Pediatric pancreatitis
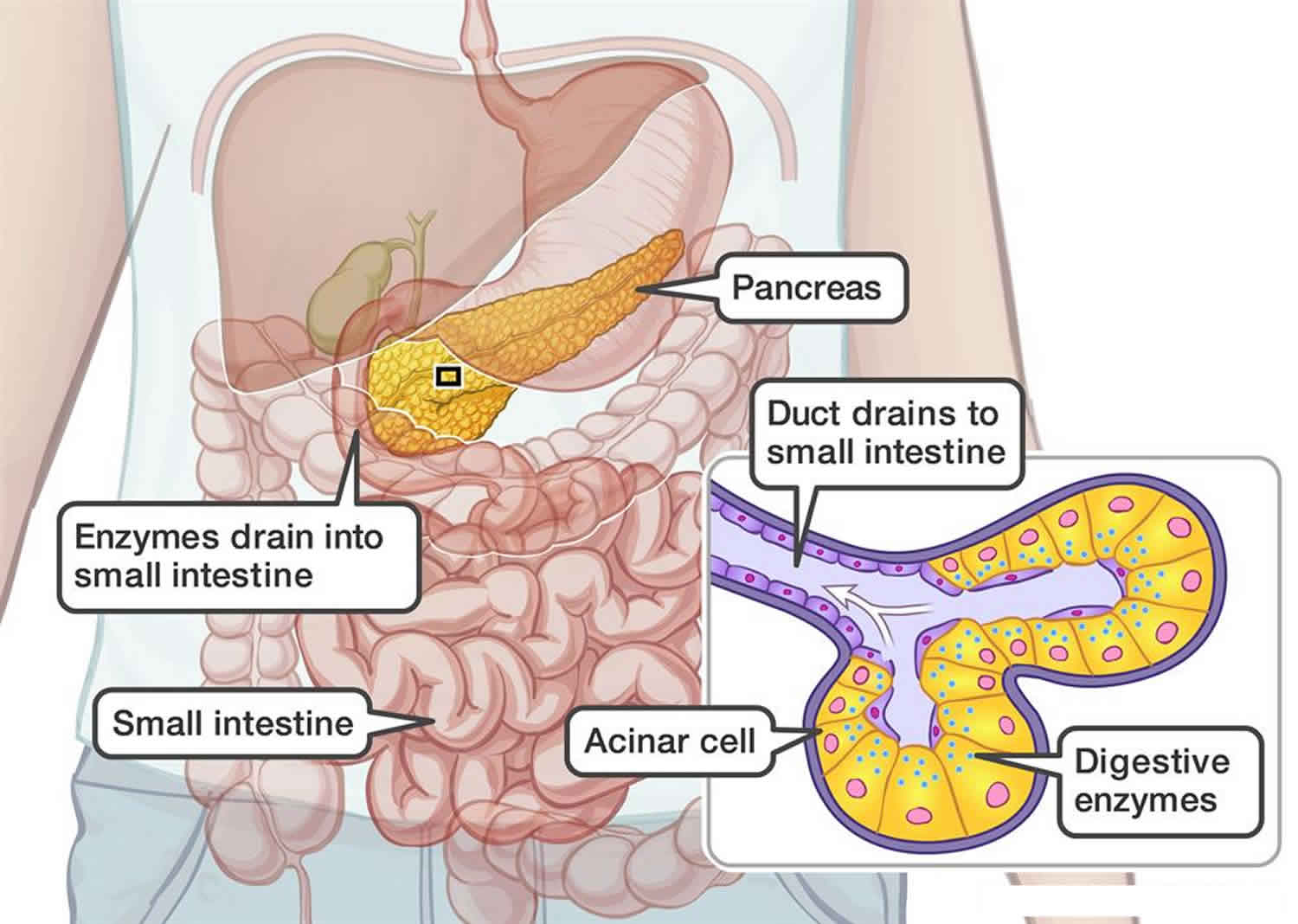
Pediatric pancreatitis is an inflammation of the pancreas in children, a large gland behind the stomach that produces digestive juices, or enzymes, that help break down food in the upper portion of the duodenum (small intestine). The pancreas also is responsible for producing insulin and glucagon, two hormones that help control levels of blood sugar, the body’s main energy source. Pediatric pancreatitis can cause symptoms like those of a stomach virus, like belly pain, vomiting, and nausea. In most cases, pancreatitis gets better on its own.
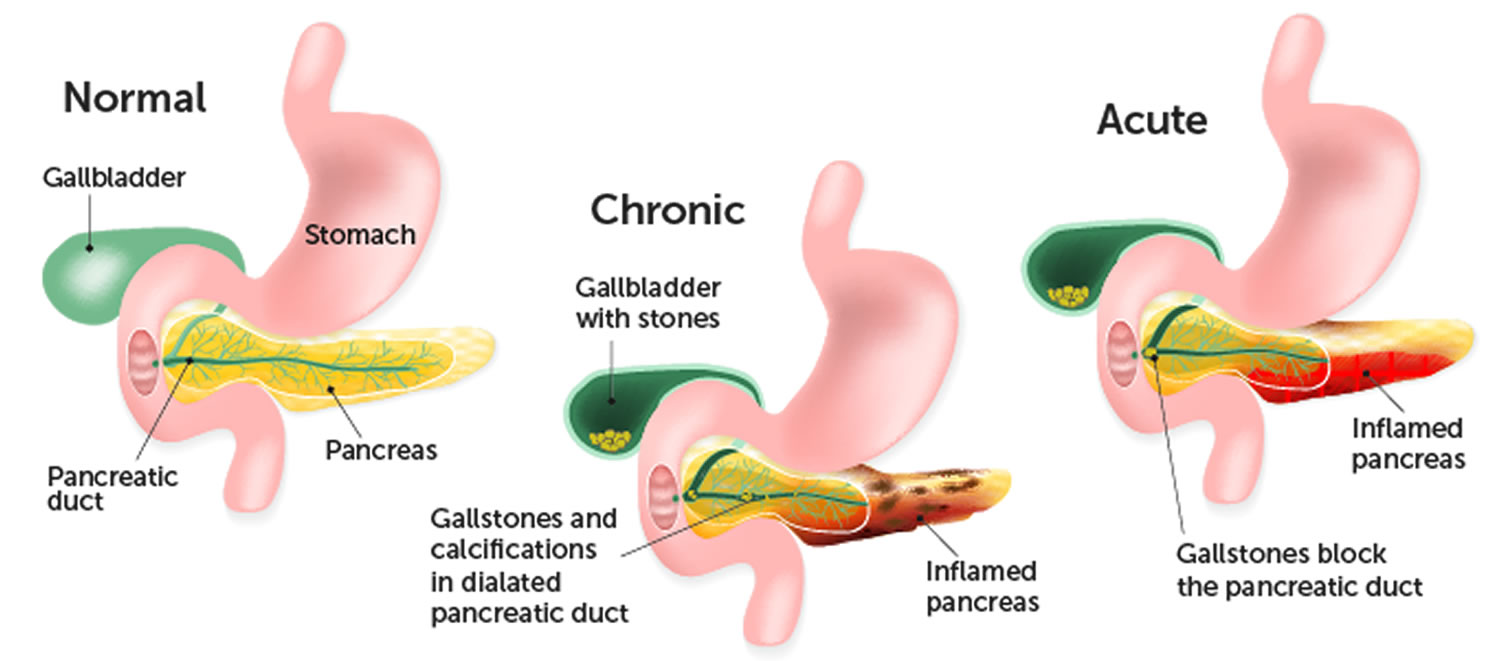
The pancreas, a large organ located in the upper abdomen and behind the stomach, plays a very important role in digestion as well as in controlling blood sugar. When the pancreas is working normally, the enzymes it secretes do not become active until they reach the duodenum. But when the pancreas is inflamed, the enzymes become activated early on (while still in the pancreas) and begin attacking internal structures. Tissues within the pancreas that produce enzymes are damaged, failing to produce new enzymes. Over time, this tissue damage can become permanent.
A normal pancreas secretes digestive enzymes that do not become active until they reach the small intestine. However, when the pancreas becomes inflamed, the digestive enzymes begin to attack the pancreas itself.
Pediatric pancreatitis can be acute (lasting for a few days) or chronic (recurring). Acute pancreatitis develops suddenly, while chronic pancreatitis develops gradually and keeps coming back. Though rare in children, chronic pancreatitis is usually inherited.
- Acute pancreatitis occurs suddenly. Typically, a child will have severe abdominal pain, perhaps with nausea and vomiting (rarely fever). The majority of cases of acute pancreatitis resolve within a week, and there are no long-term complications.
- Chronic pancreatitis can result from recurring attacks of acute pancreatitis, and where specific changes occur and impair pancreatic function. Chronic pancreatitis is rare in children and is usually part of an inherited condition.
Children usually get the acute pancreatitis, which can develop idiopathically (with no known cause) or in response to a viral infection or medication. Acute pancreatitis can result from traumatic injury to the abdomen, cystic fibrosis, or from excess fat in the blood (hyperlipidemia).
Most of the time, pancreatitis gets better on its own in about a week. As the pancreas heals, doctors can give medicine to control pain and treat nausea and vomiting. Children who can drink enough fluids and whose pain eases with oral pain medicine can be cared for at home. Children with more severe pancreatitis will need care in the hospital. They’ll get intravenous (IV) fluids and pain medicine. The healthcare team will watch for complications, such as infection, breathing problems, or kidney problems.
Doctors recommend that children with mild pancreatitis start eating as soon as possible. Children with more serious pancreatitis cases may get formula through a feeding tube that goes right into the stomach or small intestine. Some might need to get IV nutrition — called total parenteral nutrition (TPN).
Figure 1. Pancreas
Causes of pancreatitis in children
Common causes of pancreatitis in children include:
- Gallstones or problems with the ducts (tubes) in the pancreas or liver. Ten per cent to 30% of children with pancreatitis may suffer from gallstones. Treating the condition may help restore normal pancreatic function.
- Infections. Acute pancreatitis is sometimes diagnosed when a child suffers from an infection. However, it is difficult to establish a direct relationship between the two conditions. Some of the infectious diseases that have been linked to pancreatitis include: mumps, rubella, CMV, HIV, adenovirus and coxsackie virus B.
- Medications. Medications are thought to cause one quarter of the cases of pancreatitis. The most common medications that are thought to cause pancreatitis are valproic acid, L-asparaginase, prednisone and 6-mercaptopurine. It is not fully understood why these medications may cause pancreatitis. One reason may be because children treated with these drugs have other conditions that may predispose them to pancreatitis.
- Traumatic injury to abdomen. An injury to the pancreas may provoke acute pancreatitis. This type of injury may happen in a car crash, sports, falls or child abuse.
- Very high triglycerides
- Genetic or inherited disorders
- Multisystem diseases. Twenty per cent of cases of acute pancreatitis may be due to conditions affecting several organs or organ systems, such as sepsis, hemolytic-uremic syndrome or systemic lupus erythematous (SLE).
- Metabolic diseases. Metabolic disorders may be responsible for 2% to 7% of acute pancreatitis cases. Examples include errors of metabolism children are born with high lipid levels or high calcium levels.
- Anatomic abnormalities. Abnormalities in the structure of the pancreas or biliary tract can lead to pancreatitis.
Some medical conditions or illnesses, such as cystic fibrosis or celiac disease, can increase a child’s risk for pancreatitis. Sometimes, the cause of pancreatitis isn’t found, this is called idiopathic pancreatitis..
Causes of acute pancreatitis
There are many causes of acute pancreatitis, however, in approximately 30 percent of cases, a cause cannot be identified. Sometimes injury to the abdomen — such as a bicycle or playground accident or sports injury — can cause acute pancreatitis, or common medications and conditions, including:
- anti-seizure medications
- certain antibiotics
- specific types of chemotherapy
- gallstones or infections
- problems when the immune system attacks the body
- blockage of the tubes (ducts) that drain enzymes from the pancreas
- high levels of fats, called triglycerides, in the blood
- overactive parathyroid gland
Other chronic conditions may cause pancreatitis such as inflammatory bowel disease, cystic fibrosis or celiac disease.
Causes of chronic pancreatitis
Repeated episodes of acute pancreatitis can lead to chronic pancreatitis. Instead of the inflammation getting better as in acute pancreatitis, the inflammation continues in some more susceptible children and causes permanent damage to the pancreas. In some cases, genetics may be a factor. However, sometimes, the cause is unknown.
The condition lasts for long periods of time and slowly destroys the functions of the pancreas. For example, the pancreas may lose its ability to produce insulin. As a result, children can develop glucose intolerance. Chronic pancreatitis can also cause weight loss because of poor digestion. Diagnosing chronic pancreatitis relies on changes in diagnostic imaging and blood work in addition to clinical symptoms.
The pancreas is an organ located behind the stomach. It produces chemicals (called enzymes) needed to digest food. It also produces the hormones insulin and glucagon.
When scarring of the pancreas occurs, the organ is no longer able to make the right amount of these enzymes. As a result, your body may be unable to digest fat and key elements of food.
Damage to the parts of the pancreas that make insulin may lead to diabetes.
Pediatric pancreatitis symptoms
Children with pancreatitis usually have sudden, severe pain in the upper belly. They also might have pain in the back, chest, or sides. It is also important to remember that the symptoms of pancreatitis can be vague and confused with signs of other diseases, such as viral gastroenteritis. If your child is an infant and cannot verbalize pain, they may be more fussy and irritable with persistent crying.
Acute pancreatitis symptoms
A child with acute pancreatitis needs immediate medical attention and will usually require hospitalization and close monitoring. Symptoms may include:
- abdominal pain
- nausea
- vomiting
- fever
- difficulty breathing
- loss of appetite
- irritability
Your child may be more comfortable lying on their side because moving increases the pain. Your child may also feel very ill, restless and uncomfortable.
Less common symptoms include:
- ileus (where the intestines stop contracting and may become blocked)
- swollen belly (abdomen)
- jaundice (condition causing the skin, body tissues and fluids to have a yellowed colour)
- fluid build-up in the abdomen
- build-up of fluid around the lungs that can make breathing difficult
In babies and toddlers, symptoms can be more difficult to recognize. They include:
- irritability
- swollen abdomen
- fever
- bellyache (abdominal pain)
- loss of appetite
Some children who have repeated episodes of acute pancreatitis can develop chronic pancreatitis.
Chronic pancreatitis symptoms
Children usually experience signs and symptoms identical to those caused by acute pancreatitis, such as intense abdominal pain that worsens after eating a meal, nausea and vomiting and episodes will be recurrent.
The most common symptom of chronic pancreatitis is pain and discomfort in the upper abdomen, sometimes extending to the back, which may last hours or even days, and can be constant or intermittent. This pain may increase after eating and drinking.
While pain is the most common symptom, young children may not be able to communicate the severity or location of their pain.
Children with chronic pancreatitis will have symptoms related to permanent damage to the pancreas. The damaged pancreas may not produce digestive enzymes as well as a healthy pancreas, so symptoms may be related to undigested food in the gastrointestinal tract:
- Crampy abdominal pain
- Gas and bloating
- Foul-smelling, greasy diarrhea
- Poor weight gain
- Chronic weight loss, even when eating habits and amounts are normal
- Poor growth
- Nausea, vomiting and/or diarrhea
- Oily or greasy poop that is hard to flush
- Poor blood sugar control (high blood sugar or low blood sugar).
In addition, the damaged pancreas may not be able to produce hormones to regulate blood sugar. High blood sugar may cause diabetes and associated symptoms like frequent urination.
Pancreatitis or a stomach bug?
The main difference between pancreatitis and a stomach virus or other digestive system illness is the severity of abdominal pain. Children with acute pancreatitis will have severe pain in the upper abdomen that makes it difficult for them to stand or sit upright, and they’ll probably sit or lie in the fetal position to get more comfortable. After the first 2 days, the pain usually intensifies.
Other signs include:
- persistent vomiting, which increases after the first 2 days of illness
- loss of appetite
- when able to eat, inability to keep food down
- vomit that is yellowish, greenish, or brownish
- jaundice (yellow discoloration of the skin)
- fever
- in some cases, back pain or left shoulder pain
Short-term symptoms can include dehydration and low blood pressure.
Pediatric pancreatitis diagnosis
If a doctor suspects pancreatitis, the first step is to perform blood tests, like an amylase test or lipase test, to see whether the enzymes made by the pancreas are at normal working levels. If they are elevated, the doctor might order an abdominal ultrasound to check for inflammation, blockages, or stones in the pancreatic duct that leads to the first part of the duodenum, and other abnormalities.
In some cases, the doctor may order an abdominal computed tomography scan (CT) scan, which uses X-rays and computer technology to produce detailed images of the body’s internal organs, to help confirm a diagnosis of pancreatitis.
During the initial visit, the doctor might ask you to describe the color and type of your child’s vomit. If it contains a great deal of bile (greenish digestive juices from the liver), the doctor might want to further assess your child for pancreas or liver problems.
Acute pancreatitis
There is no single test to detect acute pancreatitis. The first step in the diagnosis process typically includes a blood test. This test will reveal whether there are abnormally high levels of enzymes, called amylase and lipase.
Imaging tests for acute pancreatitis may include: .
- ultrasound examination
- magnetic resonance imaging scan, also known as an MRI
- computed tomography, also called a CT scan
Blood tests and radiology scans, such as ultrasound, CT or MRI, may not always provide a clear-cut diagnosis. When this occurs, your doctor will make a clinical judgment based on your child’s history and the severity of symptoms.
Chronic pancreatitis
Unlike acute, a blood test generally does not identify chronic pancreatitis. Your clinician will perform variety of tests to determine if your child has chronic pancreatitis.
Imaging tests for chronic pancreatitis may include:
- Abdominal ultrasound: An ultrasound will indicate whether the pancreas is swollen or inflamed.
- Magnetic resonance imaging (MRI) scan: This can help rule out other causes of abdominal pain.
- Computed tomography (CT) scan: May also be used to help rule out other causes of abdominal pain.
- Endoscopic retrograde cholangiopancreatography (ERCP): A test that combines fluoroscopy (x-ray technique) with flexible endoscopy, involving a scope with a tiny high-definition camera on the end to see inside the body and help identify problems of the pancreas, pancreatic duct, liver, gallbladder and bile ducts.
In some cases, imaging tests may not always provide a clear-cut diagnosis. When this occurs, your doctor will make a clinical judgment based on your child’s history and the severity of symptoms.
Pediatric pancreatitis treatment
In most cases, pancreatitis gets better on its own. Sometimes, the doctor will recommend putting your child on a low-fat diet with plenty of fluids. This is less likely to irritate the pancreas and helps it to heal faster.
Children with a more severe case of pancreatitis who become dehydrated may need a short stay in the hospital. Treatment involves resting the pancreas by not eating or drinking, and receiving intravenous (IV) fluids and pain medication. Other medications may help to reduce the amount of acid in the body. For some children, this is enough and they can go home after a few days of treatment.
Other children might need additional treatment with special IV fluids called total parenteral nutrition (TPN). Total parenteral nutrition treatment bypasses the normal digestive process to provide the necessary nutrients of salt, glucose, amino acids, lipids, and vitamins.
Another approach is the placement of a soft plastic feeding tube called a naso-jejunal tube. This tube is guided through the nose and ends up in the small intestine, where it delivers nutrition without stimulating the pancreas. Local anesthesia is used for this procedure, so a child will experience only slight discomfort.
Once home, most children are placed on a low-fat diet to help heal the pancreas, which they should follow until their enzyme levels are back to normal. A follow-up blood test will probably be done to confirm normal enzyme levels.
Acute pancreatitis
There is no specific medication or treatment that will help the pancreas to recover. Typically, what is required is supportive care to help the body’s normal functions.
Supportive care may include:
- Providing medicine to help treat the pain.
- Giving anti-nausea medications for persistent vomiting.
- Administering intravenous fluids to ensure your child remains well hydrated.
- Acetaminophen (such as Tylenol) can treat mild pain. However, stronger pain medication, such as narcotics like morphine, may be needed.
In cases of severe pancreatitis, causing a child to not eat for many days, your doctor may recommend giving essential liquid nutrition by placing a feeding tube through the nose into the stomach or intestine. Or they may recommend providing intravenous nutrition. Nutrition is important in the healing process.
Once the pain, vomiting and discomfort associated with acute pancreatitis have resolved, your child’s appetite will slowly return. They should be encouraged to try and eat. You child’s diet will range from clear liquids to regular food. The choices will depend on what your child can tolerate.
Chronic pancreatitis
Currently, there is no specific medication or cure for chronic pancreatitis. However, many physicians offer supportive care in which they treat the symptoms in an effort to support the body’s normal function. Supportive care may include:
- medication to ease the pain associated with the condition
- provide pancreatic enzymes treatment which will help with digestion
- insulin may be given in severe cases to control the child’s sugar level
For children with chronic pancreatitis and pain, a surgical procedure called lateral pancreaticojejunostomy, or Peustow, may be recommended. This procedure connects a segment of the small intestine to the pancreas to improve drainage from the primary pancreatic duct. Another surgical option called a Total Pancreatectomy and Islet Auto Transplant, may be recommended. This complex procedure requires removing the pancreas and the hormone-producing cells and isolating and returning the cells via injection into the patient’s liver.
Pediatric pancreatitis prognosis
Fortunately, most children who develop pancreatitis get over it quickly in as little as 4 or 5 days with few or no complications. The most common complication is a collection of fluid that forms around the pancreas. This is called a pseudocyst. A pseudocyst can become infected, bleed or rupture. The fluid may go away on its own with time. However, if the fluid collection is large or if it is causing symptoms, then your doctor might suggest draining the fluid to avoid further complications.
In the unlikely case that a child develops a recurrence or complications such as cysts, bleeding, infection, or persistent pain, additional tests or surgery might be needed to rule out other conditions.
Children with chronic pancreatitis have trouble digesting food and usually need to take pancreatic enzyme supplements. Chronic pancreatitis may lead to diabetes, but this usually takes many years to happen.