Nicotine
Nicotine is an addictive (may be as addictive as heroin and cocaine) and poisonous chemical found in tobacco in regular cigarettes and e-cigarettes (vaping devices) that keeps you smoking. Nicotine is also used as a drug in nicotine replacement therapy (NRT) to help people quit smoking and as an insecticide. Nicotine can reach your brain within seconds of taking a puff. When nicotine enters your body, nicotine causes an increased heart rate and use of oxygen by your heart, and a sense of well-being and relaxation. In the brain, nicotine increases the release of brain chemicals called neurotransmitters, which help regulate your mood and behavior. Dopamine, one of these neurotransmitters in your brain, is released in the reward center of your brain and causes you to feel pleasure and improved your mood. The more you smoke, the more nicotine you need to feel good, but these effects are temporary. So you reach for another cigarette. Nicotine quickly becomes part of your daily routine and intertwined with your habits and feelings. When you stop smoking, your body needs to get used to not having nicotine. This is called nicotine withdrawal and it can be uncomfortable.
Nicotine use can have many different effects in your body. Nicotine can:
- Decrease your appetite: Fear of weight gain makes some people unwilling to stop smoking.
- Boost your mood, giving you a sense of well-being, and possibly even relieve minor depression.
- Increase the activity in your intestines.
- Create more saliva and phlegm.
- Increase your heart rate by around 10 to 20 beats per minute.
- Increase your blood pressure by 5 to 10 mm Hg.
- Possibly cause sweating, nausea, and diarrhea.
- Stimulate your memory and alertness: People who use tobacco often depend on it to help them accomplish certain tasks and perform well.
Common situations that trigger people’s urge to smoke include:
- Drinking coffee or taking breaks at work
- Talking on the phone
- Drinking alcohol
- Driving your car
- Spending time with friends
To overcome your nicotine dependence, you need to become aware of your triggers and make a plan for dealing with them.
For some people, using any amount of tobacco can quickly lead to nicotine dependence.
Signs that you may be addicted to nicotine include:
- You can’t stop smoking. You’ve made one or more serious, but unsuccessful, attempts to stop.
- You have withdrawal symptoms when you try to stop or quit. Your attempts at stopping have caused physical and mood-related symptoms, such as strong cravings, anxiety, irritability, restlessness, difficulty concentrating, depressed mood, frustration, anger, increased hunger, insomnia, constipation or diarrhea.
- You keep smoking despite having health problems. Even though you’ve developed health problems with your lungs or your heart, you haven’t been able to stop.
You give up social activities. You may stop going to smoke-free restaurants or stop socializing with family or friends because you can’t smoke in these situations.
Symptoms of nicotine withdrawal appear within 2 to 3 hours after you last use tobacco. People who smoked the longest or smoked a greater number of cigarettes each day are more likely to have withdrawal symptoms. For those who are quitting, symptoms peak about 2 to 3 days later.
Common nicotine withdrawal symptoms may include 1:
- Intense craving for nicotine
- Anxiety, anger, tension, restlessness, irritability, frustration, or impatience
- Depression
- Drowsiness or trouble sleeping
- Bad dreams and nightmares
- Feeling tense, restless, or frustrated
- Headaches
- Irritability
- Increased appetite, hunger and weight gain
- Difficulty concentrating
- Insomnia
You may notice some or all of these symptoms when switching from regular to low-nicotine cigarettes or reducing the number of cigarettes you smoke.
How bad your symptoms are depends on how long you smoked. The number of cigarettes you smoked each day also plays a role.
Like most smokers, you’ve probably made at least one serious attempt to stop. But it’s rare to stop smoking on your first attempt, especially if you try to do it without help. You’re much more likely to be able to stop smoking if you use medications and counseling, which have both been proved effective, especially in combination.
Does nicotine cause cancer?
No, nicotine has not been found to cause cancer. While nicotine is the addictive substance in tobacco and e-cigarettes (vaping devices), it is other compounds in tobacco that can cause cancer.
Harmful effects of smoking
You already know that people who smoke cigarettes are much more likely to develop and die of certain diseases than people who don’t smoke. But you may not realize just how many different health problems smoking causes:
- Lung cancer and lung disease. Smoking is the leading cause of lung cancer deaths. In addition, smoking causes lung diseases, such as emphysema and chronic bronchitis. Smoking also makes asthma worse.
- Other cancers. Smoking increases the risk of many types of cancer, including cancer of the mouth, throat (pharynx), esophagus, larynx, bladder, pancreas, kidney, cervix and some types of leukemia. Overall, smoking causes 30% of all cancer deaths.
- Heart and blood vessels problems. Smoking increases your risk of dying of heart and blood vessel (cardiovascular) disease, including heart attacks and strokes. If you have heart or blood vessel disease, such as heart failure, smoking worsens your condition.
- Diabetes. Smoking increases insulin resistance, which can set the stage for type 2 diabetes. If you have diabetes, smoking can speed the progress of complications, such as kidney disease and eye problems.
- Eye problems. Smoking can increase your risk of serious eye problems such as cataracts and loss of eyesight from macular degeneration.
- Infertility and impotence. Smoking increases the risk of reduced fertility in women and the risk of impotence in men.
- Complications during pregnancy. Mothers who smoke while pregnant face a higher risk of preterm delivery and giving birth to lower birth weight babies.
- Cold, flu and other illnesses. Smokers are more prone to respiratory infections, such as colds, the flu and bronchitis.
- Tooth and gum disease. Smoking is associated with an increased risk of developing inflammation of the gum and a serious gum infection that can destroy the support system for teeth (periodontitis).
Smoking also poses health risks to those around you. Nonsmoking spouses and partners of smokers have a higher risk of lung cancer and heart disease compared with people who don’t live with a smoker. Children whose parents smoke are more prone to worsening asthma, ear infections and colds.
Smoking and your unborn baby
Protecting your baby from tobacco smoke is one of the best things you can do to give your child a healthy start in life. It can be difficult to stop smoking, but it’s never too late to quit.
Every cigarette you smoke contains over 4,000 chemicals, many of which are dangerous, so smoking when you are pregnant harms your unborn baby. Cigarettes can restrict the essential oxygen supply to your baby. As a result, their heart must beat harder every time you smoke.
Stopping smoking will help both you and your baby immediately. Harmful gases, such as carbon monoxide and other damaging chemicals will clear from your body. When you stop smoking:
- you will reduce the risk of complications in pregnancy and birth
- you are more likely to have a healthier pregnancy and a healthier baby
- you will reduce the risk of stillbirth
- your baby is less likely to be born too early and have to face the breathing, feeding and health problems that often go with being premature
- your baby is less likely to be born with a low birth weight. Babies of smokers are, on average, lighter than other babies, which can cause problems during and after labor. For example, they are more likely to have problems keeping warm and are more likely to get infections
- you will reduce the risk of sudden infant death syndrome (SIDS), also known as “cot death”
Stopping smoking now will also help your baby later in life. Children whose parents smoke are more likely to suffer from asthma and other serious illnesses that may need hospital treatment.
The sooner you stop smoking, the better. But even if you stop in the last few weeks of your pregnancy this will benefit you and your baby.
Secondhand (passive) smoke harms your baby. If your partner or anyone else who lives with you smokes, their smoke can affect you and your baby before and after their birth. You may also find it more difficult to stop if someone around you smokes.
Secondhand smoke can also reduce your baby’s birthweight and increase the risk of sudden infant death syndrome (SIDS), also known as “cot death”. Babies whose parents smoke are more likely to be admitted to hospital for bronchitis and pneumonia during their first year.
Nicotine mechanism of action
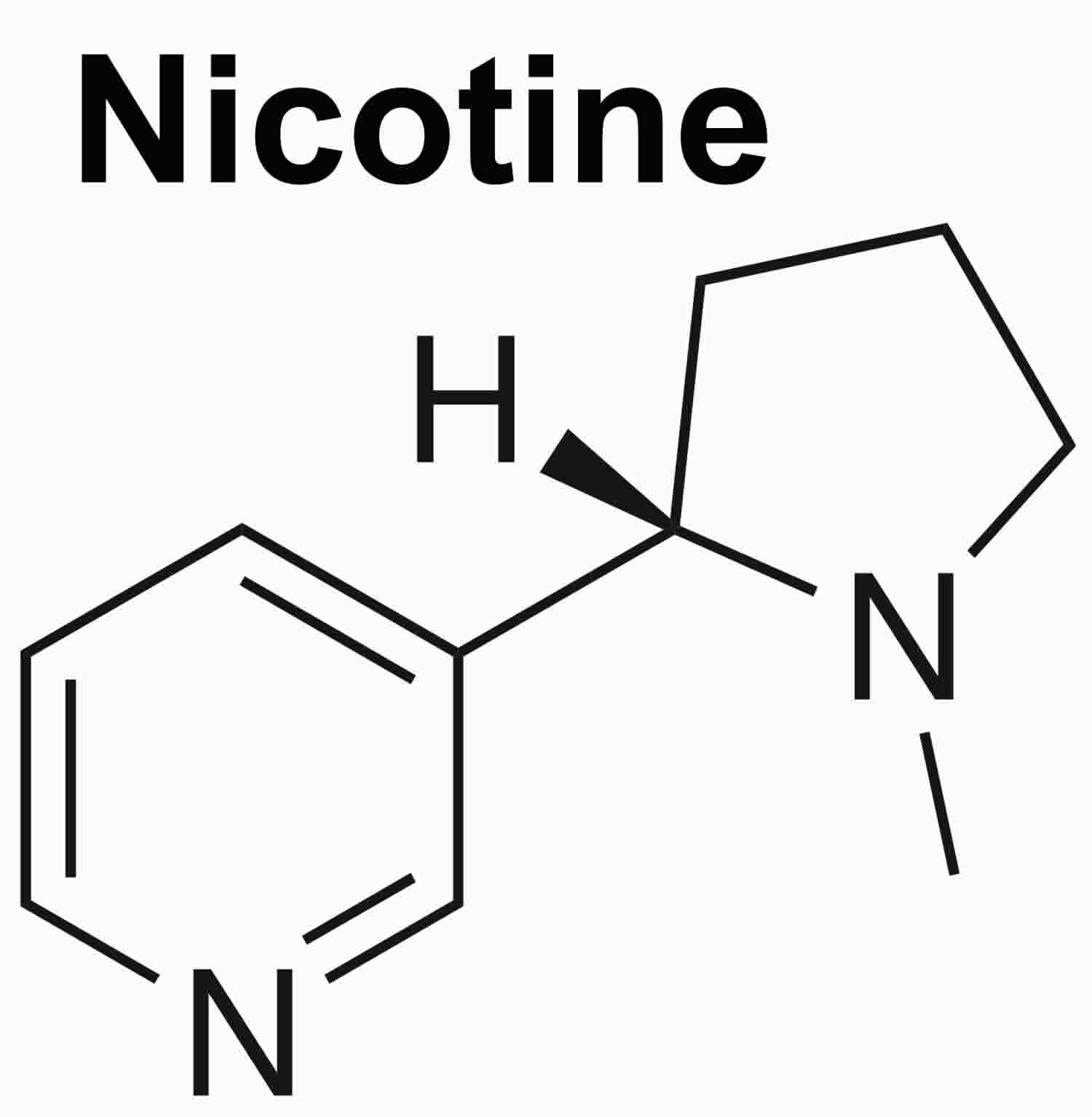
Nicotine is a plant alkaloid (1-methyl-2-[3-pyridyl] pyrrolidine) that is obtained from the leaves of tobacco (Nicotiana tabacum) 2, 3, 4. Two major sources of nicotine are Large leaf tobacco plants( Nicotiana tabacum) and small leaf tobacco plants (Nicotiana rustica) 4. Two major sources of nicotine are large leaf tobacco plants( Nicotiana tabacum) and small leaf tobacco plants (Nicotiana rustica) 4. The main means of administration are smoking pipes or cigars, chewing, and also snorting fine powders.
Structurally, nicotine is a tertiary amine featuring pyrrolidine and pyridine rings 3. Nicotine molecule exhibits selective binding to nicotinic-cholinergic receptors (nicotinic acetylcholinergic receptors [nAChRs]) located in multiple regions of the body, including the brain, neuromuscular junctions, adrenal medulla, and ganglia. Nicotine inhalation through smoking cigarettes prompts its diffusion across lung tissue and subsequently into the systemic circulation and eventual passage into the brain.
Nicotine influences the reward center located within the limbic system and exerts a stimulating impact on the cerebral cortex 3. This stimulation triggers dopamine release in key regions such as the frontal cortex, mesolimbic area, and corpus striatum 3. This surge of dopamine contributes to creating a pleasurable and rewarding experience in the brain. A recent study proposed that nicotine can modulate the activity of monoamine oxidase enzymes, namely monoamine-oxidase-A (MAO-A) and monoamine-oxidase-B (MAO-B) 2. Monoamine-oxidase enzymes are involved in the degradation of dopamine, a neurotransmitter that mainly contributes to addiction 2.
Nicotine metabolism primarily takes place in the liver 3. Therefore, when nicotine is administered through the gastrointestinal system, it undergoes first-pass metabolism by the liver, leading to a bioavailability of only about 20%. This process inherently decreases the bioavailability of nicotine within the system and may cause adverse gastrointestinal effects. Therefore, physicians recommend using non-pill forms of nicotine, including lozenges, sublingual tablets, transdermal patches, gum, inhalers, and sprays, to bypass the first-pass metabolism. These dosage forms facilitate nicotine absorption through the oral or nasal mucosa or skin, effectively bypassing the gastrointestinal system and extending the duration of bioavailability 3.
The absorption route of nicotine is contingent on pH levels. Consumption of acidic foods and beverages can decrease the absorption of nicotine. Moreover, the skin patch releases nicotine gradually, contributing to a controlled and sustained delivery of the substance. This controlled delivery approach significantly reduces the likelihood of nicotine toxicity and mitigates gastrointestinal adverse effects. In the rare instance of a nicotine overdose, symptoms may include nausea, vomiting, diarrhea, dizziness, breathing difficulties, tachycardia, weakness, or rash 3.
In situations involving nicotine cartridge poisoning, a recommended approach is administering repeated doses of activated charcoal until the nicotine cartridge has been entirely expelled through the gastrointestinal tract. This step is crucial due to the prolonged release of nicotine from the cartridge, which mandates continuous treatment to prevent continued absorption of nicotine. Healthcare professionals must promptly cease nicotine exposure and prioritize securing and maintaining airways in patients. In cases of nicotine poisoning, clinicians should offer hemodynamic support to address hypotension and cardiovascular collapse. To manage seizures, benzodiazepines can be administered, whereas atropine can be used to counteract bronchial secretions and diarrhea.
Nicotine uses
Nicotine’s main and only therapeutic use today is for treatment of tobacco dependence. A good number of nicotine replacement products have been developed and licensed as effective treatments for tobacco dependence. Nicotine isolated from tobacco has been tried as a treatment for many conditions and disorders and some positive effects have been observed in preliminary studies in the following conditions: ulcerative colitis 5, major depression 6, Tourettes’s syndrome 7, neuroleptic-induced akathisia 8, attention deficit hyperactivity disorder (ADHD) 9, Parkinsons disease 10 and mild cognitive impairment 11. The best evidence is available for Parkinson’s disease 12, 10 and ulcerative colitis 5, 13. For Parkinson’s disease a study found that smokeless tobacco users had a protective effect with an age adjusted risk of only 0.22 to die from Parkinson’s disease compared with never tobacco users 14. While cigarette smoking is a risk factor for multiple sclerosis, the use of snus (an oral smokeless tobacco product which is usually placed behind the upper lip, either in a loose form or in portioned sachets, and is primarily used in Sweden and Norway) had a protective effect with evidence of an inverse dose-response correlation between cumulative dose of snus and the risk of developing multiple sclerosis 15.
Many of the medicines for these conditions (e.g. Alzheimers disease) have marginal efficacy and it is quite likely that nicotine would have no better effect alone. However, maybe combining nicotine with the other medications would increase the efficacy of the treatment.
Nicotine side effects
Nicotine can:
- Decrease your appetite: Fear of weight gain makes some people unwilling to stop smoking.
- Boost your mood, giving you a sense of well-being, and possibly even relieve minor depression.
- Increase the activity in your intestines.
- Create more saliva and phlegm.
- Increase your heart rate by around 10 to 20 beats per minute.
- Increase your blood pressure by 5 to 10 mm Hg.
- Possibly cause sweating, nausea, and diarrhea.
- Stimulate your memory and alertness: People who use tobacco often depend on it to help them accomplish certain tasks and perform well.
Nicotine side effects may include:
- Gastrointestinal symptoms such as abdominal pain, dyspepsia, hiccups, diarrhea, nausea, and vomiting.
- Central nervous system symptoms such as headache.
- Cardiovascular system symptoms such as palpitations and hypertension 16
- Neuropsychiatric symptoms such as depression, back pain, dizziness, nervousness, drooling, shakiness, cold sweats, hypertension, increased heart rate, and vivid dreams.
- Excess salivation and swelling of the lips, throat, and tongue.
Animal studies have found nicotine exposure to increase behavioral control of conditioned stimuli, which may contribute to the compulsive smoking behavior. Although conditioning is an important element of nicotine addiction, conditioning primarily develops because of the pharmacological actions of the drug with behaviors.
Nicotine Toxicity
While there is a wealth of literature on the harmful effects of smoking – it kills half of its long-term users – much less is known about nicotine itself isolated from tobacco although it is generally understood that it is not the nicotine itself that is so harmful, but the method of delivery, i.e. the burning of tobacco 17. Most of the long-term effects of nicotine are commonly inferred from the many epidemiological studies made on snus since there is little safety data from long-term use of nicotine replacement products 18. Snus is an oral smokeless tobacco product which is usually placed behind the upper lip, either in a loose form or in portioned sachets, and is primarily used in Sweden and Norway 19. Snus users consume as much nicotine as smokers and more than nicotine replacement product users. Since snus also contains other potentially harmful substances such as nitrosamines and metals it is considered being a conservative estimate of the nicotine effects.
Nicotine is a stimulant in low doses and a depressant of nervous activity in very high doses 18. In such doses approximately 500 mg it can cause death by generalized blockade of e.g. respiration 20. The actual lethal dose is dependent on many factors, e.g. if the organism is tolerant, the speed of delivery and the route of administration. There are examples, although rare, of lethal intoxications – suicides mostly – by e.g. transdermal patches or one ingestion of e-cigarette liquid 21.
Cardiovascular disease
Although it is recognized that medicinal nicotine causes temporary changes to the cardiovascular system epidemiological studies have not found the use of nicotine replacement to be linked to the development of cardiovascular disease 22, 23 and studies have shown that nicotine replacement need not be contraindicated for smokers with heart disease 24, 25. In a study that evaluated the safety of nicotine replacement therapy (NRT) in 663 patients after acute coronary syndrome, nicotine replacement use for 1 year was not associated with an increased risk of cardiovascular events 26.
Several studies have been conducted on long-term users of snus (an oral smokeless tobacco product which is usually placed behind the upper lip) to evaluate the risk of cardiovascular heart disease, myocardial infarction or stroke. A recent meta-analysis of eight prospective observational studies concluded that snus use was not associated with acute myocardial infarction 27. Although it was suggested that snus use might slightly increase the risk for a more severe outcome in patients with stroke and a nonfatal myocardial infarction 28.
Pregnancy
Pregnant women who use snus (an oral smokeless tobacco product which is usually placed behind the upper lip) are at higher risk of having babies of lower birth weight, elevated risks for premature delivery, still birth and possibly pre-eclampsia 29, 30. From animal work it seems likely that nicotine may also have adverse neurobehavioral consequences 31.
Drug Interactions
Nicotine interactions are observed with adenosine, cimetidine, and varenicline. Adenosine might amplify the chronotropic effects of nicotine. Conversely, cimetidine can lead to elevated serum nicotine concentrations, potentially resulting in toxicity. When varenicline is coadministered with nicotine replacement therapy (NRT), there is an increased risk of experiencing sleep disturbances, nausea, and cutaneous adverse drug reactions. These reactions may include localized redness, itching, and worsening preexisting acne 32.
Nicotine Withdrawal
Nicotine is the main addictive substance in cigarettes, e-cigarettes (vaping devices) and other tobacco products. As you use tobacco or e-cigarettes (vaping devices) over time‚ your body gets used to having nicotine. When you quit‚ your body needs to get used to not having nicotine anymore, which can be uncomfortable, but is not harmful.
Nicotine is a drug that affects many parts of your body, including your brain, so quitting smoking can cause a variety of uncomfortable nicotine withdrawal symptoms. Craving a cigarette or e-cigarettes (vaping devices), feeling restless or jumpy, or having trouble sleeping are common nicotine withdrawal symptoms. Your mood can change too. Some people say that after they quit smoking, they felt irritable, anxious, or depressed.
Withdrawal is different for everyone, but for most people, symptoms are strongest in the first few days or weeks, and then symptoms get weaker and happen less often over time. Many people don’t like how withdrawal feels, and some people start smoking again to feel better. The first week after quitting is when you are at most risk to slip up and smoke a cigarette or return to smoking. Learn how to handle your withdrawal symptoms to beat these temporary feelings and succeed in quitting long term.
Common nicotine withdrawal symptoms may include 1:
- Having cravings for cigarettes, e-cigarettes (vaping devices) and other tobacco products. Most people experience cravings after they quit. These thoughts and feelings can range from mild to intense or even overwhelming. When cravings are tough to handle, it is important to remember that quitting smoking is the best action you can take for your health. Plan ahead for how you will get through cravings to help you manage them more successfully. The good news is that every craving will pass if you give it time.
- Feeling irritable or grouchy. Change is often hard and can make people feel out of sorts. Remember that you are doing a very good thing for yourself by quitting smoking. Stick with your commitment to quit now and it will help your withdrawal symptoms get easier more quickly.
- Having trouble sleeping. Getting good quality sleep is important, especially when you quit smoking. When you’re tired, you are less resilient and may be more likely to slip and return to smoking.
- Having trouble thinking clearly or concentrating. Some people notice that it is harder to concentrate or that their brain feels foggy in the days after they quit. If you feel this way, know that this too shall pass. If you’re not currently using a quit smoking medication also called nicotine replacement therapy (NRT), consider trying one to help ease your symptoms.
- Feeling restless or jumpy. If you have restless energy or feel on edge, try getting some physical activity to release the tension. You don’t have to be an athlete or even get to a gym. Just going for a walk or doing yard work or chores can be helpful. If you drink coffee, tea, or other caffeinated drinks, try to cut back for a while to lessen the symptoms.
- Feeling sad, anxious, or depressed. People who smoke are more likely to have anxiety or depression than people who don’t smoke. And some people feel increased anxiety, sadness, or depression after they quit smoking. Watch out for this, especially if you’ve ever had these symptoms before.
- Feeling hungrier. As your body adjusts to a new and healthier normal after quitting, you may find that you feel hungrier. Keep a stash of healthy snacks handy. Crunchy snacks like carrots or raw nuts can also help combat cravings by keeping your hands and mouth busy. You may also be worried about weight gain after quitting. For those who do gain weight, it can be disappointing, but it’s important to remember that quitting smoking adds years to your life and reduces your risk for serious diseases and poor health outcomes.
Other, less common nicotine withdrawal symptoms include headaches, fatigue, dizziness, coughing, mouth ulcers, and constipation 33, 34
Nicotine Dependence
Nicotine dependence occurs when you need nicotine and can’t stop using it. Nicotine is the chemical in tobacco that makes it hard to quit. In the brain, nicotine increases the release of brain chemicals called neurotransmitters, which help regulate your mood and behavior. Dopamine, one of these neurotransmitters in your brain, is released in the reward center of your brain and causes you to feel pleasure and improved your mood. The more you smoke, the more nicotine you need to feel good. Nicotine quickly becomes part of your daily routine and intertwined with your habits and feelings. When you try to stop, you experience unpleasant mental and physical changes. These are symptoms of nicotine withdrawal.
Signs that you may be addicted to nicotine include:
- You can’t stop smoking. You’ve made one or more serious, but unsuccessful, attempts to stop.
- You have withdrawal symptoms when you try to stop or quit. Your attempts at stopping have caused physical and mood-related symptoms, such as strong cravings, anxiety, irritability, restlessness, difficulty concentrating, depressed mood, frustration, anger, increased hunger, insomnia, constipation or diarrhea.
- You keep smoking despite having health problems. Even though you’ve developed health problems with your lungs or your heart, you haven’t been able to stop.
You give up social activities. You may stop going to smoke-free restaurants or stop socializing with family or friends because you can’t smoke in these situations.
Symptoms of nicotine withdrawal appear within 2 to 3 hours after you last use tobacco. People who smoked the longest or smoked a greater number of cigarettes each day are more likely to have withdrawal symptoms. For those who are quitting, symptoms peak about 2 to 3 days later.
Common nicotine withdrawal symptoms may include 1:
- Intense craving for nicotine
- Anxiety, anger, tension, restlessness, irritability, frustration, or impatience
- Depression
- Drowsiness or trouble sleeping
- Bad dreams and nightmares
- Feeling tense, restless, or frustrated
- Headaches
- Irritability
- Increased appetite, hunger and weight gain
- Difficulty concentrating
- Insomnia
To overcome your nicotine dependence, you need to become aware of your triggers and make a plan for dealing with them.
Most smokers make many attempts to stop or quit smoking before they achieve stable, long-term abstinence from smoking.
You’re more likely to stop for good if you follow a treatment plan that addresses both the physical and the behavioral aspects of nicotine dependence. Using medications and working with a counselor specially trained to help people stop smoking (a tobacco treatment specialist) will significantly boost your chances of success.
Many effective treatments are available to help you quit smoking. The best treatment for you will depend on your personal preference, your age, whether you’re pregnant or breastfeeding and any medical conditions you have. Ask your doctor for advice and help.
The main reason that people smoke is because they are addicted to nicotine. There are many ways to quit smoking. There are also resources to help you. Family members, friends, and co-workers may be supportive. But to be successful, you must really want to quit. Most people who have quit smoking were unsuccessful at least once in the past. Try not to view past attempts to quit as failures. See them as learning experiences. It is hard to stop smoking or using smokeless tobacco, but anyone can do it.
First, set a quit date. That is the day you will quit completely. Before your quit date, you may begin reducing your cigarette use. Remember, there is no safe level of cigarette smoking.
List the reasons why you want to quit. Include both short- and long-term benefits.
Identify the times you are most likely to smoke. For example, do you tend to smoke when feeling stressed or down? When out at night with friends? While drinking coffee or alcohol? When bored? While driving? Right after a meal or sex? During a work break? While watching TV or playing cards? When you are with other smokers?
Let your friends, family, and co-workers know of your plan to stop smoking. Tell them your quit date. It can be helpful if they know what you are going through, especially when you are grumpy.
Get rid of all your cigarettes just before the quit date. Clean anything that smells of smoke, such as clothes and furniture.
Stress and Smoking
Stress is a normal part of life, in moderation it can help you reach your goals, but too much stress creates more problems. For example, facing a problem like serious illness, death of a family member, divorce, or losing your job, trying to get a task done in a short time, or changing the way you live are just some challenges that might cause stress. Even happy events—like weddings, graduations, or the birth of a child—can be stressful. The causes of stress are different for everybody. You may have learned to deal with stress by smoking. But there are ways to handle stress without smoking. Managing stress is a key part of quitting smoking.
Some people smoke when they feel stressed. They use smoking as a way to cope. There are many problems with using cigarettes as a way to cope with stress or other unpleasant feelings.
- Smoking isn’t a long-term stress reliever. In the time it takes to smoke a cigarette, you could do something else that’s more effective—like take a short walk or try a relaxation exercise.
- Smoking doesn’t solve the problem that’s giving you stress. Your stress will return.
- Nicotine addiction causes stress. Cravings for nicotine feel stressful because your body begins to go through withdrawal.
Some smokers find it hard to give up cigarettes as a way to cope with stress. It’s important to find healthy ways to handle stress and take care of yourself without smoking. There are many other ways to cope with stress that don’t involve smoking.
Nicotine replacement therapy (Quit smoking medications)
Nicotine replacement therapy (NRT) is a medicine that provides you with a low level of nicotine, without the tar, carbon monoxide and other poisonous chemicals present in tobacco smoke. Many people use nicotine replacement therapy (quit smoking medications) to help them reduce withdrawal feelings and deal with cigarette cravings. Nicotine replacement therapy (quit smoking medications) can help you reduce unpleasant withdrawal effects, such as bad moods and cravings, which may occur when you stop smoking.
The US Agency for Healthcare Research and Quality states that nicotine replacement therapy (NRT) is safe for all adults who want to quit smoking except pregnant women and teens. Still, it’s best to discuss nicotine replacement therapy (NRT) use with your doctor before starting it. You may have medical problems that should be considered. When deciding whether to use nicotine replacement therapy (NRT), the benefits of quitting tobacco must outweigh the potential health risks of nicotine replacement therapy (NRT) for each person.
Nicotine replacement therapy (quit smoking medications) can be bought from pharmacies over-the-counter (OTC) and some shops. It’s also available on prescription from a doctor or some stop smoking service.
Nicotine replacement therapy is available as:
- Skin patches: Nicotine patches (transdermal nicotine systems) can be bought with or without a prescription. Patches release nicotine slowly. Some are worn all the time and some should be taken off at night. If you have pregnancy-related nausea and vomiting, patches may be a better solution. Many different types and strengths of patches are available, including 16-hour and 24-hour patches. Which patch you should use depends on how many cigarettes you smoke each day. Package instructions tell you how to use them, and list special considerations and possible side effects. Nicotine replacement therapy patches should be used for no more than 16 hours in any 24-hour period. The best way to remember this is to remove the patch at bedtime.
- How to use nicotine patches: Depending on body size and smoking habits, most people who smoke should start using a full-strength patch (15-22 mg of nicotine) daily for several weeks, and then use a weaker patch (5-14 mg of nicotine) for another several weeks. The patch is changed every day. It should be put on in the morning on a clean, dry area of the skin without much hair. It should be placed below the neck and above the waist – for instance, on the upper arm or chest. The FDA has approved using the patch for a total of 3 to 5 months, but using it longer is better than going back to smoking.
- Nicotine patch side effects may include:
- Skin irritation (redness and itching)
- Dizziness
- Racing heartbeat
- Sleep problems or unusual dreams (more common with the 24-hour patch)
- Headache
- Nausea
- Muscle aches and stiffness
- No one has all of the side effects, and some people have none. Some side effects, such as racing heart, may mean the dose of nicotine is too high for you. Stop using the patch and talk to your health care provider if this happens. You could also have nicotine withdrawal symptoms if your nicotine replacement therapy (NRT) dose is too low.
- What to do about side effects:
- Try a different brand of patch if your skin becomes irritated.
- Reduce the amount of nicotine by using a lower-dose patch.
- Sleep problems may go away in 3 or 4 days. If not, and you’re using a 24-hour patch, try switching to a 16-hour patch.
- Stop using the patch and try a different form of nicotine replacement therapy (NRT).
- Nicotine gum (nicotine polacrilex). Nicotine gum can be bought without a prescription. Nicotine gum is a fast-acting form of replacement. Nicotine is taken in through the mucous membrane of the mouth. You can buy it over the counter (without a prescription). It comes in 2 mg and 4 mg strengths. In choosing your dose, think about whether you:
- Smoke within 30 minutes of waking up
- Smoke 25 or more cigarettes per day
- Have trouble not smoking in restricted areas
- If any of these describe you, you may need to start with the higher 4mg gum dose.
- How to use nicotine gum
- For best results, follow the instructions in the package. Nicotine gum is not meant to be used like regular gum. Chew the gum slowly until you get a peppery taste or tingle. Then tuck it inside your cheek until the taste fades. Chew it to get the peppery taste back, and hold it again. Do this off and on for 20 to 30 minutes. Food and drink can affect how well the nicotine is absorbed, so don’t eat or drink for at least 15 minutes before and during gum use. This is important because many people misuse the nicotine gum and chew it like regular gum instead of how it should be used.An advantage of nicotine gum is that it allows you to control the amount of nicotine you get. The gum can be used as needed or on a fixed schedule during the day. The most recent research has shown that scheduled dosing works better. A schedule of 1 to 2 pieces per hour is common. On the other hand, with an as-needed schedule, you can use it when you need it most – when you have cravings.Chew no more than 24 pieces of gum in one day. Nicotine gum is usually recommended for 6 to 12 weeks, with the maximum being 6 months. Tapering down the amount of gum you use as you approach 3 months may help you stop using it. But it is better to keep using the gum rather than starting to smoke again.
- Nicotine gum side effects may include:
- Bad taste
- Throat irritation
- Mouth sores
- Hiccups
- Nausea
- Jaw discomfort
- Racing heartbeat
- The gum can also stick to and damage dentures and dental work.
- Stomach and jaw discomfort are usually caused by improper use of the gum, such as swallowing the nicotine or chewing too fast. No one has all of the side effects, and some people have none. If your heart is racing or beating irregularly, stop using the gum and talk to your health care provider. You could also have nicotine withdrawal symptoms if your nicotine replacement therapy (NRT) dose is too low.
- Nicotine inhalers which look like plastic cigarettes. Nicotine inhalers are available only by prescription. The nicotine inhaler is a thin plastic tube with a nicotine cartridge inside. Unlike other inhalers, which deliver most of the medicine to the lungs, the nicotine inhaler delivers most of the nicotine vapor to the mouth and throat where it’s absorbed into the bloodstream. Nicotine inhalers are the FDA-approved nicotine replacement method that’s most like smoking a cigarette, which some people trying to quit find helpful. They are not the same as electronic cigarettes, which are not approved by the FDA to help people quit smoking. At this time, nicotine inhalers are the most expensive form of nicotine replacement therapy (NRT) available. Nicotine inhalers poses an extra risk to small children and pets because the used cartridges still have enough nicotine in them to cause harm if it gets on skin or mucous membranes (for instance, if licked or touched to the eyes, mouth, or other mucous membrane). Be sure to store and dispose of the cartridges away from children and pets.
- How to use the nicotine oral inhaler:
- You puff on the inhaler and the cartridge sends a pure nicotine vapor into your mouth. You may use up the cartridge all at once over about 20 minutes, or puff on it only a few minutes at a time. The recommended dose is between 4 and 20 cartridges a day, slowly tapering off over 6 months.
- Nicotine inhaler side effects:
- The most common side effects, especially when first using the inhaler, include:Coughing
- Mouth and/or throat irritation
- Runny nose
- Upset stomach
- Other side effects are related to nicotine:
- Racing heart
- Nervousness
- Headache
- No one has all of the side effects, and some people have none. Some side effects, such as racing heart, may occur because you’ve gotten too much nicotine. Stop using the inhaler to see if the feelings get better and talk to your health care provider if this happens. You may need to use it less often. You could also have nicotine withdrawal symptoms if your nicotine replacement therapy (NRT) dose is too low.
- The most common side effects, especially when first using the inhaler, include:Coughing
- How to use the nicotine oral inhaler:
- Tablets, microtabs, oral strips and lozenges.
- Nicotine lozenges can be bought without a prescription. The lozenge is available in 2 strengths: 2 mg and 4 mg. The needed dose should be based on how long after waking up a person normally has their first cigarette. So, if you smoke your first cigarette within 30 minutes of waking up, use 4 mg nicotine lozenges. If you smoke your first cigarette more than 30 minutes after waking up, use 2 mg-nicotine lozenges. Some people who are using nicotine replacement therapy (NRT) prefer the lozenge to the gum because its use is less conspicuous.
- How to use nicotine lozenges:
- The recommended dose is 1 lozenge every 1 to 2 hours for 6 weeks, then 1 lozenge every 2 to 4 hours for weeks 7 to 9, and finally, 1 lozenge every 4 to 8 hours for weeks 10 to 12.
- The lozenge makers also recommend:
- Do not eat or drink for at least 15 minutes before using a lozenge or while using a lozenge. (Some drinks can reduce how well the lozenge works.)
- Do not use more than 1 lozenge at a time and do not use one right after another.
- Suck on the lozenge until it is fully dissolved, about 20 to 30 minutes. Move it from side to side in your mouth. Do not bite or chew it like a hard candy, and don’t swallow it. The nicotine absorbs through the mucous membranes of the mouth.
- Do not use more than 5 lozenges in 6 hours, or more than 20 lozenges per day.
- Stop using the lozenge after 12 weeks. If you still feel you need to use the lozenge, talk to your doctor.
- Nicotine lozenge side effects:
- Nausea
- Hiccups
- Sore throat
- Coughing
- Heartburn
- Headache
- Gas
- Trouble sleeping
- Racing heart
- How to use nicotine lozenges:
- Nicotine lozenges can be bought without a prescription. The lozenge is available in 2 strengths: 2 mg and 4 mg. The needed dose should be based on how long after waking up a person normally has their first cigarette. So, if you smoke your first cigarette within 30 minutes of waking up, use 4 mg nicotine lozenges. If you smoke your first cigarette more than 30 minutes after waking up, use 2 mg-nicotine lozenges. Some people who are using nicotine replacement therapy (NRT) prefer the lozenge to the gum because its use is less conspicuous.
- Nasal and mouth spray.
- Nicotine nasal spray is only available by prescription. The nasal spray delivers nicotine to the bloodstream rapidly because it’s absorbed through the nose. It relieves withdrawal symptoms very quickly and lets you control your nicotine cravings. If you have asthma, allergies, nasal polyps, or sinus problems, your doctor may suggest another form of nicotine replacement therapy (NRT). Nicotine nasal spray poses a more serious risk to small children and pets because the empty bottles of nasal spray contain enough nicotine to harm them. Do not get the liquid on your skin. If there’s any skin contact, rinse thoroughly with plain water right away. If a bottle breaks or liquid leaks out, put on plastic or rubber gloves to clean it up. Call Poison Control and get emergency help if there’s any question of overdose.
- How to use nicotine nasal spray:
- Most people are told to use 1 to 2 doses per hour. (1 dose = 2 sprays, 1 in each nostril.) At least 8 doses (16 sprays) each day may be needed when you first start, but use as directed by your health care provider. You should not use more than 40 doses (80 sprays) per day. Instructions can vary. Talk to your provider about the plan that’s best for you.
- The FDA recommends that the spray be prescribed for 3-month periods and that it not be used for longer than 6 months.
Possible side effects of nicotine spray
- The most common side effects of the spray get better in about 1 to 2 weeks and can include:
- Nasal irritation
- Runny nose
- Watery eyes
- Sneezing
- Throat irritation
- Coughing
- Other side effects are related to nicotine:
- Racing heart
- Nervousness
- Headache
- No one has all of the side effects, and some people have none. Some side effects, such as racing heart, may occur because you’ve gotten too much nicotine. Stop using the spray to see if the feelings get better and talk to your health care provider if this happens. You may need to use it less often. You could also have nicotine withdrawal symptoms if your nicotine replacement therapy (NRT) dose is too low.
There’s no evidence that any single type of nicotine replacement therapy (quit smoking medications) is more effective than another. But there is good evidence to show that using a combination of nicotine replacement therapy (quit smoking medications) is more effective than using a single product. Inhalators, gum and sprays act more quickly and may be better for helping with cravings. Often the best way to use nicotine replacement therapy (quit smoking medications) is to combine a skin patch with a faster acting form such as gum, inhalator or nasal spray.
When choosing the type of nicotine replacement therapy (NRT) you will use, think about which method will best fit your lifestyle and pattern of smoking or using smokeless tobacco. For example, do you want/need something in your mouth or something to keep your hands busy? Are you looking for once-a-day convenience? How urgent are your cravings for nicotine?
Here are some important points to think about as you decide:
- Nicotine gums, lozenges, and inhalers are substitutes you can put into your mouth that let you control your dosage to help keep cravings under better control.
- Nicotine gums and lozenges are generally sugar-free, but if you are diabetic and have any doubts, check with the manufacturer.
- Nicotine nasal spray works very quickly when you need it.
- Nicotine inhalers allow you to mimic the use of cigarettes by puffing and holding the inhaler. It also works very quickly.
- Nicotine patches are convenient and only have to be put on once a day.
- Both inhalers and nasal sprays require a doctor’s prescription.
- Some people may not be able to use patches, inhalers, or nasal sprays because of allergies or other conditions.
- Nicotine gum may stick to dentures or dental work making it hard to chew before “parking.”
Whatever type you use, take your nicotine replacement therapy (NRT) at the recommended dose. Nicotine replacement therapy (NRT) is not recommended for long-term use, but if it’s needed to prevent relapse, continuing to use nicotine replacement therapy (NRT) is preferable than returning to smoking. Treatment with nicotine replacement therapy (quit smoking medications) usually lasts 8-12 weeks, before you gradually reduce the dose and eventually stop.
If you use a different dose or stop taking it too soon, nicotine replacement therapy (NRT) can’t be expected to work like it should. If you smoke very heavily very lightly, or are a smokeless tobacco user, talk with your health care provider about how to get the nicotine replacement therapy (NRT) dose that best fits your needs.
Quit smoking medications
The most commonly used quit smoking medications are nicotine replacement therapy (NRT) because they contain varying amounts of nicotine. But nicotine replacement therapy (NRT) is only one type of medication that can help with withdrawal and reduce your urge to smoke. There are two approved quit-smoking medications that don’t contain nicotine, and both are available only by prescription:
- Bupropion SR (Zyban, Wellbutrin, or Aplenzin). Bupropion SR (Zyban) is a medicine that contains no nicotine. Bupropion is a prescription antidepressant in an extended-release form, Bupropion SR (Zyban), that helps reduce cravings and symptoms of nicotine withdrawal. Bupropion acts on chemicals in the brain that are related to nicotine craving. You need a prescription to get this medicine. Bupropion SR (Zyban) may help with nicotine withdrawal and reduce your urge to smoke. Bupropion SR (Zyban) works best if it’s started 1 or 2 weeks before you quit smoking. The usual dosage is one or two 150 mg tablets per day. If you’re still not using tobacco after taking Bupropion SR (Zyban) for 7 to 12 weeks, your doctor may have you keep taking it for some time afterward to help stop you from going back to smoking. Keep up with your other support systems during this time and for at least a few months after you quit. Make sure to use it the way your doctor prescribes it. You also shouldn’t take it if you’re taking sedatives or have recently taken a monoamine oxidase inhibitor (MAOI, an older type of antidepressant).
- Bupropion SR (Zyban) side effects of bupropion include:
- Dry mouth
- Stuffy nose
- Trouble sleeping and nightmares
- Tiredness
- Constipation
- Nausea
- Headaches
- High blood pressure
- Seizures
- Feeling depressed, anxious, agitated, hostile, aggressive, overly excited or hyperactive, or confused; or having suicidal thoughts
- If you are using bupropion, see your health care provider if you feel depressed or start thinking of suicide. Also be sure to ask what to expect while taking this drug, and what to do if you or others notice possible side effects. Bupropion can cause drug interactions and shouldn’t be used with certain other drugs or supplements. Be sure your provider knows about everything you take, such as prescription drugs, vitamins, herbs, supplements, and any medicines you take on your own when you need them, like acetaminophen (Tylenol) or aspirin. Also be sure to tell every provider you see that you’re taking bupropion.
- Bupropion SR (Zyban) may NOT be right for:
- Pregnant women
- People who have seizures
- People with cirrhosis
- People with serious head injury
- People who have eating disorders (anorexia or bulimia)
- People with bipolar (manic-depressive) illness
- People who are heavy drinkers
- Dry mouth
- Varenicline (Chantix). Varenicline (Chantix) is a medicine that contains no nicotine. Varenicline (Chantix) works by blocking the pleasant effects of nicotine (from smoking) on your brain. Varenicline (Chantix) lessens the pleasure you get from smoking and reduces your nicotine withdrawal symptoms. You need a prescription to get this medicine. Varenicline (Chantix) may help you quit by easing withdrawal symptoms and blocking the effects of nicotine from cigarettes if you start smoking again. You typically start taking varenicline (a pill) about a month to a week before your Quit Day. Take it after meals, with a full glass of water. The daily dose increases over the first 8 days you take it. If you have problems with the higher doses, a lower dose may be used while you try to quit. Typically, Varenicline (Chantix) is given for 12 weeks, but people who quit during that time may get another 12 weeks of treatment to boost their chances of staying off tobacco. It’s important to keep up with other support systems during this time and for at least a few months after quitting.
- Varenicline (Chantix) side effects may include:
- Nausea
- Vomiting
- Headache
- Trouble sleeping, unusual dreams, or sleepwalking
- Constipation
- Gas
- Changes in taste
- Skin rashes
- Seizures
- Heart or blood vessel problems (mostly in people who already have these problems)
- Vivid dreams
- Mood or behavior changes, such as depression, hallucinations, delusions, aggression, hostility, agitation, anxiety, panic, or even suicidal thoughts. If these happen, contact your doctor right away. Ask your doctor or pharmacist if this medicine is right for you. Make sure to use it the way your doctor prescribes it.
- Varenicline (Chantix) may not be right for:
- People with kidney problems
- Women who are pregnant‚ plan to become pregnant‚ or are breast-feeding
- While quit smoking medications can help, they won’t do all the work. To give yourself the best chance for success, you can combine medication with other quit methods.
- You may have heard about a US Food and Drug Administration (FDA) recall of Varenicline (Chantix) 35. If you are currently using Varenicline (Chantix) and have concerns, talk to your doctor or pharmacist about what is best for you.
- Varenicline (Chantix) side effects may include:
- Bupropion SR (Zyban) side effects of bupropion include:
Any of these products can help reduce nicotine cravings and withdrawal symptoms — making it more likely that you’ll stop smoking for good. Using more than one may help you get better results.
Research is being done to find out if Varenicline (Chantix) can be used at the same time as nicotine replacement therapy (NRT). A few studies have suggested that using Varenicline (Chantix) along with nicotine replacement therapy (NRT) is well-tolerated and safe, but others have found this has no long-term benefit in helping people quit. More research is needed.
Research on using both Varenicline (Chantix) and Bupropion SR (Zyban) at the same time is also being done. While there may be a benefit to combining the drugs vs. taking only varenicline, more research is needed to understand if this could cause more severe side effects.
Although you can buy some quit-smoking products without a prescription, it’s a good idea to talk to your doctor first. Together you can explore which products might be right for you, when to start taking them and possible side effects.
Other prescription drugs used to help people quit tobacco
For those who can’t use either of the US Food and Drug Administration (FDA)-approved drugs to help them quit, or for those who haven’t been able to quit using them, other drugs have shown promise in studies. They’re recommended by the Agency for Healthcare Research and Quality for this kind of use, but have not been approved by the FDA for this purpose and so are used “off-label.”
These drugs are only available with a prescription and are not recommended for pregnant women, teens, or people who smoke fewer than 10 cigarettes a day.
- Nortriptyline. Nortriptyline is an older anti-depressant drug that helps reduce tobacco withdrawal symptoms. Nortriptyline has been found to increase chances of success in quitting smoking when compared to those taking no medicine. It’s typically started 10 to 28 days before a person stops smoking to allow it to reach a stable level in the body. Some people have side effects like a fast heart rate, blurred vision, trouble urinating, dry mouth, constipation, weight gain or loss, and low blood pressure when they stand up. Nortriptyline can affect a person’s ability to drive or operate machinery, and certain drugs cannot be used along with it.
- If you and your doctor decide to use Nortriptyline, be sure your doctor and pharmacist know exactly what other drugs you’re taking before you start Nortriptyline. Also be sure you know how to take it and how to taper off it when you are ready to stop. The dose of nortriptyline must be slowly lowered, since the drug cannot be stopped suddenly without the risk of serious effects. People with heart disease should use Nortriptyline cautiously. Be sure to tell all your health care providers that you are taking Nortriptyline.
- Clonidine. Clonidine is another older drug that has been shown to help people quit. Clonidine is FDA-approved to treat high blood pressure. When used to quit smoking, it can be taken as a pill twice a day or worn as a skin patch that’s changed once a week. If you’re planning to use Clonidine, be sure your doctor and pharmacist know exactly what else you’re taking before you start taking it. The most common side effects of clonidine are constipation, dizziness, drowsiness, dry mouth, and unusual tiredness or weakness. There are rarely more severe side effects, such as allergic reactions, a slow heart rate, and very high or very low blood pressure. Your doctor might want to watch your blood pressure while you are on Clonidine. The drug can affect your ability to drive or operate machinery. You can start taking clonidine up to 3 days before you quit smoking, but it can also be started the day you quit. It shouldn’t be stopped suddenly. The dose must be lowered over a few days to prevent tremors, confusion, agitation, or a rapid increase in blood pressure.
Who can use nicotine replacement therapy (quit smoking medications)?
Most people are able to use nicotine replacement therapy (quit smoking medications), including:
- Adults and children over 12 years of age – although children under 18 should not use the lozenges without getting medical advice first
- Pregnant women – your doctor may suggest nicotine replacement therapy (quit smoking medications) if they think it would help you quit. You can use nicotine replacement therapy (quit smoking medications) during pregnancy if it will help you stop smoking and you’re unable to stop without it. Stop smoking tablets such as Champix (varenicline) or Zyban (bupropion) are NOT recommended during pregnancy and are not currently available.
- Breastfeeding women – your doctor can advise you how to do this safely
Always read the packet or leaflet before using nicotine replacement therapy (quit smoking medications) to check whether it’s suitable for you. Sometimes it may be advisable to get medical advice first, for example if you have kidney or liver problems, or you’ve recently had a heart attack or stroke.
Nicotine replacement therapy (quit smoking medications) side effects
Side effects of nicotine replacement therapy (quit smoking medications) can include:
- Skin irritation when using patches
- Irritation of nose, throat or eyes when using a nasal spray
- Difficulty sleeping (insomnia), sometimes with vivid dreams
- An upset stomach
- Dizziness
- Headaches
Any side effects are usually mild. But if they’re particularly troublesome, contact your doctor as the dose or type of nicotine replacement therapy (quit smoking medications) may need to be changed.
Are nicotine replacement products safe?
Long-term use of nicotine replacement products has not been associated with any serious harmful effects 36. However, nicotine replacement products are not recommended for use by people who are pregnant or trying to become pregnant.
Can you get too much nicotine from nicotine replacement therapy?
Nicotine overdose is rare, but possible. Nicotine replacement therapy (NRT) products are labeled to match the amount of nicotine you get from nicotine replacement therapy (NRT) to the amount you got from tobacco. If used this way, you should get a nicotine dose fairly close to what you’ve been getting. You don’t want to get more than that, because higher doses of nicotine can cause harm. To avoid this, follow dosing instructions carefully. Also, don’t use heat (like a heating pad or heat lamp) on the skin near your nicotine patch – you could absorb more nicotine due to the increased blood supply.
Nicotine absorbs through the skin and mucous membranes, so you must store and dispose of your nicotine replacement therapy (NRT) safely. Nicotine overdose can be fatal, but this is rare and requires taking in very high doses of nicotine. Overdose is more of a problem in children and pets because of their smaller size. Keep nicotine replacement therapy (NRT) and used gum, patches, empty cartridges, bottles, etc., safely away from children and pets. Never drop them on the street or in open trash cans where kids and animals can reach them.
Symptoms of nicotine overdose
Symptoms of nicotine overdose may include:
- Headache
- Nausea and vomiting
- Abdominal pain
- Diarrhea
- Agitation, restlessness
- Fast or irregular heartbeat
- Cold sweat
- Pale skin and mouth
- Weakness
- Tremors (shaking)
- Confusion
- Disturbed vision and hearing
- Weakness
- High blood pressure, which then drops
- Dizziness or faintness due to low blood pressure
- Seizures
- Fast breathing in early poisoning, breathing may stop later
Call Poison Control and get emergency help if you suspect nicotine overdose. If you’re taking nicotine replacement therapy (NRT) as prescribed and are still having mild symptoms such as headache, vomiting, diarrhea, or sweating, lower your dose and talk to your health care provider.
If I use nicotine replacement therapy, will still have withdrawal symptoms or cravings from quitting smoking?
Yes. You may still have withdrawal symptoms or cravings while using nicotine replacement therapy (NRT). Try to be patient. Most people find withdrawal symptoms especially difficult the first week or two after quitting. Most smokers find withdrawal symptoms less intense when using nicotine replacement therapy (quit smoking medications). If withdrawal symptoms continue a few days after you start using nicotine replacement therapy (quit smoking medications), talk to your doctor or pharmacist about different nicotine replacement therapy (quit smoking medications) products that can help.
Follow nicotine replacement therapy (quit smoking medications) product directions carefully. Some nicotine replacement therapy (quit smoking medications) products (gum, lozenge, inhaler) work better if they are not used at the same time as high-acid drinks, such as sodas and fruit juices. It is safe to continue using nicotine replacement therapy (quit smoking medications) even if you slip and smoke one or two cigarettes. Staying on nicotine replacement therapy (quit smoking medications) increases your chances of getting back on track for quitting.
How much does it cost for nicotine replacement therapy?
Many states in the United States offer free nicotine replacement therapy (NRT) through their state quitlines. The North American Quitline Consortium (https://www.naquitline.org) has a quitline map to help you find free quit smoking support and other resources near you.
People eligible for Medicare or Medicaid also may be eligible for free nicotine replacement therapy (quit smoking medications). In recent years, insurance coverage for nicotine replacement therapy (quit smoking medications) has expanded under many private insurance plans. Check your insurance plan to learn if you are eligible for coverage.
Even if nicotine replacement therapy (quit smoking medications) is not covered through your insurance or state quitline, the cost of nicotine replacement therapy (quit smoking medications) for several weeks will still be less than the cost of buying cigarettes.
Can I use one nicotine replacement therapy product with others?
Yes. Nicotine replacement therapy (NRT) products can be used safely together. For example, you might use long-acting nicotine replacement therapy (quit smoking medications) such as the patch with short-acting nicotine replacement therapy (quit smoking medications) such as a lozenge. Some people find both a long-acting patch and short-acting gum to be useful when cravings are high to handle withdrawal symptoms and fight off cravings.
Stopping nicotine replacement therapy
Nicotine replacement therapy (NRT) is meant to be used for a limited period of time only. Use should be tapered down before nicotine replacement therapy (NRT) is stopped. Studies to date have not shown that extending nicotine replacement therapy (NRT) use longer than the recommended time greatly impacts quit success. However, long-term nicotine replacement therapy (NRT) use is still preferable to smoking.
Research is still being done to refine the use of nicotine replacement therapy (NRT). If you feel that you need nicotine replacement therapy (NRT) for a different length of time than is recommended, it’s best to discuss this with your doctor.
Can I become dependent on long-term nicotine replacement therapy?
Nicotine replacement therapy (NRT) has the potential for long-term dependence. Nicotine is addictive, and people can transfer their dependence from tobacco to the nicotine replacement therapy (NRT).
Use nicotine replacement therapy (NRT) only as long as you need it, as prescribed by your health care provider. Talk to your doctor if you’re having trouble stopping nicotine replacement therapy (NRT).
How to manage cravings and deal with the urge to smoke?
Cravings are uncomfortable, but they don’t last forever. When a craving is triggered, it’s important to have a plan to beat that urge to smoke. Triggers are the things that make you want to smoke. Different people have different triggers, like a stressful situation, sipping coffee, going to a party, or smelling cigarette smoke.
Most triggers fall into one of these four categories:
- Emotional Triggers:
- Many people smoke when they have intense emotions. An emotional trigger reminds you how you felt when you used smoking to enhance a good mood or escape a bad one, like when you were:
- Stressed. Smokers often deal with stress by smoking. Stress can be caused by anything from major life events to daily hassles that add up over time.
- Anxious
- Excited
- Bored
- Down
- Happy
- Lonely
- Satisfied
- Cooled off after a fight
- Stressed. Smokers often deal with stress by smoking. Stress can be caused by anything from major life events to daily hassles that add up over time.
- Pattern Triggers: A pattern trigger is an activity that you connect with smoking. Some examples of these activities include:
- Talking on the phone
- Drinking alcohol
- Watching TV
- Driving
- Finishing a meal
- Drinking coffee
- Taking a work break
- After having sex
- Before going to bed
- Social Triggers: Social triggers are occasions that usually include other people who smoke. Some examples of social triggers include:
- Going to a bar
- Going to a party or other social event
- Going to a concert
- Seeing someone else smoke
- Being with friends who smoke
- Celebrating a big event
- Withdrawal Triggers: If you’ve been a long-time smoker, your body is used to getting a regular dose of nicotine. When you quit, nicotine withdrawal symptoms will produce cravings for nicotine. Nicotine withdrawal triggers include:
- Craving the taste of a cigarette
- Smelling cigarette smoke
- Handling cigarettes, lighters, and matches
- Needing to do something with your hands or mouth
- Feeling restless or having other withdrawal symptoms
- Many people smoke when they have intense emotions. An emotional trigger reminds you how you felt when you used smoking to enhance a good mood or escape a bad one, like when you were:
Knowing your triggers and understanding the best way to deal with them is your first line of defense.
How do I get through the rough spots after I quit smoking?
- For the first few days after you quit smoking or using smokeless tobacco, spend as much free time as you can in public places where tobacco products are not allowed. Libraries, malls, museums, theaters, restaurants without bars or patios, and churches are most often smoke-free.
- Take extra care of yourself. Drink water, eat well, and get enough sleep. This could help you have the energy you might need to handle extra stress.
- Don’t drink alcohol, coffee, or any other drinks you link with using tobacco for at least a couple of months. Try something else instead – maybe different types of water, sports drinks, or 100% fruit juices. Try to choose drinks that are low- or no-calorie.
- If you miss the feeling of having a cigarette in your hand, hold something else – a pencil, a paper clip, a coin, or a marble, for example.
- If you miss the feeling of having something in your mouth, try toothpicks, cinnamon sticks, sugarless gum, sugar-free lollipops, or celery. Some people chew on a straw or stir stick.
- Avoid temptation – stay away from activities, people, and places you link with using tobacco.
- Create new habits and a tobacco-free environment around you.
- Get ready to face future situations or crises that might make you want to smoke or chew again, and think of all the important reasons you’ve decided to quit. To remind yourself of these reasons, put a picture of the people who are the most important to you somewhere you see it every day, or keep one handy on your phone.
- Take deep breaths to relax. Picture your lungs filling with fresh, clean air.
- Remember your goal and the fact that the urge will lessen over time.
- Think about how awesome it is that you’re getting healthier. If you start to weaken, remember your goal. Remember that quitting is a learning process. Be patient with yourself.
- Brush your teeth and enjoy that fresh taste.
- Exercise in short bursts (try alternately tensing and relaxing muscles, push-ups, lunges, walking up the stairs, or touching your toes).
- Call a friend, family member, use a mobile app that connects you with others, or a telephone quitline when you need extra help or support.
- Eat 4 to 6 small meals during the day instead of 1 or 2 large ones. This keeps your blood sugar levels steady, your energy balanced, and helps prevent urges to smoke or chew. Avoid sugary or spicy foods that could be triggers.
- Reward yourself for doing your best. Give yourself rewards often if that’s what it takes to keep going. Plan to do something fun.
How to deal with cigarette cravings
Cigarette cravings are real, it’s not just your imagination. When you feel a strong urge to smoke you may also notice that your mood changes, and your heart rate and blood pressure may go up, too. Try these tips to get through these times, and hang in there – the cravings will get better.
- Keep substitutes handy that you can suck or chew on, such as carrots, pickles, apples, celery, raisins, or sugar-free gum or hard candy.
- Know that anger, frustration, anxiety, irritability, and even depression are normal after quitting and will get better as you learn ways to cope that don’t involve tobacco. See your doctor if these feelings last for more than a month.
- Go for a walk. Exercise can improve your mood and relieve stress.
- Take a shower or bath.
- Learn to relax quickly and deeply. Think about a soothing, pleasing situation, and imagine yourself there. Get away from it all for a moment. Focus on that peaceful place and nothing else.
- Light incense or a candle instead of a cigarette.
- Tell yourself “no.” Say it out loud. Practice doing this a few times, and listen to yourself. Some other things you can say to yourself might be, “I’m too strong to give in to cravings,” “I don’t use tobacco anymore,” or “I will not let my friends and family down.” And most important, “I will not let myself down.”
- Never let yourself think that “just one slip won’t hurt,” because it very likely will.
- Wear a rubber band around your wrist. Whenever you think about smoking or chewing, snap it against your wrist to remind yourself of all the reasons that made you want to quit in the first place. Then remember that you won’t always need a rubber band to help you stay with your plans to quit.
How to deal with cigarette cravings with exercise
Having cravings for a cigarette is one of the most common symptoms of nicotine withdrawal when you quit smoking. It helps to have a plan to manage cravings when they hit. Including exercise in your plan can help you get past cravings. Exercise can distract you and keep you busy until the craving passes.
Exercise has other benefits too:
- Studies show that even short periods of physical activity, especially aerobic exercise, reduce the urge to smoke. Aerobic exercise is physical activity that makes you sweat, causes you to breathe harder, and gets your heart beating faster. It strengthens your heart and lungs. Walking, swimming, running, dancing, cycling, and boxing are a few types of aerobic exercise.
- Withdrawal symptoms and cravings for cigarettes decrease during exercise and up to 50 minutes after exercising.
- Exercise decreases appetite and helps limit the weight gain some people have when they quit smoking.
- Exercise helps you cope with stress and have more energy.
- Exercise can improve your mood. If you’re feeling low, take a walk, jump rope, or run up and down the stairs.
Here are some tips to get you started with exercise and help you ride out cigarette cravings:
- Try to set aside a regular time for exercise that works with your schedule.
- Try for 30 minutes of physical activity most days of the week. Don’t have 30 minutes? Studies show that exercising for 10 minutes three times a day gives the same benefits as 30 minutes of non-stop exercise.
- Do activities you enjoy. Walking is one way of getting more physical activity. You might also think about biking, swimming, dancing, or yoga. Even housework or gardening can provide exercise benefits. Playing music while you clean out your closets will help you step up the pace.
- Build exercise into other activities. Take the stairs at work instead of the elevator. At the mall, use the stairs instead of the escalator. Wherever you go, park your car farther away and walk to your destination.
- Plan activities with family, friends, or co-workers that include physical activity. Maybe a hike or volleyball game.
- Change your exercise routine or try a new activity from time to time so you don’t get bored.
What can I do about anger, frustration, and irritability after I quit?
After you quit smoking or using other tobacco products, you may feel edgy and short-tempered, and you may want to give up on tasks more quickly than usual. You may be less tolerant of others and get into more arguments.
Studies have found that the most common negative feelings associated with quitting are feelings of anger, frustration, and irritability. These negative feelings peak within 1 week of quitting and may last 2 to 4 weeks 34.
Here are some tips for managing these negative feelings:
- Remind yourself that these feelings are temporary.
- Engage in an enjoyable physical activity, such as taking a walk.
- Reduce caffeine by limiting or avoiding coffee, soda, and tea.
- Try meditation or other relaxation techniques, such as getting a massage, soaking in a hot bath, or breathing deeply through your nose and out through your mouth for 10 breaths.
- Try nicotine replacement products or ask your doctor about other medications.
What can I do about anxiety after I quit?
Within 24 hours of quitting smoking or other tobacco products, you may feel tense and agitated. You may feel a tightness in your muscles—especially around the neck and shoulders. Studies have found that anxiety is one of the most common negative feelings associated with quitting. If anxiety occurs, it usually builds over the first 3 days after quitting and may last several weeks (1).
Here are some tips for dealing with your anxiety:
- Remind yourself that anxiety will pass with time.
- Set aside some quiet time every morning and evening—a time when you can be alone in a quiet environment.
- Engage in an enjoyable physical activity, such as taking a walk.
- Reduce caffeine by limiting or avoiding coffee, soda, and tea.
- Try meditation or other relaxation techniques, such as getting a massage, soaking in a hot bath, or breathing deeply through your nose and out through your mouth for 10 breaths.
- Try nicotine replacement products or ask your doctor about other medications.
What can I do about depression after I quit?
It is common to feel sad for a period of time soon after you quit smoking or using other tobacco products. If mild depression occurs, it will usually begin within the first day, continue for a couple of weeks, and go away within a month.
People who have a history of depression often have more-severe withdrawal symptoms, including more-severe depression. Some studies have found that many people with a history of major depression will have a new major depressive episode after quitting (5, 6). However, in those with no history of depression, major depression after quitting is rare.
Many former smokers and people who are quitting have a strong urge to smoke when they feel depressed. Here are some tips for managing feelings of depression:
- Get together with a friend.
- Identify your specific feelings at the time that you seem depressed. Are you actually feeling tired, lonely, bored, or hungry? Focus on and address these specific needs.
- Participate in physical activities that you find enjoyable. This will help to improve your mood, decrease your fatigue, and reduce your depression.
- Breathe deeply.
- Make a list of things that are upsetting to you and write down solutions for them.
- Ask your doctor about prescription medications that may help you with depression. Studies show that bupropion and nortriptyline can help people with a past history of depression who try to quit smoking. Nicotine replacement products may also help 37.
How can I start the day without smoking?
Many smokers light up a cigarette right after they wake up. After 6 to 8 hours of sleep, a smoker’s nicotine level drops and they need a boost of nicotine to start the day. After you quit, you must be ready to overcome the physical need and routine of waking up and smoking a cigarette. Instead of reaching for your cigarettes in the morning, here are some tips:
- The morning can set the tone for the rest of the day. Plan a different wake-up routine to divert your attention from smoking.
- Be sure no cigarettes are available. Instead, keep sugar-free gum, mints, or nuts in the locations where you previously kept your cigarettes so when you automatically reach for cigarettes a healthy alternative is at hand.
- Before you go to sleep, make a list of things you need to avoid in the morning that will make you want to smoke. Place this list where you used to place your cigarettes.
- Begin each day with a planned activity that will keep you busy for an hour or more. Keeping your mind and body busy will distract you from thinking about smoking.
- Begin each day with deep breathing and by drinking one or more glasses of water.
How can I resist the urge to smoke when I’m feeling stressed?
Most smokers report that one reason they smoke is to handle stress. Smoking cigarettes causes temporary changes in your brain chemistry that can cause you to experience decreased anxiety, enhanced pleasure, and alert relaxation. Once you stop smoking and your brain chemistry returns to normal, you may become more aware of stress.
Everyday worries, responsibilities, and annoyances can all contribute to stress. As you go longer without smoking, you will get better at handling stress, especially if you learn stress reduction and relaxation techniques.
Here are some tips:
- Know the causes of stress in your life (your job, traffic, your children, money) and identify the stress signals (headaches, nervousness, or trouble sleeping). Once you pinpoint high-risk trigger situations, you can start to develop new ways to handle them.
- Create peaceful times in your schedule. For example, set aside an hour where you can get away from other people and your usual environment. Or try visualizing yourself in a peaceful setting.
- Try relaxation techniques, such as progressive muscle relaxation or yoga, and stick with the one that works best for you.
- Try this breathing exercise: Take a deep breath through your nose and blow out slowly through your mouth. Repeat 10 times.
- Try meditation involving focused breathing or repetition of words or phrases to quiet your mind.
- Rehearse and visualize your relaxation plan. Put your plan into action. Change your plan as needed.
- You may find it helpful to read a book about how to handle stress.
How can I resist the urge to smoke when I’m driving or riding in a car?
You may have become used to smoking while driving—to relax in a traffic jam or to stay alert on a long drive. Like many smokers, you may like to light up when driving to and from work to relieve stress, stay alert, relax, or just pass the time.
Tips for short trips:
- Remove the ashtray, lighter, and cigarettes from your car.
- Keep healthy substitutions, such as sugar-free gum, mints, or nuts, in your car.
- Turn on your favorite music and sing along.
- Take an alternate route to work or try carpooling.
- Clean your car and use deodorizers to reduce the tobacco smell.
- Tell yourself:
- “This urge will go away in a few minutes.”
- “So, I’m not enjoying this car ride. Big deal! It won’t last forever!”
- “My car smells clean and fresh!”
- “I’m a better driver now that I’m not smoking while driving”
When you are driving or riding with other people:
- Do not allow passengers to smoke in your car.
- If you’re not driving, find something to do with your hands.
Your desire to smoke may be stronger and more frequent on longer trips. On long trips:
- Take stretch breaks.
- Take healthy snacks along.
- Plan rest stops.
How can I resist the urge to smoke when I’m having coffee or tea?
You may be used to smoking when drinking coffee or tea (for example, during or after meals or during work breaks), and you may associate good feelings with drinking a hot beverage. When you give up smoking, expect to feel a strong urge to reach for a cigarette while drinking coffee or tea. Some people quit drinking coffee or tea temporarily while they’re quitting cigarettes to avoid the urge to smoke. Although you do not have to give up coffee or tea to quit smoking, you should expect that coffee or tea will not taste the same without a cigarette.
Here are some tips:
- If you used to smoke while drinking coffee or tea, tell people you have quit, so they won’t offer you a cigarette.
- Between sips of coffee or tea, take deep breaths to inhale the aroma. Breathe in deeply and slowly while you count to five, and then breathe out slowly, counting to five again.
- Try changing your routine around drinking coffee or tea. For example, try switching what drink you consume or try having your coffee or tea in a different location than when you were smoking to help change the routine.
- Keep your hands busy by nibbling on healthy foods, doodling, playing games on your phone, or making a list of tasks for the day.
- If the urge to smoke is very strong, drink your coffee or tea more quickly than usual and then change activities or rooms.
- When you quit smoking, drinking coffee or tea without smoking may make you feel sad. Focus on what you’ve gained by quitting.
How can I resist the urge to smoke when I’m enjoying a meal?
Food often tastes better after you quit smoking, and you may have a bigger appetite. Expect to want to smoke after meals. Your desire to smoke after meals may depend on whether you are alone, with other smokers, or with nonsmokers.
Your urge to smoke may be stronger with certain foods, such as spicy or sweet foods. Also, the urge to smoke may be stronger at different mealtimes.
Here are some tips:
- Know what kinds of foods increase your urge to smoke and stay away from them.
- If you are alone, call a friend or take a walk as soon as you’ve finished eating.
- Brush your teeth or use mouthwash right after meals.
- Wash the dishes by hand after eating—you can’t smoke with wet hands!
How can I resist the urge to smoke when I’m drinking an alcoholic beverage?
You may be used to smoking when drinking beer, wine, liquor, or mixed drinks. When you quit smoking, you may feel a strong urge to smoke when you drink alcohol. Know this up front if you are going to drink because your ability to resist triggers to smoke may be impaired under the influence of alcohol.
Here are some tips for the first few weeks after quitting smoking:
- Many people find it helpful to drink less alcohol or avoid it completely.
- If you do drink, choose different alcoholic beverages than you used to have when smoking.
- Stay away from the places you usually drink alcohol.
How can I resist the urge to smoke when I’m feeling bored?
When you quit smoking, you may miss the increased excitement and good feeling that nicotine gave you. This may be particularly true when you are feeling bored.
Here are some tips:
- Plan more activities than you have time for.
- Make a list of things to do when confronted with free time.
- Get active. Do not stay in the same place too long.
- If you feel bored when waiting for something or someone (a bus, your friend, your kids), distract yourself with a book, magazine, puzzle, or your phone.
- Look at and listen to what is going on around you.
- Carry something to keep your hands busy.
- Listen to a favorite song.
- Go outdoors, if you can, but not to places you associate with smoking.
How to deal with emotional triggers
Managing stress is a key part of quitting smoking. Here are a few ideas you might find helpful. Some of these tips may take practice, but others you can do right away. Try one or more to learn what works for you.
You can learn how to cope with your feelings without leaning on cigarettes. Try these ways to deal with emotional triggers and stress:
- Talk about your emotions. You don’t have to deal with stress alone. Telling a friend or family member how you feel can help.
- Locate your stress. Take a minute to figure out how stress affects your body. Where do you feel tension in your body? Finding ways to reduce that tension will also help your mental stress. A warm bath, a massage, or stretching can help you release built-up tension.
- Take some slow, deep breaths. Take a few slow, deep breaths—in through your nose, out through your mouth. Deep breathing will slow down your body, quiet your mind, and reduce cravings. This is also a great way to manage stress and anxiety.
- Exercise. Physical activity is a great way to handle emotions. When you exercise, your brain releases endorphins. Endorphins are chemicals in the brain that make you feel good and reduce your stress. Sometimes a short walk is all it takes to relieve stress. And walking is free!
- Listen to calming music. Music can relax you by slowing your heart rate, lowering blood pressure, and decreasing stress hormones.
- Visualize. Think of a place where you feel safe, comfortable, and relaxed. Picture it as clearly as you can, including imagining what you would feel, hear, and maybe even smell if you were in that relaxing place. Let yourself enjoy being there for a few minutes.
- Focus. Life can sometimes be overwhelming. Try not to get caught up in worrying about what’s next. Instead, try to focus on what is happening now, not what you might have to deal with in the future.
- Take care of yourself. Make an extra effort to take care of yourself. This includes basic things like eating a balanced diet, drinking lots of water, and getting enough sleep.
- Do Good for others. Doing something nice for others can make your day a little better too. Being caring toward others helps you reduce your own stress.
- Decaffeinate. Caffeine can help you stay awake, but it also can make you feel tense, jittery, and stressed. Cutting back or even doing away with caffeine can help reduce your feelings of stress. Switching to herbal tea or even hot water with lemon gives you a chance to enjoy a hot beverage but without the caffeine.
- Acceptance. Life is full of twists and turns. You’ll always have some stress in your life. It helps to understand that there will be good days and bad days.
- Relax. Your body responds to stress by releasing hormones that increase your heart rate and raise your blood pressure. Practicing relaxation techniques, like the ones below, may improve your health and help you handle your stress in positive ways.
How to boost your mood
Mood changes are common after quitting smoking. You might be irritable, restless, or feel down or blue. If you have these feelings after quitting smoking, there are things you can do to help lift your mood.
- Stay active. Any kind of exercise or physical activity can help. Taking a walk, going to the gym, or joining a team sport are a few you might try. If you need to, start small and build up over time. This can be hard to do when you are feeling down, but making the effort can pay off.
- Structure your day. Create a plan to stay busy. Try to get out of the house whenever you can.
- Do things with other people. Some people who are feeling down are cut off from others. Having regular contact with other people can help your mood. Try to connect with people regularly, whether it’s in person, over the phone, or via text message.
- Build rewards into your life. For many people who are sad, rewards and fun activities are missing from their lives. Finding ways to reward yourself can help lift your mood. Even small things, like reading a magazine or listening to music, can add up and help you feel better.
- Do what used to be fun. One of the common signs of depression is not wanting to do activities that used to be fun. It may be hard, but you might try doing fun activities again to help improve your mood. Try making a list of activities or events that you enjoy and plan to do one a day.
- Get support. You don’t have to deal with negative moods alone. Social support is key to achieving a stable and solid, smoke-free life. Getting support from the important people in your life can make a big difference when you quit smoking. Your friends, family, and others who are important to you can support you. Let them know what they can do to help.
How to deal with pattern triggers
A pattern trigger is an activity that you connect with smoking. Some examples of pattern triggers include drinking coffee, drinking alcohol, after having sex, talking on the phone and driving.
One way to beat pattern triggers is to break the association with the trigger and transfer the feeling to another activity:
- Find a replacement. Chew gum. Eat sugar-free candy. Suck on a straw.
- Try activities that keep your hands busy. Squeeze a handball. Do beading or needlework. Hold on to a silver dollar or “worry stone.”
- Stay active. Go for a walk. Ride a bike. Go swimming. Exercising can distract you from smoking.
- Change your routine. For example, try drinking your coffee at a different time or brushing your teeth right after you eat a meal.
Social triggers are occasions that usually include other people who smoke. Some examples of social triggers include going to a bar, going to a concert, being with friends who smoke and celebrating a big event. Once you’ve made the decision to quit, it is best to avoid places where people smoke and ask your friends not to smoke around you. Over time, it will get easier. Tell your friends and family that you have quit. Ask them for their support.
How to control your weight gain after quitting
Many people delay quitting smoking because they are worried about gaining weight. While many smokers gain some weight after they quit, it is better for your health if you quit as soon as possible. Once you quit, you can begin to build healthy habits for exercise, nutrition, and—if necessary—weight loss.
Here is how you can control weight gain after quitting:
- Control your appetite. Smoking cigarettes makes you feel less hungry. When you quit smoking, you might feel hungrier and eat more than you used to eat. Portion control can help you prevent overeating. And make sure you stay hydrated. It will keep you from eating when you are actually thirsty.
- Start exercising regularly. Smoking cigarettes increases your metabolism, so you burn more calories. When you stop smoking, you may burn fewer calories, which can lead to weight gain. Regular exercise can help you continue to burn those calories. Just 10 minutes of exercise a day can make a difference.
- Eat mindfully. Eating can become a substitute for smoking. It doesn’t have to. Learn how to eat mindfully. Mindful eating means preparing, choosing, and eating with awareness. Here are some tips to help you eat healthier and enjoy your food more:
- Avoid distractions. Turn off the phone, television, and computer.
- Eat at your dinner table so you can focus on eating.
- Think carefully about your portion sizes. Consider starting with a smaller portion.
- Avoid serving food family style. If you still feel hungry, you will have to get up from the table for seconds.
- Do a gut check. Are you really hungry or eating for some other reason?
- Learn to cope with emotions without cigarettes. When you stop smoking, you may want to turn to eating when you feel bad or life is stressful. But you can learn other ways to cope without smoking.
How to deal with nicotine withdrawal triggers
Many people use quit smoking medications to help reduce withdrawal feelings and cigarette cravings. Quit smoking medications can double your chances of quitting for good.
Nicotine replacement therapy (NRT) is a medicine that provides you with a low level of nicotine, without the tar, carbon monoxide and other poisonous chemicals present in tobacco smoke. Nicotine replacement therapy (NRT) is the most commonly used family of quit smoking medications. Nicotine replacement therapy (NRT) reduces withdrawal feelings by giving you a small controlled amount of nicotine, but none of the other dangerous chemicals found in cigarettes. This small amount of nicotine helps satisfy your craving for nicotine and reduces the urge to smoke.
Doctors and other medical experts think nicotine replacement therapy (quit smoking medications) is the one of the most helpful tools smokers can use to quit. Some smokers have mild to moderate side effects. However, research shows that nicotine replacement therapy (quit smoking medications) is safe and effective. Nicotine replacement therapy (quit smoking medications) can be an important part of almost every smoker’s quit smoking strategy.
Nicotine replacement therapy (NRT) comes in a variety of forms that are used in different ways. You can choose which forms you like best. Some nicotine replacement therapy (quit smoking medications) products work better than others for some people. Some people might prefer certain nicotine replacement therapy (quit smoking medications) products instead of others.
Nicotine replacement therapy (quit smoking medications) can be bought from pharmacies over-the-counter (OTC) and some shops. It’s also available on prescription from a doctor or some stop smoking service.
Nicotine replacement therapy (NRT) is available as:
- Skin patches: Patches release nicotine slowly. Some are worn all the time and some should be taken off at night. If you have pregnancy-related nausea and vomiting, patches may be a better solution. Nicotine replacement therapy patches should be used for no more than 16 hours in any 24-hour period. The best way to remember this is to remove the patch at bedtime.
- Chewing gum
- Inhalators which look like plastic cigarettes
- Tablets, microtabs, oral strips and lozenges
- Nasal and mouth spray
Inhalators, gum and sprays act more quickly and may be better for helping with cravings.
There’s no evidence that any single type of nicotine replacement therapy (quit smoking medications)is more effective than another. But there is good evidence to show that using a combination of nicotine replacement therapy (quit smoking medications) is more effective than using a single product.
Often the best way to use nicotine replacement therapy (quit smoking medications) is to combine a skin patch with a faster acting form such as gum, inhalator or nasal spray.
Treatment with nicotine replacement therapy (quit smoking medications) usually lasts 8-12 weeks, before you gradually reduce the dose and eventually stop.
Stop smoking support groups and programs
Your healthcare provider can refer you to stop smoking programs. These are offered by hospitals, health departments, community centers, work sites, and national organizations. Nicotine Anonymous (https://www.nicotine-anonymous.org). Nicotine Anonymous uses a similar approach as Alcoholics Anonymous. As part of this group, you will be asked to admit that you are powerless over your addiction to nicotine. Also, a sponsor is often available to help you get through urges to smoke.
The best smoking cessation programs combine numerous approaches and target the fears and problems you have when quitting. They also provide ongoing support for staying away from tobacco.
Be wary of stop smoking programs that:
- Are short and offer no help over time
- Charge a high fee
- Offer supplements or pills that are only available through the program
- Promise an easy path to quitting
Stop smoking programs and classes
Stop smoking programs can also help you find a quitting method that suits your needs. They will help you be aware of problems that come up while you’re trying to quit and offer tools to cope with these problems. These programs can help you avoid making common mistakes.
Stop smoking programs may either have one-on-one sessions or group counseling. Some programs offer both. Programs should be run by counselors who are trained to help people quit smoking.
Stop smoking programs that provide more sessions or longer sessions have a better chance of success. The American Cancer Society recommends Stop smoking programs with the following features:
- Each session lasts at least 15 to 30 minutes.
- There are at least 4 sessions.
- The program lasts at least 2 weeks, although longer is usually better.
- The leader is trained in smoking cessation.
Internet-based Stop smoking programs are also becoming more available. These services send you personalized reminders using e-mail, texting, or other methods.
Telephone-based services can also help you design a stop smoking program that meets your needs. These services are easy to use. The counselors can help you avoid common mistakes. This kind of support can be as effective as face-to-face counseling.
Telephone stop smoking programs are often available on nights and weekends. Trained counselors will help you set up a support network for quitting and help you decide which stop smoking aids to use. Choices may include:
- Medicines
- Nicotine replacement therapy (NRT)
- Support programs or classes
Staying tobacco free
The first few weeks after quitting can be hard for anyone. And staying away from tobacco may be extra tough especially during a holiday season, when stress and the temptation to overindulge are often worse. Many of these ideas can also help throughout the year.
Celebrate being tobacco-free and try these tips to keep your mind off smoking:
- Think about being a host. Consider hosting the family dinner to keep yourself busy. Shopping and cooking will certainly take up a lot of your time. If you’d prefer being a guest this year, maybe you can make a special dish to take with you.
- Don’t overdo it. You might be inclined to go overboard with the holiday feasting. Be aware of how much you’re eating and drinking; it may be easy to give in to these other temptations. If you do overdo it, forgive yourself. Remember, next year it won’t be as hard.
- Try to stay away from alcohol. Stick to sugar-free seltzer, punch without alcohol, club soda, or apple cider. This will curb the urge to light up when drinking and can also help keep off extra pounds.
- Avoid spicy and sugary foods. Spicy and sugary foods tend to make people crave cigarettes more.
- Nibble on low-calorie foods. Low-calorie foods such as carrot sticks, apples, and other healthy snacks, can help satisfy your need for crunch without adding extra pounds.
- Stretch out meals. Eat slowly and pause between bites to make a meal more satisfying. For dessert, grab an orange or tangerine, or crack some nuts – something that will keep your hands busy, too.
- Keep busy at parties. Serving snacks and meeting guests will help keep your mind off smoking. If the urge to smoke or chew presents itself, put something in your hand other than a cigarette.
- Treat yourself to something special. Celebrate staying quit. Think about buying yourself something special you’ve been wanting.
- Learn to cope with frustration. Any added frustration can leave you wanting a cigarette or a dip. Take along your favorite magazine or book, check your email, or text a friend while waiting in lines. When you feel you’re about to lose control, stop and think. Take hold of yourself and start talking with someone in line next to you, or start looking at what you brought with you.
If you have a weak moment and slip, don’t panic. Take a deep breath. Remind yourself of your commitment to quit, and all the reasons you quit. Commit to going back to your quit program right away. Destroy any tobacco products you have before you’re tempted again. Try to figure out why you had a setback and learn from it.
How to quit smoking without using medicines
Cold turkey and gradual withdrawal
A lot of people who smoke quit cold turkey – they stop completely, all at once, with no medicines or nicotine replacement therapy (NRT). You may hear that more people quit cold turkey than by using assistance. That is true, but it reflects the fact that so many more people use the cold turkey method. In fact, the chances of a successful quit attempt are much higher when someone uses assistance.
Another way is gradual withdrawal – cutting down on the number of cigarettes you smoke a little bit each day. This way, you slowly reduce the amount of nicotine in your body. You might cut out cigarettes smoked with a cup of coffee, or you might decide to smoke only at certain times of the day. It makes sense to cut down before your quit date in order to reduce withdrawal symptoms, but this can be hard to do. It’s important to know that merely cutting back (and not quitting) has only minimal health benefits.
Filters
Filters that reduce tar and nicotine in cigarettes do not help people quit smoking, nor do they reduce the health risks from smoking.
Smoking deterrents
Other methods have been used to help stop smoking, such as over-the-counter products that change the taste of tobacco, stop-smoking diets that curb nicotine cravings, and combinations of vitamins. At this time there’s no scientific evidence that any of these work.
Counseling
Medications help you cope by reducing withdrawal symptoms and cravings, while behavioral treatments help you develop the skills you need to give up tobacco for good. The more time you spend with a counselor, the better your treatment results will be.
During individual or group counseling, you learn techniques you can use to help you stop smoking. Many hospitals, health care plans, health care providers and employers offer treatment programs. Some medical centers provide residential treatment programs — the most intensive treatment available.
Hypnosis
Hypnosis methods vary a great deal, which makes it hard to study as a way to stop smoking. For the most part, reviews that looked at controlled studies of hypnosis to help people quit smoking have not found that it’s a quitting method that works. Still, some people say that it helps. If you’d like to try it, ask your health care provider to recommend a good licensed therapist who does hypnotherapy.
Acupuncture
Acupuncture has been used to help people quit smoking, but there’s little evidence to show that it works. Acupuncture for smoking is usually done on certain parts of the ears.
Magnet therapy
Magnet therapy to quit smoking involves 2 small magnets that are put in a certain spot, opposite each other on either side of the ear. Magnetism holds them in place. There’s no scientific evidence to date to suggest that magnet therapy helps people stop smoking. There are many on-line companies that sell these magnets, and they report various “success” rates. But there’s no clinical trial data to back up these claims.
Cold laser therapy
Cold laser therapy also called low level laser therapy, and is related to acupuncture. In this method, cold lasers are used instead of needles for acupuncture. Despite claims of success by some cold laser therapy providers, there’s no scientific evidence that shows this helps people stop smoking.
Herbs and supplements
There’s little scientific evidence to support the use of homeopathic aids and herbal supplements as stop-smoking methods. Because they are marketed as dietary supplements (not drugs), they don’t need FDA approval to be sold. This means that the manufacturers don’t have to prove they work, or even that they’re safe.
Be sure to look closely at the label of any product that claims it can help you stop smoking. No dietary supplement has been proven to help people quit smoking. Most of these supplements include combinations of herbs, but not nicotine. They have no proven track record of helping people to stop smoking.
Mind-body practices
Some studies have looked at cessation programs using yoga, mindfulness, and meditation to aid in quitting smoking. Results were not clearly in favor of these methods, but some did show lower craving and less smoking. More research is needed, and studies of these practices are still going on. Cognitive processing methods (cognitive-behavioral approaches) are also being studied.
References- American Psychiatric Association . Diagnostic and statistical manual of mental disorders: DSM 5. American Psychiatric Association; Washington: 2013.
- Tiwari RK, Sharma V, Pandey RK, Shukla SS. Nicotine Addiction: Neurobiology and Mechanism. J Pharmacopuncture. 2020 Mar 31;23(1):1-7. doi: 10.3831/KPI.2020.23.001
- Sandhu A, Hosseini SA, Saadabadi A. Nicotine Replacement Therapy. [Updated 2023 Nov 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK493148
- Widysanto A, Combest FE, Dhakal A, et al. Nicotine Addiction. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499915
- Sandborn WJ. Nicotine therapy for ulcerative colitis: a review of rationale, mechanisms, pharmacology, and clinical results. Am J Gastroenterol. 1999 May;94(5):1161-71. doi: 10.1111/j.1572-0241.1999.01059.x
- McClernon FJ, Hiott FB, Westman EC, Rose JE, Levin ED. Transdermal nicotine attenuates depression symptoms in nonsmokers: a double-blind, placebo-controlled trial. Psychopharmacology (Berl). 2006 Nov;189(1):125-33. doi: 10.1007/s00213-006-0516-y
- Silver AA, Shytle RD, Philipp MK, Wilkinson BJ, McConville B, Sanberg PR. Transdermal nicotine and haloperidol in Tourette’s disorder: a double-blind placebo-controlled study. J Clin Psychiatry. 2001 Sep;62(9):707-14. doi: 10.4088/jcp.v62n0908
- Anfang MK, Pope HG Jr. Treatment of neuroleptic-induced akathisia with nicotine patches. Psychopharmacology (Berl). 1997 Nov;134(2):153-6. doi: 10.1007/s002130050436
- Gehricke JG, Hong N, Whalen CK, Steinhoff K, Wigal TL. Effects of transdermal nicotine on symptoms, moods, and cardiovascular activity in the everyday lives of smokers and nonsmokers with attention-deficit/hyperactivity disorder. Psychol Addict Behav. 2009 Dec;23(4):644-55. doi: 10.1037/a0017441
- Thiriez C, Villafane G, Grapin F, Fenelon G, Remy P, Cesaro P. Can nicotine be used medicinally in Parkinson’s disease? Expert Rev Clin Pharmacol. 2011 Jul;4(4):429-36. doi: 10.1586/ecp.11.27
- Newhouse P, Kellar K, Aisen P, White H, Wesnes K, Coderre E, Pfaff A, Wilkins H, Howard D, Levin ED. Nicotine treatment of mild cognitive impairment: a 6-month double-blind pilot clinical trial. Neurology. 2012 Jan 10;78(2):91-101. doi: 10.1212/WNL.0b013e31823efcbb
- Fagerström K, Eissenberg T. Dependence on tobacco and nicotine products: a case for product-specific assessment. Nicotine Tob Res. 2012 Nov;14(11):1382-90. doi: 10.1093/ntr/nts007
- Green JT, Thomas GA, Rhodes J, Williams GT, Evans BK, Russell MA, Feyerabend C, Rhodes P, Sandborn WJ. Nicotine enemas for active ulcerative colitis–a pilot study. Aliment Pharmacol Ther. 1997 Oct;11(5):859-63. doi: 10.1046/j.1365-2036.1997.00220.x
- O’Reilly EJ, McCullough ML, Chao A, Henley SJ, Calle EE, Thun MJ, Ascherio A. Smokeless tobacco use and the risk of Parkinson’s disease mortality. Mov Disord. 2005 Oct;20(10):1383-4. doi: 10.1002/mds.20587
- Hedström AK, Hillert J, Olsson T, Alfredsson L. Nicotine might have a protective effect in the etiology of multiple sclerosis. Mult Scler. 2013 Jul;19(8):1009-13. doi: 10.1177/1352458512471879
- Lee PN, Fariss MW. A systematic review of possible serious adverse health effects of nicotine replacement therapy. Arch Toxicol. 2017 Apr;91(4):1565-1594. doi: 10.1007/s00204-016-1856-y
- ASH (Action on Smoking, Health) (2007). Nicotine replacement therapy guidelines for healthcare professionals on using nicotine replacement therapy for smokers not yet ready to stop smoking. (17 pp.). ASH (Action on Smoking, Health) (2012). E-cigarette use in Great Britain: 2010 and 2012.
- Fagerström, K. (2014). Nicotine: Pharmacology, Toxicity and Therapeutic use. Journal of Smoking Cessation, 9(2), 53-59. doi:10.1017/jsc.2014.27
- Clarke, E., Thompson, K., Weaver, S. et al. Snus: a compelling harm reduction alternative to cigarettes. Harm Reduct J 16, 62 (2019). https://doi.org/10.1186/s12954-019-0335-1
- Meyer, B. (2013). How much nicotine kills a human? Tracing back the generally accepted lethal dose to dubious self-experiments in the nineteenth century. Archives of Toxicology, 88, 5–7. 10.1007/s00204-013-1127-0
- Electronic Cigarette Kills Toddler in Israel. https://www.greenprophet.com/2013/05/electronic-cigarette-kills-toddler-in-israel/
- Benowitz NL, Hansson A, Jacob P 3rd. Cardiovascular effects of nasal and transdermal nicotine and cigarette smoking. Hypertension. 2002 Jun;39(6):1107-12. doi: 10.1161/01.hyp.0000018825.76673.ea
- Hubbard R, Lewis S, Smith C, Godfrey C, Smeeth L, Farrington P, Britton J. Use of nicotine replacement therapy and the risk of acute myocardial infarction, stroke, and death. Tob Control. 2005 Dec;14(6):416-21. doi: 10.1136/tc.2005.011387
- Greenland S, Satterfield MH, Lanes SF. A meta-analysis to assess the incidence of adverse effects associated with the transdermal nicotine patch. Drug Saf. 1998 Apr;18(4):297-308. doi: 10.2165/00002018-199818040-00005
- Kimmel SE, Berlin JA, Miles C, Jaskowiak J, Carson JL, Strom BL. Risk of acute first myocardial infarction and use of nicotine patches in a general population. J Am Coll Cardiol. 2001 Apr;37(5):1297-302. doi: 10.1016/s0735-1097(01)01124-x
- Joseph AM, Norman SM, Ferry LH, Prochazka AV, Westman EC, Steele BG, Sherman SE, Cleveland M, Antonuccio DO, Hartman N, McGovern PG. The safety of transdermal nicotine as an aid to smoking cessation in patients with cardiac disease. N Engl J Med. 1996 Dec 12;335(24):1792-8. doi: 10.1056/NEJM199612123352402. Erratum in: N Engl J Med. 2007 Jun 14;356(24):2554.
- Hansson J, Galanti MR, Hergens MP, Fredlund P, Ahlbom A, Alfredsson L, Bellocco R, Eriksson M, Hallqvist J, Hedblad B, Jansson JH, Nilsson P, Pedersen N, Trolle Lagerros Y, Ostergren PO, Magnusson C. Use of snus and acute myocardial infarction: pooled analysis of eight prospective observational studies. Eur J Epidemiol. 2012 Oct;27(10):771-9. doi: 10.1007/s10654-012-9704-8
- Hergens MP, Alfredsson L, Bolinder G, Lambe M, Pershagen G, Ye W. Long-term use of Swedish moist snuff and the risk of myocardial infarction amongst men. J Intern Med. 2007 Sep;262(3):351-9. doi: 10.1111/j.1365-2796.2007.01816.x. Erratum in: J Intern Med. 2007 Nov;262(5):590.
- Baba, S., Wikström, A. K., Stephansson, O., & Cnattingius, S. (2013). Changes in snuff and smoking habits in Swedish pregnant women and risk for small for gestational age births. BJOG: An International Journal of Obstetrics & Gynaecology, 120 (4), 456–462. doi: 10.1111/1471-0528.12067
- Wikström AK, Stephansson O, Cnattingius S. Tobacco use during pregnancy and preeclampsia risk: effects of cigarette smoking and snuff. Hypertension. 2010 May;55(5):1254-9. doi: 10.1161/HYPERTENSIONAHA.109.147082
- Pauly, J. R., & Slotkin, T. A. (2008). Maternal tobacco smoking, nicotine replacement and neurobehavioural development. Acta Paediatrica, 97 (10), 1331–1337. doi: 10.1111/j.1651-2227.2008.00852.x
- Koegelenberg CF, Noor F, Bateman ED, van Zyl-Smit RN, Bruning A, O’Brien JA, Smith C, Abdool-Gaffar MS, Emanuel S, Esterhuizen TM, Irusen EM. Efficacy of varenicline combined with nicotine replacement therapy vs varenicline alone for smoking cessation: a randomized clinical trial. JAMA. 2014 Jul;312(2):155-61. doi: 10.1001/jama.2014.7195
- McLaughlin I, Dani JA, De Biasi M. Nicotine withdrawal. Curr Top Behav Neurosci. 2015;24:99-123. doi: 10.1007/978-3-319-13482-6_4
- John R. Hughes, Effects of Abstinence From Tobacco: Valid Symptoms and Time Course, Nicotine & Tobacco Research, Volume 9, Issue 3, March 2007, Pages 315–327, https://doi.org/10.1080/14622200701188919
- FDA Updates and Press Announcements on Nitrosamine in Varenicline (Chantix). https://www.fda.gov/drugs/drug-safety-and-availability/fda-updates-and-press-announcements-nitrosamine-varenicline-chantix
- Hartmann-Boyce J, Chepkin SC, Ye W, Bullen C, Lancaster T. Nicotine replacement therapy versus control for smoking cessation. Cochrane Database Syst Rev. 2018 May 31;5(5):CD000146. doi: 10.1002/14651858.CD000146.pub5
- Clinical Practice Guideline Treating Tobacco Use and Dependence 2008 Update Panel, Liaisons, and Staff. A clinical practice guideline for treating tobacco use and dependence: 2008 update. A U.S. Public Health Service report. Am J Prev Med. 2008 Aug;35(2):158-76. doi: 10.1016/j.amepre.2008.04.009