muscle spasms, tetany), loss of appetite, nausea, vomiting, and personality changes 17.
- Untreated, magnesium deficiency or hypomagnesemia can lead to:
- Cardiac arrest
- Respiratory arrest
- Coma
- Death
In addition, (severe) hypomagnesemia may have further consequences during pregnancy, as suggested by findings that a magnesium deficient diet in pregnant mice was able to induce fetal malformations 18. Conversely, supplementation with magnesium sulfate (MgSO4) during pregnancy is a treatment for pre-eclampsia 19, 20, suggesting a role for a relative shortage of magnesium in this disease too. Furthermore, some diseases, such as Parkinson’s disease and diabetes, have merely been associated with low serum magnesium concentrations 21. However, it is not yet clear whether hypomagnesemia is the cause, a consequence or simply an epiphenomenon in these diseases.
Magnesium also affects the electrical activity of the heart muscle (myocardium) and vascular tone, which is why patients with hypomagnesemia are at risk for cardiac arrhythmias. In addition, when magnesium is low, there is inhibition of renal outer medullary potassium channels, leading to increased urinary excretion and depletion of intracellular potassium levels. This reduces the threshold required for generating an action potential in the heart muscle cell (cardiac myocyte) 1. Moreover, reduced intracellular potassium levels also prolong the time to repolarize the cell membrane, increasing the risk of arrhythmias 1. In a systematic review and meta-analysis of experimental studies, authors showed that subjects with prediabetes had significantly lower serum Mg concentration than healthy controls (about 0.07 mmol/L) 22.
The risk of magnesium deficiency or hypomagnesemia depends on multiple characteristics in various healthcare settings. The reported prevalence in the general population is 2.5% to 15% 1. In hospitalized patients, magnesium deficiency or hypomagnesemia ranges from 12 to 20% 23, 24. The prevalence is even higher in critically ill patients, estimated to be 65% in a study 2. In a study of 100 critically ill children (mean age 4.9 years) admitted to a pediatric intensive care unit in India, the prevalence of magnesium deficiency or hypomagnesemia was about 55%. A study revealed a 30% prevalence of magnesium deficiency or hypomagnesemia in patients with chronic alcohol use disorder 25.
The diagnosis of magnesium deficiency or low magnesium is challenging 26, because magnesium serum concentration does not reflect the total content in the human body 27. You may have a “normal” serum magnesium concentration (0.7–1 mmol/L or 1.7–2.4 mg/dL) 28, but have relatively low levels of skeletal or cellular magnesium 29. Up till now, no single reliable indicator of magnesium deficiency is considered satisfactory 26. The difficulties of accessing total body magnesium concentration concerns its main two compartments, namely bone and muscle, while in blood it is present only in very small amounts (less than 1%) 30, 10, 31. It is possible that an individual can be in a magnesium-depleted state but have plasma or serum values within the “normal” range 32. Consequently, the clinical impact of magnesium deficiency may be underestimated. In plasma, the concentration of free magnesium is reported to be ~0.6 mmol/L (~14 mg/L) 33, with about 30% complexed by proteins 34. The major magnesium binding protein in plasma is serum albumin 35, 33.
In clinical practice, the total serum or plasma magnesium concentration is the most commonly used test to assess the magnesium status, and the normal reference range is usually 0.7–1 mmol/L (1.7–2.43 mg/dL) 28, 36. Plasma magnesium concentrations are closely related to bone metabolism, as there is continuous exchange between the skeleton and blood 37. However, the normal value varies from laboratory to laboratory, and different studies have used slightly different ranges. This may partially explain the differences in the prevalence of magnesium imbalances reported in different groups of patients with similar characteristics 12.
The treatment of patients with hypomagnesemia is based on a patient’s kidney function, the severity of their symptoms, and hemodynamic stability 1. If a patient is hemodynamically unstable in an acute hospital setting, 1 to 2 grams of magnesium sulfate can be given in about 15 minutes Gragossian A, Bashir K, Bhutta BS, et al. Hypomagnesemia. [Updated 2022 Nov 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK500003. For symptomatic, severe hypomagnesemia in a stable patient, 1 to 2 grams of magnesium sulfate can be given over one hour Gragossian A, Bashir K, Bhutta BS, et al. Hypomagnesemia. [Updated 2022 Nov 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK500003. Non-emergent repletion of magnesium in adult patient is generally 4 to 8 grams of magnesium sulfate given slowly over 12 to 24 hours 1. In children patients, the magnesium sulfate dose is 25 to 50 mg/kg (with a maximum of 2 grams) 38, 39.
For an asymptomatic patient with hypomagnesemia who is not hospitalized and can tolerate medications by mouth, sustained-release oral replacement should be tried first. Asymptomatic patients with hypomagnesemia can benefit from oral sustained-release magnesium preparations (magnesium chloride containing 64-71.5 mg or magnesium L-lactate containing 84 mg elemental magnesium) 1. After repletion, serum electrolyte levels must be rechecked (whether in an inpatient or outpatient setting) to ensure effective treatment. Although serum magnesium levels rise quickly with treatment, intracellular magnesium takes longer to replete. Therefore, patients with normal kidney function should try to continue magnesium repletion for two days after the level normalizes 1.
What is magnesium?
Magnesium (Mg or Mg2+) is an abundant mineral in your body that your body needs to stay healthy and is naturally present in many foods, added to other food products, available as a dietary supplement, and present in some medicines such as antacids and laxatives 40. Magnesium is an essential mineral which acts as a cofactor (a compound that is essential for the activity of an enzyme) in more than 300 enzyme systems that regulate diverse biochemical reactions in your body, including making protein, bone, and DNA, energy production, oxidative phosphorylation, glycolysis (the metabolic pathway in which glucose is broken down to produce energy), regulating muscle and nerve function, blood sugar control, blood pressure regulation, ion transport and cell signaling 41, 42, 43, 44, 45, 46, 47. According to the United States Food and Nutrition Board, recommended daily allowance for magnesium is 420 mg for adult males and 320 mg for adult females, respectively 48, 43. Approximately 10% of the daily magnesium requirement is derived from water 10. Green vegetables, nuts, seeds, and unprocessed cereals are rich sources of magnesium. Also, some magnesium is available in fruits, fish, meat, and milk products 49.
You can get recommended amounts of magnesium by eating a variety of foods, including the following 50:
- Legumes, nuts, seeds, whole grains, and green leafy vegetables (such as spinach)
- Fortified breakfast cereals and other fortified foods
- Milk, yogurt, and some other milk products
Magnesium contributes to the structural development of bone and is required for the synthesis of DNA, RNA, and the antioxidant glutathione. Magnesium also plays a role in the active transport of calcium and potassium ions across cell membranes, a process that is important to nerve impulse conduction, muscle contraction, and normal heart rhythm 45. Magnesium deficiency in healthy individuals who are consuming a balanced diet is quite rare because magnesium is abundant in both plant and animal foods and because the kidneys are able to limit urinary excretion of magnesium when intake is low 42. However, before you reach for a magnesium supplement, though, you should know that just a few servings of magnesium-rich foods a day can meet your need for this important nutrient.
The majority of the population in the Western countries consume less than the recommended amount of magnesium, contributed by the consumption of processed foods, demineralized water, and agricultural practices using soil deficient in magnesium for growing food 48, 12, 51. Approximately half (48%) of the US population has been shown to consume less than the daily requirement of magnesium from foods 52, partly because of the processing of food, a lower consumption of whole grains and fruits and vegetables than recommended, and a greater consumption of fast food that has a low magnesium content 53. The 2015 Dietary Guidelines Advisory Committee found magnesium to be underconsumed relative to the Estimated Average Requirement (EAR) and characterized it as a shortfall nutrient of public health concern 54. The European Food Safety Authority (EFSA) recently published a scientific opinion on dietary reference values for magnesium and found that “although the role of Mg in bone structure and physiology is well established, there are few quantitative data for using this relation for setting dietary reference values for magnesium” 55. Nevertheless, the impact of chronically low magnesium intake on serum magnesium concentrations and long-term health remains poorly studied; most trials have been of short duration, and most observational studies have lacked repeated serum measures.
Low magnesium levels, also called hypomagnesemia, may have no or few nonspecific symptoms in the short term. Early signs of magnesium deficiency (hypomagnesemia) include weakness, loss of appetite, fatigue, nausea, and vomiting 41. Afterwards, muscle contractions and cramps, numbness, tingling, personality changes, coronary spasms, abnormal heart rhythms (cardiac arrhythmias) and seizures can occur when magnesium deficiency worsens 56, 57. Finally, severe magnesium deficiency can result in low blood calcium (hypocalcemia) or low blood potassium (hypokalemia) because mineral homeostasis is disrupted 58. Long term (chronic) or severe low magnesium levels can increase your risk of high blood pressure, heart disease, type 2 diabetes and osteoporosis 59. Persistent or severe magnesium deficiencies can cause nausea, loss of appetite, fatigue, confusion, muscle cramps, seizures, changes in heart rate, and numbness or tingling. Severe magnesium deficiency can impede vitamin D and also affect calcium metabolism and exacerbate calcium deficiencies. Magnesium deficiencies or hypomagnesemia may be seen in those with gastrointestinal or kidney disorders, those suffering from chronic alcoholism, and older people 42. Poor dietary intake, gastrointestinal problems, and increased urinary loss of magnesium may all contribute to magnesium depletion in people suffering from alcoholism 42. Older adults have relatively low dietary magnesium intakes 60, 61. Intestinal magnesium absorption tends to decrease with age, and urinary magnesium excretion tends to increase with age; thus, suboptimal dietary magnesium intake may increase the risk of magnesium depletion in the elderly 62.
The following conditions increase the risk of magnesium deficiency 63:
- Gastrointestinal disorders: Prolonged diarrhea, Crohn’s disease, malabsorption syndromes, celiac disease, surgical removal of a portion of the small intestine, and intestinal inflammation due to radiation may all lead to magnesium depletion.
- Kidney disorders (magnesium wasting): Diabetes mellitus and long-term use of certain diuretics (see Drug interactions) may result in increased urinary loss of magnesium. Multiple other medications can also result in renal magnesium wasting 17.
- Endocrine and metabolic disorders: Several conditions, such as diabetes mellitus, parathyroid gland disorders, phosphate depletion, primary aldosteronism, and even excessive lactation, can lead to magnesium depletion.
An excess of magnesium also called hypermagnesemia may happen with the ingestion of antacids and laxatives that contain magnesium and with a decreased ability of the kidneys to excrete the excess magnesium (Mg). But clinically significant hypermagnesemia is rare due to the kidney’s ability to increase excretion when needed. Symptoms of excess magnesium (hypermagnesemia) can be similar to those of magnesium deficiency and include nausea and vomiting, muscle weakness, fatigue, loss of appetite, trouble breathing, an irregular heart rate and in severe cases, cardiac arrest (the sudden stopping of the heart) 64. Severe hypermagnesemia (levels greater than 12 mg/dL) can lead to cardiovascular complications (hypotension, and arrhythmias) and neurological disorder (confusion and lethargy). Higher values of serum magnesium (exceeding 15 mg/dL) can induce cardiorespiratory arrest and coma 65.
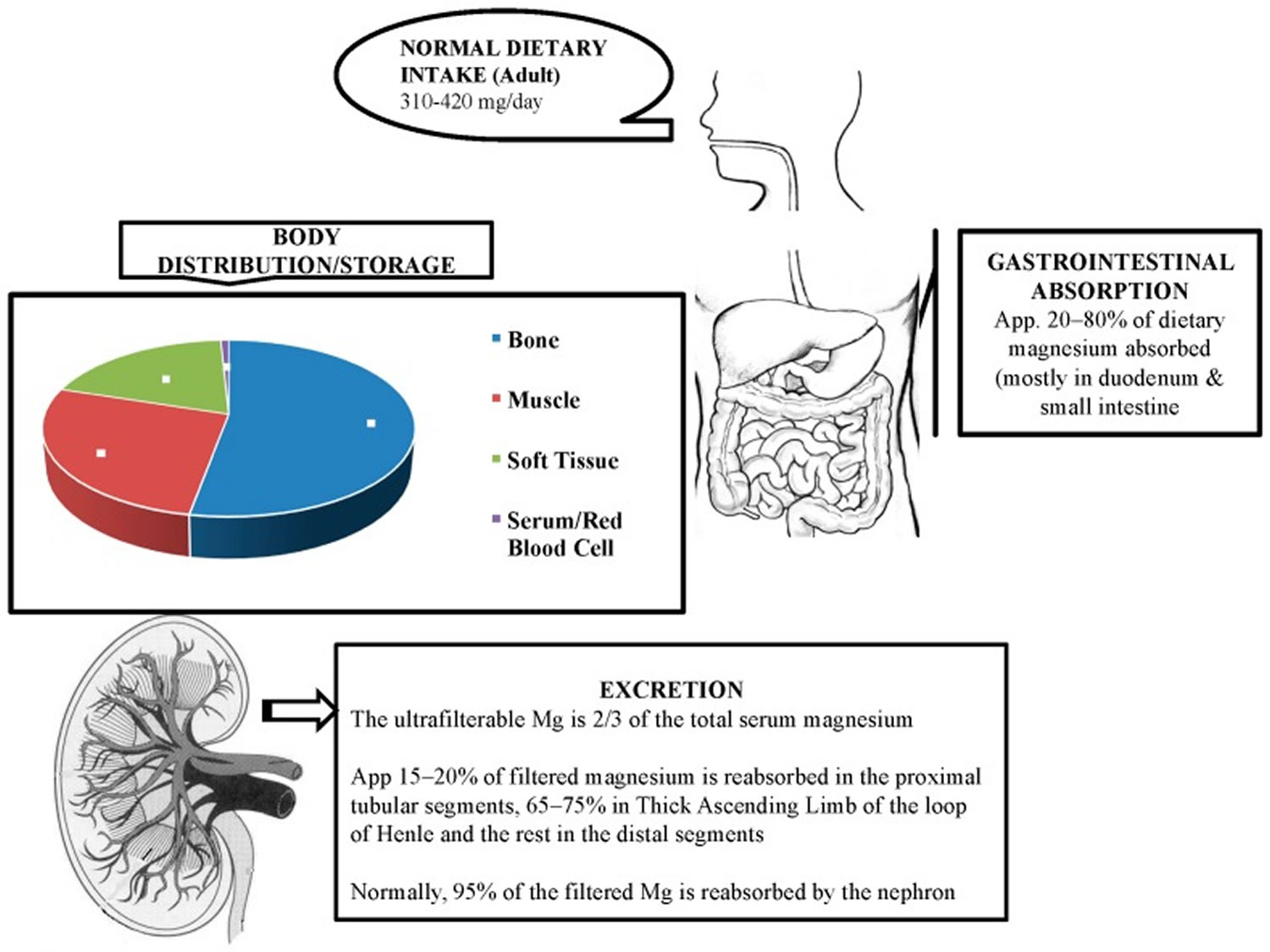
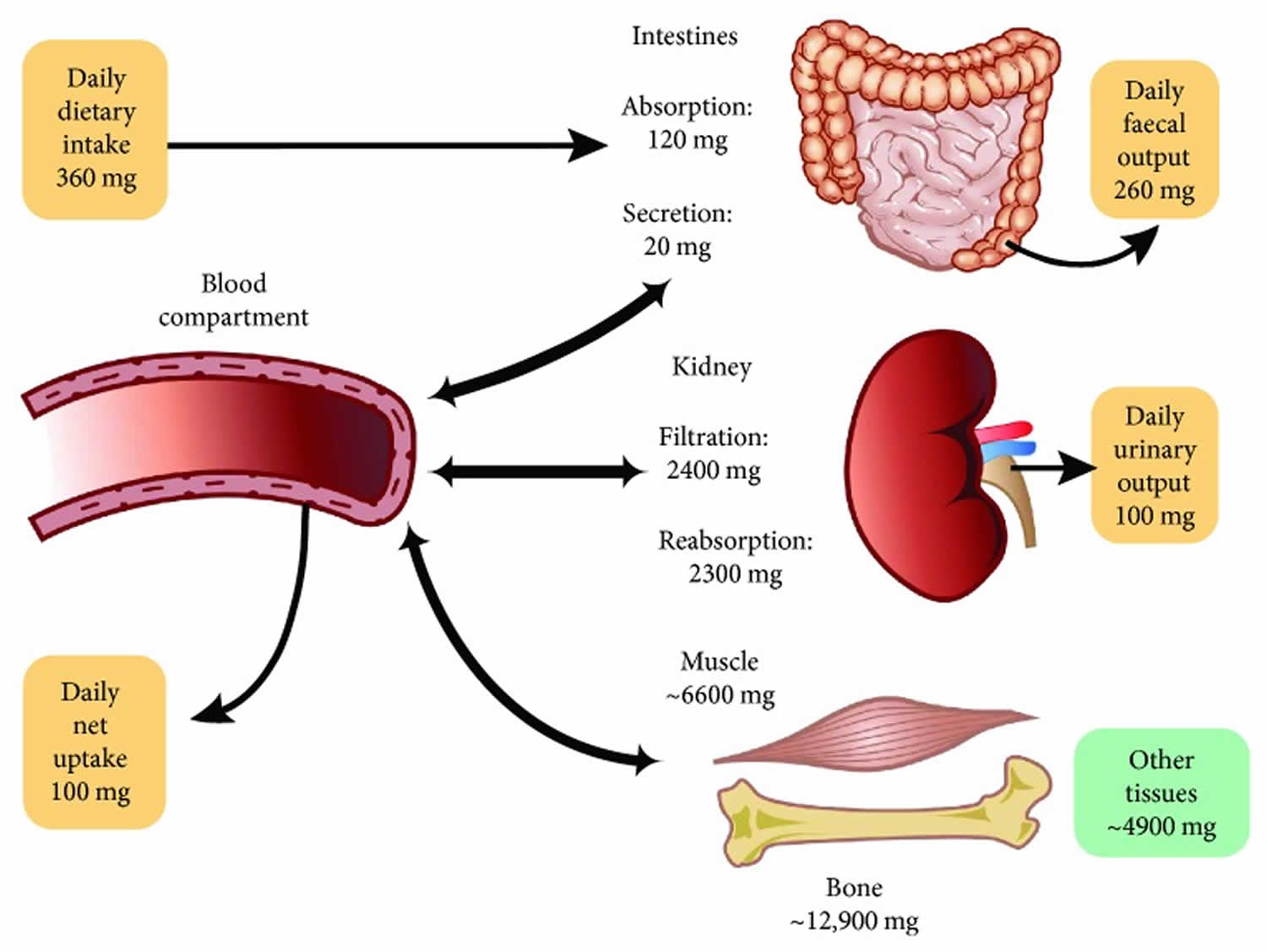
Magnesium enters your body through your diet and is absorbed by your small intestine and large intestine (colon). The total body magnesium in the average adult is approximately 1000 mmol or 25 g magnesium, that is, 20 mmol/kg of lean body mass, with 50% to 60% present in your bones and most of the rest in your muscles and other soft tissues (34% to 50%) 12, 48, 66, 67. Around one-third of the bone magnesium content is available for exchange to maintain the levels of extracellular magnesium 12. Less than 1% of total magnesium in the body is available in serum and red blood cells, accounting for the extracellular magnesium in your body 48. The magnesium levels in blood serum and extracellular fluids are kept under tight control through its absorption, reservoir, and excretion process by various organs such as the gut, bone, and kidney 9. Besides these organs, several hormones, namely vitamin D, parathyroid hormone (PTH), and estrogen, are involved in the regulation of normal level of magnesium 49, 68. The relationship between parathyroid hormone (PTH) and magnesium is complex and similar to calcium; high serum magnesium levels suppress the secretion of parathyroid hormone (PTH) via activation of calcium-sensing receptor (CaSR) present on the chief cells of the parathyroid glands 10. In contrast, low serum magnesium stimulates parathyroid hormone (PTH) secretion 10.
The magnesium homeostasis is primarily regulated by your kidneys 12. The glomeruli filter around 2400 mg of magnesium per day 32. Normally, only 3% of filtered magnesium appears in urine. About 97% of excreted magnesium is passively reabsorbed, mainly by the thick ascending limb of the loop of Henle (65%) and to a lesser extent in the distal tubules (30%) 65, 69, 70, 12, 71. Only around 100 mg to 120 mg of magnesium is excreted in the urine each day, and the kidneys can regulate the amount excreted, depending on the serum level of magnesium 12, 44, 70. Urinary excretion is reduced when magnesium status is low 43. Figure 2 below illustrates the magnesium balance in the human body.
Relatively little is known about cellular magnesium transport mechanisms 70. This factor is essential for the pathophysiology of kidney-related hypermagnesemia as along the loop of Henle, not only the volume of the filtrate gets reduced, but also the osmolarity decreases significantly (-66%), and consequently the solutes become less concentrated. Furthermore, this explains the high resorbent capacity of the kidney, which generally maintains magnesium equilibrium until the creatinine clearance falls below 20 ml/minute 65. Thus, an increase in plasma magnesium levels is practically impossible to achieve with diet alone in conditions of perfect kidney health. However, the odds of hypermagnesemia can increase by taking mega-doses of magnesium. The pathophysiology of hypermagnesemia related to excess laxative use is different. In this case, the huge amount of magnesium given through the digestive tract can lead to overwhelming the excretory mechanism, especially in cases with underlying subclinical renal failure 65.
Magnesium concentration within red blood cells is three times higher than in plasma 72. In mammalian cells, Mg2+ is an abundant cation present at concentrations ranging from 5 to 20 millimoles (mmol)/L (12.15 to 48.6 mg/dL) 73. In the plasma, the magnesium concentration is a little lower at around 1 mmol/L (2.43 mg/dL) 32. Many different reference values for serum magnesium have been proposed, which collectively suggest that, in healthy adults plasma magnesium concentration ranges somewhere between 0.6 and 1.2 millimoles (mmol)/L (1.46 to 2.92 mg/dL) 74, 43, 75. The Canadian Health Measure Survey Cycle 3 conducted in 2012–2013, measured serum magnesium in subjects aged 3–79 years 76. They reported that 9.5% to 16.6% of adults and 15.8% to 21.8% of adolescents (12–19 years) had serum magnesium concentrations < 0.75 mmol/L (< 1.82 mg/dL), which is a level currently accepted as an indication of hypomagnesemia or magnesium deficiency 76, 77, 78, 79. However, it has recently been suggested that serum magnesium concentrations < 0.75 mmol/L (< 1.82 mg/dL) value is likely to be too low and should be raised to <0.85 mmol/L (< 2.07 mg/dL), as values in this range are associated with increased health risks 74, 80. Razzaque 81 suggests that individuals with serum magnesium levels between 0.75 to 0.85 mmol/L (1.82 to 2.07 mg/dL) to undergo further investigation to confirm body magnesium status.
Approximately 30% of total plasma magnesium is protein-bound and approximately 70% is filterable through artificial membranes (15% complexed, 55% free Mg2+ ions) 82. With a glomerular filtration rate (GFR) of approximately 150 L per day and an ultrafiltrable magnesium concentration of 14 mg/L, the filtered magnesium load is approximately 2,100 mg per day.
Assessing magnesium status is difficult because most magnesium is inside cells or in bone 45. The most commonly used and readily available method for assessing magnesium status is measurement of serum magnesium concentration, even though serum levels have little correlation with total body magnesium levels or concentrations in specific tissues 79. Other methods for assessing magnesium status include measuring magnesium concentrations in red blood cells, saliva, and urine; measuring ionized magnesium concentrations in blood, plasma, or serum; and conducting a magnesium-loading (or “tolerance”) test. No single method is considered satisfactory 83. Some experts 66 but not others 45 consider the tolerance test (in which urinary magnesium is measured after parenteral infusion of a dose of magnesium) to be the best method to assess magnesium status in adults. To comprehensively evaluate magnesium status, both laboratory tests and a clinical assessment might be required 79.
Clinical and preclinical studies revealed that the magnesium level is found to be low in various pathological conditions such as migraine, diabetes, osteoporosis, asthma, preeclampsia, cardiovascular diseases and its correction is an important treatment strategy for these conditions 84, 85, 86, 87, 88, 89.
According to European Register on Nutrition and Health Claims 90, 41, the following claims about magnesium have been authorized. The claim may be used only for food which is at least a source of magnesium as referred to in the claim “a source of” magnesium as listed in the Annex to Regulation (EC) No 1924/2006.
- “Magnesium contributes to a reduction of tiredness and fatigue”;
- “Magnesium contributes to electrolyte balance”;
- “Magnesium contributes to normal energy-yielding metabolism”;
- “Magnesium contributes to normal functioning of the nervous system”;
- “Magnesium contributes to normal muscle function”;
- “Magnesium contributes to normal protein synthesis”;
- “Magnesium contributes to normal psychological function”;
- “Magnesium contributes to the maintenance of normal bones”;
- “Magnesium contributes to the maintenance of normal teeth”;
- “Magnesium has a role in the process of cell division”.
Figure 2. Physiology of magnesium
Footnote: Magnesium homeostasis is facilitated by intestinal absorption, bone which acts as a reservoir/store, and kidneys which are responsible for magnesium excretion.
[Source 91 ]Figure 3. Magnesium homeostasis
[Source 10 ]What does magnesium do?
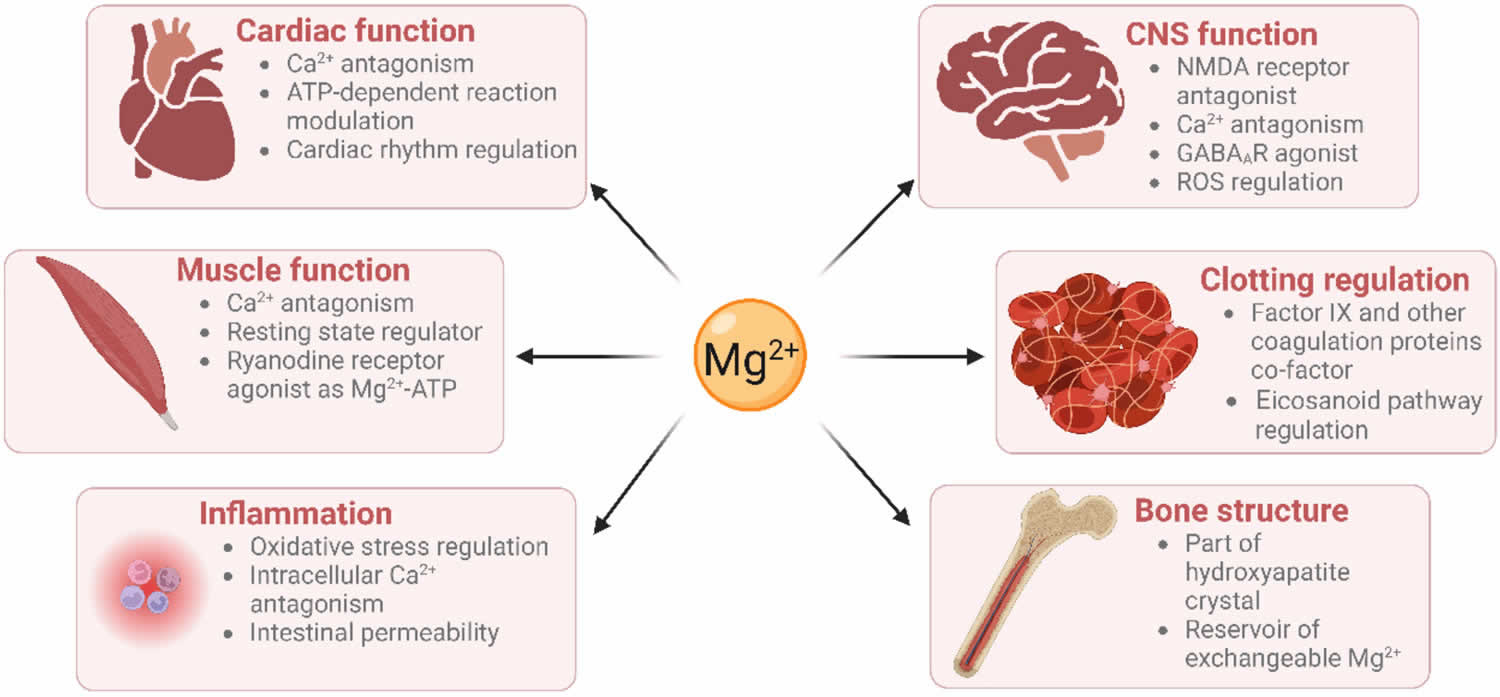
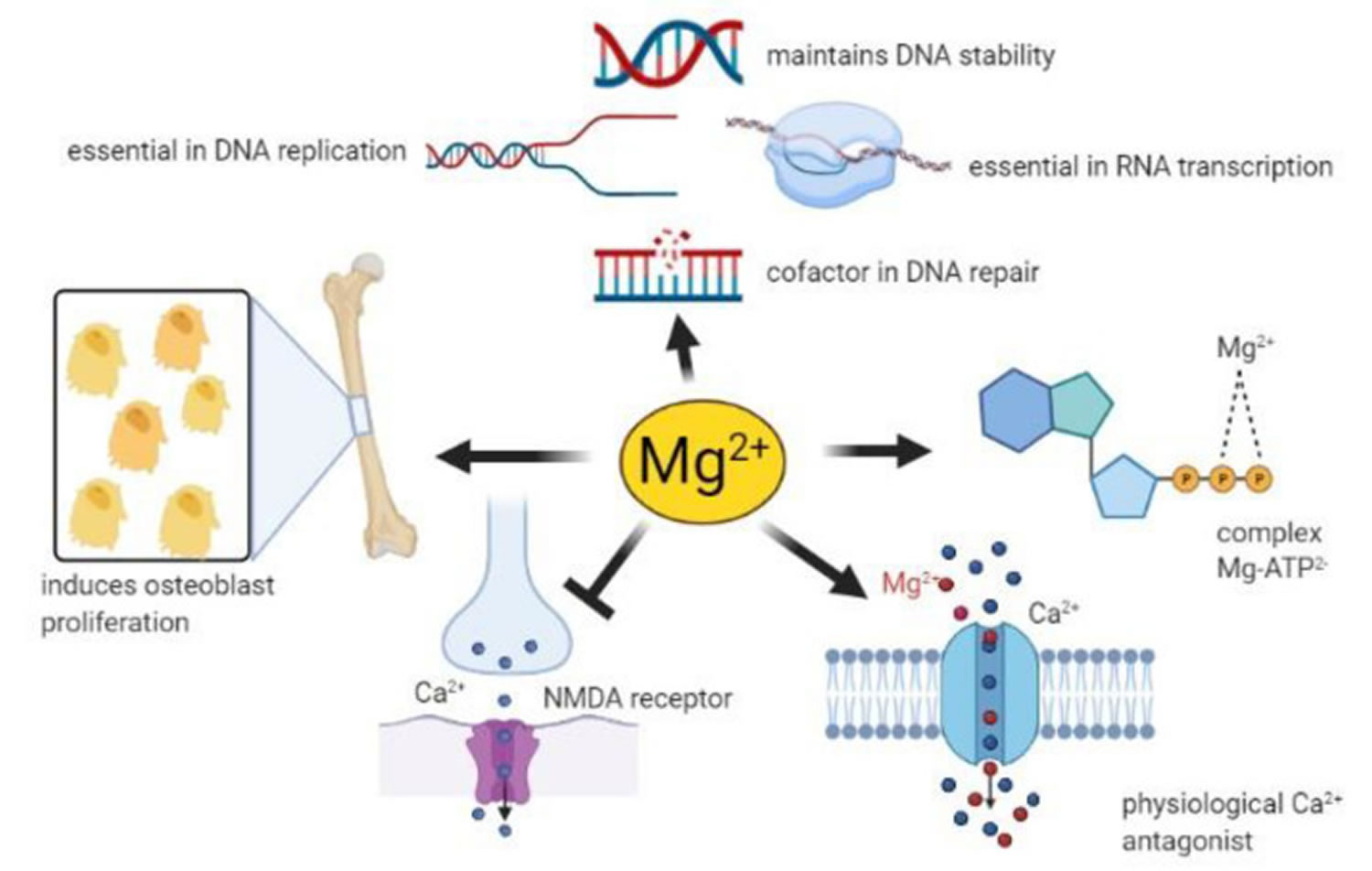
Every organ in your body, especially your heart, muscles, and kidneys, needs the mineral magnesium. Magnesium also contributes to the makeup of teeth and bones. Magnesium is important for physiological functions in your body, including regulating muscle and nerve function, blood sugar levels, and blood pressure; making protein and bone; regulating inflammation; maintaining hemostasis (a process that prevent and stop bleeding from a blood vessel), deoxyribonucleic acid (DNA) and ribonucleic acid (RNA) stability; as well as making the antioxidant glutathione 92, 93, 94, 95, 32, 41, 42, 43, 44, 45, 46, 47. Magnesium also plays a role in the active transport of calcium and potassium ions across cell membranes, a process that is important to nerve impulse conduction, muscle contraction, and normal heart rhythm 45.
Role of magnesium in the human body 13, 96, 97, 49, 13, 32, 26:
- Cofactor in more than 300 enzymes involved in:
- Protein synthesis, muscle and nerve transmission, neuromuscular conduction, and blood glucose and blood pressure regulation.
- Platelet function (clotting and/or thrombus formation).
- Muscle contraction/relaxation.
- Insulin regulation.
- Bone formation
- Role in active transport
- Facilitates active transport of calcium and potassium ions across cell membranes, which is essential for the conduction of nerve impulses (neurotransmission), muscle contraction, maintaining vascular tone and normal heart rhythm.
- Structural roles
- Important for the structure of bones, proteins, many enzymes, mitochondria, DNA, and RNA.
- Role in immunological functions
- Involved in macrophage activation, adherence, and bactericidal activity of granulocyte oxidative burst, lymphocyte proliferation, and endotoxin binding to monocytes.
Magnesium is a cofactor (a compound that is essential for the activity of an enzyme) in more than 300 enzyme 96, 95. These include protein kinases which are commonly utilized to regulate gene transcription in response to extracellular stimuli 98. Magnesium is also required for the structure and functioning of DNA and RNA polymerases 99, 100. These DNA and RNA polymerases are not only involved in nucleic acid synthesis, but some are also involved in DNA repair and genome maintenance 32. Virtually all enzymes taking part in mismatch repair, nucleotide repair, and base excision repair use magnesium as a cofactor 32. Given that defects in genome maintenance pathways are considered a hallmark of many cancers, magnesium deficiency might contribute to oncogenesis (the process through which healthy cells become transformed into cancer cells) 101. Furthermore, magnesium deficiency has been shown to be associated with diverse pathologies including prediabetes, platelet hyper-reactivity, pre-eclampsia, heart attack (acute myocardial infarction) and even some therapies 22, 102, 103, 84.
In fact, magnesium is used as a primary ingredient in some laxatives 104. Phillips’ Milk of Magnesia®, for example, provides 500 mg elemental magnesium (as magnesium hydroxide) per tablespoon; the directions advise taking up to 4 tablespoons/day for adolescents and adults 105. Although such a dose of magnesium is well above the safe upper level, some of the magnesium is not absorbed because of the medication’s laxative effect. Magnesium is also included in some remedies for heartburn and upset stomach due to acid indigestion 104. Extra-strength Rolaids®, for example, provides 55 mg elemental magnesium (as magnesium hydroxide) per tablet, although Tums® is magnesium free.
Magnesium is also used for the treatment of pre-eclampsia and eclampsia 84, 91. Pre-eclampsia is a disorder of pregnancy characterized by hypertension and proteinuria. Eclampsia is the occurrence of one or more convulsions associated with pre-eclampsia. Magnesium sulfate is now the drug of choice for women with eclampsia and is better than antiepileptic drugs. The Magpie trial 106 was a randomized controlled trial comparing magnesium sulfate with a placebo for pre-eclampsia. The results demonstrated a reduction by about 50% in the risk of eclampsia in the pre-eclamptic women 106.
Figure 4. Magnesium function
Footnote: Magnesium has roles in many physiological processes
[Source 32 ]Figure 5. Magnesium role in many cellular processes
Footnote: Neuronal magnesium concentrations downregulate the excitability of the N-methyl-D-aspartate (NMDA) receptor, which is essential for excitatory synaptic transmission and neuronal plasticity in learning and memory 107. Magnesium blocks the calcium channel in the NMDA receptor and must be removed for glutamatergic excitatory signaling. Low serum magnesium levels increase NMDA receptor activity thus enhancing Ca2+ and Na+ influx and neuronal excitability. For these reasons, a deficiency of magnesium has been hypothesized in many neurological disorders, such as migraine, chronic pain, epilepsy, Alzheimer’s disease, Parkinson’s disease and stroke, as well as anxiety and depression 108.
[Source 41 ]Energy production
The metabolism of carbohydrates (sugars) and fats to produce energy requires numerous magnesium-dependent chemical reactions. Magnesium is required by the adenosine triphosphate (ATP)-synthesizing protein in mitochondria. ATP, the molecule that provides energy for almost all metabolic processes, exists primarily as a complex with magnesium (MgATP) 17.
Synthesis of essential molecules
Magnesium is required for a number of steps during synthesis of deoxyribonucleic acid (DNA), ribonucleic acid (RNA), and proteins. Several enzymes participating in the synthesis of carbohydrates and lipids require magnesium for their activity. Glutathione, an important antioxidant, requires magnesium for its synthesis 17.
Structural roles in bone, cell membranes, and chromosomes
Magnesium plays a structural role in bone, cell membranes, and chromosomes 17.
Ion transport across cell membranes
Magnesium is required for the active transport of ions like potassium and calcium across cell membranes. Through its role in ion transport systems, magnesium affects the conduction of nerve impulses, muscle contraction, and normal heart rhythm 17.
Cell signaling
Cell signaling requires Mg-ATP for the phosphorylation of proteins and the formation of the cell-signaling molecule, cyclic adenosine monophosphate (cAMP). cAMP is involved in many processes, including the secretion of parathyroid hormone (PTH) from the parathyroid glands 17.
Cell migration
Calcium and magnesium concentrations in the fluid surrounding cells affect the migration of a number of different cell types. Such effects on cell migration may be important in wound healing 17.
How much magnesium do I need?
The amount of magnesium you need depends on your age and sex. Average daily recommended magnesium amounts are listed below in milligrams (mg). Intake recommendations for magnesium and other nutrients are provided in the Dietary Reference Intakes (DRIs) developed by the Food and Nutrition Board (FNB) at the Institute of Medicine of the National Academies 43. Dietary Reference Intake (DRI) is the general term for a set of reference values used to plan and assess nutrient intakes of healthy people. These values, which vary by age and sex, include:
- Recommended Dietary Allowance (RDA): average daily level of intake sufficient to meet the nutrient requirements of nearly all (97%–98%) healthy individuals.
- Adequate Intake (AI): established when evidence is insufficient to develop an RDA and is set at a level assumed to ensure nutritional adequacy.
- Estimated Average Requirement (EAR): average daily level of intake estimated to meet the requirements of 50% of healthy individuals. It is usually used to assess the adequacy of nutrient intakes in population groups but not individuals.
- Tolerable Upper Intake Level (UL): maximum daily intake unlikely to cause adverse health effects.
Table 1 lists the current Recommended Dietary Allowances (RDAs) for magnesium 43. For infants from birth to 12 months, the Food and Nutrition Board established an Adequate Intake (AI) for magnesium that is equivalent to the mean intake of magnesium in healthy, breastfed infants, with added solid foods for ages 7–12 months.
As per the United States Food and Nutrition, Recommended Daily Allowance (RDA) of magnesium is 420 mg for males and 320 mg for females 43. Around 10% of magnesium is obtained through drinking water. Other sources of magnesium include green vegetables, unprocessed cereals, nuts, seeds, fish, meat, and milk products 57.
Too much magnesium from foods isn’t a concern for healthy adults. However, the same can’t be said for supplements. High doses of magnesium from supplements or medications can cause nausea, abdominal cramping and diarrhea. In addition, the magnesium in supplements can interact with some types of antibiotics and other medicines. Check with your doctor or pharmacist if you’re considering magnesium supplements, especially if you routinely use magnesium-containing antacids or laxatives.
Table 1. Recommended Dietary Allowances (RDAs) for Magnesium
| Life Stage | Recommended Amount |
|---|---|
| Birth to 6 months | 30 mg |
| Infants 7–12 months | 75 mg |
| Children 1–3 years | 80 mg |
| Children 4–8 years | 130 mg |
| Children 9–13 years | 240 mg |
| Teen boys 14–18 years | 410 mg |
| Teen girls 14–18 years | 360 mg |
| Men | 400–420 mg |
| Women | 310–320 mg |
| Pregnant teens | 400 mg |
| Pregnant women | 350–360 mg |
| Breastfeeding teens | 360 mg |
| Breastfeeding women | 310–320 mg |
Footnote: *Adequate Intake (AI) is the intake at this level is assumed to ensure nutritional adequacy; established when evidence is insufficient to develop an Recommended Dietary Allowance (RDA).
[Source 109 ]What foods provide Magnesium?
Magnesium is widely distributed in plant and animal foods and in beverages 110. Green leafy vegetables, such as spinach, legumes, nuts, seeds, and whole grains, are good sources of magnesium 43, 45. In general, foods containing dietary fiber provide magnesium. Magnesium is also added to some breakfast cereals and other fortified foods. Some types of food processing, such as refining grains in ways that remove the nutrient-rich germ and bran, lower magnesium content substantially 43. Selected food sources of magnesium are listed in Table 2.
You can get recommended amounts of magnesium by eating a variety of foods, including the following 50:
- Legumes, nuts, seeds, whole grains, and green leafy vegetables (such as spinach)
- Fortified breakfast cereals and other fortified foods
- Milk, yogurt, and some other milk products
Tap, mineral, and bottled waters can also be sources of magnesium, but the amount of magnesium in water varies by source and brand (ranging from 1 mg/L to more than 120 mg/L) 111.
Approximately 30% to 40% of the dietary magnesium consumed is typically absorbed by the body 44, 112.
The U.S. Department of Agriculture’s (USDA’s) FoodData Central (https://fdc.nal.usda.gov) lists the nutrient content of many foods and provides comprehensive list of foods containing magnesium arranged by nutrient content (https://ods.od.nih.gov/pubs/usdandb/Magnesium-Content.pdf) and by food name (https://ods.od.nih.gov/pubs/usdandb/Magnesium-Food.pdf).
Table 2. Magnesium Rich Foods
| Food | Milligrams (mg) per serving | Percent Daily Value (DV)* |
|---|---|---|
| Pumpkin seeds, roasted, 1 ounce | 156 | 37 |
| Chia seeds, 1 ounce | 111 | 26 |
| Almonds, dry roasted, 1 ounce | 80 | 19 |
| Spinach, boiled, ½ cup | 78 | 19 |
| Cashews, dry roasted, 1 ounce | 74 | 18 |
| Peanuts, oil roasted, ¼ cup | 63 | 15 |
| Cereal, shredded wheat, 2 large biscuits | 61 | 15 |
| Soymilk, plain or vanilla, 1 cup | 61 | 15 |
| Black beans, cooked, ½ cup | 60 | 14 |
| Edamame, shelled, cooked, ½ cup | 50 | 12 |
| Peanut butter, smooth, 2 tablespoons | 49 | 12 |
| Potato, baked with skin, 3.5 ounces | 43 | 10 |
| Rice, brown, cooked, ½ cup | 42 | 10 |
| Yogurt, plain, low fat, 8 ounces | 42 | 10 |
| Breakfast cereals, fortified with 10% of the DV for magnesium, 1 serving | 42 | 10 |
| Oatmeal, instant, 1 packet | 36 | 9 |
| Kidney beans, canned, ½ cup | 35 | 8 |
| Banana, 1 medium | 32 | 8 |
| Salmon, Atlantic, farmed, cooked, 3 ounces | 26 | 6 |
| Milk, 1 cup | 24–27 | 6 |
| Halibut, cooked, 3 ounces | 24 | 6 |
| Raisins, ½ cup | 23 | 5 |
| Bread, whole wheat, 1 slice | 23 | 5 |
| Avocado, cubed, ½ cup | 22 | 5 |
| Chicken breast, roasted, 3 ounces | 22 | 5 |
| Beef, ground, 90% lean, pan broiled, 3 ounces | 20 | 5 |
| Broccoli, chopped and cooked, ½ cup | 12 | 3 |
| Rice, white, cooked, ½ cup | 10 | 2 |
| Apple, 1 medium | 9 | 2 |
| Carrot, raw, 1 medium | 7 | 2 |
Footnote: *DV = Daily Value. Daily Values (DVs) were developed by the U.S. Food and Drug Administration (FDA) to help consumers compare the nutrient contents of products within the context of a total diet. The Daily Value (DV) for magnesium is 400 mg for adults and children aged 4 and older. However, the FDA does not require food labels to list magnesium content unless a food has been fortified with this nutrient. Foods providing 20% or more of the DV are considered to be high sources of a nutrient, but foods providing lower percentages of the DV also contribute to a healthful diet.
[Source 113 ]Magnesium deficiency causes
Magnesium deficiency causes include insufficient dietary supply, malabsorption, endocrine causes, renal disease, redistribution and intracellular shift of magnesium, medication use, or other factors such as chronic alcoholism or stress 30, 114:i3–i14. doi: 10.1093/ndtplus/sfr163)), 115.
Magnesium deficiency or hypomagnesemia can be secondary to decreased intake, as seen in the following 12, 116:
- Decreased intake. Several dietary surveys have shown that people in North America and Europe consume less than recommended daily allowance (RDA) for magnesium as a result of food processing and the use of poor soil for agriculture 49, 51, 117. Hypomagnesemia can also occur in times of prolonged fasting, total parenteral nutrition, or
- Starvation
- Alcohol use disorder (with a reported prevalence of 30%) 118
- Anorexia nervosa
- Terminal cancer
- Critically ill patients who are receiving total parenteral nutrition
- Prolonged nasogastric suctioning.
Magnesium deficiency or hypomagnesemia can also be secondary to the following medications 2, 119, 114:i3–i14. doi: 10.1093/ndtplus/sfr163)):
- Loop and thiazide diuretics
- Proton pump inhibitors
- Aminoglycoside antibiotics
- Amphotericin B
- Pentamidine
- Digitalis
- Tacrolimus
- Chemotherapeutic drugs, such as cisplatin, cyclosporine
- Antibodies that bind to epidermal growth factor (EGF) receptors (cetuximab, matuzumab, panitumumab)
- Laxative abuse
Magnesium deficiency or hypomagnesemia can also result from redistribution from the extracellular to the intracellular compartment 120, 115:
- Treatment of diabetic ketoacidosis by insulin
- Refeeding syndrome
- Correction of metabolic acidosis
- Acute pancreatitis
- Ethanol withdrawal syndrome
- Pregnancy
- Lactation
- Cardiopulmonary surgeries
Magnesium deficiency or hypomagnesemia can be induced by malabsorption or gastrointestinal disorders 30, 11:
- Crohn’s disease,
- Ulcerative colitis,
- Inflammatory bowel diseases,
- Malabsorption syndromes,
- Celiac disease,
- Short bowel syndrome,
- Whipple’s disease,
- Acute diarrhea
- Chronic diarrhea,
- Pancreatic insufficiency
- Acute pancreatitis
- Gastric bypass surgery
- Surgical removal of a portion of the small intestine
- Intestinal inflammation due to radiation.
Magnesium deficiency or hypomagnesemia can be induced by kidney losses 2, 11:
- Hungry bone syndrome (an increased magnesium uptake by renewing bone following parathyroidectomy or thyroidectomy, causing a decrease in serum magnesium)
- Genetic disorders 8
- Gitelman syndrome. Gitelman syndrome is caused by recessive mutations in the gene that codes for the thiazide-sensitive sodium chloride cotransporter (SLC12A3) in the distal convoluted tubule. Transcellular reabsorption of magnesium in the distal convoluted tubule is impaired, leading to increased calcium reabsorption and the subsequent hypocalciuria (low urine calcium) and fluid loss have the tendency to lower blood pressure. In addition, fluid loss activates the renin-angiotensin-aldosterone system, and increased aldosterone causes increased potassium secretion in exchange for sodium and subsequent hypokalemia (low blood potassium).
- Bartter syndrome
- Familial hypomagnesemia with hypercalciuria and nephrocalcinosis
- Hypercalciuric hypomagnesemias: Mutations affect the reabsorption of magnesium and calcium ions in the thick ascending limb of Henle, leading to hypercalciuric hypomagnesemia that ultimately results in nephrocalcinosis or chronic kidney disease.
- Renal malformations and early-onset diabetes mellitus caused by HNF1-beta mutation
- Autosomal recessive isolated hypomagnesemia caused by EGF mutation
- Autosomal dominant isolated hypomagnesemia caused by Na-K-ATPase gamma subunit, Kv1.1, and cyclin M2 mutations.
- Intestinal hypomagnesemia with secondary hypocalcemia
- EAST (SeSAME) syndrome. EAST (SeSAME) syndrome is caused by loss-of-function mutations in the gene encoding the potassium channel, KCNJ10 (Kir4.1), on the basolateral membrane of the distal convoluted tubule. It results in hypomagnesemia, salt wasting, metabolic alkalosis, and hypokalemia. The mechanism, however, is poorly understood 121.
- Acquired renal tubular dysfunction may result in increased urinary loss of magnesium 114:i3–i14. doi: 10.1093/ndtplus/sfr163)), 115:
- Post-kidney transplantation
- Recovery from acute tubular necrosis
- Postobstructive diuresis
- Chronic renal failure
- Dialysis
- Excessive volume expansion
- Chronic metabolic acidosis
- Diabetes mellitus
- Long-term use of certain diuretics
Magnesium deficiency or hypomagnesemia due to endocrine disorders 114:i3–i14. doi: 10.1093/ndtplus/sfr163)), 30:
- Aldosteronism,
- Hyperparathyroidism,
- Hyperthyroidism,
- Poorly-controlled diabetes
Other causes
Poor dietary intake, gastrointestinal problems, and increased urinary loss of magnesium may all contribute to magnesium depletion in people suffering from alcoholism. Older adults have relatively low dietary intakes of magnesium 61, 60. Intestinal magnesium absorption tends to decrease with age, and urinary magnesium excretion tends to increase with age; therefore, suboptimal dietary magnesium intake may increase the risk of magnesium depletion in the elderly 62.
Groups at risk of magnesium deficiency
The following groups of people are more likely than others to get too little magnesium:
- People with gastrointestinal diseases (such as Crohn’s disease and celiac disease)
- People with type 2 diabetes
- People with long-term alcoholism
- Older people
Magnesium inadequacy can occur when intakes fall below the RDA but are above the amount required to prevent overt deficiency. The following groups are more likely than others to be at risk of magnesium inadequacy because they typically consume insufficient amounts or they have medical conditions (or take medications) that reduce magnesium absorption from the gut or increase losses from the body.
People with gastrointestinal diseases
The chronic diarrhea and fat malabsorption resulting from Crohn’s disease, gluten-sensitive enteropathy (celiac disease), and regional enteritis can lead to magnesium depletion over time 44. Resection or bypass of the small intestine, especially the ileum, typically leads to malabsorption and magnesium loss 44.
People with type 2 diabetes
Magnesium deficits and increased urinary magnesium excretion can occur in people with insulin resistance and/or type 2 diabetes 122. The magnesium loss appears to be secondary to higher concentrations of glucose in the kidney that increase urine output 44.
People with alcohol dependence
Magnesium deficiency is common in people with chronic alcoholism 44. In these individuals, poor dietary intake and nutritional status; gastrointestinal problems, including vomiting, diarrhea, and steatorrhea (fatty stools) resulting from pancreatitis; renal dysfunction with excess excretion of magnesium into the urine; phosphate depletion; vitamin D deficiency; acute alcoholic ketoacidosis; and hyperaldosteronism secondary to liver disease can all contribute to decreased magnesium status 44.
Older adults
Older adults have lower dietary intakes of magnesium than younger adults 123. In addition, magnesium absorption from the gut decreases and renal magnesium excretion increases with age 124. Older adults are also more likely to have chronic diseases or take medications that alter magnesium status, which can increase their risk of magnesium depletion 125.
Magnesium deficiency prevention
It is important to consume an adequate amount of magnesium through diet. The good sources of magnesium include green vegetables, nuts, seeds, unprocessed cereals, and dark chocolate (Table 2). A lower concentration of magnesium is present in fruits, meat, fish, and dairy products. Drinking water supplies about 10% of daily magnesium intake 114:i3–i14. doi: 10.1093/ndtplus/sfr163)). It is worth adding that dietary factors such as lactose, fructose, or glucose can enhance magnesium absorption, while a high intake of zinc, fiber, free fatty acids, oxalate, or phytate can cause its decrease 126.
Magnesium deficiency signs and symptoms
The clinical signs and symptoms of magnesium deficiency or hypomagnesemia are often non-specific 10. The major signs and symptoms of low magnesium or magnesium deficiency include neuromuscular and cardiovascular manifestations and other electrolyte abnormalities. Early signs of magnesium deficiency may be fatigue, weakness, loss of appetite, nausea, or vomiting. As magnesium deficiency worsens, the next symptoms may include tremors, agitation and muscle fasciculation, cramps, seizures, cardiac arrhythmia, ventricular tachycardia, personality changes, or depression 127. In addition, clinical symptoms of hypomagnesemia are often correlated with a rapid decrease in magnesium levels compared to a gradual change. Hypomagnesemia is frequently accompanied by other electrolyte abnormalities, especially hypokalemia and hypocalcemia. Thus, the diagnosis of magnesium deficiency should be supported by laboratory determinations of other macroelements, i.a., calcium, potassium, or phosphorus 128:i15–i24. doi: 10.1093/ndtplus/sfr164)). The impact of chronic magnesium deficiency is shown is Figure 6.
Magnesium deficiency or low magnesium common symptoms include 7:
- Abnormal eye movements (nystagmus)
- Convulsions
- Fatigue
- Muscle spasms or cramps
- Muscle weakness
- Numbness
Early presentation of low magnesium or hypomagnesemia includes nausea, vomiting, loss of appetite, fatigue, and weakness 12. Patients may complain of dysphagia, muscular weakness, and other symptoms as described below 120. A case report describes symptoms of cerebellar ataxia, generalized convulsions, intermittent downbeat nystagmus, and supraventricular tachycardia in a 59-year-old man with severe hypomagnesemia 129.
Figure 6. Chronic magnesium depletion consequences
[Source 10 ]Neuromuscular signs and symptoms
- Neuromuscular hyperexcitability (often the first clinical manifestation) 38
- Tremors
- Tetany, including positive Trousseau and Chvostek signs, muscle spasms, and muscle cramps. It may occur in the absence of hypocalcemia and alkalosis and is thought to be due to the lowering of the threshold for nerve stimulation 130.
- Choreoathetosis 131
- Seizures
- Vertical nystagmus
- Apathy
- Delirium
- Depression
- Agitation
- Psychosis
- Delirium
- Coma
Cardiovascular signs and symptoms
- Electrocardiogram (ECG) changes, including widening of the QRS complex, peaked T waves (with mild to moderate deficiency), prolongation of the PR interval, and diminution of the T wave (with severe deficiency) 132
- Atrial and ventricular premature systoles
- Atrial fibrillation (AF)
- Ventricular arrhythmias, including torsades de pointes
- Cardiac ischemia
- Increased risk of digoxin toxicity by inhibiting Na-K-ATPase and depleting intracellular potassium 133
- Hypertension. Low dietary magnesium and hypomagnesemia might be a contributing factor in the pathophysiology of hypertension. Magnesium reduces vascular tone and resistance by enhancing vasodilator effect of nitric oxide, antagonizing the vasoconstrictor effect of calcium, bradykinin, angiotensin 2, serotonin, and prostaglandin in F2α, and protecting the vascular endothelium through its antioxidant effect 134. Several clinical trials have been conducted to study the effect of magnesium supplementation on the blood pressure, and at present, there is no strong evidence to support the use of magnesium supplementation in the routine management of hypertension 48, 135.
Other Electrolyte and Hormone Abnormalities
- Hypocalcemia
- Symptoms typically occur at magnesium levels below 0.5 mmol/L or 1.22 mg/dL.
- Milder hypomagnesemia (between 0.55 mmol/L and 0.65 mmol/L) lowers the plasma calcium concentration only slightly (0.2 mg/dL or 0.05 mmol/L) 136
- Hypoparathyroidism
- Hypokalemia (about 60% of cases).
Magnesium deficiency complications
Dangerously low levels of magnesium have the potential to cause fatal cardiac arrhythmias, such as torsades de pointes (polymorphous ventricular tachycardia with marked QT prolongation) 1. Moreover, hypomagnesemia in patients with heart attack (acute myocardial infarction) puts them at a higher risk of ventricular arrhythmias within the first 24 hours. Moreover, it may also cause chondrocalcinosis 8.
Magnesium deficiency diagnosis
Your health care provider will do a physical exam and ask about your symptoms.
History may include the causes adn symptoms mentioned above.
On examination, vertical nystagmus and tetany may be observed. The following signs can be checked:
- Chvostek sign: Tapping on facial nerve leads to twitching of facial muscles
- Trousseau sign: Carpopedal spasm induced by inflated blood pressure cuff
Tests that may be ordered include blood tests, urine tests and an electrocardiogram (ECG) to rule out arrhythmias.
Blood and urine tests that may be done include:
- Calcium blood test
- Comprehensive metabolic panel
- Potassium blood test
- Urine magnesium test
- Genetic testing may be considered if there is positive family history, unexplained hypomagnesemia, or if discovered early in infancy.
The diagnosis of magnesium deficiency or low magnesium is challenging 26, because magnesium serum concentration does not reflect the total content in the human body 27. You may have a “normal” serum magnesium concentration (0.7–1 mmol/L or 1.7–2.4 mg/dL) 28, but have relatively low levels of skeletal or cellular magnesium 29. Up till now, no single reliable indicator of magnesium deficiency is considered satisfactory 26. The difficulties of accessing total body magnesium concentration concerns its main two compartments, namely bone and muscle, while in blood it is present only in very small amounts (less than 1%) 30, 10, 31. It is possible that an individual can be in a magnesium-depleted state but have plasma or serum values within the “normal” range 32. Consequently, the clinical impact of magnesium deficiency may be underestimated. In plasma, the concentration of free magnesium is reported to be ~0.6 mmol/L (~14 mg/L) 33, with about 30% complexed by proteins 34. The major magnesium binding protein in plasma is serum albumin 35, 33.
In clinical practice, the total serum or plasma magnesium concentration is the most commonly used test to assess the magnesium status, and the normal reference range is usually 0.7–1 mmol/L (1.7–2.43 mg/dL) 28, 36. Plasma magnesium concentrations are closely related to bone metabolism, as there is continuous exchange between the skeleton and blood 37. However, the normal value varies from laboratory to laboratory, and different studies have used slightly different ranges. This may partially explain the differences in the prevalence of magnesium imbalances reported in different groups of patients with similar characteristics 12.
Normal serum magnesium does not necessarily mean adequate content of total body magnesium because only less than 0.3% of total body magnesium is found in serum 12. Serum magnesium is in most places not part of routine blood tests, and it should be assessed in the relevant clinical conditions such as arrhythmia, low blood potassium (hypokalemia), low blood calcium (hypocalcemia), diarrhea, and chronic alcoholism that tend to be associated with magnesium derangement 97. Serum magnesium test is also recommended if the patient is critically ill or when being administered certain medications known to cause hypomagnesemia. Table 3 lists other more accurate but lesser used measures of assessing magnesium status 49, 137.
The magnesium loading test also known as the magnesium retention test is considered to be the gold standard for measuring magnesium status, which basically determines magnesium retention using 24-hour urine collection following the intravenous administration of magnesium 3. A magnesium deficiency is indicated if a patient has <80% excretion (over 24 hours) of an infused magnesium load (2.4 mg/kg of lean body weight given over the initial 4 hours) 138, 139. Despite the magnesium loading test or magnesium retention test is a good indicator of magnesium deficiency or hypomagnesemia in adults, it appears to be poorly sensitive to changes in magnesium status in healthy people. Moreover, the magnesium loading test or magnesium retention test is invasive and cumbersome, and thus difficult to use routinely 140.
Additional tests for magnesium deficiency involve measuring the magnesium/creatinine ratio in spot urine or in 24 hour urine collections 29. It is also possible to directly measure magnesium in the urine; this can be used to gain insight into kidney functioning and magnesium wasting. A 24 hour urinary magnesium level of > 24 mg is indicative of magnesium wasting 141. Another method to assess magnesium status is through measurements of plasma ionized magnesium, which represents the physiologically active form of magnesium. However, it is unknown whether plasma ionized magnesium reflect body stores 140.
In practice, magnesium status is usually determined through assessments of dietary magnesium intake, serum magnesium concentration, and/or urinary magnesium concentration 140. However, each of these indicators has limitations. Although predominantly used in epidemiological studies and the sole indicator available to clinicians, serum magnesium concentration has been found to poorly respond to magnesium supplementation 42. Regarding dietary intakes of magnesium, about 30 to 40% of ingested magnesium is absorbed, yet absorption varies with the amount of magnesium ingested and with the food matrix composition 42. Finally, a state of magnesium deficiency has not been associated to a clear cutoff concentration of magnesium in the urine 42. Urinary magnesium concentration fluctuates rapidly with dietary intakes, but measurements of 24-hour urinary magnesium can be used in addition to other indicators to assess population status. Presently, a combination of all three markers — dietary, serum, and urinary magnesium — may be used to get a valid assessment of magnesium status 140.
For differentiating hypomagnesemia of renal origin from intestinal hypomagnesemia is determination of the fractional excretion of magnesium (FEMg) 142, which can be calculated with the following formula 8:
- Fractional excretion of magnesium (FEMg) = [([Mg2+]urine × [creatinine]plasma)/ (0.7 [Mg2+]plasma × [creatinine]urine)] × 100 %
Note: The factor of 0.7 is included to adjust the total plasma magnesium concentration to the freely filtered fraction.
A fractional excretion of magnesium (FEMg) of >4 % in a hypomagnesemic patient is consistent with renal magnesium wasting, while a patient with a FEMg of <2 % will likely have an extra-renal origin of their hypomagnesemia 142. However, a FEMg <4 % does not rule out renal magnesium wasting. First, a low glomerular filtration rate (GFR) may result in a lower filtered load of magnesium. If the absorptive capacity of the kidney for magnesium is sufficient to cope with this lower load, the result may be a normal or even low FEMg. By the same mechanism, severe (renal) hypomagnesemia may result in a lower filtered load of magnesium and thus a normal or low FEMg. To account for these confounding factors, the serum magnesium levels of hypomagnesemic patients should be increased by means of intravenous magnesium supplementation before the FEMg is measured 143.
Table 3. Assessment of magnesium status
| Test | Comments |
|---|---|
| Serum magnesium | Sometimes not adequate since less than 0.3% of total body magnesium is found in serum. However, it is easy, accessible, and cheap. |
| 24 hours excretion in urine or the fractional excretion of magnesium | Helps in differentiating renal wasting of magnesium from inadequate intake or poor absorption as an etiology for hypomagnesemia. |
| Magnesium loading test | Identifies patients with normomagnesic magnesium deficiency. |
| Assesses intestinal absorption of magnesium. | |
| Indirectly assesses bone status of magnesium. | |
| Magnesium concentration in red blood cell counts | Can give early indication of magnesium deficiency. |
| Isotopic analysis of magnesium | Assesses the absorption of magnesium from the gastrointestinal tract in research setting. |
| Ionized magnesium | More accurate, especially in critically ill patients with rapid change in hemodynamics. |
| Not effected by low albumin. | |
Magnesium deficiency treatment
Treatment depends on the type of low magnesium problem you have and may include:
- Fluids given through a vein (IV)
- Magnesium by mouth or through a vein
- Medicines to relieve symptoms.
The treatment of patients with hypomagnesemia is based on a patient’s kidney function, the severity of their symptoms, and hemodynamic stability 1. If a patient is hemodynamically unstable in an acute hospital setting, 1 to 2 grams of magnesium sulfate can be given in about 15 minutes 1. For symptomatic, severe hypomagnesemia in a stable patient, 1 to 2 grams of magnesium sulfate can be given over one hour 1. Non-emergent repletion of magnesium in adult patient is generally 4 to 8 grams of magnesium sulfate given slowly over 12 to 24 hours 1. In children patients, the magnesium sulfate dose is 25 to 50 mg/kg (with a maximum of 2 grams) 38, 39.
For an asymptomatic patient with hypomagnesemia who is not hospitalized and can tolerate medications by mouth, sustained-release oral replacement should be tried first. Asymptomatic patients with hypomagnesemia can benefit from oral sustained-release magnesium preparations (magnesium chloride containing 64-71.5 mg or magnesium L-lactate containing 84 mg elemental magnesium) 1. After repletion, serum electrolyte levels must be rechecked (whether in an inpatient or outpatient setting) to ensure effective treatment. Although serum magnesium levels rise quickly with treatment, intracellular magnesium takes longer to replete. Therefore, patients with normal kidney function should try to continue magnesium repletion for two days after the level normalizes 1.
Use caution in repleting magnesium in patients with abnormal kidney function (defined as creatinine clearance less than 30 mL/min/1.73 m²) 1. These patients are at risk of hypermagnesemia (too much magnesium). Studies recommend reducing the magnesium dose by 50% and closely monitoring magnesium levels in these patients 1.
Magnesium deficiency prognosis
Magnesium deficiency prognosis or outcome depends on the condition that is causing the low magnesium. Patients with low magnesium or hypomagnesemia from an identifiable cause have a good prognosis for complete recovery 1. However, in critically ill patients, low magnesium or hypomagnesemia is associated with higher mortality, the need of mechanical ventilation and increased length of ICU stay in patients admitted to ICU 144.
References- Gragossian A, Bashir K, Bhutta BS, et al. Hypomagnesemia. [Updated 2022 Nov 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK500003
- Ayuk J, Gittoes NJ. How should hypomagnesaemia be investigated and treated? Clin Endocrinol (Oxf). 2011 Dec;75(6):743-6. doi: 10.1111/j.1365-2265.2011.04092.x
- Volpe SL. Magnesium. In: Erdman Jr. JW, Macdonald IA, Ziegler EE, eds. Present Knowledge in Nutrition. 10th ed: ILSI Press; 2012:459-474.
- Nielsen FH. Magnesium deficiency and increased inflammation: current perspectives. J Inflamm Res. 2018 Jan 18;11:25-34. doi: 10.2147/JIR.S136742
- Kim E. Pathogenesis and treatment of electrolyte problems post transplant. Curr Opin Pediatr. 2019 Apr;31(2):213-218. doi: 10.1097/MOP.0000000000000715
- Fulchiero R, Seo-Mayer P. Bartter Syndrome and Gitelman Syndrome. Pediatr Clin North Am. 2019 Feb;66(1):121-134. doi: 10.1016/j.pcl.2018.08.010
- Magnesium deficiency. https://medlineplus.gov/ency/article/000315.htm
- Viering DHHM, de Baaij JHF, Walsh SB, Kleta R, Bockenhauer D. Genetic causes of hypomagnesemia, a clinical overview. Pediatr Nephrol. 2017 Jul;32(7):1123-1135. doi: 10.1007/s00467-016-3416-3
- Mathew AA, Panonnummal R. ‘Magnesium’-the master cation-as a drug-possibilities and evidences. Biometals. 2021 Oct;34(5):955-986. doi: 10.1007/s10534-021-00328-7
- Al Alawi AM, Majoni SW, Falhammar H. Magnesium and Human Health: Perspectives and Research Directions. Int J Endocrinol. 2018 Apr 16;2018:9041694. doi: 10.1155/2018/9041694
- Pham P. C., Pham P. A., Pham S. V., Pham P. T., Pham P. M., Pham P. T. Hypomagnesemia: a clinical perspective. International Journal of Nephrology and Renovascular Disease. 2014;7:219–230. doi: 10.2147/ijnrd.s42054
- Jahnen-Dechent W., Ketteler M. Magnesium basics. Clinical Kidney Journal. 2012;5(Supplement 1):i3–i14. doi: 10.1093/ndtplus/sfr163
- Martin K. J., Gonzalez E. A., Slatopolsky E. Clinical consequences and management of hypomagnesemia. Journal of American Society of Nephrology. 2009;20(11):2291–2295. doi: 10.1681/ASN.2007111194
- Andreozzi F, Cuminetti G, Karmali R, Kamgang P. Electrolyte Disorders as Triggers for Takotsubo Cardiomyopathy. Eur J Case Rep Intern Med. 2018 Apr 24;5(4):000760. doi: 10.12890/2018_000760
- Kurstjens S, Bouras H, Overmars-Bos C, Kebieche M, Bindels RJM, Hoenderop JGJ, de Baaij JHF. Diabetes-induced hypomagnesemia is not modulated by metformin treatment in mice. Sci Rep. 2019 Feb 11;9(1):1770. doi: 10.1038/s41598-018-38351-3
- Brophy C, Woods R, Murphy MS, Sheahan P. Perioperative magnesium levels in total thyroidectomy and relationship to hypocalcemia. Head Neck. 2019 Jun;41(6):1713-1718. doi: 10.1002/hed.25644
- Rude RK, Shils ME. Magnesium. In: Shils ME, Shike M, Ross AC, Caballero B, Cousins RJ, eds. Modern Nutrition in Health and Disease. 10th ed. Baltimore: Lippincott Williams & Wilkins; 2006:223-247.
- Schlegel RN, Cuffe JS, Moritz KM, Paravicini TM. Maternal hypomagnesemia causes placental abnormalities and fetal and postnatal mortality. Placenta. 2015;36:750–758. doi: 10.1016/j.placenta.2015.03.011
- Hall DG. Serum magnesium in pregnancy. Obstet Gynecol. 1957;9:158–162. doi: 10.1097/00006250-195706000-00019
- Kolisek M, Galaviz-Hernández C, Vázquez-Alaniz F, Sponder G, Javaid S, Kurth K, Nestler A, Rodríguez-Moran M, Verlohren S, Guerrero-Romero F, Aschenbach JR, Vormann J. SLC41A1 is the only magnesium responsive gene significantly overexpressed in placentas of preeclamptic women. Hypertens Pregnancy. 2013 Nov;32(4):378-89. doi: 10.3109/10641955.2013.810237
- de Baaij JH, Hoenderop JG, Bindels RJ. Magnesium in man: implications for health and disease. Physiol Rev. 2015;95:1–46. doi: 10.1152/physrev.00012.2014
- Mousavi E., Ghoreishy S., Hemmati S.M., Mohammadi A. Association between Magnesium Concentrations and Prediabetes: A Systematic Review and Meta-Analysis. Sci. Rep. 2021;11:24388. doi: 10.1038/s41598-021-03915-3
- Agus ZS. Mechanisms and causes of hypomagnesemia. Curr Opin Nephrol Hypertens. 2016 Jul;25(4):301-7. doi: 10.1097/MNH.0000000000000238
- Cheungpasitporn W, Thongprayoon C, Qian Q. Dysmagnesemia in Hospitalized Patients: Prevalence and Prognostic Importance. Mayo Clin Proc. 2015 Aug;90(8):1001-10. doi: 10.1016/j.mayocp.2015.04.023
- De Marchi S, Cecchin E, Basile A, Bertotti A, Nardini R, Bartoli E. Renal tubular dysfunction in chronic alcohol abuse–effects of abstinence. N Engl J Med. 1993 Dec 23;329(26):1927-34. doi: 10.1056/NEJM199312233292605
- Pelczyńska M, Moszak M, Bogdański P. The Role of Magnesium in the Pathogenesis of Metabolic Disorders. Nutrients. 2022 Apr 20;14(9):1714. doi: 10.3390/nu14091714
- Workinger J.L., Doyle R.P., Bortz J. Challenges in the Diagnosis of Magnesium Status. Nutrients. 2018;10:1202. doi: 10.3390/nu10091202
- Williamson M. A., Snyder L. M., Wallach J. B. Wallach’s Interpretation of Diagnostic Tests. 9th. Philadelphia, PA, USA: Wolters Kluwer/Lippincott Williams & Wilkins; 2011. xvi, 1143.
- Ismail A.A.A., Ismail Y., Ismail A.A. Chronic magnesium deficiency and human disease; time for reappraisal? QJM. 2018;111:759–763. doi: 10.1093/qjmed/hcx186
- Gröber U., Schmidt J., Kisters K. Magnesium in Prevention and Therapy. Nutrients. 2015;7:8199–8226. doi: 10.3390/nu7095388
- Tibbetts D.M., Aub J.C. Magnesium metabolism in health and disease. I. the magnesium and calcium excretion of normal individuals, also the effects of magnesium, chloride, and phosphate ions. J. Clin. Investig. 1937;16:491–501. doi: 10.1172/JCI100874
- Fritzen R, Davies A, Veenhuizen M, Campbell M, Pitt SJ, Ajjan RA, Stewart AJ. Magnesium Deficiency and Cardiometabolic Disease. Nutrients. 2023 May 17;15(10):2355. doi: 10.3390/nu15102355
- Deng B., Li X., Zhu P., Xu X., Xu Q., Kang Y. Speciation of magnesium in rat plasma using capillary electrophoresis-inductively coupled plasma-atomic emission spectrometry. Electrophoresis. 2008;29:1534–1539. doi: 10.1002/elps.200700423
- WALSER M. Ion association. VI. Interactions between calcium, magnesium, inorganic phosphate, citrate and protein in normal human plasma. J Clin Invest. 1961 Apr;40(4):723-30. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC373170/pdf/jcinvest00303-0131.pdf
- Peters T., Jr. All about Albumin: Biochemistry, Genetics, and Medical Applications. Academic Press; New York, NY, USA: 1995.
- Ryan M.F. The role of magnesium in clinical biochemistry: An overview. Ann. Clin. Biochem. 1991;28:19–26. doi: 10.1177/000456329102800103
- Alfrey A.C., Miller N.L., Trow R. Effect of age and magnesium depletion on bone magnesium pools in rats. J. Clin. Investig. 1974;54:1074–1081. doi: 10.1172/JCI107851
- Hansen BA, Bruserud Ø. Hypomagnesemia in critically ill patients. J Intensive Care. 2018 Mar 27;6:21. doi: 10.1186/s40560-018-0291-y
- Greco DS. Endocrine causes of calcium disorders. Top Companion Anim Med. 2012 Nov;27(4):150-5. doi: 10.1053/j.tcam.2012.11.001
- National Institutes of Health. Magnesium. https://ods.od.nih.gov/factsheets/Magnesium-HealthProfessional/
- Fiorentini D, Cappadone C, Farruggia G, Prata C. Magnesium: Biochemistry, Nutrition, Detection, and Social Impact of Diseases Linked to Its Deficiency. Nutrients. 2021 Mar 30;13(4):1136. doi: 10.3390/nu13041136
- Magnesium. https://lpi.oregonstate.edu/mic/minerals/magnesium
- Institute of Medicine (IOM). Food and Nutrition Board. Dietary Reference Intakes: Calcium, Phosphorus, Magnesium, Vitamin D and Fluoride. Washington, DC: National Academy Press, 1997.
- Rude RK. Magnesium. In: Coates PM, Betz JM, Blackman MR, Cragg GM, Levine M, Moss J, White JD, eds. Encyclopedia of Dietary Supplements. 2nd ed. New York, NY: Informa Healthcare; 2010:527-37.
- Rude RK. Magnesium. In: Ross AC, Caballero B, Cousins RJ, Tucker KL, Ziegler TR, eds. Modern Nutrition in Health and Disease. 11th ed. Baltimore, Mass: Lippincott Williams & Wilkins; 2012:159-75.
- Pham PCT, Pham PAT, Pham SV, Pham PTT, Pham PMT, Pham PTT. Hypomagnesemia: a clinical perspective. Int J Nephrol Renovasc Dis. 2014 doi: 10.2147/IJNRD.S42054
- Bharadwaj J, Darbari A, Naithani M. Magnesium: the fifth electrolyte. J Med Nutr Nutraceuticals. 2014;3:186. doi: 10.4103/2278-019x.131955
- de Baaij J. H. F., Hoenderop J. G. J., Bindels R. J. M. Magnesium in man: implications for health and disease. Physiological Reviews. 2015;95(1):1–46. doi: 10.1152/physrev.00012.2014
- Grober U., Schmidt J., Kisters K. Magnesium in prevention and therapy. Nutrients. 2015;7(9):8199–8226. doi: 10.3390/nu7095388
- Magnesium. https://ods.od.nih.gov/factsheets/Magnesium-Consumer
- Olza J., Aranceta-Bartrina J., Gonzalez-Gross M., et al. Reported dietary intake, disparity between the reported consumption and the level needed for adequacy and food sources of calcium, phosphorus, magnesium and vitamin D in the Spanish population: findings from the ANIBES study † Nutrients. 2017;9(2) doi: 10.3390/nu9020168
- Moshfegh A, Goldman JD, Ahuja J, Rhodes D, LaComb R. What we eat in America, NHANES 2005–2006: usual nutrient intakes from food and water compared to 1997 Dietary Reference Intakes for vitamin D, calcium, phosphorus, and magnesium. Washington (DC): USDA; 2009.
- Costello RB, Elin RJ, Rosanoff A, Wallace TC, Guerrero-Romero F, Hruby A, Lutsey PL, Nielsen FH, Rodriguez-Moran M, Song Y, Van Horn LV. Perspective: The Case for an Evidence-Based Reference Interval for Serum Magnesium: The Time Has Come. Adv Nutr. 2016 Nov 15;7(6):977-993. doi: 10.3945/an.116.012765
- US Department of Health and Human Services. Scientific report of the 2015 Dietary Guidelines Advisory Committee. https://health.gov/our-work/nutrition-physical-activity/dietary-guidelines/previous-dietary-guidelines/2015/advisory-report
- European Food Safety Authority. Scientific opinion on dietary reference values for magnesium. EFSA J 2015;13:4186.
- Jahnen-Dechent W., Ketteler M. Magnesium basics. Clin. Kidney J. 2012;5:i3–i14. doi: 10.1093/ndtplus/sfr163
- Alexander RT, Hoenderop JG, Bindels RJ. Molecular determinants of magnesium homeostasis: insights from human disease. J Am Soc Nephrol. 2008;19:1451–1458. doi: 10.1681/ASN.2008010098
- Gröber U. Magnesium and Drugs. Int. J. Mol. Sci. 2019;20:2094. doi: 10.3390/ijms20092094
- Ahmed F, Mohammed A. Magnesium: the forgotten electrolyte—a review on hypomagnesemia. Med Sci. 2019;7:56. doi: 10.3390/medsci7040056
- Moshfegh A, Goldman J, Ahuja J, Rhodes D, LaComb R. What We Eat in America, NHANES 2005-2006: Usual Nutrient Intakes from Food and Water Compared to 1997 Dietary Reference Intakes for Vitamin D, Calcium, Phosphorus, and Magnesium. 2009. https://www.ars.usda.gov/ARSUserFiles/80400530/pdf/0506/usual_nutrient_intake_vitD_ca_phos_mg_2005-06.pdf
- Sebastian RS, Cleveland LE, Goldman JD, Moshfegh AJ. Older adults who use vitamin/mineral supplements differ from nonusers in nutrient intake adequacy and dietary attitudes. J Am Diet Assoc. 2007 Aug;107(8):1322-32. doi: 10.1016/j.jada.2007.05.010
- Food and Nutrition Board, Institute of Medicine. Magnesium. Dietary Reference Intakes: Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. Washington, D.C.: National Academy Press; 1997:190-249. https://nap.nationalacademies.org/read/5776/chapter/8
- Rude RK. Magnesium. In: Ross AC, Caballero B, Cousins RJ, Tucker KL, Ziegler TR, eds. Modern Nutrition in Health and Disease. 11th ed. China: Williams & Wilkins; 2014:159-175.
- Magnesium Blood Test. https://medlineplus.gov/lab-tests/magnesium-blood-test
- Cascella M, Vaqar S. Hypermagnesemia. [Updated 2023 May 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK549811
- Volpe SL. Magnesium. In: Erdman JW, Macdonald IA, Zeisel SH, eds. Present Knowledge in Nutrition. 10th ed. Ames, Iowa; John Wiley & Sons, 2012:459-74.
- Schuchardt J.P., Hahn A. Intestinal Absorption and Factors Influencing Bioavailability of Magnesium-An Update. Curr. Nutr. Food Sci. 2017;13:260–278. doi: 10.2174/1573401313666170427162740
- Groenestege W. M., Hoenderop J. G., van den Heuvel L., Knoers N., Bindels R. J. The epithelial Mg2+ channel transient receptor potential melastatin 6 is regulated by dietary Mg2+ content and estrogens. Journal of the American Society of Nephrology. 2006;17(4):1035–1043. doi: 10.1681/ASN.2005070700
- Quamme GA. Control of magnesium transport in the thick ascending limb. Am J Physiol. 1989 Feb;256(2 Pt 2):F197-210. doi: 10.1152/ajprenal.1989.256.2.F197
- Musso CG. Magnesium metabolism in health and disease. Int Urol Nephrol. 2009;41(2):357-62. doi: 10.1007/s11255-009-9548-7
- Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. Washington (DC): National Academies Press (US); 1997. Available from: https://www.ncbi.nlm.nih.gov/books/NBK109825/ doi: 10.17226/5776
- Ismail A.A.A., Ismail Y., Ismail A.A. Chronic magnesium deficiency and human disease; time for reappraisal? QJM. 2018;111:759–763. doi: 10.1093/qjmed/hcx186
- Rude R. Magnesium disorders. In: Kokko J., Tannen R., editors. Fluids and Electrolytes. W.B. Saunders Company; Philadelphia, PA, USA: 1996. pp. 421–445.
- Rosanoff A., West C., Elin R., Micke O., Baniasadi S., Barbagallo M., Campbell E., Cheng F.C., Costello R.B., Gamboa-Gomez C., et al. Recommendation on an updated standardization of serum magnesium reference ranges. Eur. J. Nutr. 2022;61:3697–3706. doi: 10.1007/s00394-022-02916-w
- Elin RJ. Assessment of magnesium status for diagnosis and therapy. Magnes Res. 2010 Dec;23(4):S194-8. doi: 10.1684/mrh.2010.0213
- Bertinato J., Wang K.C., Hayward S. Serum magnesium concentrations in the Canadian population and associations with diabetes, glycemic regulation, and insulin resistance. Nutrients. 2017;9:296. doi: 10.3390/nu9030296
- Witkowski M., Hubert J., Mazur A. Methods of assessment of magnesium status in humans: A systematic review. Magnes. Res. 2011;24:163–180. doi: 10.1684/mrh.2011.0292
- Gröber U., Schmidt J., Kisters K. Magnesium in Prevention and Therapy. Nutrients. 2015;7:8199–8226. doi: 10.3390/nu7095388
- Gibson, RS. Principles of Nutritional Assessment, 2nd ed. New York, NY: Oxford University Press, 2005.
- Micke O, Vormann J, Kraus A, Kisters K. Serum magnesium: time for a standardized and evidence-based reference range. Magnes Res. 2021 May 1;34(2):84-89. doi: 10.1684/mrh.2021.0486
- Razzaque M.S. Magnesium: Are we consuming enough? Nutrients. 2018;10:1863. doi: 10.3390/nu10121863
- Hypermagnesemia. https://emedicine.medscape.com/article/246489-overview
- Witkowski M, Hubert J, Mazur A. Methods of assessment of magnesium status in humans: a systematic review. Magnes Res. 2011 Dec;24(4):163-80. doi: 10.1684/mrh.2011.0292
- Abad C., Vargas F. R., Zoltan T., et al. Magnesium sulfate affords protection against oxidative damage during severe preeclampsia. Placenta. 2015;36(2):179–185. doi: 10.1016/j.placenta.2014.11.008
- Dolati S, Rikhtegar R, Mehdizadeh A, Yousefi M. The role of magnesium in pathophysiology and migraine treatment. Biol Trace Elem Res. 2019 doi: 10.1007/s12011-019-01931-z
- Gröber U, Schmidt J, Kisters K. Magnesium in prevention and therapy. Nutrients. 2015;7:8199–8226. doi: 10.3390/nu7095388
- DiNicolantonio JJ, O’Keefe JH, Wilson W. Subclinical magnesium deficiency: a principal driver of cardiovascular disease and a public health crisis. Open Hear. 2018 doi: 10.1136/openhrt-2017-000668
- Li X, Han X, Yang J, Bao J, Di X, Zhang G, Liu H. Magnesium sulfate provides neuroprotection in eclampsia-like seizure model by ameliorating neuroinflammation and brain edema. Mol Neurobiol. 2017;54:7938–7948. doi: 10.1007/s12035-016-0278-4
- Euser AG, Cipolla MJ. Magnesium sulfate for the treatment of eclampsia: a brief review. Stroke. 2009;40:1169–1175. doi: 10.1161/STROKEAHA.108.527788
- EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies), 2015. Scientific Opinion on Dietary Reference Values for magnesium. EFSA Journal 2015; 13( 7):4186, 63 pp. doi:10.2903/j.efsa.2015.4186
- Ahmed F, Mohammed A. Magnesium: The Forgotten Electrolyte-A Review on Hypomagnesemia. Med Sci (Basel). 2019 Apr 4;7(4):56. doi: 10.3390/medsci7040056
- Maier J.A.M., Locatelli L., Fedele G., Cazzaniga A., Mazur A. Magnesium and the brain: A focus on neuroinflammation and neurodegeneration. Int. J. Mol. Sci. 2022;24:223. doi: 10.3390/ijms24010223
- Kirkland A.E., Sarlo G.L., Holton K.F. The role of magnesium in neurological disorders. Nutrients. 2018;10:730. doi: 10.3390/nu10060730
- Maier J.A., Castiglioni S., Locatelli L., Zocchi M., Mazur A. Magnesium and inflammation: Advances and perspectives. Semin. Cell Dev. Biol. 2021;115:37–44. doi: 10.1016/j.semcdb.2020.11.002
- Andreini C., Bertini I., Cavallaro G., Holliday G.L., Thornton J.M. Metal ions in biological catalysis: From enzyme databases to general principles. J. Biol. Inorg. Chem. 2008;13:1205–1218. doi: 10.1007/s00775-008-0404-5
- Viering D. H. H. M., de Baaij J. H. F., Walsh S. B., Kleta R., Bockenhauer D. Genetic causes of hypomagnesemia, a clinical overview. Pediatric Nephrology. 2017;32(7):1123–1135. doi: 10.1007/s00467-016-3416-3
- Ryan M. F. The role of magnesium in clinical biochemistry: an overview. Annals of Clinical Biochemistry: International Journal of Laboratory Medicine. 1991;28(1):19–26. doi: 10.1177/000456329102800103
- Buelens F.P., Leonov H., de Groot B.L., Grubmüller H. ATP-magnesium coordination: Protein structure-based force field evaluation and corrections. J. Chem. Theory Comput. 2021;17:1922–1930. doi: 10.1021/acs.jctc.0c01205
- Brautigam C.A., Steitz T.A. Structural and functional insights provided by crystal structures of DNA polymerases and their substrate complexes. Curr. Opin. Struct. Biol. 1998;8:54–63. doi: 10.1016/S0959-440X(98)80010-9
- Suh W.C., Leirmo S., Record M.T., Jr. Roles of Mg2+ in the mechanism of formation and dissociation of open complexes between Escherichia coli RNA polymerase and the lambda PR promoter: Kinetic evidence for a second open complex requiring Mg2+ Biochemistry. 1992;31:7815–7825. doi: 10.1021/bi00149a011
- de Baaij J.H.F., Hoenderop J.G.J., Bindels R.J.M. Magnesium in man: Implications for health and disease. Physiol. Rev. 2015;95:1–46. doi: 10.1152/physrev.00012.2014
- Salehidoost R., Taghipour Boroujeni G., Feizi A., Aminorroaya A., Amini M. Effect of oral magnesium supplement on cardiometabolic markers in people with prediabetes: A double blind randomized controlled clinical trial. Sci. Rep. 2022;12:18209. doi: 10.1038/s41598-022-20277-6
- Al Alawi A.M., Majoni S.W., Falhammar H. Magnesium and human health: Perspectives and research directions. Int. J. Endocrinol. 2018;2018:9041694. doi: 10.1155/2018/9041694
- Guerrera MP, Volpe SL, Mao JJ. Therapeutic uses of magnesium. Am Fam Physician 2009;80:157-62. https://www.aafp.org/afp/2009/0715/p157.html
- https://www.phillipsdigestive.com/products/milk-magnesia/
- Altman D., Carroli G., Duley L., Farrell B., Moodley J., Neilson J., Smith D., Magpie Trial Collaborative Group Do women with pre-eclampsia, and their babies, benefit from magnesium sulphate? The magpie trial: A randomised placebo-controlled trial. Lancet. 2002;359:1877–1890. doi: 10.1016/s0140-6736(02)08778-0
- Paoletti P., Bellone C., Zhou Q. NMDA receptor subunit diversity: Impact on receptor properties, synaptic plasticity and disease. Nat. Rev. Neurosci. 2013;14:383–400. doi: 10.1038/nrn3504
- Kirkland A.E., Sarlo G.L., Holton K.F. The Role of Magnesium in Neurological Disorders. Nutrients. 2018;10:730. doi: 10.3390/nu10060730
- Institute of Medicine (IOM). Food and Nutrition Board. Dietary Reference Intakes: Calcium, Phosphorus, Magnesium, Vitamin D and Fluoride. Washington, DC: National Academy Press, 1997. https://www.nap.edu/read/5776/chapter/1
- Magnesium. https://ods.od.nih.gov/factsheets/Magnesium-HealthProfessional
- Azoulay A, Garzon P, Eisenberg MJ. Comparison of the mineral content of tap water and bottled waters. J Gen Intern Med 2001;16:168-75. https://www.ncbi.nlm.nih.gov/pubmed/11318912
- Fine KD, Santa Ana CA, Porter JL, Fordtran JS. Intestinal absorption of magnesium from food and supplements. J Clin Invest 1991;88:396-402. https://www.ncbi.nlm.nih.gov/pubmed/1864954
- United States Department of Agriculture Agricultural Research Service. USDA Food Composition Databases. https://ndb.nal.usda.gov/ndb/
- Jahnen-Dechent W., Ketteler M. Magnesium Basics. Clin. Kidney J. 2012;5((Suppl. S1
- Pham P.C.T., Pham P.A.T., Pham S.V., Pham P.T.T., Pham P.M.T., Pham P.T.T. Hypomagnesemia: A Clinical Perspective. Int. J. Nephrol. Renovasc. Dis. 2014;7:219–230. doi: 10.2147/IJNRD.S42054
- Seo J. W., Park T. J. Magnesium metabolism. Electrolyte Blood Pressure. 2008;6(2):86–95. doi: 10.5049/EBP.2008.6.2.86
- Bergman C., Gray-Scott D., Chen J. J., Meacham S. What is next for the dietary reference intakes for bone metabolism related nutrients beyond calcium: phosphorus, magnesium, vitamin D, and fluoride? Critical Reviews in Food Science and Nutrition. 2009;49(2):136–144. doi: 10.1080/10408390701764468
- Koulouridis I, Alfayez M, Tighiouart H, Madias NE, Kent DM, Paulus JK, Jaber BL. Out-of-hospital use of proton pump inhibitors and hypomagnesemia at hospital admission: a nested case-control study. Am J Kidney Dis. 2013 Oct;62(4):730-7. doi: 10.1053/j.ajkd.2013.02.373
- Alawi A., Majoni A.M., Falhammar S.W. Magnesium and Human Health: Perspectives and Research Directions. Int. J. Endocrinol. 2018;2018:9041694. doi: 10.1155/2018/9041694
- Moe SM. Disorders involving calcium, phosphorus, and magnesium. Prim Care. 2008 Jun;35(2):215-37, v-vi. doi: 10.1016/j.pop.2008.01.007
- Zhang C, Wang L, Zhang J, Su XT, Lin DH, Scholl UI, Giebisch G, Lifton RP, Wang WH. KCNJ10 determines the expression of the apical Na-Cl cotransporter (NCC) in the early distal convoluted tubule (DCT1). Proc Natl Acad Sci U S A. 2014 Aug 12;111(32):11864-9. doi: 10.1073/pnas.1411705111
- Chaudhary DP, Sharma R, Bansal DD. Implications of magnesium deficiency in type 2 diabetes: a review. Biol Trace Elem Res 2010;134:119–29. https://www.ncbi.nlm.nih.gov/pubmed/19629403
- Ford ES, Mokdad AH. Dietary magnesium intake in a national sample of U.S. adults. J Nutr 2003;133:2879-82. https://www.ncbi.nlm.nih.gov/pubmed/12949381
- Musso CG Magnesium metabolism in health and disease. Int Urol Nephrol 2009;41:357-62. https://www.ncbi.nlm.nih.gov/pubmed/19274487
- Barbagallo M, Belvedere M, Dominguez LJ. Magnesium homeostasis and aging. Magnes Res 2009;22:235-46. https://www.ncbi.nlm.nih.gov/pubmed/20228001
- Costello R.B., Nielsen F. Interpreting Magnesium Status to Enhance Clinical Care: Key Indicators. Curr. Opin. Clin. Nutr. Metab. Care. 2017;20:504–511. doi: 10.1097/MCO.0000000000000410
- Gröber U. Micronutrients: Metabolic Tuning-Prevention-Therapy. MedPharm Scientific Publishers; Stuttgart, Germany: 2009.
- de Baaij J.H.F., Hoenderop J.G.J., Bindels R.J.M. Regulation of Magnesium Balance: Lessons Learned from Human Genetic Disease. Clin. Kidney J. 2012;5((Suppl. S1
- Sedehizadeh S, Keogh M, Wills AJ. Reversible hypomagnesaemia-induced subacute cerebellar syndrome. Biol Trace Elem Res. 2011 Aug;142(2):127-9. doi: 10.1007/s12011-010-8757-3
- Tong GM, Rude RK. Magnesium deficiency in critical illness. J Intensive Care Med. 2005 Jan-Feb;20(1):3-17. doi: 10.1177/0885066604271539
- Cohen L, Kitzes R. Clinical clues to magnesium deficiency. Isr J Med Sci. 1987 Dec;23(12):1238-41.
- An G, Du Z, Meng X, Guo T, Shang R, Li J, An F, Li W, Zhang C. Association between low serum magnesium level and major adverse cardiac events in patients treated with drug-eluting stents for acute myocardial infarction. PLoS One. 2014 Jun 5;9(6):e98971. doi: 10.1371/journal.pone.0098971
- Seller RH, Cangiano J, Kim KE, Mendelssohn S, Brest AN, Swartz C. Digitalis toxicity and hypomagnesemia. Am Heart J. 1970 Jan;79(1):57-68. doi: 10.1016/0002-8703(70)90394-7
- Paravicini TM, Yogi A, Mazur A, Touyz RM. Dysregulation of vascular TRPM7 and annexin-1 is associated with endothelial dysfunction in inherited hypomagnesemia. Hypertension. 2009 Feb;53(2):423-9. doi: 10.1161/HYPERTENSIONAHA.108.124651
- Efstratiadis G, Sarigianni M, Gougourelas I. Hypomagnesemia and cardiovascular system. Hippokratia. 2006 Oct;10(4):147-52. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2464251
- Fatemi S, Ryzen E, Flores J, Endres DB, Rude RK. Effect of experimental human magnesium depletion on parathyroid hormone secretion and 1,25-dihydroxyvitamin D metabolism. J Clin Endocrinol Metab. 1991 Nov;73(5):1067-72. doi: 10.1210/jcem-73-5-1067
- Millart H, Durlach V, Durlach J. Red blood cell magnesium concentrations: analytical problems and significance. Magnes Res. 1995 Mar;8(1):65-76.
- Gullestad L., Midtvedt K., Dolva L.O., Norseth J., Kjekshus J. The magnesium loading test: Reference values in healthy subjects. Scand. J. Clin. Lab. Investig. 1994;54:23–31. doi: 10.3109/00365519409086506
- Holm CN, Jepsen JM, Sjøgaard G, Hessov I. A magnesium load test in the diagnosis of magnesium deficiency. Hum Nutr Clin Nutr. 1987 Jul;41(4):301-6.
- Costello RB, Nielsen F. Interpreting magnesium status to enhance clinical care: key indicators. Curr Opin Clin Nutr Metab Care. 2017 Nov;20(6):504-511. doi: 10.1097/MCO.0000000000000410
- Rosner M.H., Ha N., Palmer B.F., Perazella M.A. Acquired Disorders of Hypomagnesemia. Mayo Clin. Proc. 2023;98:581–596. doi: 10.1016/j.mayocp.2022.12.002
- Elisaf M, Panteli K, Theodorou J, Siamopoulos KC. Fractional excretion of magnesium in normal subjects and in patients with hypomagnesemia. Magnes Res. 1997 Dec;10(4):315-20.
- Schlingmann KP, Sassen MC, Weber S, et al. Novel TRPM6 mutations in 21 families with primary hypomagnesemia and secondary hypocalcemia. J Am Soc Nephrol. 2005 Oct;16(10):3061-9. doi: 10.1681/ASN.2004110989
- Upala S, Jaruvongvanich V, Wijarnpreecha K, Sanguankeo A. Hypomagnesemia and mortality in patients admitted to intensive care unit: a systematic review and meta-analysis. QJM. 2016 Jul;109(7):453-459. doi: 10.1093/qjmed/hcw048