What is metformin
Metformin is an oral medication for type 2 diabetes that helps control your blood sugar levels by decreasing your liver’s glucose output and increasing your muscles’ glucose uptake. Metformin also increases your body’s response to insulin, a natural substance that controls the amount of glucose in your blood. Metformin is in a class of drugs called biguanides. Taken one to three times a day; extended-release (XR) formulations of metformin can be taken once daily. Possible side effects of metformin are nausea, upset stomach, diarrhea (can sometimes be avoided by taking with food or by using the extended-release formulations). Metformin should not be taken by persons with decreased kidney function or certain other medical conditions.
Metformin is used together with diet and exercise to improve blood sugar control in adults with type 2 diabetes mellitus. Metformin lowers your blood sugar levels by improving the way your body handles insulin. Metformin is usually prescribed for type 2 diabetes when diet and exercise alone have not been enough to control your blood sugar levels.
Metformin is also used to treat insulin resistance in polycystic ovarian syndrome (PCOS).
Metformin is sometimes used together with insulin or other medications, but metformin is not used for treating type 1 diabetes.
Type 2 diabetes is an illness where the body doesn’t make enough insulin, or the insulin that it makes doesn’t work properly. This can cause high blood sugar levels (hyperglycemia).
Polycystic ovary syndrome (PCOS) is a condition that affects how the ovaries work.
For women with PCOS, metformin stimulates ovulation even if they don’t have diabetes. It does this by lowering insulin and blood sugar levels.
It’s best to take metformin tablets with a meal to reduce the side effects. Swallow your metformin tablets whole with a glass of water. Do not chew them.
- The maximum daily dose is 2,000mg a day (for example, 4 x 500mg tablets).
- Metformin tablets come in different strengths. Your doctor will tell you how many tablets to take a day.
Metformin may rarely cause a serious, life-threatening condition called lactic acidosis. Tell your doctor if you have kidney disease. Your doctor will probably tell you not to take metformin. Also, tell your doctor if you are over 65 years old and if you have ever had a heart attack; stroke; diabetic ketoacidosis (blood sugar that is high enough to cause severe symptoms and requires emergency medical treatment); a coma; or heart or liver disease. Taking certain other medications with metformin may increase the risk of lactic acidosis. Tell your doctor if you are taking acetazolamide (Diamox), dichlorphenamide (Keveyis), methazolamide, topiramate (Topamax, in Qsymia), or zonisamide (Zonegran).
Tell your doctor if you have recently had any of the following conditions, or if you develop them during treatment: serious infection; severe diarrhea, vomiting, or fever; or if you drink much less fluid than usual for any reason. You may have to stop taking metformin until you recover.
If you are having surgery, including dental surgery, or any major medical procedure, tell the doctor that you are taking metformin. Also, tell your doctor if you plan to have any x-ray procedure in which dye is injected, especially if you drink or have ever drunk large amounts of alcohol or have or have had liver disease or heart failure. You may need to stop taking metformin before the procedure and wait 48 hours to restart treatment. Your doctor will tell you exactly when you should stop taking metformin and when you should start taking it again.
If you experience any of the following symptoms, stop taking metformin and call your doctor immediately: extreme tiredness, weakness, or discomfort; nausea; vomiting; stomach pain; decreased appetite; deep and rapid breathing or shortness of breath; dizziness; lightheadedness; fast or slow heartbeat; flushing of the skin; muscle pain; or feeling cold, especially in your hands or feet.
Tell your doctor if you regularly drink alcohol or sometimes drink large amounts of alcohol in a short time (binge drinking). Drinking alcohol increases your risk of developing lactic acidosis or may cause a decrease in blood sugar. Ask your doctor how much alcohol is safe to drink while you are taking metformin.
Keep all appointments with your doctor and the laboratory. Your doctor will order certain tests before and during treatment to check how well your kidneys are working and your body’s response to metformin. Talk to your doctor about the risk(s) of taking metformin.
LACTIC ACIDOSIS
- Postmarketing case of metformin-associated lactic acidosis have resulted in death, hypothermia, hypotension, and resistant bradyarrhythmias. The onset is often subtle, accompanied only by nonspecific symptoms such as malaise, myalgias, respiratory distress, somnolence, and abdominal pain. Metformin-associated lactic acidosis has been characterized by elevated blood lactate levels (greater than 5 mmol/L) anion gap acidosis (without evidence of ketonuria or ketonemia), an increased lactate/pyruvate ratio, and metformin plasma levels generally greater than 5 mcg/mL.
- Risk factors for metformin-associated lactic acidosis include with renal impairment, concomitant use of certain drugs (e.g., carbonic anhydrase inhibitors such as topiramate), age 65 years old or greater, having a radiological study with contrast, surgery, and other procedures, hypoxic states (e.g., acute congestive heart failure), excessive alcohol intake, and hepatic impairment; recommendations are provided in the full prescribing guidelines to reduce the risks.
- If acidosis is suspected, immediately discontinue drug and hospitalize patient. Prompt hemodialysis is recommended.
Safety and efficacy have not been established in patients younger than 10 years.
Different types of metformin
Metformin comes as 2 different types of tablet – standard-release tablets and slow-release tablets.
- Standard-release tablets release metformin into your body quickly. You may need to take them several times a day depending on your dose.
- Slow-release tablets (Metformin XR tablets) dissolve slowly so you don’t have to take them as often. One dose in the morning is usually enough.
Your doctor or pharmacist will explain what type of metformin tablets you are on and how to take them.
Metformin is also available as a liquid for children and people who find it difficult to swallow tablets. Liquid metformin is called by the brand name Riomet.
Key facts
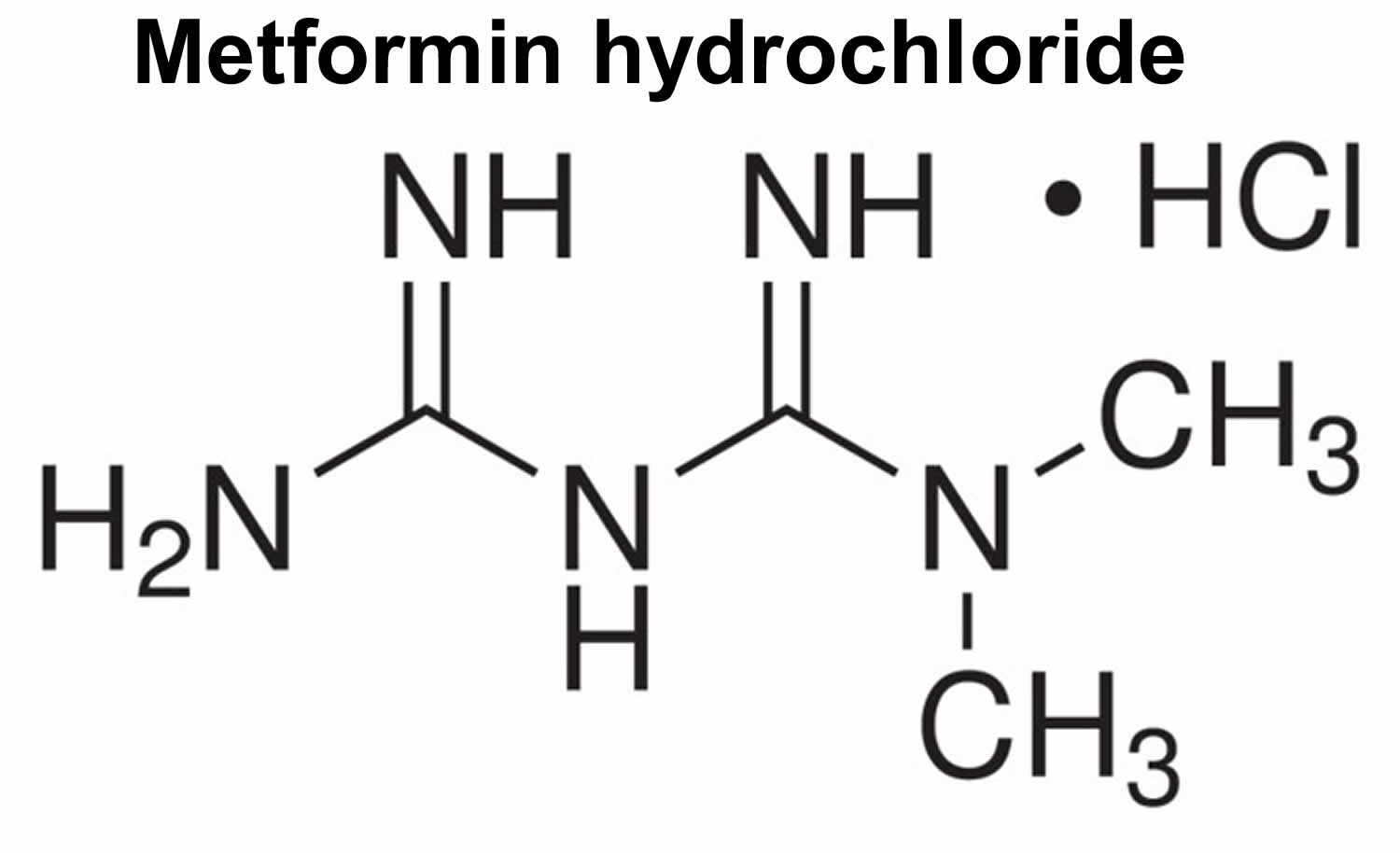
- Metformin hydrochloride improves glucose tolerance by lowering both your basal and postprandial plasma glucose. Metformin hydrochloride decreases your liver glucose production, decreases intestinal absorption of glucose, and improves insulin sensitivity by increasing your muscles’ glucose uptake and utilization. Be sure to follow all exercise and dietary recommendations made by your doctor or dietitian. It is important to eat a healthful diet with Metformin.
- It’s best to take metformin with a meal to reduce the side effects.
- The most common side effects are feeling sick, vomiting, diarrhea, stomach ache and going off your food.
- Metformin does not cause weight gain (unlike some other diabetes medicines).
- Before starting metformin, your doctor must measure your eGFR (estimated glomerular filtration rate). Your estimated glomerular filtration rate (eGFR) measurement reflects how well your kidneys are functioning
- Metformin is contraindicated in patients with an eGFR (estimated glomerular filtration rate) below 30 mL/minute/1.73 m2.
- Starting metformin in patients with an eGFR between 30-45 mL/minute/1.73 m2 is not recommended.
- Your eGFR (estimated glomerular filtration rate) must be measured at least annually whilst taking metformin. In patients at increased risk for the development of renal impairment such as the elderly, renal function should be assessed more frequently.
- In patients taking metformin whose eGFR later falls below 45 mL/minute/1.73 m2, your doctor need assess the benefits and risks of continuing treatment.
- Discontinue metformin if the patient’s eGFR later falls below 30 mL/minute/1.73 m2.
- Discontinue metformin at the time of or before an iodinated contrast imaging procedure in patients with an eGFR between 30 and 60 mL/minute/1.73 m2; in patients with a history of liver disease, alcoholism, or heart failure; or in patients who will be administered intra-arterial iodinated contrast. Re-evaluate eGFR 48 hours after the imaging procedure; restart metformin if renal function is stable.
- Metformin may also be called by the brand names see below.
Metformin brand names:
- Fortamet®
- Glucophage®
- Glumetza®
- Riomet®
- Bolamyn®
- Diagemet®
- Glucient®
- Metabet®
Brand names of combination metformin products:
- Actoplus Met® (containing Metformin, Pioglitazone)
- Avandamet® (containing Metformin, Rosiglitazone)
- Invokamet® (containing Canagliflozin, Metformin)
- Janumet® (containing Metformin, Sitagliptin)
- Jentadueto® (containing Linagliptin, Metformin)
- Kazano® (containing Alogliptin, Metformin)
- Kombiglyze® XR (containing Metformin, Saxagliptin)
- Metaglip® (containing Glipizide, Metformin)*
- Prandimet® (containing Metformin, Repaglinide)
- Segluromet® (containing Ertugliflozin, Metformin)
- Synjardy® (containing Empagliflozin, Metformin)
- Xigduo® XR (containing Dapagliflozin, Metformin)
* This branded product is no longer on the market. Generic alternatives may be available.
Table 1. FDA Approved metformin-containing medicines**
| Brand name | Active ingredient(s) |
|---|---|
| Actoplus Met | metformin and pioglitazone |
| Actoplus Met XR | metformin extended release and pioglitazone |
| Avandamet | metformin and rosiglitazone |
| Fortamet | metformin extended release |
| Glucophage | metformin |
| Glucophage XR | metformin extended release |
| Glucovance | metformin and glyburide |
| Glumetza | metformin extended release |
| Invokamet | metformin and canagliflozin |
| Invokamet XR | metformin extended release and canagliflozin |
| Janumet | metformin and sitagliptin |
| Janumet XR | metformin extended release and sitagliptin |
| Jentadueto | metformin and linagliptin |
| Jentadueto XR | metformin extended release and linagliptin |
| Kazano | metformin and alogliptin |
| Kombiglyze XR | metformin extended release and saxagliptin |
| Prandimet | metformin and repaglinide |
| Riomet | metformin |
| Synjardy | metformin and empagliflozin |
| Synjardy XR | metformin extended release and empagliflozin |
| Xigduo XR | metformin extended release and dapagliflozin |
**These medicines are also available in multiple generic versions.
[Source 1]How long will I take metformin for?
Treatment for diabetes is usually for life. Keep taking metformin tablets unless your doctor tells you to stop.
Can I take metformin for a long time?
Metformin is safe to take for a long time. It will not make you put on weight – it may even help you lose some weight. It also helps keep your cholesterol at a healthy level.
Your doctor will check at least once a year how well your kidneys work. You may need more checks if you are an older person or if your kidneys are not working normally. If your kidneys are not working properly, your doctor will tell you to stop taking metformin.
Metformin can cause vitamin B12 deficiency if you take it for a long time. Your doctor may also check the vitamin B12 level in your blood. If you become deficient, this can be treated by taking vitamin B12 supplements.
Can I come off metformin?
Don’t stop taking metformin without talking to your doctor.
If you stop taking metformin suddenly you may reduce the control over your diabetes.
Treatment for diabetes is usually for life. However, if your kidneys are not working properly, your doctor will tell you to stop taking metformin.
Will metformin affect my contraception?
For women, metformin will not affect contraceptive pills or the morning after pill.
However, some women might need a small adjustment in their metformin dose after starting contraceptive pills. That’s because contraceptive pills change how your body handles sugar.
I use metformin for the treatment of type 2 diabetes. Should I stop metformin before I get pregnant?
If you become pregnant while using metformin, you should not stop your medication without first talking to your health care provider.
High blood sugar levels before and during pregnancy increase the chance of birth defects and other complications. Insulin is usually the medication of choice in pregnancy because it can usually control blood sugar levels better than oral medications. However, metformin is used to treat type 2 diabetes in pregnant women when insulin alone does not result in good blood sugar control. Please consult your health care beforepregnancy to determine which medication(s) is/are the most appropriate for you.
Does metformin cause birth defects? Is it safe to take it during the first trimester?
Recent studies 2, 3, 4, 5, 6, 7, 8, 9 looking at the use of metformin during pregnancy in women with pre-gestational diabetes and in those with PCOS concluded that the use of metformin did not increase the chance for birth defects. Studies noted that women with poorly controlled pre-gestational diabetes did have an increased chance of having a baby with a birth defect.
If I use metformin throughout pregnancy will it affect the baby?
It is unlikely. A small study initially showed a link between the use of metformin during pregnancy and preeclampsia (high blood pressure requiring immediate medical attention). However, this was not seen in later studies.
Other studies compared the use of metformin with the use of insulin during pregnancy and found that metformin did not increase the risk of complications for mothers and babies. There have been some reports of jaundice in babies exposed to metformin during pregnancy, but these reports do not prove that metformin was the cause of the jaundice.
One study looked at the outcome of pregnancy after treatment of PCOS with metformin throughout pregnancy. Infants were found to have normal birth weight and height. At 6 months of age, these infants had normal weight, height, and social and motor development.
I have been diagnosed with gestational diabetes. Is it safe to take metformin during the second and third trimester?
Studies suggest that women receiving metformin during the second and third trimesters for the treatment of gestational diabetes are not expected to have higher chances of complications in their newborns.
Can I take metformin while breastfeeding?
Metformin appears to be safe during breastfeeding. Several reports have shown that the amount of metformin that gets into breastmilk is low. Another study found that infants of mothers who received metformin throughout pregnancy and while breastfeeding achieved the same growth at six months of age as infants who were formula-fed. Be sure to talk to your health care provider about all your breastfeeding questions.
Are there other diabetes medicines beside metformin?
Metformin is usually the first choice of medicine prescribed to treat type 2 diabetes.
There are different types, or classes, of drugs that work in different ways to lower blood glucose (blood sugar) levels:
- Sulfonylureas such as gliclazide
- Meglitinides
- Thiazolidinediones
- DPP-4 inhibitors such as saxagliptin
- SGLT2 Inhibitors such as dapagliflozin
- GLP-1 agonists such as exenatide
- Alpha-glucosidase inhibitors
- Bile Acid Sequestrants
- Insulin
All of these medicines can be taken on their own or at the same time as metformin.
Sulfonylureas
Sulfonylureas stimulate the beta cells of the pancreas to release more insulin. Sulfonylurea drugs have been in use since the 1950s. Chlorpropamide (Diabinese) is the only first-generation sulfonylurea still in use today. The second generation sulfonylureas are used in smaller doses than the first-generation drugs. There are three second-generation drugs: glipizide (Glucotrol and Glucotrol XL), glyburide (Micronase, Glynase, and Diabeta), and glimepiride (Amaryl). These drugs are generally taken one to two times a day, before meals. All sulfonylurea drugs have similar effects on blood glucose levels, but they differ in side effects, how often they are taken, and interactions with other drugs.
Meglitinides
Meglitinides are drugs that also stimulate the beta cells to release insulin. Repaglinide (Prandin) and nateglinide (Starlix) are meglitinides. They are taken before each of three meals.
Because sulfonylureas and meglitinides stimulate the release of insulin, it is possible to have hypoglycemia (low blood glucose levels).
You should know that alcohol and some diabetes pills may not mix. Occasionally, chlorpropamide and other sulfonylureas, can interact with alcohol to cause vomiting, flushing or sickness. Ask your doctor if you are concerned about any of these side effects.
Thiazolidinediones
Rosiglitazone (Avandia) and pioglitazone (ACTOS) are in a group of drugs called thiazolidinediones. These drugs help insulin work better in the muscle and fat and also reduce glucose production in the liver. The first drug in this group, troglitazone (Rezulin), was removed from the market because it caused serious liver problems in a small number of people. So far rosiglitazone and pioglitazone have not shown the same problems, but users are still monitored closely for liver problems as a precaution. Both drugs appear to increase the risk for heart failure in some individuals, and there is debate about whether rosiglitazone may contribute to an increased risk for heart attacks. Both drugs are effective at reducing hemoglobin A1c (glycosated hemoglobin) and generally have few side effects.
DPP-4 Inhibitors
A new class of medications called DPP-4 inhibitors help improve hemoglobin A1c (glycosated hemoglobin) without causing hypoglycemia. They work by by preventing the breakdown of a naturally occurring compound in the body, GLP-1. GLP-1 reduces blood glucose levels in the body, but is broken down very quickly so it does not work well when injected as a drug itself. By interfering in the process that breaks down GLP-1, DPP-4 inhibitors allow it to remain active in the body longer, lowering blood glucose levels only when they are elevated. DPP-4 inhibitors do not tend to cause weight gain and tend to have a neutral or positive effect on cholesterol levels. Sitagliptin (Januvia), saxagliptin (Onglyza), linagliptin (Tradjenta), alogliptin (Nesina) are the DPP-4 inhibitors currently on the market in the US.
SGLT2 Inhibitors
Glucose in the bloodstream passes through the kidneys, where it can either be excreted or reabsorbed. Sodium-glucose transporter 2 (SGLT2) works in the kidney to reabsorb glucose, and a new class of medication, SGLT2 inhibitors, block this action, causing excess glucose to be eliminated in the urine. Canagliflozin (Invokana) and dapagliflozin (Farxiga) are SGLT2 inhibitors that have recently been approved by the FDA to treat type 2 diabetes. Because they increase glucose levels in the urine, side effects can include urinary tract and yeast infections.
Alpha-glucosidase inhibitors
Acarbose (Precose) and miglitol (Glyset) are alpha-glucosidase inhibitors. These drugs help the body to lower blood glucose levels by blocking the breakdown of starches, such as bread, potatoes, and pasta in the intestine. They also slow the breakdown of some sugars, such as table sugar. Their action slows the rise in blood glucose levels after a meal. They should be taken with the first bite of a meal. These drugs may have side effects, including gas and diarrhea.
Bile Acid Sequestrants
The bile acid sequestrant colesevelam (Welchol) is a cholesterol-lowering medication that also reduces blood glucose levels in patients with diabetes. Bile acid sequestrants help remove cholesterol from the body, particularly LDL cholesterol, which is often elevated in people with diabetes. The medications reduce LDL cholesterol by binding with bile acids in the digestive system; the body in turn uses cholesterol to replace the bile acids, which lowers cholesterol levels. The mechanism by which colesevelam lowers glucose levels is not well understood. Because BASs are not absorbed into the bloodstream, they are usually safe for use by patients who may not be able to use other medications because of liver problems. Because of the way they work, side effects of bile acid sequestrants can include flatulence and constipation.
Oral combination therapy
Because the drugs listed above act in different ways to lower blood glucose levels, they may be used together. For example, a biguanide and a sulfonylurea may be used together. Many combinations can be used. Though taking more than one drug can be more costly and can increase the risk of side effects, combining oral medications can improve blood glucose control when taking only a single pill does not have the desired effects. Switching from one single pill to another is not as effective as adding another type of diabetes medicine.
Can I take metformin before surgery?
Your doctor may tell you to stop taking metformin a few days before having an operation or a medical tests.
Metformin may interact with the dye used for an X-ray or CT scan. A general anaesthetic that puts you to sleep can also hide low blood sugar.
Can I drink alcohol with metformin?
Yes, you can drink alcohol while taking metformin. However, alcohol can increase the risk of low blood sugar levels. Try not to drink on an empty stomach.
Is there any food or drink I need to avoid?
It’s a good idea to cut down on foods with added sugar. Check the nutrition labels as many foods and drinks are high in sugar, such as:
- sweets
- cakes
- biscuits
- chocolate
- some fizzy drinks
- juice drinks
Karela (also called bitter gourd) is used to flavor foods including curries such as bitter gourd masala. It has a bitter taste and is also made into juice and tea.
Be careful eating food and drink containing karela (bitter gourd) because it can lower your blood sugar levels and that means your diabetes isn’t controlled as well as it should be.
Can lifestyle changes help diabetes and PCOS?
There are some lifestyle changes you can make to help control the symptoms of diabetes and PCOS.
These include:
- eating a healthy diet
- losing any excess weight
- not smoking
- not drinking too much alcohol – no more than 2 units a day
- exercising regularly – up to 30 minutes a day, 5 times a week is ideal
Metformin is usually prescribed when diet and exercise alone have not been enough to control your blood sugar levels.
How does metformin work?
Metformin hydrochloride is a biguanide, an antihyperglycemic agent, that lowers your blood glucose levels in patients with type 2 diabetes by decreasing the amount of glucose produced by the liver and reduces the amount of sugar your liver releases into your blood. Metformin also decreases intestinal absorption of glucose from food and makes your body respond better to insulin. Insulin is the hormone that controls the level of sugar in your blood. Metformin is usually taken two times a day. A side effect of metformin may be diarrhea, but this is improved when the drug is taken with food.
Intravenous single-dose studies in normal subjects demonstrate that metformin is excreted unchanged in the urine and does not undergo hepatic metabolism (no metabolites have been identified in humans) nor biliary excretion. Renal clearance of metformin is approximately 3.5 times greater than creatinine clearance, which indicates that tubular secretion is the major route of metformin elimination. Following oral administration of metformin, approximately 90% of the absorbed drug is eliminated via the renal route within the first 24 hours, with a plasma elimination half-life of approximately 6.2 hours. In blood, the elimination half-life is approximately 17.6 hours, suggesting that the erythrocyte mass may be a compartment of distribution.
Metformin benefits
Initiating the treatment of type 2 diabetes with metformin is associated with a lower long-term risk of heart attack, stroke, and death than starting with a sulfonylurea, researchers report 10. It’s not known whether the difference is due to additional risk from sulfonylureas, benefits from metformin, or both. The results back up expert recommendations that metformin be considered first in the treatment of type 2.
Metformin for PCOS
Metformin stimulates ovulation in women with PCOS and can encourage regular periods, even if you don’t have diabetes. It does this by lowering insulin and blood sugar levels. PCOS can’t be cured but the symptoms can be managed.
Metformin isn’t licensed to treat PCOS specifically but it can sometimes be prescribed to improve fertility. You may have to see a specialist doctor for this. It will normally be prescribed when other treatments, such as clomifene, have not worked.
With treatment, most women with PCOS are able to get pregnant.
Polycystic ovary syndrome (PCOS) is a common condition that affects how a woman’s ovaries work.
The three main features of PCOS are:
- Irregular periods – which means your ovaries don’t regularly release eggs (ovulation)
- Excess androgen – high levels of “male hormones” in your body, which may cause physical signs such as excess facial or body hair (see signs and symptoms below)
- Polycystic ovaries – your ovaries become enlarged and contain many fluid-filled sacs (follicles) which surround the eggs (it’s important to note that, despite the name, if you have PCOS you don’t actually have cysts)
If you have at least two of these features you may be diagnosed with PCOS.
If you do have signs and symptoms of PCOS, they’ll usually become apparent during your late teens or early twenties. They can include:
- irregular periods or no periods at all
- difficulty getting pregnant as a result of irregular ovulation or failure to ovulate
- excessive hair growth (hirsutism) – usually on the face, chest, back or buttocks
- weight gain
- thinning hair and hair loss from the head
- oily skin or acne
PCOS is also associated with an increased risk of developing health problems in later life, such as type 2 diabetes and high cholesterol levels.
Pregnancy risks
If you have PCOS, you have a higher risk of pregnancy complications, such as high blood pressure (hypertension), pre-eclampsia, gestational diabetes and miscarriage. These risks are particularly high if you’re obese.
If you’re overweight or obese, you can lower your risk by losing weight before trying for a baby.
What causes PCOS?
The exact cause of PCOS is unknown, but it often runs in families. It’s related to abnormal hormone levels in the body, including high levels of insulin.
Insulin is a hormone that controls sugar levels in the body. Many women with PCOS are resistant to the action of insulin in their body and produce higher levels of insulin to overcome this.
This contributes to the increased production and activity of hormones such as testosterone. Being overweight or obese also increases the amount of insulin your body produces.
Treating PCOS
There’s no cure for PCOS, but the symptoms can be treated. Speak to your GP if you think you may have the condition.
If you have PCOS and you’re overweight, losing weight and eating a healthy, balanced diet can make some symptoms better.
Medications are also available to treat symptoms such as excessive hair growth, irregular periods and fertility problems.
If fertility medications are ineffective, a simple surgical procedure called laparoscopic ovarian drilling may be recommended. This involves using heat or a laser to destroy the tissue in the ovaries that’s producing androgens, such as testosterone.
With treatment, most women with PCOS are able to get pregnant.
The main PCOS treatment options are discussed in more detail below.
- Lifestyle changes
In overweight women, the symptoms and overall risk of developing long-term health problems from PCOS can be greatly improved by losing excess weight. Weight loss of just 5% can lead to a significant improvement in PCOS.
You can find out whether you’re a healthy weight by calculating your body mass index (BMI), which is a measurement of your weight in relation to your height. A normal BMI is 18.5-24.9. Use the BMI healthy weight calculator to work out whether your BMI is in the healthy range.
You can lose weight by exercising regularly and having a healthy, balanced diet. Your diet should include plenty of fruit and vegetables, (at least five portions a day), whole foods (such as wholemeal bread, wholegrain cereals and brown rice), lean meats, fish and chicken. Your GP may be able to refer you to a dietitian if you need specific dietary advice.
- Medications
A number of medications are available to treat different symptoms associated with PCOS. These are described below.
Irregular or absent periods
The contraceptive pill may be recommended to induce regular periods, or periods may be induced using an intermittent course of progestogen tablets (which are usually given every three to four months, but can be given monthly).
This will also reduce the long-term risk of developing cancer of the womb lining (endometrial cancer) associated with not having regular periods. Other hormonal methods of contraception, such as an intrauterine (IUS) system, will also reduce this risk by keeping the womb lining thin, but they may not cause periods.
Fertility problems
With treatment, most women with PCOS are able to get pregnant.
The majority of women can be successfully treated with a short course of tablets taken at the beginning of each cycle for several cycles. If these aren’t successful, you may be offered injections or IVF treatment. There’s an increased risk of multiple pregnancy (rarely more than twins) with these treatments.
A medication called clomifene is usually the first treatment recommended for women with PCOS who are trying to get pregnant. Clomifene encourages the monthly release of an egg from the ovaries (ovulation).
If clomifene is unsuccessful in encouraging ovulation, another medication called metformin may be recommended. Metformin is often used to treat type 2 diabetes, but it can also lower insulin and blood sugar levels in women with PCOS.
As well as stimulating ovulation, encouraging regular monthly periods and lowering the risk of miscarriage, metformin can also have other, long-term health benefits, such as lowering high cholesterol levels and reducing the risk of heart disease.
Metformin isn’t licensed for treating PCOS in the US, but because many women with PCOS have insulin resistance, it can be used “off-label” to encourage fertility and control the symptoms of PCOS. Possible side effects of metformin include nausea, vomiting, stomach pain, diarrhoea and loss of appetite.
As metformin can stimulate fertility, if you’re considering using it for PCOS and aren’t trying to get pregnant, make sure you use suitable contraception if you’re sexually active.
Letrozole and tamoxifen are sometimes used to stimulate ovulation instead of clomifene. These medications can also be used for treating breast cancer. Use of letrozole for fertility treatment is “off-label”. This means that the medication’s manufacturer hasn’t applied for a licence for it to be used to treat PCOS.
In other words, although letrozole is licensed for treating breast cancer, it doesn’t have a license for treating PCOS. Doctors sometimes use an unlicensed medication if they think it’s likely to be effective and the benefits of treatment outweigh any associated risks.
If you’re unable to get pregnant despite taking oral medications, a different type of medication called gonadotrophins may be recommended. These are given by injection and there’s a higher risk that they may overstimulate your ovaries and lead to multiple pregnancies.
An alternative to gonadotrophins is a surgical procedure called laparoscopic ovarian drilling. This treatment can be as effective as using gonadotrophins, but it doesn’t increase your risk of multiple pregnancies.
It’s likely that a fertility specialist will check that your fallopian tubes aren’t blocked before most of these treatments are used.
Unwanted hair growth and hair loss
Medications to control excessive hair growth (hirsutism) and hair loss (alopecia) include:
- particular types of combined oral contraceptive tablets (such as co-cyprindiol, Dianette, Marvelon and Yasmin)
- cyproterone acetate
- spironolactone
- flutamide
- finasteride
These medications work by blocking the effects of “male hormones”, such as testosterone, and some also suppress production of these hormones by the ovaries.
A cream called eflornithine can also be used to slow down the growth of unwanted facial hair. This cream doesn’t remove hair or cure unwanted facial hair, so you may wish to use it alongside a hair-removal product. Improvement may be seen four to eight weeks after treatment with this medication.
If you have unwanted hair growth, you may also want to remove the excess hair (by methods such as plucking, shaving, threading, creams or laser removal).
Other symptoms
Medications can also be used to treat some of the other problems associated with PCOS, including:
- weight-loss medication, such as orlistat, if you’re overweight
- cholesterol-lowering medication (statins), if you have high levels of cholesterol in your blood
- acne treatments
Surgery
A minor surgical procedure called laparoscopic ovarian drilling (LOD) may be a treatment option for fertility problems associated with PCOS.
Under general anaesthetic, your doctor will make a small cut in your lower abdomen (tummy) and pass a long, thin microscope called a laparoscope through into your abdomen. The ovaries will then be surgically treated using heat or a laser to destroy the tissue that’s producing androgens (male hormones).
Laparoscopic ovarian drilling has been found to lower levels of testosterone and luteinising hormone (LH) and raise levels of follicle-stimulating hormone (FSH). This corrects your hormone imbalance and can restore the normal function of your ovaries.
Metformin uses
Metformin is used alone or with other medications, including insulin, to treat type 2 diabetes (condition in which the body does not use insulin normally and, therefore, cannot control the amount of sugar in the blood). Metformin helps to control the amount of glucose (sugar) in your blood. Metformin decreases the amount of glucose you absorb from your food and the amount of glucose made by your liver. Metformin also increases your body’s response to insulin, a natural substance that controls the amount of glucose in the blood. Metformin is NOT used to treat type 1 diabetes (condition in which the body does not produce insulin and therefore cannot control the amount of sugar in the blood).
Metformin is also sometimes used to treat polycystic ovary syndrome (PCOS). For women with PCOS, metformin stimulates ovulation even if they don’t have diabetes. It does this by lowering insulin and blood sugar levels.
Over time, people who have diabetes and high blood sugar can develop serious or life-threatening complications, including heart disease, stroke, kidney problems, nerve damage, and eye problems. Taking medication(s), making lifestyle changes (e.g., diet, exercise, quitting smoking), and regularly checking your blood sugar may help to manage your diabetes and improve your health. Metformin may also decrease your chances of having a heart attack, stroke, or other diabetes-related complications such as kidney failure, nerve damage (numb, cold legs or feet; decreased sexual ability in men and women), eye problems, including changes or loss of vision, or gum disease. Your doctor and other healthcare providers will talk to you about the best way to manage your diabetes.
Before taking metformin
- tell your doctor and pharmacist if you are allergic to metformin, any of the ingredients of metformin liquid or tablets, or any other medications. Ask your pharmacist or check the manufacturer’s patient information for a list of the ingredients.
- tell your doctor and pharmacist what other prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking. Be sure to mention any of the following: amiloride (Midamor); angiotensin-converting enzyme (ACE) inhibitors such as benazepril (Lotensin, in Lotrel), captopril, enalapril (Vasotec, in Vaseretic), fosinopril, lisinopril (in Zestoretic), moexipril (Univasc), perindopril (Aceon), quinapril (Accupril), ramipril (Altace), and trandolapril (Mavik); beta-blockers such as atenolol (Tenormin), labetalol (Trandate), metoprolol (Lopressor, Toprol XL), nadolol (Corgard, in Corzide), and propranolol (Hemangeol, Inderal, InnoPran); calcium channel blockers such as amlodipine (Norvasc), diltiazem (Cardizem, Cartia, Diltzac, others), felodipine, isradipine, nicardipine (Cardene), nifedipine (Adalat, Afeditab CR, Procardia), nimodipine (Nymalize), nisoldipine (Sular), and verapamil (Calan, Covera, Verelan, in Tarka); cimetidine (Tagamet); digoxin (Lanoxin); diuretics (‘water pills’); furosemide (Lasix); hormone replacement therapy; insulin or other medications for diabetes; isoniazid (Laniazid, in Rifamate, in Rifater); medications for asthma and colds; medications for mental illness and nausea; medications for thyroid disease; morphine (MS Contin, others); niacin; oral contraceptives (‘birth control pills’); oral steroids such as dexamethasone, methylprednisolone (Medrol), and prednisone (Rayos); phenytoin (Dilantin, Phenytek); procainamide; quinidine (in Nuedexta); quinine; ranitidine (Zantac); triamterene (Dyrenium, in Maxzide, others); trimethoprim (Primsol); or vancomycin (Vancocin). Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you have or have ever had any medical condition, especially those mentioned in the IMPORTANT WARNING section.
- tell your doctor if you are pregnant, plan to become pregnant, or are breastfeeding. If you become pregnant while taking metformin, call your doctor.
- tell your doctor if you eat less or exercise more than usual. This can affect your blood sugar. Your doctor will give you instructions if this happens.
Who can and can’t take metformin
Metformin can be taken by adults.
It can also be taken by children from 10 years of age on the advice of a doctor.
Pregnancy
Recent studies 2, 3, 4, 5, 6, 7, 8, 9 looking at the use of metformin during pregnancy in women with pre-gestational diabetes and in those with PCOS concluded that the use of metformin did not increase the chance for birth defects. Studies noted that women with poorly controlled pre-gestational diabetes did have an increased chance of having a baby with a birth defect.
Metformin and breastfeeding
You can take metformin while you’re breastfeeding. Metformin passes into breast milk but the amount is too small to affect your baby. Metformin appears to be safe during breastfeeding. Several reports have shown that the amount of metformin that gets into breastmilk is low. Another study found that infants of mothers who received metformin throughout pregnancy and while breastfeeding achieved the same growth at six months of age as infants who were formula-fed. Be sure to talk to your health care provider about all your breastfeeding questions.
Metformin isn’t suitable for some people. Tell your doctor before starting the medicine if you:
- have had an allergic reaction to metformin or other medicines in the past
- have uncontrolled diabetes
- have liver or kidney problems
- have a severe infection
- are being treated for heart failure or you have recently had a heart attack
- have severe problems with your circulation or breathing difficulties
- drink a lot of alcohol
You may need to stop taking metformin before having surgery and certain medical tests. Tell your doctor if you need to have:
- a test such as an X-ray or scan involving the injection of a dye that contains iodine into your blood
- surgery where you will be put to sleep
Metformin contraindications
Metformin hydrochloride tablets is contraindicated in patients with:
- Severe renal impairment (eGFR below 30 mL/min/1.73m²).
- Known hypersensitivity to metformin hydrochloride.
- Acute or chronic metabolic acidosis, including diabetic ketoacidosis, with or without coma. Diabetic ketoacidosis should be treated with insulin.
Current US Food and Drug Administration Prescribing Guidelines for Metformin as Related to Kidney Function 1
- Metformin is contraindicated in “renal disease or renal dysfunction (eg, as suggested by serum creatinine levels ≥1.5 mg/dL [males], ≥1.4 mg/dL [females]) or abnormal creatinine clearance (CrCl).”
- Metformin “should not be initiated in patients ≥80 years of age unless measurement of creatinine clearance demonstrates that renal function is not reduced.”
Cautions with other medicines
There are some medicines that interfere with the way metformin works.
If you are taking any of the following medicines, your blood sugar levels may need to be checked more often and your dose adjusted:
- steroid tablets such as prednisolone
- water tablets such as furosemide
- medicines to treat heart problems and high blood pressure
- male and female hormones such as testosterone, oestrogen and progesterone
- other diabetes medicines
- mixing metformin with herbal remedies and supplements.
Some women might need a small adjustment in their metformin dose after starting contraceptive pills. That’s because contraceptive pills change how your body handles sugar.
Metformin dosage
There is no fixed dosage regimen for the management of hyperglycemia in patients with type 2 diabetes with Metformin hydrochloride tablets any other pharmacologic agent. Dosage of Metformin hydrochloride tablets must be individualized on the basis of both effectiveness and tolerance, while not exceeding the maximum recommended daily doses. The maximum recommended daily dose of Metformin hydrochloride tablet is 2,550 mg in adults and 2,000 mg in pediatric patients (10-16 years of age).
Metformin hydrochloride tablets should be given in divided doses with meals. Metformin hydrochloride tablets should be started at a low dose, with gradual dose escalation, both to reduce gastrointestinal side effects and to permit identification of the minimum dose required for adequate glycemic control of the patient.
During treatment initiation and dose titration, fasting plasma glucose should be used to determine the therapeutic response to Metformin hydrochloride tablets and identify the minimum effective dose for the patient. Thereafter, glycosylated hemoglobin should be measured at intervals of approximately 3 months. The therapeutic goal should be to decrease both fasting plasma glucose and glycosylated hemoglobin levels to normal or near normal by using the lowest effective dose of Metformin hydrochloride tablets, either when used as monotherapy or in combination with sulfonylurea or insulin.
Monitoring of blood glucose and glycosylated hemoglobin will also permit detection of primary failure, i.e., inadequate lowering of blood glucose at the maximum recommended dose of medication, and secondary failure, i.e., loss of an adequate blood glucose lowering response after an initial period of effectiveness.
Short-term administration of Metformin hydrochloride tablets may be sufficient during periods of transient loss of control in patients usually well-controlled on diet alone.
When to take metformin
Metformin comes as a liquid, a tablet, and an extended-release (long-acting) tablet to take by mouth. It’s best to take metformin tablets with a meal to reduce the side effects. Swallow your metformin tablets whole with a glass of water. Do not chew them.
The liquid is usually taken with meals one or two times a day. The regular tablet is usually taken with meals two or three times a day. The extended-release tablet is usually taken once daily with the evening meal. To help you remember to take metformin, take it around the same time(s) every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take metformin exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Swallow metformin extended-release tablets whole; do not split, chew, or crush them.
Your doctor may start you on a low dose of metformin and gradually increase your dose not more often than once every 1–2 weeks. You will need to monitor your blood sugar carefully so your doctor will be able to tell how well metformin is working.
Metformin controls diabetes but does not cure it. Continue to take metformin even if you feel well. Do not stop taking metformin without talking to your doctor.
Ask your pharmacist or doctor for a copy of the manufacturer’s information for the patient.
Will my dose go up or down?
Your doctor will check your blood sugar levels regularly and may change your dose of metformin if necessary.
When you first start taking metformin standard-release tablets you will be advised to increase the dose slowly. This reduces the chances of getting side effects.
For example:
- one 500mg tablet with or after breakfast for at least 1 week, then
- one 500mg tablet with or after breakfast and evening meal for at least 1 week, then
- one 500mg tablet with or after breakfast, lunch and evening meal
If you find you can’t tolerate the side effects of standard-release metformin, your doctor may suggest switching to slow-release tablets.
What should I do if I forget a dose?
Take the missed dose as soon as you remember it. However, if it is almost time for the next dose, skip the missed dose and continue your regular dosing schedule. Do not take a double dose to make up for a missed one.
If you often forget doses, it may help to set an alarm to remind you. You could also ask your pharmacist for advice on other ways to help you remember to take your medicine.
What if I take too much?
If you take too many metformin tablets by accident, contact your doctor or hospital straight away.
An overdose of a large number of metformin tablets can cause serious health problems. The symptoms are severe and quick to appear.
They include:
- tummy pain
- diarrhea
- fast or shallow breathing
- feeling cold and unusual sleepiness
- tiredness, or weakness
If you need to go to hospital, take the metformin packet or leaflet inside it plus any remaining medicine with you to the hospital.
Adult Dose for Diabetes Type 2
Use: To improve glycemic control in adults with type 2 diabetes mellitus as an adjunct to diet and exercise.
Immediate-release:
- Initial dose: 500 mg orally twice a day or 850 mg orally once a day
- Dose titration: Increase in 500 mg weekly increments or 850 mg every 2 weeks as tolerated
- Maintenance dose: 2000 mg daily in divided doses
- Maximum dose: 2550 mg/day
Extended-release:
- Initial dose: 500 to 1000 mg orally once a day
- Dose titration: Increase in 500 mg weekly increments as tolerated
- Maintenance dose: 2000 mg daily
- Maximum dose: 2500 mg daily
Comments:
- Metformin, if not contraindicated, is the preferred initial pharmacologic agent for treatment of type 2 diabetes mellitus.
- Immediate-release: Take in divided doses 2 to 3 times a day with meals; titrate slowly to minimize gastrointestinal side effects. In general, significant responses are not observed with doses less than 1500 mg/day.
- Extended-release: Take with the evening meal; if glycemic control is not achieved with 2000 mg once a day, may consider 1000 mg of extended-release product twice a day; if glycemic control is still not achieve, may switch to immediate-release product.
Pediatric Dose for Diabetes Type 2
10 years or older (studies have not been conducted in pediatric patients below the age of 10 years)
Use: To improve glycemic control in children with type 2 diabetes mellitus as an adjunct to diet and exercise.
Immediate-release:
- Initial dose: 500 mg orally twice a day
- Dose titration: Increase in 500 mg weekly increments as tolerated
- Maintenance dose: 2000 mg daily
- Maximum dose: 2000 mg daily
Comments: Take in divided doses 2 to 3 times a day with meals. Titrate slowly to minimize gastrointestinal side effects.
Safety and effectiveness of metformin extended-release has not been established in pediatric patients less than 18 years of age.
Renal Dose Adjustments
Obtain eGFR prior to initiating therapy:
- eGFR less than 30 mL/min/1.73 m2: Use is contraindicated
- eGFR 30 to 45 mL/min/1.73 m2: Initiating therapy is not recommended
- eGFR that falls below 30 mL/min/1.73 m2 during therapy: Discontinue therapy
- eGFR that falls below 45 mL/min/1.73 m2 during therapy: Assess risks versus benefit of continued therapy
- eGFR greater than 45 mL/min/1.73 m2: No dose adjustments recommended
Iodinated contrast procedure:
- For patients with eGFR between 30 and 60 mL/min/1.73 m2: Stop metformin at the time of, or before imaging procedure; re-evaluate eGFR 48 hours after procedure; restart therapy only if renal function is stable.
Liver Dose Adjustments
Not recommended in patients with liver impairment.
Metformin side effects
Metformin may cause changes in your blood sugar. You should know the symptoms of low and high blood sugar and what to do if you have these symptoms.
Metformin may cause side effects, although not everyone gets them.
Common side effects
Common side effects happen in more than 1 in 100 people. Talk to your doctor or pharmacist if these side effects bother you or don’t go away after 1 week:
- feeling sick
- being sick (vomiting) or diarrhea
- stomach ache
- loss of appetite
- a metallic taste in the mouth
Serious side effects
Serious side effects are rare and happen in less than 1 in 10,000 people.
Tell your doctor straight away if you get warning signs of:
- a general feeling of discomfort with severe tiredness, fast or shallow breathing, being cold and a slow heartbeat
- yellowing of the skin or whites of the eyes – this could be a sign of liver problems
- extreme tiredness, lack of energy, pins and needles, a sore and red tongue, mouth ulcers, muscle weakness and disturbed vision – these could be signs of anemia
- a skin rash, redness or itching – this could be a sign of a skin disorder
Serious allergic reaction
In rare cases, it’s possible to have a serious allergic reaction to metformin. A serious allergic reaction is an emergency. Contact a doctor straight away if you think you or someone around you is having a serious allergic reaction.
The warning signs of a serious allergic reaction are:
- getting a skin rash that may include itchy, red, swollen, blistered or peeling skin
- wheezing
- tightness in the chest or throat
- having trouble breathing or talking
- swelling of the mouth, face, lips, tongue, or throat
Tell your doctor if any of these symptoms are severe, do not go away, go away and come back, or do not begin for some time after you begin taking metformin:
- diarrhea
- bloating
- stomach pain
- gas
- indigestion
- constipation
- unpleasant metallic taste in mouth
- heartburn
- headache
- flushing of the skin
- nail changes
- muscle pain
Some side effects can be serious. If you experience any of these symptoms or those listed in the IMPORTANT WARNING section, call your doctor immediately or get emergency treatment:
- chest pain
- rash
Gastrointestinal
Gastrointestinal events such as nausea, vomiting, diarrhea, abdominal pain, and loss of appetite have been frequently reported during therapy initiation and resolve spontaneously in most cases.
- Very common (10% or more): Diarrhea (53.2%), nausea/vomiting (25.5%), flatulence (12.1%)
- Common (1% to 10%): Indigestion, abdominal discomfort, abnormal stools, dyspepsia, loss of appetite
Adverse events in the pediatric population appear to be similar in nature and severity to that published in adults.
Metabolic
- Common (1% to 10%): Hypoglycemia
- Very rare (less than 0.01%): Lactic acidosis
Hematologic
- Very rare (less than 0.01%): Subnormal vitamin B12 levels
Other
- Common (1% to 10%): Asthenia, chills, flu syndrome, accidental injury
Hepatic
- Very rare (less than 0.01%): Liver function test abnormalities, hepatitis
Cardiovascular
- Common (1% to 10%): Chest discomfort, flushing, palpitation
Dermatologic
- Common (1% to 10%): Rash, nail disorder, increased sweating
- Very rare (less than 0.01%): Erythema, pruritus, urticaria
Endocrine
- Frequency not reported: Reduction in thyrotropin (TSH) levels
Immunologic
- Very common (10% or more): Infection (20.5%)
Musculoskeletal
- Common (1% to 10%): Myalgia
Nervous system
- Common (1% to 10%): Lightheadedness, taste disturbances
Psychiatric
- Common (1% to 10%): Headache
Respiratory
- Common (1% to 10%): Rhinitis
These are not all the side effects of metformin. For a full list see the leaflet inside your medicines packet. Call your doctor if you have any unusual problems while taking metformin.
How to cope with metformin side effects
What to do about:
- feeling sick – take metformin with food to reduce the chances of feeling sick – it may also help to slowly increase your dose over several weeks
- being sick (vomiting) or diarrhea – have small but frequent sips of water. Speak to a pharmacist if you have signs of dehydration, such as peeing less than usual or having dark, strong-smelling pee. Don’t take any other medicines to treat diarrhoea or vomiting without speaking to a pharmacist or doctor.
- a metallic taste in the mouth – if you find that metformin is giving you a metallic taste in the mouth, try chewing sugar-free gum
If you find you are suffering from side effects talk to your doctor about switching to a slow-release tablet.
Metformin overdose
Overdose of Metformin hydrochloride has occurred, including ingestion of amounts greater than 50 grams. Hypoglycemia was reported in approximately 10% of cases, but no causal association with Metformin hydrochloride has been established. Lactic acidosis has been reported in approximately 32% of Metformin overdose cases. Metformin is dialyzable with a clearance of up to 170 mL/min under good hemodynamic conditions. Therefore, hemodialysis may be useful for removal of accumulated drug from patients in whom metformin overdosage is suspected.
Symptoms of overdose may include hypoglycemia symptoms as well as the following:
- extreme tiredness
- weakness
- discomfort
- vomiting
- nausea
- stomach pain
- decreased appetite
- deep, rapid breathing
- shortness of breath
- dizziness
- lightheadedness
- abnormally fast or slow heartbeat
- flushing of the skin
- muscle pain
- feeling cold
- FDA Drug Safety Communication: FDA revises warnings regarding use of the diabetes medicine metformin in certain patients with reduced kidney function. https://www.fda.gov/Drugs/DrugSafety/ucm493244.htm
- Panchaud A, et al. 2017. Pregnancy outcomes in women on metformin for diabetes or other indications among those seeking teratology information services. Br J Clin Pharmacol. doi: 10.1111/bcp.13481.
- Cassina M, et al. 2014. First-trimester exposure to metformin and risk of birth defects: a systematic review and meta-analysis. Hum Reprod Update. 20(5):656-69.
- Gilbert C et al. 2006. Pregnancy outcome after first-trimester exposure of metformin: a meta-analysis. Fertil Steril 86:658-63.
- Glueck CJ, et al. 2001. Continuing metformin throughout pregnancy in women with polycystic ovary syndrome appears to safely reduce first-trimester spontaneous abortion: a pilot study. Fertil Steril 75:46-52.
- Feig DS et al. 2007. Oral antidabetic agents in pregnancy and lactation: a paradigm shift? Ann Pharmacother 41:1174-80.
- Coetzee EJ et al. 1984. Oral hypoglycaemics in the first trimester and fetal outcome. S Afr Med J 65:635-7.
- Glueck CJ et al. 2004. Height, weight, and motor-social development during the first 18 months of life in 126 infants born to 109 mothers with polycystic ovary syndrome who conceived on and continued metformin through pregnancy. Hum Reprod 19:1323-30.
- Glueck CJ et al. 2013. Effects of metformin-diet intervention before and throughout pregnancy on obstetric and neonatal outcomes in patients with polycystic ovary syndrome
- Annals of Internal Medicine, Nov. 6, 2012; The Lancet, published online Nov. 7, 2012