Median raphe cyst
Median raphe cyst is a very rare, benign congenital lesion occurring mainly on the ventral aspect of the penis, but can develop anywhere in the midline between the external urethral meatus and anus 1. Median raphe cysts represent an embryologic fusion abnormality of the median raphe which may lead to formation of cyst(s) in the midline, and hence the name median raphe cyst. Median raphe cyst is benign but may become secondarily infected 2. Median raphe cyst may slightly fluctuate in size throughout life. Lesions are flesh-to-yellow in appearance and may appear as continuous or intermittent from the urethral meatus to the anus 3. Median raphe cyst are most common near the glans penis, but may occur anywhere from the urethral meatus to the anus 4. Patients are asymptomatic. As the median raphe cyst is lined by a layer of epithelium, complete surgical excision is required to prevent recurrence 2.
Several terms have been used in the past to describe median raphe cyst. It includes genitoperineal cyst of median raphe 5, mucoid cyst of penis 6, apocrine cystadenoma or hydrocystoma of penis 7 and epidermoid cysts 8. A cyst close to the meatus has been referred to as parameatal cyst 9. It’s still debatable if all these entities are actually same or different 10. One fact that unites these conditions is that they all reflect developmental defect in male genitalia during embryogenesis. Mucoid cyst may result from faulty closure of penoscrotoperineal raphe with sequestration of ectopic urethral mucosa 6. An apocrine cystadenoma or hydrocystoma has bluish hue on clinical examination, while pathological details would reveal focal areas of decapitation secretion in epithelial lining, along with a myoepithelial layer 7. An epidermoid cyst may result due abnormal closure of the median raphe during embryogenesis or rarely, following mechanical implantation in acquired cases 11. A parameatal cyst may arise due to obstruction of paraurethral duct or anomalous fusion of urethra 12.
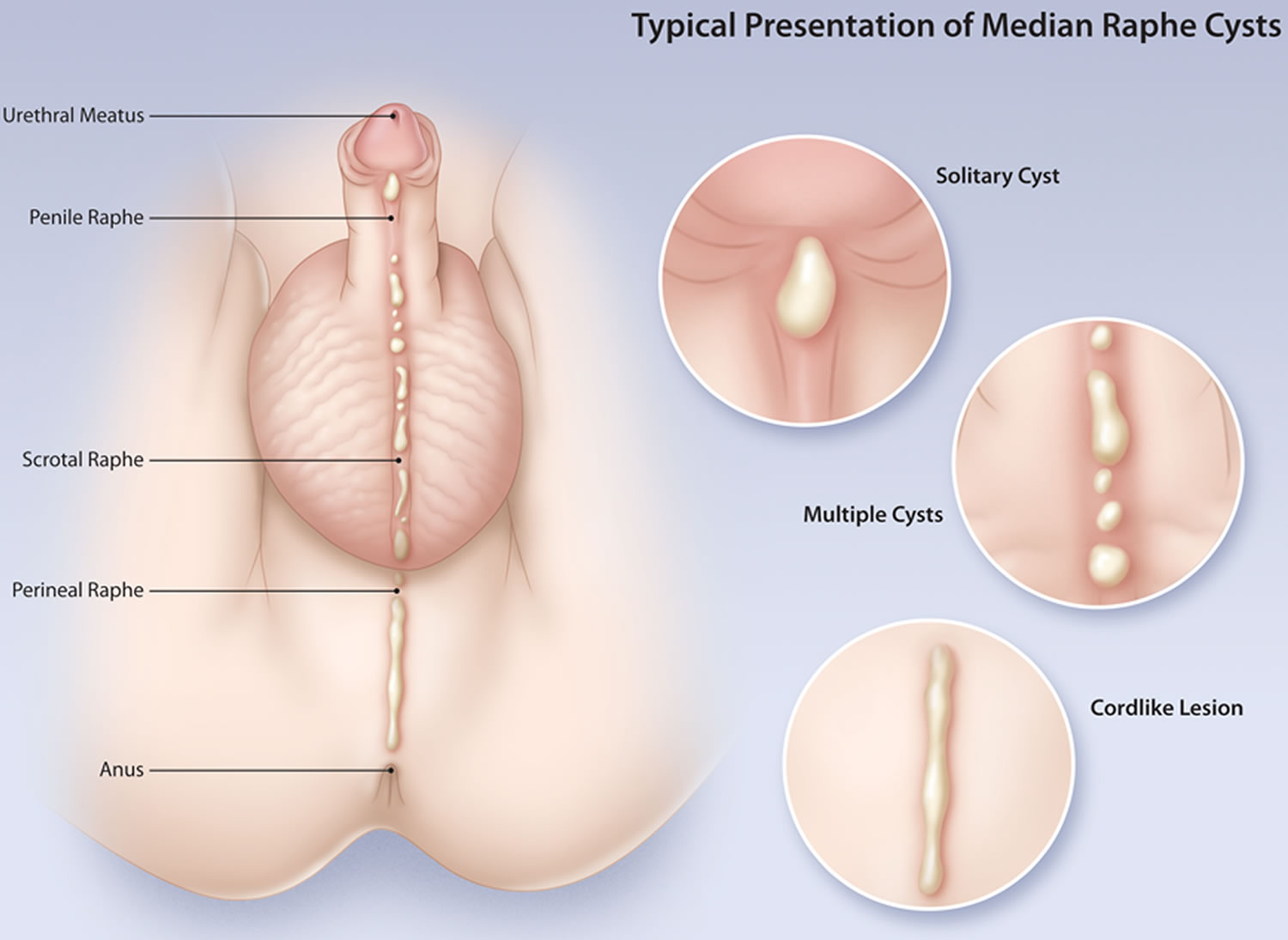
Figure 1. Median raphe cyst
Median raphe cyst cause
The exact cause of median raphe cyst is unknown. Median raphe cyst may represent an embryological developmental abnormality of male genitalia or a defect in closure of the median raphe. The genital tubercle, two urethral folds and the scrotal swellings, give rise to male external genitalia. The scrotal swellings fuse in the midline to form the scrotum, which leaves a permanent surface marking in the form of median raphe. An incomplete closure of the genital or urethral fold gives rise to epithelial rest. The rest may develop into either a cyst or a canal, depending on the presence or absence of an opening on skin surface 13. A cyst can appear even after primary closure from split-off outgrowths of embryonic epithelium 13. A theory that also finds support is “tissue trapping,” in which epithelial rests may get buried during midline fusion and evolve into a cyst or canal 14. Autologous transplant of skin tissue specimens has shown the development of cysts at the transplant sites, lending credibility to the tissue-trapping theory 15. Shiraki 16, on the basis of a study of nine cases of parameatal cyst of glans penis, proposed the occlusion of paraurethral ducts resulting in cyst formation as an explanation. A congenital obliteration of these ducts hampered the physiological drainage and led to development of cysts 16. Infection and trauma are acquired contributory factors in the obstruction 17. Light and electron microscopic findings of Otsuka et al. support this theory 18. Cole and Helwig 6 proposed an alternative, stating that these cysts could be the result of sequestered ectopic periurethral glands of Littre. However, strong evidence in support of this explanation is still lacking.
Median raphe cyst symptoms
Median raphe cysts are mostly asymptomatic 3 and grow proportionately with body size 19. Median raphe cyst is most commonly noticed in the first decade of life; however, because of the condition being asymptomatic, the patient often presents during second to third decades of life 20. Shao et al. 21 mentioned the mean age of presentation to be 26.7 years with a bimodal age distribution at approximately 1–10 years and 21–40 years. Navalón-Monllor et al. 22 found a slightly lower mean age (24.6 years) with similar bimodal age characteristics, having higher presentation during the first and third decades of life.
Though asymptomatic, median raphe cyst has the potential to cause psychological embarrassment and discomfort 23. Parameatal cysts are more likely to give rise to symptoms of urinary obstruction 24. These symptoms are limited to dysuria, urinary frequency, or deflected urinary stream 25. Pain, if present, is an indication of infection 21. Rarely, hematuria, hematospermia 21 and difficulty in sexual function 24 may be presenting complaints. A median raphe cyst near the anal region can be mistaken for hemorrhoids 26. The most common reason for consultation is aesthetic 22. The more distal the median raphe cyst and earlier the age at presentation, the greater the chances of it being symptomatic 21. A case of appearance of median raphe cyst in the shaft of the penis following intense, prolonged sexual intercourse has been described 27.
Median raphe cyst is generally solitary 22, sometimes double 3 and rarely presents as a chain of cystic swellings along the median raphe 28. The chain of cysts gives a cordlike appearance and has been described as canaliform median raphe cysts 29. Another variant is the presence of cysts within the raphe canal, which is an elongated tract along the median raphe 30. Coexistence of a cystic-type lesion and canaliform variant in different regions has also been reported 26. Videodermatoscopy can help confirm the presence of a true canal 30. The cyst is always obvious on the surface; however, a case of median raphe cyst was reported from the United Kingdom in which median raphe cyst presented as nonvisible palpable swelling that was confirmed on ultrasound and magnetic resonance imaging (MRI) 31. Another variation in presentation could be the beginning of the condition with a single lesion with subsequent appearance of more cysts 32. The cyst very rarely may have central umbilication, giving rise to differential diagnosis of molluscum contagiosum 33.
The cysts are generally translucent, and the penile shaft is the most common location. However, many authors have separately defined parameatal urethral cysts, whose numbers exceed those of cysts in any other location 3. Consideration of parameatal cyst as a separate condition or a form of median raphe cyst needs more discussion in the scientific community. The cyst may have a bluish hue 34, which is more a characteristic of cystadenoma/hydrocystoma of the penis. Pigmented cysts appearing as brown-black in color due to presence of melanocytes and melanin pigment in the epithelial lining have also been reported 35. Multiple areas are rarely involved. The majority of the cysts do not reach size in excess of 1 cm 22. However, Matsuyama et al. 3 reported that about 70% of the patients in their study had size less than 0.5 cm. Scrotal cysts tend to be larger than cysts elsewhere 21. Median raphe cysts with sizes in excess of 2 cm have also been reported 36.
Median raphe cyst complications
Median raphe cyst may be secondarily infected and manifest as pain, tenderness, erythema, or pus discharge. About 16% of patients reported by Shao et al. 21 had infected cysts. The most common organism found is Neisseria gonorrhoeae 37. Infection with Trichomonas vaginalis can also occur, but it is rare 38. However, these are case reports of infection of the median raphe rather median raphe cyst. Staphylococcus aureus infecting median raphe cyst of the scrotum and penis has been noted in old case reports 39. Infection of median raphe cyst has been uncommonly documented in recent decades. The culture of the cystic content can help confirm the infective organism. Infection is generally a phenomenon noticed after sexual intercourse. The cyst may also be traumatized by other means and become infected. Urinary obstruction, if due to a parameatal cyst, does not lead to urethritis. median raphe cysts never communicate with the urethra; however, recently, a case of an epidermoid variant traversing the corpus cavernosum has been reported 40. Another case of median raphe cyst in the scrotum was found to mimic a serous tumor and was associated with cryptorchidism 41.
Median raphe cyst diagnosis
Median raphe cyst diagnosis is mostly clinical and is confirmed histologically. Ultrasound shows an isoechoic cystic lesion 24. Ultrasound can help to rule out vascularity and continuity to overlying or underlying structures. However, it has a very limited role in diagnosis and is not frequently ordered. The use of MRI is also not encouraged and reveals low T2-weighted signal of a soft tissue lesion without any appreciable contrast enhancement 31. Like ultrasound, MRI also helps in determining the anatomical extent of the cyst 42. A urethrogram will not show any communication between the cyst and urethra 43.
Median raphe cyst treatment
Spontaneous resolution has been reported 12. Observation is another option when the cyst is small and the child is asymptomatic 14. Because median raphe cyst mostly remains symptom-free, some patients deny any active treatment 34. If left untreated, median raphe cyst may rupture on its own and heal uneventfully 14. Aspiration of the cyst is associated with recurrence 21. Marsupialization or unroofing is not recommended, because it may lead to gaping sinus 16. However, marsupialization has been found to be effective in treating canals 44. Median raphe canals have also been treated with incision followed by electrodessication 45. Excision followed by primary closure remains the treatment of choice and provides cosmetically acceptable results. When the cyst lies in the prepuce, circumcision can also be performed 36. A giant cyst hanging at the frenulum has been treated with excision and repair by frenuloplasty 17.
Excision is associated with excellent results, with no evidence of recurrence in 6 months 46, 1 year 24 and 4 years 47 of follow-up. In a case series with six patients, Asarch et al. 45 noted recurrence in one of the patients after 5 years, and the cyst was reexcised with no subsequent recurrence. One of the patients of Shao et al. 21 developed a fistula following excision. In a retrospective study spanning 14 years, Matsuyama et al. 3 did not identify a single case of recurrence following treatment.
References- Sagar J, Sagar B, Patel AF, Shak DK. Ciliated median raphe cyst of perineum presenting as perianal polyp: a case report with immunohistochemical study, review of literature, and pathogenesis. ScientificWorldJournal. 2006;6:2339-2344. Published 2006 Mar 5. doi:10.1100/tsw.2006.365
- Median Raphe Cyst of the Perineum. Rediscovering the Physical Exam Volume 216, P236, January 01, 2020. https://doi.org/10.1016/j.jpeds.2019.07.050
- Matsuyama S, Matsui F, Yazawa K, Matsumoto F, Shimada K, Matsuoka K. Long-term follow-up of median raphe cysts and parameatal urethral cysts in male children. Urology. 2017;101:99–103.
- Asarch RG, Golitz LE, Sausker WF, Kreye GM. Median raphe cysts of the penis. Arch Dermatol. 1979 Sep;115(9):1084-6.
- Wang C, Lee J, Huang H. Median raphe canals of the genitoperineum. Dermatol Sinica. 1996;14(2):95–99.
- Cole LA, Helwig EB. Mucoid cysts of the penile skin. J Urol. 1976;115(4):397–400.
- Powell RF, Palmer CH, Smith EB. Apocrine cystadenoma of the penile shaft. Arch Dermatol. 1977;113(9):1250–1251.
- Papali AC, Alpert SA, Edmondson JD, Maizels M, Yerkes E, Hagerty J, et al. A review of pediatric glans malformations: a handy clinical reference. J Urol. 2008;180(4 Suppl):1737–1742.
- Koga S, Arakaki Y, Matsuoka M, Ohyama C. Parameatal urethral cysts of the glans penis. Br J Urol. 1990;65(1):101–103.
- Dini M, Baroni G, Colafranceschi M. Median raphe cyst of the penis: a report of two cases with immunohistochemical investigation. Am J Dermatopathol. 2001;23(4):320–324.
- Suwa M, Takeda M, Bilim V, Takahashi K. Epidermoid cyst of the penis: a case report and review of the literature. Int J Urol. 2000;7(11):431–433.
- Willis HL, Snow BW, Cartwright PC, Wallis MC, Oottamasathien S, deVries C. Parameatal urethral cysts in prepubertal males. J Urol. 2011;185(3):1042–1045.
- Neff J. Congenital canals and cysts of the genito-perineal raphe. Am J Surg. 1936;31(2):308–315.
- Little JS, Jr, Keating MA, Rink RC. Median raphe cysts of the genitalia. J Urol. 1992;148(6):1872–1873.
- Epstein WL, Kligman AM. Epithelial cysts in buried human skin. AMA Arch Dermatol. 1957;76(4):437–445.
- Shiraki IW. Parametal cysts of the glans penis: a report of 9 cases. J Urol. 1975;114(4):544–548.
- Hill JT, Ashken MH. Parameatal urethral cysts: a review of 6 cases. Br J Urol. 1977;49(4):323–325.
- Otsuka T, Ueda Y, Terauchi M, Kinoshita Y. Median raphe (parameatal) cysts of the penis. J Urol. 1998;159(6):1918–1920.
- Redman J. Median raphe cysts of the perineum and scrotum. Revista Peruana Urol. 2009;18(2):111–112.
- Syed MMA, Amatya B, Sitaula S. Median raphe cyst of the penis: a case report and review of the literature. J Med Case Rep. 2019;13(1):214. Published 2019 Jul 14. doi:10.1186/s13256-019-2133-5 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6626626
- Shao IH, Chen TD, Shao HT, Chen HW. Male median raphe cysts: serial retrospective analysis and histopathological classification. Diagn Pathol. 2012;7:121.
- Navalon-Monllor V, Ordono-Saiz MV, Ordono-Dominguez F, Sabater-Marco V, Pallas-Costa Y, Navalon-Verdejo P. Median raphe cysts in men: presentation of our experience and literature review. Actas Urol Esp. 2017;41(3):205–209.
- Sagar Jayesh, Sagar Bethani, Patel Adam F., Shak D.K. Ciliated Median Raphe Cyst of Perineum Presenting as Perianal Polyp: A Case Report with Immunohistochemical Study, Review of Literature, and Pathogenesis. The Scientific World JOURNAL. 2006;6:2339–2344.
- Deliktas H, Sahin H, Celik OI, Erdogan O. Median raphe cyst of the penis. Urol J. 2015;12(4):2287–2288.
- Lu CC. A median raphe cyst of the glans penis in a 10-year old boy with urination complaints. Incont Pelvic Floor Dysfunct. 2010;4(1):23.
- Takahashi M, Watanabe T, Sato K, Ohno M, Yamada K, Takezoe T, et al. Congenital median raphe cysts: coexistence of cystic lesions and canal-like lesions. Open J Pediatr. 2013;3(3):2.
- Sharkey MJ, Grabski WJ, McCollough ML, Berger TG. Postcoital appearance of a median raphe cyst. J Am Acad Dermatol. 1992;26(2 Pt 1):273–274.
- Bandyopadhyay D. Canaliform median raphe cyst. Indian J Dermatol Venereol Leprol. 2018;84(1):108.
- Shin S, Hann SK, Kim DY. A case of multiple canaliform median raphe cysts showing a mixed type lining of epithelium: a case report and review of the literature. Ann Dermatol. 2016;28(3):398–399.
- LaCarrubba F, Tedeschi A, Francesconi L, Micali G. Canal versus cysts of the penile median raphe: advancing diagnostic methods using videodermatoscopy. Pediatr Dermatol. 2010;27(6):667–669.
- Parnham AS, Freeman A, Kirkham A, Muneer A. An unusual swelling in the male perineum. BMJ Case Rep. 2015;2015:bcr2014206199
- Colmenero I, Sastre N, de Prada I, Hernandez-Martin A. Pigmented cyst of the median raphe of the scrotum in a boy [in Spanish] Actas Dermosifiliogr. 2009;100(7):633–634.
- Romani J, Barnadas MA, Miralles J, Curell R, de Moragas JM. Median raphe cyst of the penis with ciliated cells. J Cutan Pathol. 1995;22(4):378–381.
- Nagore E, Sanchez-Motilla JM, Febrer MI, Aliaga A. Median raphe cysts of the penis: a report of five cases. Pediatr Dermatol. 1998;15(3):191–193.
- Urahashi J, Hara H, Yamaguchi Z, Morishima T. Pigmented median raphe cysts of the penis. Acta Derm Venereol. 2000;80(4):297–298.
- Bhasin S, Loach R, Sharma G, Gorka V. Giant median raphe prepuceal cyst in an elderly male. Int Surg J. 2016;2016(2):1018–1020.
- Rice JS. Gonorrhea in median raphe of penis. Arch Dermatol. 1963;87(3):395.
- Pavithran K. Trichomonal abscess of the median raphe of the penis. Int J Dermatol. 1993;32(11):820–821.
- Oshin DR, Bowles WT. Congenital cysts and canals of the scrotal and perineal raphe. J Urol. 1962;88(3):406–408.
- Yu A, Capolicchio JP. A case of epidermoid median raphe cyst traversing the corpora cavernosa. Can Urol Assoc J. 2017;11(3–4):E119–E121.
- Hara N, Kawaguchi M, Koike H, Takahashi K. Median raphe cyst in the scrotum, mimicking a serous borderline tumor, associated with cryptorchidism after orchiopecxy. Int J Urol. 2004;11(12):1150–1152.
- Navarro HP, Lopez PC, Ruiz JM, Martinez Sanchiz C, Cha SH, Sanchez AS, et al. Median raphe cyst: report of two cases and literature review. Arch Esp Urol. 2009;62(7):585–589.
- Sasagawa I, Nakada T, Yamaguchi O, Shiraiwa Y. Different types of median raphe cysts in the penis. Int Urol Nephrol. 1992;24(2):187–191.
- Golitz LE, Robin M. Median raphe canals of the penis. Cutis. 1981;27(2):170–172.
- Asarch RG, Golitz LE, Sausker WF, Kreye GM. Median raphe cysts of the penis. Arch Dermatol. 1979;115(9):1084–1086.
- Arrabal-Martin M, Jimenez-Pacheco A, Arrabal-Polo M, Arias-Santiago S. Median raphe cyst of the penis: diagnosis and therapeutic approach [abstract] J Am Acad Dermatol. 2012;66(4):AB38.
- Unal B, Bassorgun C, Karanis M, Elpek G. Perianal median raphe cyst: a rare lesion with unusual histology and localization. Case Rep Dermatol Med. 2015;2015:3.