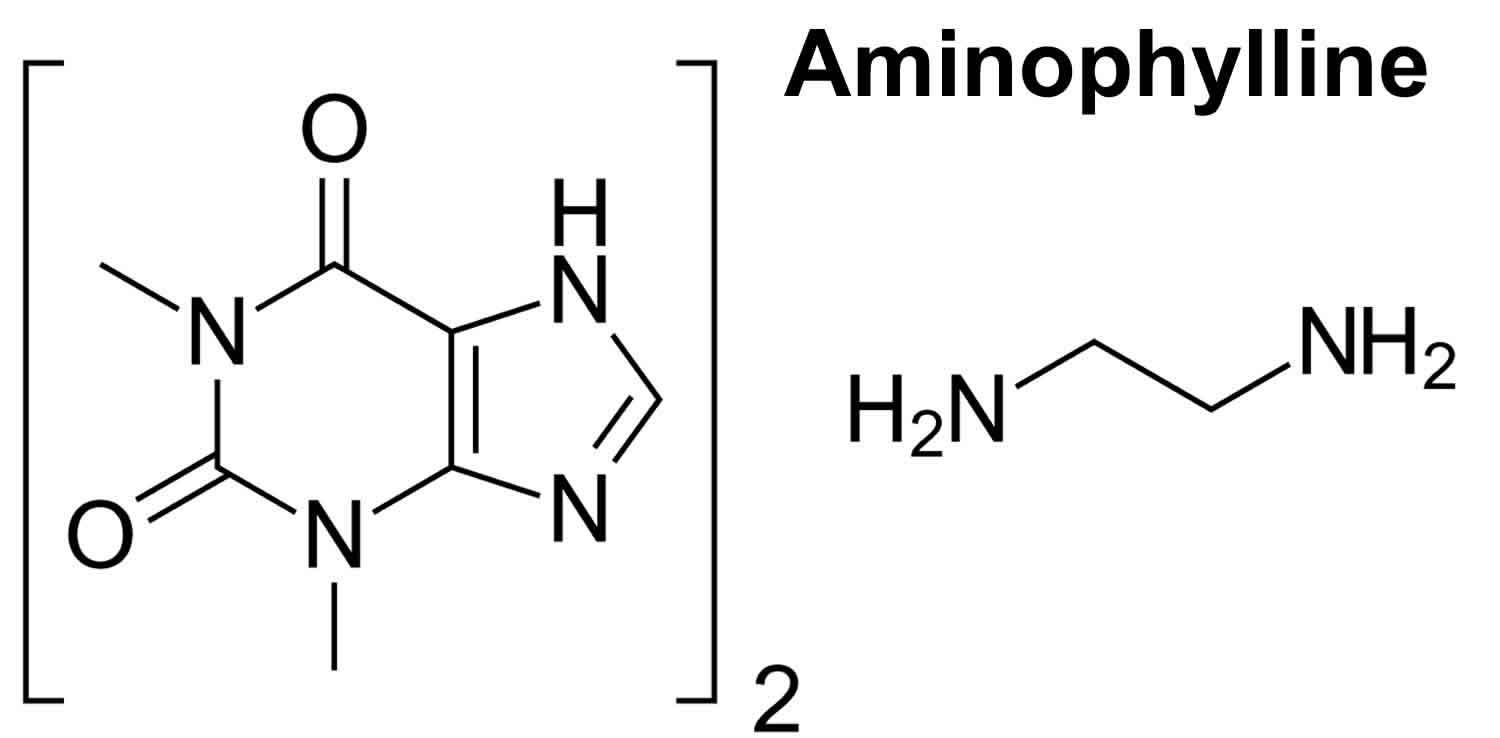
What is aminophylline
Aminophylline is used to prevent and treat wheezing, shortness of breath, and difficulty breathing caused by asthma, chronic bronchitis, emphysema, and other lung diseases. Aminophylline relaxes and opens air passages in the lungs, making it easier to breathe.
Aminophylline belongs to a group of medicines known as bronchodilators. Bronchodilators are medicines that relax the muscles in the bronchial tubes (air passages) of the lungs. They relieve cough, wheezing, shortness of breath, and troubled breathing by increasing the flow of air through the bronchial tubes.
Aminophylline is available only with a doctor’s prescription. Aminophylline is sometimes prescribed for other uses; ask your doctor or pharmacist for more information.
Aminophylline is sometimes used to treat breathing problems in premature infants. Talk to your doctor about the possible risks of using this drug for your baby’s condition.
Aminophylline comes as a tablet and syrup to take by mouth and a suppository to insert rectally. It usually is taken every 6, 8, or 12 hours. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take aminophylline exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Take the tablets or oral liquid with a full glass of water on an empty stomach, at least 1 hour before or 2 hours after a meal. Do not chew or crush the long-acting tablets; swallow them whole.
Aminophylline controls symptoms of asthma and other lung diseases but does not cure them. Continue to take aminophylline even if you feel well. Do not stop taking aminophylline without talking to your doctor.
To insert a aminophylline rectal suppository, follow these steps:
- Remove the wrapper.
- Dip the tip of the suppository in water.
- Lie down on your left side and raise your right knee to your chest. (A left-handed person should lie on the right side and raise the left knee.)
- Using your finger, insert the suppository into the rectum, about 1/2 to 1 inch (1.25 to 2.5 centimeters) in infants and children and 1 inch (2.5 centimeters) in adults. Hold it in place for a few moments.
- Stand up after about 15 minutes. Wash your hands thoroughly and resume your normal activities.
Aminophylline precautions
Before taking aminophylline:
- tell your doctor and pharmacist if you are allergic to aminophylline or any other drugs.
- tell your doctor and pharmacist what prescription medications you are taking, especially allopurinol (Zyloprim), azithromycin (Zithromax) carbamazepine (Tegretol), cimetidine (Tagamet), ciprofloxacin (Cipro), clarithromycin (Biaxin), diuretics (‘water pills’), erythromycin, lithium (Eskalith, Lithobid), oral contraceptives, phenytoin (Dilantin), prednisone (Deltasone), propranolol (Inderal), rifampin (Rifadin), tetracycline (Sumycin), and other medications for infections or heart disease.
- tell your doctor and pharmacist what nonprescription medications and vitamins you are taking, especially nonprescription medications containing ephedrine, epinephrine, phenylephrine, phenylpropanolamine, or pseudoephedrine. Many nonprescription products contain these drugs (e.g., diet pills and medications for colds and asthma), so check labels carefully. Do not take these medications without talking to your doctor; they can increase the side effects of aminophylline.
- tell your doctor if you have or have ever had seizures, heart disease, an overactive or underactive thyroid gland, high blood pressure, or liver disease or if you have a history of alcohol abuse.
- tell your doctor if you are pregnant, plan to become pregnant, or are breast-feeding. If you become pregnant while taking aminophylline, call your doctor.
- tell your doctor if you use tobacco products. Cigarette smoking may affect the effectiveness of aminophylline.
It is very important that your doctor check the progress of you or your child while you receive aminophylline. Blood tests may be needed to check for unwanted effects.
A change in your usual behavior or physical well-being may affect the way aminophylline works in your body. Tell your doctor if you or your child:
- Have had a fever of 102 °F (38.9 °C) or higher for at least 24 hours or more.
- Have started or stopped smoking tobacco or marijuana in the last few weeks.
- Have started or stopped taking another medicine in the last few weeks.
- Have changed your diet in the last few weeks.
Check with your doctor right away if you or your child have the following symptoms after using aminophylline:
- nausea or vomiting that continues, headaches, trouble with sleeping, seizures, or irregular heartbeats.
Before you have any medical tests, tell the medical doctor in charge that you or your child are using aminophylline. The results of some tests may be affected by this medicine.
Aminophylline may add to the central nervous system (CNS) stimulant effects of caffeine-containing foods or beverages such as chocolate, cocoa, tea, coffee, and cola drinks. Avoid eating or drinking large amounts of these foods or beverages while using this medicine. If you have questions about this, check with your doctor.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines for appetite control, asthma, colds, cough, hay fever, or sinus problems, and herbal or vitamin supplements.
What special dietary instructions should I follow?
Drinking or eating foods high in caffeine, like coffee, tea, cocoa, and chocolate, may increase the side effects caused by aminophylline. Avoid large amounts of these substances while you are taking aminophylline.
Aminophylline uses
Aminophylline (and theophylline) are medicines used to treat lung diseases such as asthma, chronic bronchitis, emphysema, and other lung diseases. They help prevent and treat wheezing and other breathing problems.
Aminophylline is sometimes used to treat breathing problems in premature infants. Talk to your doctor about the possible risks of using this drug for your baby’s condition.
Aminophylline contraindications
You must not be given Aminophylline Injection if you have an allergy to aminophylline, theophylline, ethylenediamine or any of the ingredients listed in the product leaflet.
Symptoms of an allergic reaction may include:
- shortness of breath, wheezing or difficulty breathing
- swelling of the face, lips, tongue or other parts of the body
- rash, itching or hives on the skin.
You must not be given Aminophylline Injection if you have any of the following conditions:
- heart disease caused by poor blood flow in the blood vessels of the heart (coronary artery disease)
- bronchiolitis (bronchopneumonia – a serious lung infection with fever, chills and coughing).
Aminophylline injection
Aminophylline injection is used together with other medicines to treat the acute symptoms of asthma, bronchitis, emphysema, and other lung diseases in a hospital setting.
Aminophylline is used to relieve breathing problems which may occur with:
- asthma
- emphysema,
- bronchitis or
- other diseases.
Aminophylline works by helping to open up your airways, allowing more air into your lungs.
Your doctor may have prescribed Aminophylline Injection for another reason.
Ask your doctor if you have any questions about why Aminophylline Injection has been prescribed for you.
Aminophylline Injection is available in the following dosage forms:
- Solution
Before Using Aminophylline IV Route
In deciding to use a medicine, the risks of taking the medicine must be weighed against the good it will do. This is a decision you and your doctor will make. For this medicine, the following should be considered:
Allergies
- Tell your doctor if you have ever had any unusual or allergic reaction to this medicine or any other medicines. Also tell your health care professional if you have any other types of allergies, such as to foods, dyes, preservatives, or animals. For non-prescription products, read the label or package ingredients carefully.
Pediatric
- Appropriate studies performed to date have not demonstrated pediatric-specific problems that would limit the usefulness of aminophylline injection in children. However, children younger than 1 year of age are more likely to have serious side effects, which may require caution and an adjustment in the dose for patients receiving aminophylline injection.
Geriatric
- Appropriate studies performed to date have not demonstrated geriatric-specific problems that would limit the usefulness of aminophylline injection in the elderly. However, elderly patients may be more sensitive to the effects of aminophylline injection than younger adults, which may require caution and an adjustment in the dose for patients receiving aminophylline injection.
Pregnancy
- Pregnancy Category C (all trimesters): Animal studies have shown an adverse effect and there are no adequate studies in pregnant women OR no animal studies have been conducted and there are no adequate studies in pregnant women.
Breastfeeding
- Studies in women suggest that this medication poses minimal risk to the infant when used during breastfeeding.
Drug Interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are receiving aminophylline, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using aminophylline with any of the following medicines is not recommended. Your doctor may decide not to treat you with aminophylline or change some of the other medicines you take.
- Riociguat
Using aminophylline with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Adenosine
- Amifampridine
- Bupropion
- Ceritinib
- Cimetidine
- Ciprofloxacin
- Deferasirox
- Desogestrel
- Dienogest
- Dihydroartemisinin
- Donepezil
- Drospirenone
- Enoxacin
- Erythromycin
- Estradiol Cypionate
- Estradiol Valerate
- Ethinyl Estradiol
- Ethynodiol Diacetate
- Etintidine
- Etonogestrel
- Fluconazole
- Fluvoxamine
- Fosphenytoin
- Halothane
- Idrocilamide
- Imipenem
- Levofloxacin
- Levonorgestrel
- Medroxyprogesterone Acetate
- Mestranol
- Mexiletine
- Norelgestromin
- Norethindrone
- Norgestimate
- Norgestrel
- Pefloxacin
- Peginterferon Alfa-2a
- Peginterferon Alfa-2b
- Phenytoin
- Pixantrone
- Regadenoson
- Rofecoxib
- Thiabendazole
- Troleandomycin
- Vemurafenib
- Zileuton
Using aminophylline with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Adinazolam
- Alprazolam
- Aminoglutethimide
- Amiodarone
- Azithromycin
- Brotizolam
- Cannabis
- Carbamazepine
- Chlordiazepoxide
- Clobazam
- Clonazepam
- Clorazepate
- Diazepam
- Disulfiram
- Estazolam
- Febuxostat
- Flunitrazepam
- Flurazepam
- Halazepam
- Interferon Alfa-2a
- Ipriflavone
- Isoproterenol
- Ketazolam
- Lorazepam
- Lormetazepam
- Medazepam
- Methotrexate
- Midazolam
- Nilutamide
- Nitrazepam
- Oxazepam
- Pancuronium
- Pentoxifylline
- Phenobarbital
- Piperine
- Prazepam
- Propafenone
- Quazepam
- Rifampin
- Rifapentine
- Ritonavir
- Secobarbital
- St John’s Wort
- Tacrine
- Telithromycin
- Temazepam
- Ticlopidine
- Triazolam
- Viloxazine
- Zafirlukast
Other Interactions
Certain medicines should not be used at or around the time of eating food or eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using aminophylline with any of the following is usually not recommended, but may be unavoidable in some cases. If used together, your doctor may change the dose or how often you use this medicine, or give you special instructions about the use of food, alcohol, or tobacco.
- Tobacco
Using aminophylline with any of the following may cause an increased risk of certain side effects but may be unavoidable in some cases. If used together, your doctor may change the dose or how often you use this medicine, or give you special instructions about the use of food, alcohol, or tobacco.
- Caffeine
Other Medical Problems
The presence of other medical problems may affect the use of aminophylline. Make sure you tell your doctor if you have any other medical problems, especially:
- Congestive heart failure or
- Cor pulmonale (heart condition) or
- Fever of 102 degrees F or higher for 24 hours or more or
- Hypothyroidism (underactive thyroid) or
- Infection, severe (e.g., sepsis) or
- Kidney disease in infants younger than 3 months of age or
- Liver disease (e.g., cirrhosis, hepatitis) or
- Pulmonary edema (lung condition) or
- Shock (serious condition with very little blood flow in the body)—Use with caution. The effects may be increased because of slower removal of aminophylline from the body.
- Heart rhythm problems (e.g., arrhythmia)
- Seizures, or history of seizures
- Stomach ulcer—Use with caution. Aminophylline may make these conditions worse.
Aminophylline dose
Your doctor will decide what dose of Aminophylline Injection you will receive and how long you will receive it for. This depends on your medical condition and other factors, such as your weight.
Sometimes only a single dose is required.
How Aminophylline Injection is given
Aminophylline Injection can be given in two ways:
- as a slow injection into a vein
- as an infusion (drip) into a vein.
Aminophylline Injection must only be given by a doctor or nurse.
Adult Dose for Asthma – Acute
Use(s): As an adjunct to inhaled beta-2 selective agonists and systemic corticosteroids for treatment of acute exacerbations of the symptoms and reversible airflow obstruction associated with asthma and other chronic lung diseases such as emphysema and chronic bronchitis
THESE RECOMMENDATIONS SHOULD SERVE AS THE UPPER LIMIT FOR DOSE ADJUSTMENTS. ADJUST DOSE BASED ON SERUM THEOPHYLLINE CONCENTRATIONS
Loading dose (to achieve a target serum concentration of 10 mcg/mL theophylline):
For patients with NO theophylline use in the previous 24 hours:
- 5.7 mg aminophylline/kg (ideal body weight) intravenously over 30 minutes
For patient who HAVE had theophylline in the past 24 hours, based on theophylline serum concentration measurements in mcg/mL:
- Loading dose = (Desired concentration – measured concentration) (volume of distribution)
- Mean volume of distribution can be assumed to be 0.5 L/kg (actual range 0.3 to 0.7).
- Desired serum concentration should be conservative (e.g. 10 mcg/mL) to allow for variability of volume of distribution.
Once a serum concentration of 10 to 15 mcg/mL theophylline is achieved by loading dose:
- 1 mg aminophylline/kg ideal body weight/hour as a constant infusion
- Obtain a second serum theophylline concentration about one half-life after starting the infusion; the manufacturer product information should be consulted.
Comments:
- Steady state serum theophylline concentrations are a function of the infusion rate and rate of theophylline clearance in the individual patient.
- The dose required to achieve a serum theophylline concentration in the 10 to 20 mcg/mL range varies fourfold because of different rates of theophylline clearance.
- There is no single dose that is safe and effective for all patients.
- Administering the median dose may result in subtherapeutic or toxic blood levels.
- The dose must be individualized based on serum theophylline concentrations to achieve maximum benefit with minimal risk.
- Do not give a loading dose until a serum theophylline concentration has been obtained if the patient received any theophylline in the previous 24 hours.
- For acute bronchodilation, a therapeutic serum concentration is best achieved with an intravenous loading dose.
Geriatric Dose for Asthma – Acute
Use(s): As an adjunct to inhaled beta-2 selective agonists and systemic corticosteroids for treatment of acute exacerbations of the symptoms and reversible airflow obstruction associated with asthma and other chronic lung diseases such as emphysema and chronic bronchitis
THESE RECOMMENDATIONS SHOULD SERVE AS THE UPPER LIMIT FOR DOSE ADJUSTMENTS. ADJUST DOSE BASED ON SERUM THEOPHYLLINE CONCENTRATIONS
Loading dose (to achieve a target serum concentration of 10 mcg/mL theophylline):
For patients with NO theophylline use in the previous 24 hours:
- 5.7 mg aminophylline/kg (ideal body weight) intravenously over 30 minutes
For patient who HAVE had theophylline in the past 24 hours, based on theophylline serum concentration measurements in mcg/mL:
- Loading dose = (Desired concentration – measured concentration) (volume of distribution)
- Mean volume of distribution can be assumed to be 0.5 L/kg (actual range 0.3 to 0.7).
- Desired serum concentration should be conservative (e.g. 10 mcg/mL) to allow for variability of volume of distribution.
Once a serum concentration of 10 to 15 mcg/mL theophylline is achieved by loading dose:
- 1 mg aminophylline/kg ideal body weight/hour as a constant infusion
- Obtain a second serum theophylline concentration about one half-life after starting the infusion; the manufacturer product information should be consulted.
Comments:
- Careful attention to dose reduction and frequent monitoring of serum theophylline concentrations are required.
- Steady state serum theophylline concentrations are a function of the infusion rate and rate of theophylline clearance in the individual patient.
- The dose required to achieve a serum theophylline concentration in the 10 to 20 mcg/mL range varies fourfold because of different rates of theophylline clearance.
- There is no single dose that is safe and effective for all patients.
- Administering the median dose may result in subtherapeutic or toxic blood levels.
- The dose must be individualized based on serum theophylline concentrations to achieve maximum benefit with minimal risk.
- Do not give a loading dose until a serum theophylline concentration has been obtained if the patient received any theophylline in the previous 24 hours.
- For acute bronchodilation, a therapeutic serum concentration is best achieved with an intravenous loading dose.
Pediatric Dose for Asthma – Acute
Use(s): As an adjunct to inhaled beta-2 selective agonists and systemic corticosteroids for treatment of acute exacerbations of the symptoms and reversible airflow obstruction associated with asthma and other chronic lung diseases such as emphysema and chronic bronchitis
THESE RECOMMENDATIONS SHOULD SERVE AS THE UPPER LIMIT FOR DOSE ADJUSTMENTS. ADJUST DOSE BASED ON SERUM THEOPHYLLINE CONCENTRATIONS
Loading dose (to achieve a target serum concentration of 10 mcg/mL theophylline):
For patients with NO theophylline use in the previous 24 hours:
- 5.7 mg aminophylline/kg (ideal body weight) intravenously over 30 minutes
For patient who HAVE had theophylline in the past 24 hours, based on theophylline serum concentration measurements in mcg/mL:
- Loading dose = (Desired concentration – measured concentration) (volume of distribution)
- Mean volume of distribution can be assumed to be 0.5 L/kg (actual range 0.3 to 0.7).
- Desired serum concentration should be conservative (e.g. 10 mcg/mL) to allow for variability of volume of distribution.
Once a serum concentration of 10 to 15 mcg/mL theophylline is achieved by loading dose:
- 1 mg aminophylline/kg ideal body weight/hour as a constant infusion
- Obtain a second serum theophylline concentration about one half-life after starting the infusion; the manufacturer product information should be consulted.
Comments:
- Select the infusion rate with caution, as theophylline clearance is highly variable across the age range of neonates to adolescents.
- Patients under 1 year old have immature theophylline metabolic pathways; particular attention to dosage and frequent monitoring of serum theophylline concentrations are required.
- Steady state serum theophylline concentrations are a function of the infusion rate and rate of theophylline clearance in the individual patient.
- The dose required to achieve a serum theophylline concentration in the 10 to 20 mcg/mL range varies fourfold because of different rates of theophylline clearance.
- There is no single dose that is safe and effective for all patients.
- Administering the median dose may result in subtherapeutic or toxic blood levels.
- The dose must be individualized based on serum theophylline concentrations to achieve maximum benefit with minimal risk.
- Do not give a loading dose until a serum theophylline concentration has been obtained if the patient received any theophylline in the previous 24 hours.
- For acute bronchodilation, a therapeutic serum concentration is best achieved with an intravenous loading dose.
Renal Dose Adjustments
- No adjustment recommended in adults and children over 3 months with renal insufficiency
- Careful attention to dose reduction and frequent monitoring of serum theophylline concentrations is required in neonates, as a large fraction dose is excreted unchanged in the urine in neonates.
Liver Dose Adjustments
- Dose adjustment(s) may be required; however, no specific guidelines have been suggested. Caution is recommended.
- Theophylline clearance is decreased by 50% in hepatic insufficiency.
- Frequent monitoring of serum theophylline concentrations is required.
Dialysis
Data not available
Monitoring
- If patients develop nausea or vomiting, particularly repetitive vomiting, or other symptoms consistent with theophylline toxicity, stop the infusion and measure serum theophylline immediately, even if another cause of toxicity is suspected.
- Since theophylline clearance may be dose dependent, dose increases because of subtherapeutic serum concentrations should be conservative; limiting increases to about 25% of the previous infusion rate reduces the risk of excessive serum theophylline concentrations.
- Carefully consider interacting drugs and physiologic conditions that may affect theophylline clearance prior to initiating therapy and prior to dose increases.
- Serum theophylline concentration measurements are readily available and should be used to determine whether the dosage is appropriate.
- Measure serum theophylline before dose increases, for signs and symptoms of theophylline toxicity, for new illness or worsening of existing illness, or changes in the treatment regimen that may alter theophylline clearance.
- The manufacturer product information should be consulted for specific monitoring guidelines.
What should I do if I forget a dose?
Take the missed dose as soon as you remember it. However, if it is almost time for the next dose, skip the missed dose and continue your regular dosing schedule. Do not take a double dose to make up for a missed one. If you become severely short of breath, call your doctor.
Aminophylline side effects
Along with its needed effects, aminophylline may cause some unwanted side effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Tell your doctor if any of these symptoms are severe or do not go away:
- upset stomach
- stomach pain
- diarrhea
- headache
- restlessness
- insomnia
- irritability
If you experience any of the following symptoms, call your doctor immediately:
- vomiting
- increased or rapid heart rate
- irregular heartbeat
- seizures
- skin rash
Aminophylline overdose
Aminophylline or theophylline overdose occurs when someone takes more than the normal or recommended amount of these medicines. This can be by accident or on purpose.
In case of overdose, call the poison control helpline at 1-800-222-1222. Information is also available online at https://www.poisonhelp.org/help. If the victim has collapsed, had a seizure, has trouble breathing, or can’t be awakened, immediately call your emergency services number.
Aminophylline overdose symptoms
The most serious life-threatening symptoms of theophylline overdose are seizures and disturbances in heart rhythm.
Aminophylline overdose symptoms in adults may include:
STOMACH AND INTESTINES
- Increased appetite
- Increased thirst
- Nausea
- Vomiting (possibly with blood)
HEART AND BLOOD
- High or low blood pressure
- Irregular heartbeat
- Rapid heart rate
- Pounding heartbeat (palpitations)
LUNGS
- Breathing difficulty
MUSCLES AND JOINTS
- Muscle twitching and cramping
NERVOUS SYSTEM
- Confusion, hallucination
- Convulsions
- Dizziness
- Fever
- Headache
- Irritability, restlessness
- Confused thinking, poor judgment and agitation (psychosis)
- Sweating
- Trouble sleeping
Aminophylline overdose symptoms in babies may include:
STOMACH AND INTESTINES
- Nausea
- Vomiting
HEART AND BLOOD
- Irregular heartbeat
- Low blood pressure
- Rapid heartbeat
- Shock
LUNGS
- Rapid, deep breathing
MUSCLES AND JOINTS
- Muscle cramps
- Twitching
NERVOUS SYSTEM
- Convulsions
- Irritability
- Tremors
What to expect at the Emergency Room
Take the container with you to the hospital, if possible.
The doctor will measure and monitor the person’s vital signs, including temperature, pulse, breathing rate, and blood pressure.
Tests that may be done include:
- Blood and urine tests
- Chest x-ray
- ECG (electrocardiogram, or heart tracing)
Treatment may include:
- Activated charcoal
- Intravenous fluids (given through a vein)
- Laxative
- Medicine to treat symptoms
- Shock to the heart, for serious heart rhythm disturbances
- Breathing support, including tube through the mouth into the lungs and connected to a breathing machine
- Dialysis (kidney machine), in severe cases
Aminophylline overdose prognosis
Convulsions and irregular heartbeats may be difficult to control. Some symptoms may occur up to 12 hours after the overdose.
Death may occur with large aminophylline overdoses, especially in very young or old people.