Is nipple discharge normal?
Nipple discharge isn’t usually a sign of anything serious, but sometimes it’s a good idea to get it checked just in case. Nipple discharge refers to any fluid that seeps out of the nipple of your breast. Nipple discharge by itself isn’t usually a sign of breast cancer and is most often benign (non-cancerous), but rarely, it can be a sign of breast cancer. It is important to find out what is causing it and to get treatment.
Nipple discharge is the third most common breast complaint after breast pain and breast mass. Fifty percent to 80% of women in their reproductive years had a nipple discharge, and 6.8% of these were referred to a breast surgeon. Most nipple discharge is benign in origin (97%) 1.
Each human breast has 15 to 20 milk ducts. A discharge can come from one or more of these milk ducts (lactiferous ducts) 1.
Nipple discharge is normal during last weeks of pregnancy, after the childbirth and during the breastfeeding period. It can also be normal in women who are not pregnant and are not breastfeeding, especially during reproductive years. Certain manipulations of the breasts, such as fondling, sucking, or massaging can stimulate milk ducts to secrete fluid. Stress also has been shown to cause nipple discharge.
Lots of women have nipple discharge from time to time. You are more likely to have nipple discharge if you have been pregnant at least once. Nipple discharge may just be normal for you. It’s also not unusual for babies (boys and girls) to have milky nipple discharge soon after they’re born. This is caused by hormones from the mother before birth. It should go away in 2 weeks.
Nipple discharge in women who are not pregnant or breast-feeding may not be abnormal, but it’s wise to have any unexpected nipple discharge evaluated by a doctor.
All postmenopausal nipple discharge, however, is significant and requires further evaluation 1. Patient’s age is very important, as women older than 40 years old are at higher risk of having pathologic causes of the nipple discharge. Post-menopausal women with nipple discharge rarely have a benign cause of their symptom.
Nipple discharge in men is always abnormal and also must prompt an evaluation 1.
Nipple discharge has many possible causes.
Common nipple discharge causes include:
- Breastfeeding
- Pregnancy
- Postpartum galactorrhea which may last up to two years after delivery
- After spontaneous or intentional termination of pregnancy
- A blocked or enlarged milk duct
- Fibrocystic changes of breast
- Hormonal fluctuations associated with menstrual cycle
- Duct ectasia
- Intraductal papilloma
- A small, non-cancerous lump in the breast
- A breast infection (mastitis)
- A side effect of certain medicines – including the contraceptive pill
- Use of certain herbs, such as anise and fennel
- Rubbing on the area from a bra or t-shirt
- Injury to the breast
- Inflammation and clogging of the breast ducts
- Noncancerous pituitary tumors
- Severe underactive thyroid gland (hypothyroidism)
- Fibrocystic breast (normal lumpiness in the breast)
- Widening of the milk ducts
The color of your nipple discharge isn’t a good way of telling if it’s anything serious. Normal nipple discharge can have lots of colors. The color of the discharge does not tell you whether it is normal. The nipple discharge can look milky, clear, yellow, green, or brown. About 50% of women in their reproductive years have physiologic nipple discharge that is characterized by bilateral, milky, green or yellow fluid expressed from multiple nipple duct openings and often associated with nipple stimulation 2.
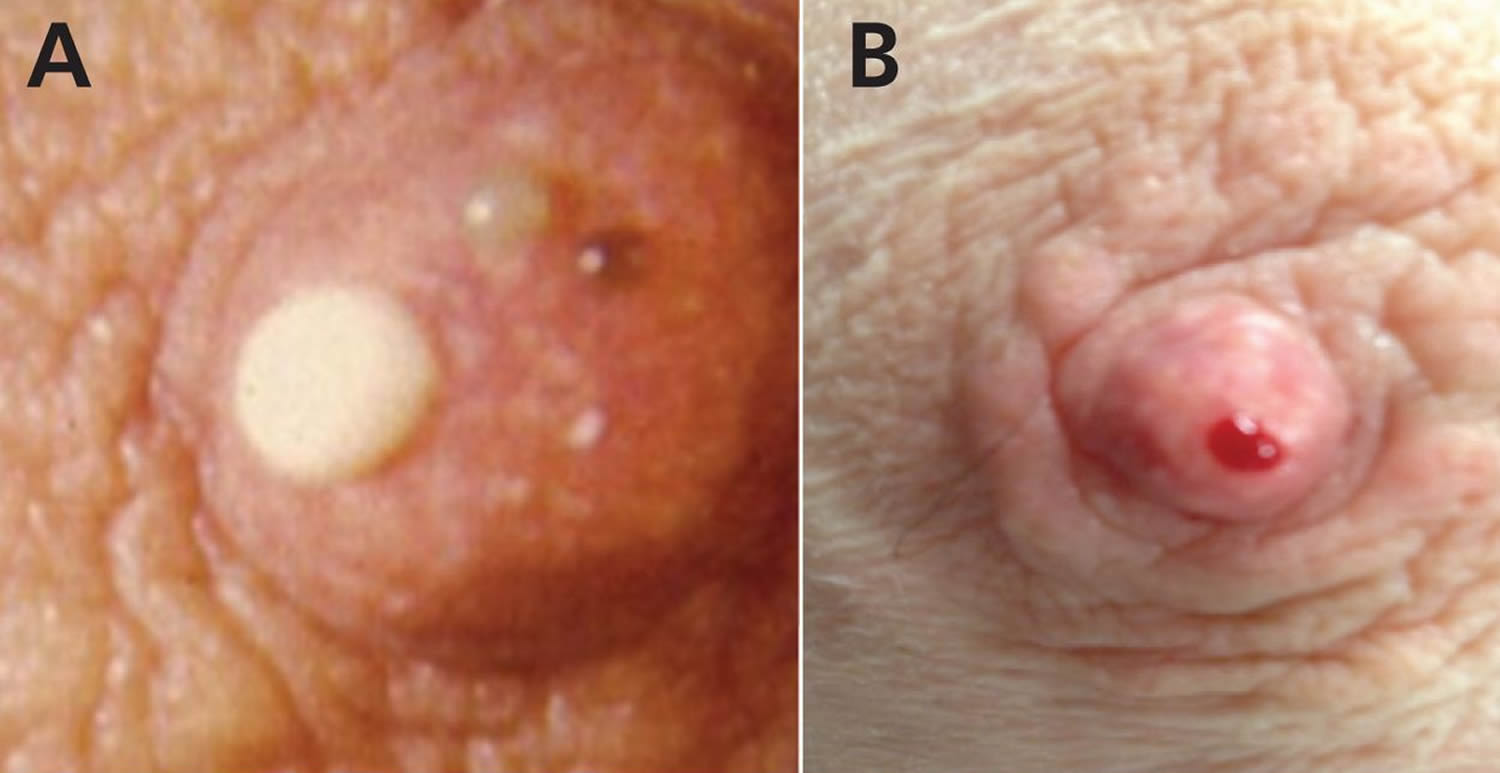
Pathologic nipple discharge is spontaneous and often coming out of one nipple 2. Pathologic nipple discharge may arise from a single duct or be associated with a mass or new skin changes. It can be bloody, serous, green or black 3. Benign intraductal papilloma (48%), ductal ectasia (15%–20%) and carcinoma (10%–15%) are the most common causes 4. All cases of pathologic nipple discharge need tissue diagnosis. Patients with pathologic discharge should have histologic evaluation through surgical excision of the involved duct (if no lesion is identified), or targeted excision of the lesion (if papilloma is identified) via open or needle biopsy 5.
Nipple discharge that is NOT normal is:
- Bloody nipple discharge – blood coming out of one nipple is one of the symptoms of ductal carcinoma in situ (DCIS)
- Comes from only one nipple
- Comes out on its own without you squeezing or touching your nipple
Cancers such as Paget disease (a rare type of cancer involving the skin of the nipple) can also cause nipple discharge.
Nipple discharge is more likely to be normal if it:
- Comes out of both nipples
- Happens when you squeeze your nipples
One or both breasts may produce a nipple discharge, either spontaneously or when you squeeze your nipples or breasts. A nipple discharge may look milky, or it may be clear, yellow, green, brown or bloody. Nonmilk discharge comes out of your nipple through the same nipple openings that carry milk. The consistency of nipple discharge can vary — it may be thick and sticky or thin and watery.
Squeezing your nipple to check for discharge can make it worse. Leaving the nipple alone may make the discharge stop.
Figure 1. Normal breast (female)
Nipple discharge is rarely a sign of breast cancer. But it might be a sign of an underlying condition that requires treatment.
See a doctor if you have nipple discharge and any of these:
- it happens regularly and isn’t just a one-off
- it only comes from 1 breast
- it’s bloodstained or smelly
- you’re not breastfeeding and it leaks out without any pressure on your breast
- you’re over 50
- you have other symptoms – such as a lump, pain, redness or swelling in your breast
- you’re a man
It’s probably nothing serious. But there’s a small chance it could be cancer, so it’s best to get checked.
If you’re still having menstrual periods and your nipple discharge doesn’t resolve on its own after your next menstrual cycle, make an appointment with your doctor to have it evaluated. However, if you’ve completed menopause and you’re experiencing a spontaneous nipple discharge that involves one breast and a single duct, see your doctor right away for further evaluation.
In the meantime, take care to avoid nipple stimulation — including frequent checks for discharge — because stimulation actually makes the nipple discharge continue.
Male nipple discharge
Nipple discharge in men isn’t normal. Nipple discharge in men under any circumstances could be a problem and needs further evaluation.
Nipple discharge causes
Nipple discharge is a normal part of breast function during pregnancy or breast-feeding. It also may be associated with menstrual hormone changes and fibrocystic changes. The milky discharge after breast-feeding will normally affect both breasts and can continue for up to two or three years after stopping nursing.
A papilloma is a noncancerous (benign) tumor that can be associated with bloody discharge. It appears spontaneously and involves a single duct. Although the bloody discharge may resolve on its own, this situation requires evaluation with an ultrasound of the area behind the nipple and areola. If the ultrasound shows a lesion within a milk duct, you may need a biopsy to confirm that it’s a papilloma or to exclude a cancer.
Often, nipple discharge stems from a benign condition.
However, breast cancer is a possibility, especially if:
- You have a lump in your breast
- Only one breast is affected
- The discharge contains blood
- The discharge is spontaneous and persistent
- The discharge affects only a single duct
Possible causes of nipple discharge include:
- Abscess
- Birth control pills
- Breast cancer
- Ductal carcinoma in situ (DCIS)
- Endocrine disorders
- Excessive breast stimulation
- Fibrocystic breasts (lumpy or rope-like breast tissue)
- Galactorrhea
- Injury or trauma to the breast
- Intraductal papilloma (a benign, wartlike growth in a milk duct)
- Mammary duct ectasia
- Mastitis (an infection in breast tissue that most commonly affects women who are breast-feeding)
- A side effect of medications that inhibit dopamine secretion [e.g., opioids, oral contraceptives, antihypertensives (methyldopa, reserpine, verapamil), antidepressants and antipsychotics, prokinetics (e.g., metoclopramide) and H2-blockers (e.g., cimetidine)] 3
- Menstrual cycle hormone changes
- Paget’s disease of the breast
- Periductal mastitis
- Pregnancy and breast-feeding
- Pituitary tumor/prolactinoma
- Systemic disease/endocrinopathies that elevate prolactin level (e.g., hypothyroidism, disorders of the pituitary gland or hypothalamus, chronic kidney or liver disorders)
Nipple discharge possible complications
Nipple discharge may be a symptom of breast cancer or a pituitary tumor.
Skin changes around the nipple may be caused by Paget disease.
Nipple discharge diagnosis
Your doctor will look at and examine your breasts.
Your doctor may refer you to a hospital or breast clinic for further tests. These will usually show that you don’t have cancer.
What happens at the breast clinic
At the hospital or breast clinic, you may have a:
- Breast examination
- Prolactin blood test
- Thyroid blood tests
- Head CT scan or MRI to look for pituitary tumor
- Mammography – a breast X-ray (mammogram)
- Ultrasound of the breast
- Breast biopsy – where a needle is inserted into your breast to remove some cells for testing
- Ductography or ductogram: an x-ray with contrast dye injected into the affected milk duct
- Skin biopsy, if Paget disease is a concern
The tests are often done during the same visit.
You’ll usually be told the results on the same day, although biopsy results can take longer – you should get them in a week or two.
Nipple discharge treatment
Once the cause of your nipple discharge is found, your provider can recommend ways to treat it. You may:
- Need to change any medicine that caused the discharge
- Have lumps removed
- Have all or some of the breast ducts removed
- Receive creams to treat skin changes around your nipple
- Receive medicines to treat a health condition
If all of your tests are normal, you may not need treatment. You should have another mammogram and physical exam within 1 year.
Nipple discharge prognosis
Most of the time, nipple problems are not breast cancer. These problems will either go away with the right treatment, or they can be watched closely over time.
References- Sajadi-Ernazarova KR, Adigun R. Breast, Nipple Discharge. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430938
- Nipple discharge. Sasha Mazzarello, Angel Arnaout. CMAJ May 2015, 187 (8) 599; DOI: 10.1503/cmaj.140633
- Onstad M, Stuckey A. Benign breast disorders. Obstet Gynecol Clin N Am 2013;40:459–73.
- Hussain AN, Policarpio C, Vincent MT. Evaluating nipple discharge. Obstet Gynecol Surv 2006;61: 278–83.
- NCCN clinical practice guidelines in oncology: breast cancer screening and diagnosis: version 1. Fort Washington (PA): National Comprehensive Cancer Network; 2014