Pancreatic elastase
Elastase is an enzyme produced by special (exocrine) tissue in the pancreas. The pancreas is an organ located in the abdomen that consists of two kinds of tissues: exocrine and endocrine. The exocrine pancreas is responsible for producing elastase along with other enzymes that are transported to the small intestine to break down fats, proteins, and carbohydrates as part of food digestion.
In the digestive tract, pancreatic elastase is not broken down by other enzymes and is eventually eliminated from the body in the stool. Pancreatic elastase can be detected and measured in the stool when a person’s pancreas is functioning normally. The level in the stool is decreased when the exocrine tissues of the pancreas are not producing sufficient elastase and other digestive enzymes. This condition is called exocrine pancreatic insufficiency.
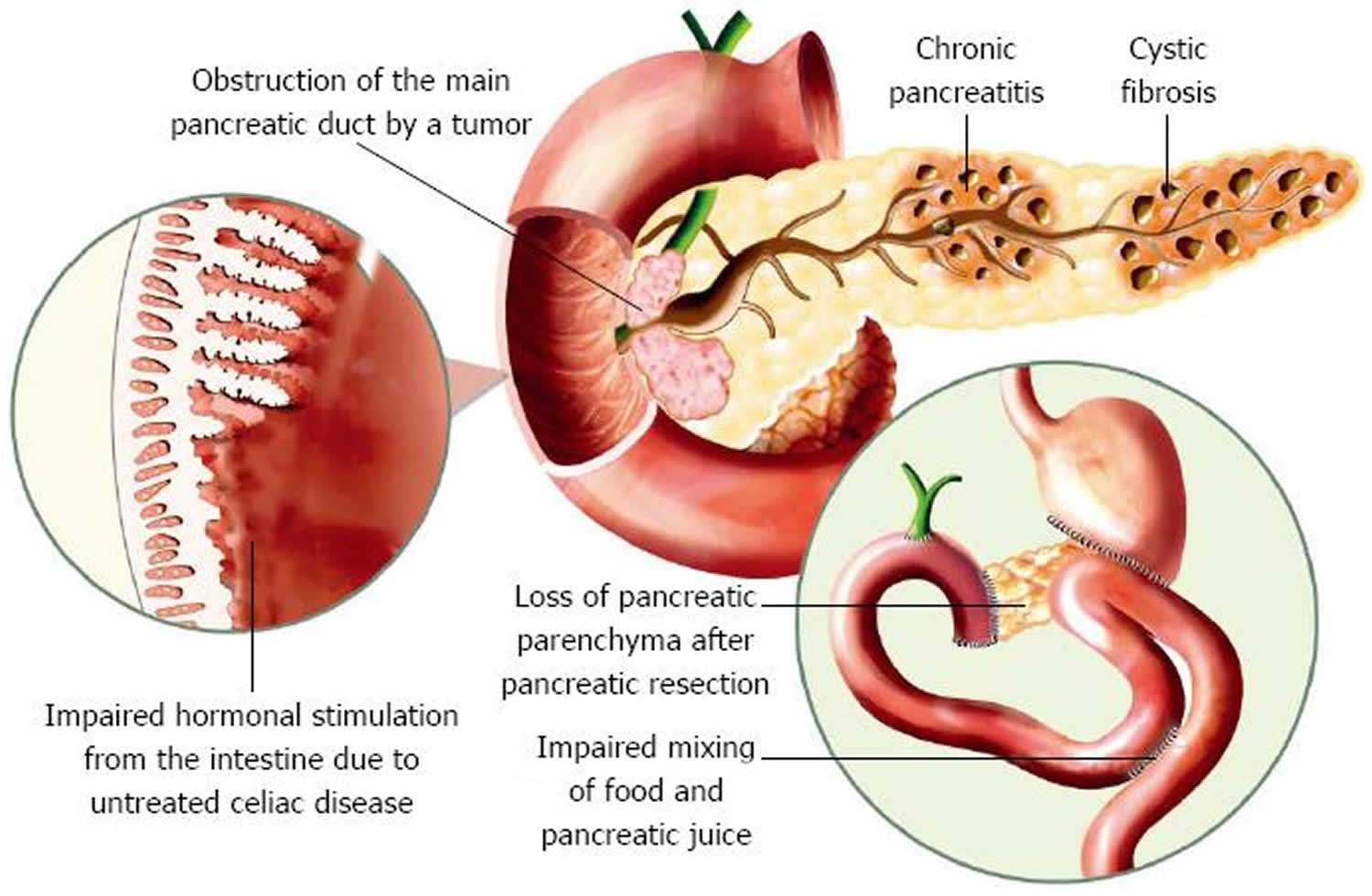
Exocrine pancreatic insufficiency occurs when the amount of enzymes released and transported to the small intestine is inadequate for proper food digestion and absorption of nutrients. Any condition that blocks the pancreatic ducts or damages or destroy the cells that produce elastase can cause pancreatic insufficiency. Exocrine pancreatic insufficiency is often seen in conditions such as chronic pancreatitis and sometimes pancreatic cancer. In children, it is most frequently associated with cystic fibrosis (CF) or Shwachman-Diamond syndrome.
Exocrine pancreatic insufficiency is a condition characterized by deficiency of the exocrine pancreatic enzymes, resulting in the inability to digest food properly, or maldigestion. Exocrine pancreatic insufficiency is characterized by poor absorption of fats, proteins, and, to a lesser extent carbohydrates. Clinicians can make the diagnosis of exocrine pancreatic insufficiency by one of 3 criteria: fecal elastase test (fecal elastase-1), fecal fat test, or a direct pancreatic function test 1.
Fecal elastase refers to the testing of the concentration of the pancreatic elastase-1 enzyme found in fecal matter with an enzyme-linked immunosorbent assay (ELISA). Results of this test can give a good indication of exocrine pancreatic status and is less invasive and expensive that the current “gold standard”, secretin-cholecystokinin test 2 . Levels of fecal elastase lower than 200 μg/g of stool indicate an exocrine insufficiency. Correlations between low levels and chronic pancreatitis and cancer have been reported.
What causes pancreatic insufficiency?
Pancreatic insufficiency can be caused by regular bouts of acute pancreatitis or by chronic pancreatitis. It is less frequently but sometimes associated with pancreatic cancer. Other causes of insufficiency may include celiac disease, Crohn disease, autoimmune pancreatitis (immunoglobulin G4-related disease), Zollinger-Ellison syndrome, and some surgical procedures that can lead to a decrease in digestive system or pancreatic function.
In children, pancreatic insufficiency is most frequently associated with cystic fibrosis (CF) or Shwachman-Diamond syndrome. Shwachman-Diamond syndrome is the second most common cause of inherited pancreatic insufficiency, after cystic fibrosis. All those with Shwachman-Diamond syndrome have some degree of pancreatic insufficiency beginning in infancy.
Additionally, people who are carriers of one mutated copy of the CFTR gene, the gene typically responsible for cystic fibrosis, may have pancreatic insufficiency and experience the associated signs and symptoms.
Pancreatic insufficiency diagnosis
Laboratory tests that may be used to detect pancreatic insufficiency include:
- Stool elastase or fecal elastase-1 test: Fecal elastase-1 test measures the level of pancreatic elastase (an enzyme made by the pancreas) in a sample of your stool. The amount of this enzyme is reduced in pancreatic insufficiency. This test is more effective at detecting moderate to severe exocrine pancreatic insufficiency than milder cases.
- Chymotrypsin: Chymotrypsin test measures chymotrypsin (a pancreatic enzyme that breaks down proteins) in your stool. With exocrine pancreatic insufficiency, chymotrypsin is absent in the stool.
- Immunoreactive trypsinogen: Immunoreactive trypsinogen is a blood test that measures trypsinogen, an inactive precursor produced by the pancreas that is converted to the enzyme trypsin. Trypsin is the pancreatic enzyme that digests proteins. Immunoreactive trypsinogen may be elevated with pancreatitis, which may cause exocrine pancreatic insufficiency.
- Fecal fat (fat in the stool): Fecal fat test detects excess fat in your stool, often the first sign of exocrine pancreatic insufficiency. Because the stool elastase test (see above) is easier to perform, it has largely replaced this test.
- 13C-mixed triglyceride breath test: 13C-mixed triglyceride breath test is a newer method of diagnosing moderate pancreatic insufficiency, but it is not widely used and not commonly available. The test may also be used to evaluate the effectiveness of enzyme therapy on fat digestion in people with exocrine pancreatic insufficiency.
Non-laboratory tests used in diagnosing pancreatic insufficiency may include:
- Computed tomography (CT) scan: can be used to detect inflammation or scarring of the pancreas
- Endoscopic retrograde cholangiopancreatography (ERCP): an endoscope (a hollow tube) is guided through your mouth, down your throat and stomach to your small intestine. A smaller tube (catheter) is inserted through the endoscope to inject contrast dye into the pancreatic and bile ducts. Abdominal x-rays are taken to examine the pancreas, gallbladder, and the ducts that carry digestive enzymes from those organs to the small intestine. Endoscopic retrograde cholangiopancreatography (ERCP) can be used look for blockages or damage to the ducts.
- Magnetic resonance cholangiopancreatography (MRCP): a specific type of magnetic resonance imaging (MRI) that uses powerful magnets and radio waves to create images of the pancreas, pancreatic duct, and bile ducts. It is often used before or instead of endoscopic retrograde cholangiopancreatography (ERCP) to look for abnormalities in the pancreas because it is faster and non-invasive. It is also useful in distinguishing pancreatitis from pancreatic cancer.
- Ultrasound: may be used to create and send images of your pancreas to a video monitor. An endoscopic ultra sound is an exam that involves a thin, flexible tube that is used to view inside the digestive tract and is more accurate than an abdominal ultrasound.
Pancreatic insufficiency treatment
Management of pancreatic insufficiency may include:
- Taking enzyme supplements (pancreatic enzyme replacement therapy or PERT) to replace the enzymes your pancreas isn’t making any more
- Eating a healthy, balanced diet; you might need guidance from a nutritionist to create a diet that meets your needs.
- Taking vitamin supplements (especially vitamins A, D, E, and K) if needed
- Making lifestyle changes, such not drinking alcohol and not smoking
Treatment of exocrine pancreatic insufficiency also involves managing or resolving the underlying cause when possible.
In Shwachman-Diamond syndrome, unlike in cystic fibrosis, production of pancreatic lipase (an enzyme that digests fats) often increases with age. The reasons for this are not yet known, but about 50% of children with Shwachman-Diamond syndrome will experience improvements in pancreatic function and fat absorption as they get older and will no longer require enzyme replacement therapy.
Pancreatic elastase stool test
The pancreatic elastase test is used along with other tests, such as fecal fat and/or fecal chymotrypsin, to evaluate both children and adults for pancreatic insufficiency.
Pancreatic insufficiency is the inability of the pancreas to produce and/or transport enough digestive enzymes to break down food in the intestine and aid in the absorption of nutrients. It typically occurs as a result of ongoing and worsening pancreatic damage.
The pancreatic elastase test is most effective at detecting severe pancreatic insufficiency and not as effective for mild or moderate pancreatic insufficiency forms.
A stool that is watery, such as with diarrhea, is not a good sample as the water in the stool will dilute the pancreatic elastase 1 and decrease the amount measured.
When is pancreatic elastase 1 test ordered?
A pancreatic elastase 1 test may be ordered when a person has signs and symptoms of pancreatic insufficiency, such as:
- Abdominal pain and cramps (the pain is sometimes referred to as “epigastric” because it occurs in the upper middle part of the abdomen)
- Frequent gas and/or abdominal bloating
- Foul-smelling, bulky, greasy stools that sometimes float
- In children, an inability to gain weight, delayed growth
- Malabsorption
- Fatigue (tiredness)
- Frequent diarrhea
- Malnutrition
- Vitamin deficiencies
- Unexplained weight loss
Laboratory evaluation is often necessary to diagnose pancreatic insufficiency because symptoms may not be evident or may be similar to those of other digestive tract disorders.
Pancreatic elastase 1 normal range
- Pancreatic elastase normal range: >200 mcg/g
- Moderate Pancreatic Insufficiency: 100-200 mcg/g
- Severe Pancreatic Insufficiency: <100 mcg/g
A normal amount of elastase will be present in the stool of healthy individuals.
A decreased amount of stool elastase may mean that the person tested has pancreatic insufficiency. It is not diagnostic, but it does indicate that further testing may be indicated. If your signs and symptoms continue and a strong suspicion of pancreatic insufficiency remains, your healthcare practitioner may order stool tests for fecal fat and chymotrypsin or blood tests for amylase and lipase to look at other aspects of pancreas and digestive function.
If there are not enough pancreatic enzymes (and bile from the liver) available, then fat and other foods cannot be properly digested. If a condition prevents the intestines from absorbing nutrients, then they are “lost” by elimination in the stool. In both cases – improper digestion or absorption – the affected person can experience symptoms associated with malabsorption and, in severe cases, symptoms of malnutrition and vitamin deficiency.
People with pancreatic dysfunction often need to be monitored closely by their healthcare practitioner. They may find symptom relief and nutritional improvement from prescribed enzymes taken by mouth (oral) and vitamin supplements.
References- Karnik NP, Jan A. Pancrelipase. [Updated 2019 May 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534847
- Molinari, I., et al., Fecal chymotrypsin and elastase-1 determination on one single stool collected at random: diagnostic value for exocrine pancreatic status. Clin Biochem, 2004. 37(9): p. 758-763.