Opsoclonus
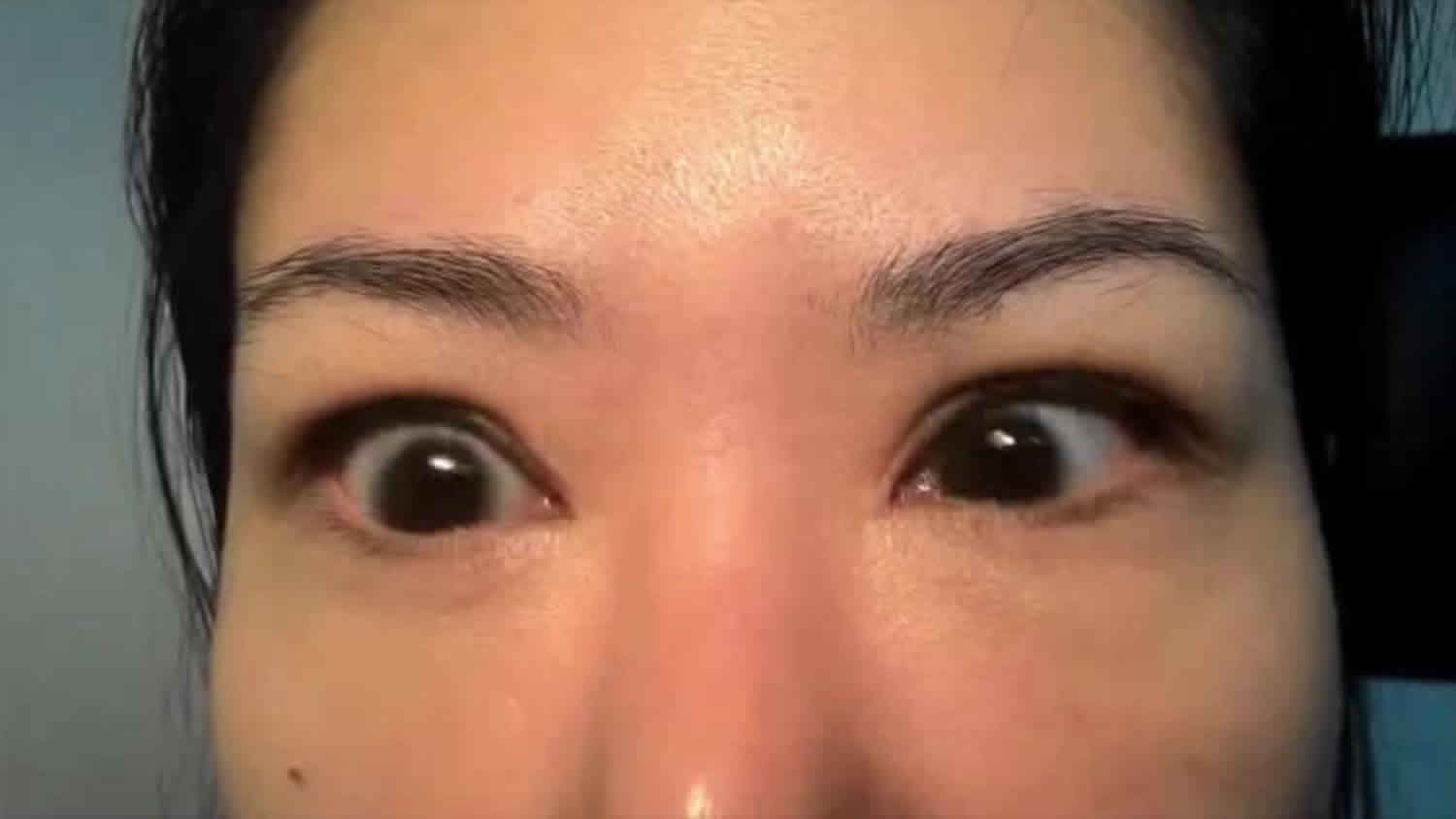
Opsoclonus is an ocular dyskinesia. Opsoclonus is defined as chaotic, continuous multidirectional rapid eye movements (saccadic oscillations) without an intersaccadic interval. Eye movements in opsoclonus are sudden, involuntary, chaotic, arrhythmic and multidirectional (upwards, downwards and torsional) conjugate saccadic eye movements. The resulting symptoms of oscillopsia and visual blurring are attributed to their large amplitude and high frequency. Opsoclonus must be differentiated from nystagmus (rapid jerks followed by a slow corrective saccade) and ocular flutter (horizontal back-to-back saccades). Frequently, generalized myoclonus and ataxia coexist; hence, the term opsoclonus-myoclonus-ataxia.
Paraneoplastic (neuroblastoma in children; small-cell lung cancer in adults), parainfectious, metabolic and toxic aetiologies can be identified; however, it can be idiopathic. The cell-mediated and humeral immunities contribute to the pathogenesis of the paraneoplastic and idiopathic varieties. Although it has been associated with several autoantibodies, several patients are seronegative. The treatment is directed towards the underlying cause; tumour surgery, chemotherapy and immune suppressive therapy, including intravenous immunoglobulin. Clonazepam may be a useful symptomatic treatment in those who did not respond to immune suppressants 1.
Opsoclonus myoclonus ataxia syndrome
Opsoclonus-myoclonus syndrome also known as opsoclonus-myoclonus ataxia, dancing eye syndrome or Kinsbourne syndrome, is a inflammatory neurological disorder which develops over days or weeks in early childhood, often with paraneoplastic cause 2. Opsoclonus-myoclonus syndrome is characterized by involuntary, multidirectional eye movements (opsoclonus) with myoclonic jerks of the limbs and trunk with or without ataxia, behavioral, sleep, and language disturbances 3. The onset is usually abrupt, often severe, and it can become chronic.
Opsoclonus-myoclonus syndrome key clinical features are unsteadiness (ataxia), jerky movements of the trunk and limbs (myoclonus), rapid involuntary eye movements in all directions (opsoclonus) and usually marked irritability with sleep disturbance.
The occurrence of marked irritability with behavioral change and sleep disturbance in an infant with new onset ataxia is one of the strongest clues that this may be opsoclonus-myoclonus syndrome or dancing eye syndrome. Most children develop opsoclonus-myoclonus syndrome in the second or third year of life but rarely it may occur earlier or later. In children the condition may occur with no clear trigger or it may follow a viral illness or it may be associated with a neuroblastoma 4.
It appears that in opsoclonus myoclonus syndrome an area of the brain called the cerebellum is attacked 4. The cerebellum is responsible for coordinating eye movements, muscle coordination and speech. Around half of children diagnosed with opsoclonus myoclonus syndrome are found to have a neuroblastoma tumor. It occurs in about 3% of all children with neuroblastomas 2. This is usually, but not always, a benign form of neuroblastoma tumor. Most children identified with a neuroblastoma will need to undergo staging and surgical resection, followed by monitoring by the neuro-oncology team. Treatment of the neuroblastoma, while important in its own right, does not appear to alter the outcome of opsoclonus-myoclonus syndrome.
In children who do not have neuroblastoma, the condition may follow an infectious illness or no clear trigger may be found.
Opsoclonus-myoclonus syndrome is an exceedingly rare disorder with about 1 per 5 million individuals worldwide per year 5. Opsoclonus-myoclonus syndrome usually affects infants and young children, although it is also known to affect adults. The peak age in children is about 18 months, with very few diagnosed before 1 year, and a long tail out to about 5 – 6 years. Occurrence of opsoclonus in infants under 6 months old is quite uncommon, and opsoclonus in that age group, when isolated, is usually from another cause. Opsoclonus-myoclonus syndrome occurs in only slightly more girls than boys.
The aims of treatment are firstly to treat the neuroblastoma tumor if present and secondly to attacks to the cerebellum and prevent any lasting damage.
Neuroblastoma tumors in children with opsoclonus myoclonus syndrome are usually very small so are best removed using surgery. Occasionally chemotherapy or radiotherapy is needed before and afterwards, especially if the entire tumor cannot be removed during the operation.
The immune system is modulated by using a combination of medicines. Steroids are given either by mouth or in ‘pulses’ intravenously (into a vein), sometimes alongside another medicine such as rituximab. Rituximab removes some of the white blood cells in the body called B cells. Sometimes another medicine called cyclophosphamide is used instead of rituximab but this affects all types of blood cell. Intravenous immunoglobulin (IVIg), which damps down the immune system, may also be used. Treatment continues until the symptoms of opsoclonus myoclonus syndrome improve.
Opsoclonus myoclonus syndrome causes
The causes of opsoclonus-myoclonus syndrome may be divided into three main categories:
- Paraneoplastic,
- Para-infectious,
- Idiopathic.
The type of primary malignancy identified in paraneoplastic cases varies based on age. The most common cause of opsoclonus-myoclonus syndrome in young children is paraneoplastic. In children, roughly 50% of opsoclonus-myoclonus syndrome may be attributed to neuroblastoma or tumors of neural crest origin 6. A small, often hidden tumor presumably provokes the immune system into attacking the nervous system, which may also control the tumor or even cause it to regress. Tumors are NOT in the brain, but are in other areas of the body, usually in chest or abdomen. In 50-80 percent of affected young children, a tumor of embryonic nerve cells (neuroblastoma or ganglioneuroblastoma) is responsible for the symptoms associated with opsoclonus-myoclonus syndrome. In other affected individuals, opsoclonus-myoclonus syndrome has been designated ‘idiopathic’ or attributed to various mostly viral infections. However, the high rate of spontaneous tumor regression means that the tumor may be gone before it is looked for. In older children or teens, viral infections are the most frequent apparent cause of opsoclonus-myoclonus syndrome.
In adults, paraneoplastic cause is more common, most due to lung or breast cancers. In contrast to paraneoplastic opsoclonus-myoclonus syndrome in infants and young children, whose tumors are biologically inactive and often benign, the tumors in adults are commonly malignant, often disseminated.
A recent review of 116 adult onset opsoclonus-myoclonus syndrome cases in the literature reported 51% of cases were paraneoplastic in etiology 7. Female adults under 40 years of age are most likely to develop paraneoplastic opsoclonus-myoclonus syndrome secondary to ovarian teratoma, whereas adults over 40 years most often develop opsoclonus-myoclonus syndrome in the setting of small cell lung cancer, breast cancer, or ovarian malignancies 8. In the second category, para-infectious opsoclonus-myoclonus syndrome has been described in association with streptococcal infection, Lyme disease, varicella zoster, HIV/AIDS, and others 9. Most other cases of opsoclonus-myoclonus syndrome are idiopathic, although rare cases also have been reported in association with toxic and metabolic abnormalities 7. Eight cases of opsoclonus-myoclonus syndrome have been reported due to West Nile virus 10.
Opsoclonus myoclonus syndrome signs and symptoms
The symptoms of opsoclonus myoclonus syndrome are very variable and may not all be present at the same time. The clinical features of opsoclonus-myoclonus syndrome include repeated, random and rapid eye movements in both horizontal, vertical and diagonal directions (opsoclonus); unsteady gait or loss of ability to stand and walk (ataxia); brief, repeated, shock-like spasms of several muscles within the arms, legs (myoclonus), or tremor interfering with hand use. Unsteadiness (ataxia) and muscle jerks affecting all or some areas of the body are usually the first symptom to appear. Behavioral problems and sleep disturbances, including extreme irritability, inconsolable crying, reduced and fragmented sleep (insomnia) and rage attacks are common. These symptoms tend to appear quite quickly, often leading to skills such as sitting and walking being lost in a matter of days. Difficulty articulating speech (dysarthria), sometimes with complete loss of speech and language may occur, for instance losing previously-fluent speech or not speaking at all. Additional symptoms such as decreased muscle tone (hypotonia) and vomiting are common.
Typically opsoclonus myoclonus appears around the age of one to two years but can occur at any time in childhood.
Signs and symptoms of opsoclonus-myoclonus syndrome may include 11:
- Unsteady, trembling gait (manner of walking)
- Sudden, brief, shock-like muscle spasms (myoclonus). While it occurs most when trying to move and worsens with agitation or stimulation, it can also be present at rest. Myoclonus can make a person appear nervous or shaky, or have jerking movements. The face, eyelids, limbs, fingers, head and trunk may be involved. When the illness is at its worst, sitting or standing is difficult or impossible.
- Irregular, rapid eye movements (opsoclonus)
Other symptoms may include difficulty speaking or inability to speak, difficulty eating or sleeping, excessive drooling, lack of coordination, rage attacks, head tilt, a decrease in muscle tone, and/or general feeling of discomfort or illness 12.
Children may appear to be nervous, irritable, or lethargic while adults may have mental clouding (encephalopathy) 11.
Opsoclonus myoclonus syndrome diagnosis
Opsoclonus-myoclonus syndrome diagnosis is clinical; there is no diagnostic test yet, as the antigen remains unidentified. The presence of the ‘dancing eyes’, the shock-like muscle spasms, and the impairment of gait, especially if accompanied by irritability, are highly reliable indicators of this syndrome.
To be diagnosed with opsoclonus myoclonus syndrome, a child must have three of the following four conditions
- rapid eye movement (opsoclonus or ocular flutter)
- ataxia (unsteadiness) or jerky muscle spasms (myoclonus)
- behavioral or sleep problems and
- neuroblastoma.
Opsoclonus myoclonus can be mistaken for other similar appearing conditions, so diagnosis at a specialist center is advised.
To detect a tumor in children, either a CT scan with oral and IV contrast or MRI with gadolinium of the neck, chest, abdomen, and pelvis need to be done. PET scanning is often done in adults with opsoclonus-myoclonus syndrome looking for other occult tumors. In addition, a spinal tap to detect neuroinflammation is necessary. Besides routine tests for infection, recommended CSF studies include so-called “MS panel”, to include oligoclonal bands (with paired serum sample), looking for antibodies secreted by B cells in the CSF. Also, lymphocyte subset analysis (flow cytometry) using immunophenotyping reveals an increased frequency of CSF CD 19+ B cells, which is an invaluable biomarker of opsoclonus-myoclonus syndrome disease activity. Autoantibodies in some children with opsoclonus-myoclonus syndrome have been at detected in research laboratories, but commercial autoantibody testing is not cost-effective and best reserved for atypical cases. Overall, neuronal antibodies have not been found to be syndrome-specific and likely reflect a wider autoimmune process 13.
Adult patients younger than 40-years-old are more likely to have idiopathic or infectious opsoclonus-myoclonus syndrome. Aggressive investigations for occult neoplasm or paraneoplastic antibodies may not be necessary, with the exception of ovarian teratoma 8. HIV infection should always be excluded as HIV-related opsoclonus-myoclonus syndrome has no characteristic clinical features. Further work-up for para-infectious causes may include CSF and/or serum serologies for streptococcus, treponema pallidum, VZV, EBV, CMV, HSV 1 and 2, JC virus, and Lyme antibodies. In older patients, lung cancer, especially small cell carcinoma, is the most common paraneoplastic cause, followed by breast and gynecologic cancers 8.
Opsoclonus myoclonus syndrome treatment
The goal of treatment of opsoclonus-myoclonus syndrome is early and aggressive immunotherapy with the goal of gaining a durable complete neurological remission. If a tumor is present, surgical resection is standard. The tumors in young children are usually low stage neuroblastomas or ganglioneuroblastomas (stage 1 or 2), and tumor chemotherapy or radiation therapy are not generally indicated. Tumor resection does not usually provide sufficient clinical benefit for opsoclonus-myoclonus syndrome, however.
Opsoclonus-myoclonus syndrome treatment, which is usually continued over at least 1-2 years, should involve combined immunotherapies as soon as possible after diagnosis. A three-agent protocol involving initial use of high-dose ACTH (adrenocorticotrophic hormone or corticotropin), human intravenous immunoglobulins (IVIG) and rituximab has the best-documented outcomes for moderately severe and severe cases. Rituximab is a monoclonal antibody against B cells (anti-CD20). Almost all patients (80-90%) show improvement with this treatment, but maintaining sustained improvement may require additional treatment and very gradual weaning. Over time, treatment with ACTH may have substantial cortisol-related adverse effects that must be monitored carefully, particularly weight gain, hypertension, and reductions in bone density. Monthly pulse dose dexamethasone instead of ACTH is an option in mild and more moderate cases. The use of prednisone-type oral steroids is not recommended, because they are the least effective of the steroids for pediatric opsoclonus-myoclonus syndrome. For opsoclonus-myoclonus syndrome relapse, low-dose IV cyclophosphamide (3-6 cycles) or repeated courses of rituximab (1-2 cycles) are given. Oral weekly methotrexate may be a useful steroid sparer in chronic relapse.
Opsoclonus myoclonus syndrome prognosis
The outlook for children and young people with opsoclonus myoclonus syndrome is variable depending on the severity of the symptoms when the condition is diagnosed. Almost all children with neuroblastoma and opsoclonus-myoclonus syndrome survive their tumor, which usually does not behave aggressively, though some tumors may be large and pose difficulties for resection. Occasionally children recover fully without treatment. Others respond to treatment partially or incompletely. In contrast, the tumors that are associated with opsoclonus-myoclonus syndrome in adults are often aggressive and are sometimes fatal. The majority of children however, will have a chronic relapsing disease course and will require long-term immunosuppressive treatment. The opsoclonus-myoclonus syndrome relapse rate in children treated with only conventional agents is 50-75%. Increased immunosuppression has improved neurodevelopmental outcomes in opsoclonus-myoclonus syndrome. With more aggressive initial therapies in children, the relapse rate appears to be much lower. Relapses may be triggered either as the treatment is withdrawn or following a viral infection. It is important for those affected to be identified early as they might benefit from new advances in immunomodulating therapy in specialist centers.
Opsoclonus-myoclonus syndrome onset in the first two years of life is particularly damaging to expressive speech and language development, and may result in a higher incidence of residual cognitive impairment with ongoing problems with learning, coordination, behavior and sleep. These difficulties require targeted intervention from the wider multidisciplinary team including speech and language therapy, occupational therapy and physiotherapy.
The best responders appear to be those who received early combination therapy and were only of mild to moderate severity. Failure to achieve complete neurological remission and multiple relapses may result in chronic-progressive opsoclonus-myoclonus syndrome, with permanent deficits, such as attention deficient disorder (ADD) attention-deficit/hyperactivity disorder (ADHD), obsessive-compulsive disorder (OCD), and irreversible cognitive impairment (low IQ). Children in the chronic sick role can become oppositional, depressed, and aggressive, and attention to these issues often helps to improve quality of life. Parents with a severely ill infant or child may develop “fragile child syndrome” and have difficulty ever seeing their child as a normal, thriving individual, with “ordinary” behavioral issues of childhood. These parents may benefit from counselling to gradually adjust their management of their child’s ongoing behavioral and developmental issues.
References- Pike M. Opsoclonus-myoclonus syndrome. Handb Clin Neurol 2013;112:1209–11. doi:10.1016/B978-0-444-52910-7.00042-8
- Opsoclonus-myoclonus syndrome. https://rarediseases.org/rare-diseases/opsoclonus-myoclonus-syndrome
- Ophthalmology AAo. Saccadic Intrusions. Basic and Clinical Science Course: Section 5, 2017-2018. Neuro-ophthalmology. . San Francisco: American Academy of Ophthalmology; 2017; p. 248-249.
- Opsoclonus Myoclonus Syndrome/Dancing Eye syndrome. https://www.gosh.nhs.uk/conditions-and-treatments/conditions-we-treat/opsoclonus-myoclonus-syndrome-dancing-eye-syndrome-omsdes
- Pang KK, de Sousa C, Lang B, Pike MG. A prospective study of the presentation and management of dancing eye syndrome/opsoclonus-myoclonus syndrome in the United Kingdom. Eur J Paediatr Neurol 2010;14(2):156-161.
- Tate ED, Allison TJ, Pranzatelli MR, Verhulst SJ. Neuroepidemiologic trends in 105 US cases of pediatric opsoclonus-myoclonus syndrome. J Pediatr Oncol Nurs 2005;22(1):8-19
- Klaas JP, Ahlskog JE, Pittock SJ, Matsumoto JY, Aksamit AJ, Bartleson JD, Kumar R, McEvoy KF, McKeon A. Adult-onset opsoclonus-myoclonus syndrome. Arch Neurol 2012;69(12):1598-1607.
- Armangué T, Sabater L, Torres-Vega E, Martínez-Hernández E, Ariño H, Petit-Pedrol M, Planagumà J, Bataller L, Dalmau J, Graus F. Clinical and Immunological Features of Opsoclonus-Myoclonus Syndrome in the Era of Neuronal Cell Surface Antibodies. JAMA Neurol 2016;73(4):417-424.
- Wong A. An update on opsoclonus. Curr Opin Neurol 2007;20(1):25-31.
- Zaltzman R, Klein C, Gordon CR. Opsoclonus myoclonus ataxia associated with West Nile virus infection: A dramatic presentation with benign prognosis? J Neurol Sci 2017;376:38-41.
- Pranzatelli MR. What is the Opsoclonus-Myoclonus Syndrome?. Opsoclonus-Myoclonus U.S.A. And International web site. http://www.omsusa.org/pranzatelli-Brochure1.htm
- Opsoclonus Myoclonus Information Page. https://www.ninds.nih.gov/Disorders/All-Disorders/Opsoclonus-Myoclonus-Information-Page
- Balint B, Vincent A, Meinck HM, Irani SR, Bhatia KP. Movement disorders with neuronal antibodies: syndromic approach, genetic parallels and pathophysiology. Brain 2018;141(1):13-36.