Peeling skin syndrome
Peeling skin syndrome is a very rare genetic disorder characterized by widespread painless peeling of the skin in superficial sheets 1. Peeling skin syndrome is characterized by continuous shedding of stratum corneum. Peeling can be produced by rubbing skin specially if presoaked in water. Affected individuals may also experience itching and reddening of the skin. The signs and symptoms of peeling skin syndrome usually appear soon after birth, but they may also develop later in life.
Less than 100 cases of peeling skin syndrome have been reported in the medical literature. Peeling skin syndrome due to variants in the CHST8 and CSTA genes were reported in consanguineous Pakistani and in Bedouin families, respectively.
Two forms of peeling skin syndrome are recognized, namely 1:
- Acral peeling skin syndrome, which is caused by mutations in the TGM5 gene, encoding transglutaminase 5, and skin peeling is strictly limited to the hands and feet,
- Generalized peeling skin syndrome 2. Generalized peeling skin syndrome is further divided into three types, namely:
- Noninflammatory type A. Peeling skin syndrome type A is characterized by noninflammatory and asymptomatic peeling. Onset is congenital or before 6 years of age. Type A peeling skin syndrome has been shown to have its genetic basis in the CHST8 gene encoding a Golgi transmembrane N-acetylgalactosamine-4-O-sulfotransferase (GALNAC4-ST1) in 2012 3. In histology, hyperkeratosis, parakeratosis, reduction of the granular layer and acanthosis are seen. There is separation of the stratum corneum from the underlying granular layer.
- Inflammatory type B. Peeling skin syndrome type B is caused by deleterious mutations in the CDSN gene encoding corneodesmosin. Onset is congenital. The epidermis is psoriasiform with an absent or reduced granular layer, with marked parakeratosis and acanthosis. The split occurs at the level of the granular layer.
- Inflammatory type C. Peeling skin syndrome type C starts in infancy and severe palmoplantar subcorneal blistering, ichthyosis, and keratotic cheilitis. Electron microscopy of skin is helpful. Many patients have elevated IgE.
In both the peeling skin syndrome types A and B skin involvement is generalized, however, in type A presentation is erythroderma at birth, showing overlapping with camel netherton syndrome 4.
Peeling skin syndrome has an autosomal recessive pattern of inheritance. Mutations in the TGM5 gene have been identified in several patients with the acral peeling skin syndrome 5.
No effective treatment is reported for peeling skin syndrome till date. However, some improvement is seen with keratolytic agents and urea. Topical calcipotriol is also found to be little effective. Other treatment modalities such as topical tar, emollient, topical steroid, methotrexate, and phototherapy had been used but not effective.
Figure 1. Peeling skin syndrome
Footnote: Photograph of both hands. Note the erythema, swelling and remnant peeling of the skin of both hands.
Footnote: Right foot of 6 years old girl with peeling of the feet extending to the dorsum. It is more prominent on the toes. The toes are also macerated after wearing closed shoes.
Peeling skin syndrome causes
The cause of peeling skin syndrome is still unknown with an autosomal recessive inheritance.
To date, genetic changes in several distinct genes have been reported to cause the generalized type of peeling skin syndrome. These genes encode proteins that are important for formation, integrity and continual renewal of the outermost horny layer of the epidermis called stratum corneum.
Generalized peeling skin syndrome inflammatory type B (PSS1), is caused by deleterious loss-of-function changes in the corneodesmosin gene, CDSN. Corneodesmosin is a secreted glycoprotein and main component of cell-cell adhesion structures called corneodesmosomes within the stratum corneum and is also found in hair follicles. While complete loss of corneodesmosin results in generalized peeling skin syndrome, abnormal corneodesmosin (due to sequence changes on only one copy of the gene) have been described in the autosomal dominant hair disorder ‘hypotrichosis simplex’. In Japanese individuals, a particularly common cause of generalized peeling skin syndrome is a genomic deletion of 6 genes including the entire CDSN gene. The generalized inflammatory type B of peeling skin syndrome may be reminiscent of skin features in individuals with Netherton syndrome, which is caused by autosomal recessive mutations in the SPINK5 gene, and also leads to detachment of the outer horny layers of the skin.
In only very few families with generalized, non-inflammatory type A, loss-of-function changes in the carbohydrate sulfotransferase gene CHST8 causing generalized peeling skin syndrome inflammatory type B (PSS3), or in the protease inhibitor cystatin A gene CSTA causing acral peeling skin syndrome have been reported 6.
Finally, the transglutaminase-5 (TGM5) gene is responsible for the acral, localized form of peeling skin syndrome. Disease-causing genetic variants in TGM5 result in loss of function of this important cross-linking enzyme in the upper skin layers. One specific variant, p.Gly113Cys, is especially common among patients from Europe. Also CSTA-related peeling skin syndrome may be limited to hands and feet, thus demonstrating the overlap between generalized and acral forms 6.
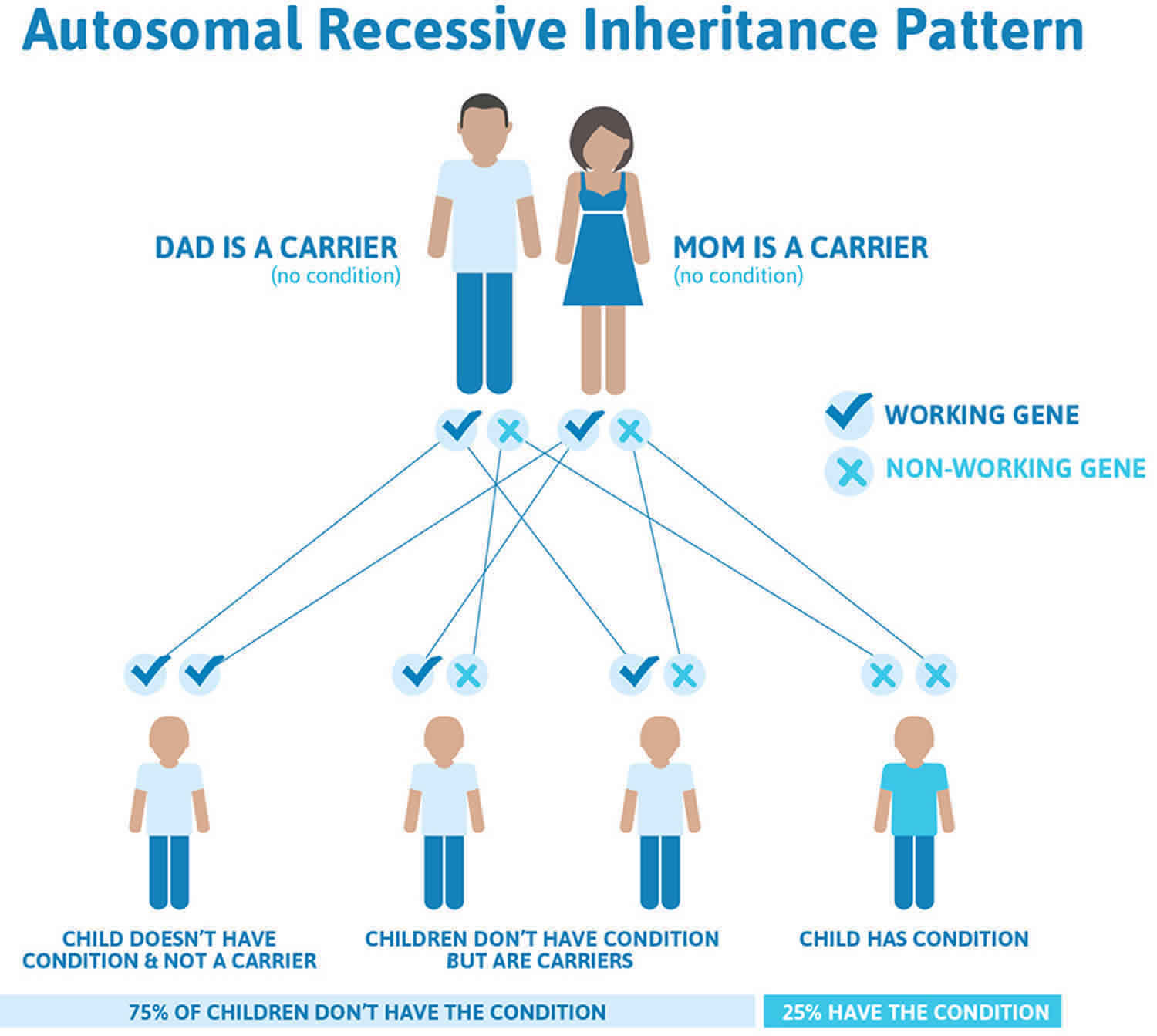
All known forms of peeling skin syndrome are inherited as autosomal recessive traits. Genetic disorders are caused by changes or variants in specific genes associated with a particular trait. The genes are located on the chromosomes received from the father and the mother.
Recessive genetic disorders occur when an individual inherits two abnormal copies of the disease gene, usually one from each parent. If an individual receives one normal gene copy and one abnormal gene copy for the disease, the person will be a carrier for the disease, but usually will not show symptoms. The risk for two carrier parents to both pass the altered gene copy and, therefore, have an affected child is 25% with each pregnancy. The risk to have a child who is a carrier like the parents is 50% with each pregnancy. The chance for a child to receive normal genes from both parents and be genetically normal for that particular trait is 25%. The risk is the same for males and females.
All individuals are thought to be carriers for at least 4-5 abnormal recessive genes. Parents who are close relatives (consanguineous) have a higher chance than unrelated parents to both carry the same abnormal gene, which increases the risk to have children with a recessive genetic disorder.
To discuss the risk of having children with this disorder and the possibility of genetic testing, genetic counseling may be of benefit for affected individuals and their families.
Figure 2. Peeling skin syndrome autosomal recessive inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Peeling skin syndrome symptoms
Peeling skin syndrome is a form of congenital ichthyosis with autosomal recessive inheritance. The ichthyoses comprise a group of dermatological disorders characterized by dry, thickened, scaly skin involving all or most of the body. Individuals with peeling skin syndrome exhibit lifelong spontaneous, painless, shedding or peeling of the outermost layer of the skin (horny layer or stratum corneum). Often, affected individuals and/or their caregivers can remove sheets of skin manually, comparable to skin peeling after a severe sunburn.
Other findings associated with peeling skin syndrome may include itching, short stature, and/or newly formed hairs that can be plucked out more easily than normal. Peeling skin syndrome is caused by a superficial detachment of the outermost horny layers of the skin. The generalized form of peeling skin syndrome has been further sub-classified into a non-inflammatory type (A) and an inflammatory type (B).
In some people, peeling skin syndrome is limited to the arms and legs (acral extremities), diagnosed as “acral peeling skin syndrome”. In the acral peeling skin syndrome, most patients develop blisters and erosions on hands and feet at birth or during infancy, which is reminiscent of another blistering skin disorder, epidermolysis bullosa simplex.
Peeling skin syndrome diagnosis
A good history and physical exam are often sufficient to make the diagnosis, although specialized tests including surgical removal and microscopic evaluation (biopsy) of affected tissue may be necessary at times. The continual shedding of large sheets of skin distinguishes peeling skin syndrome from Netherton syndrome and from other types of autosomal recessive congenital ichthyosis, such as congenital ichthyosiform erythroderma. The skin of so-called “collodion babies” peels off after a few weeks and does not return, in contrast to patients with peeling skin syndrome whose symptoms return time after time.
Peeling skin syndrome treatment
Treating peeling skin syndrome by applying skin softening (emollient) ointments, especially after a bath while the skin is moist, may offer some relief. Plain petroleum jelly or Vaseline is preferred. None of the corticosteroids or systemic retinoids (vitamin A derivatives) is indicated or effective and all may have serious side effects or adverse reactions.
Acral peeling skin syndrome
Acral peeling skin syndrome is a skin disorder characterized by painless peeling of the top layer of skin. The term “acral” refers to the fact that the skin peeling in this condition is most apparent on the hands and feet 7. Occasionally, peeling also occurs on the arms and legs. The peeling is usually evident from birth, although the condition can also begin in childhood or later in life. Skin peeling is made worse by exposure to heat, humidity and other forms of moisture, and friction. The underlying skin may be temporarily red and itchy, but it typically heals without scarring. Acral peeling skin syndrome is not associated with any other health problems.
Acral peeling skin syndrome is a rare condition, with several dozen cases reported in the medical literature 8. However, because its signs and symptoms tend to be mild and similar to those of other skin disorders, the condition is likely underdiagnosed.
There is currently no effective treatment for acral peeling skin syndrome 9. Treatments with analgesics, emollients, anti-histamines, keratolytics, methotrexate, steroids, isotretinoin, and ultraviolet rays have all been tried with limited successes 9. Until there is adequate understanding of the cause of peeling skin syndrome sufficient to inform the development of effective treatment, management remains symptomatic. Considering the current lack of an effective treatment, genetic counseling is mandatory, as this promotes patient understanding of the condition and helps patients to cope 10.
Acral peeling skin syndrome causes
Acral peeling skin syndrome is caused by mutations in the TGM5 gene. This gene provides instructions for making an enzyme called transglutaminase 5, which is a component of the outer layer of skin (the epidermis). Transglutaminase 5 plays a critical role in the formation of a structure called the cornified cell envelope, which surrounds epidermal cells and helps the skin form a protective barrier between the body and its environment.
TGM5 gene mutations reduce the production of transglutaminase 5 or prevent cells from making any of this protein. A shortage of transglutaminase 5 weakens the cornified cell envelope, which allows the outermost cells of the epidermis to separate easily from the underlying skin and peel off. This peeling is most noticeable on the hands and feet probably because those areas tend to be heavily exposed to moisture and friction.
Acral peeling skin syndrome inheritance pattern
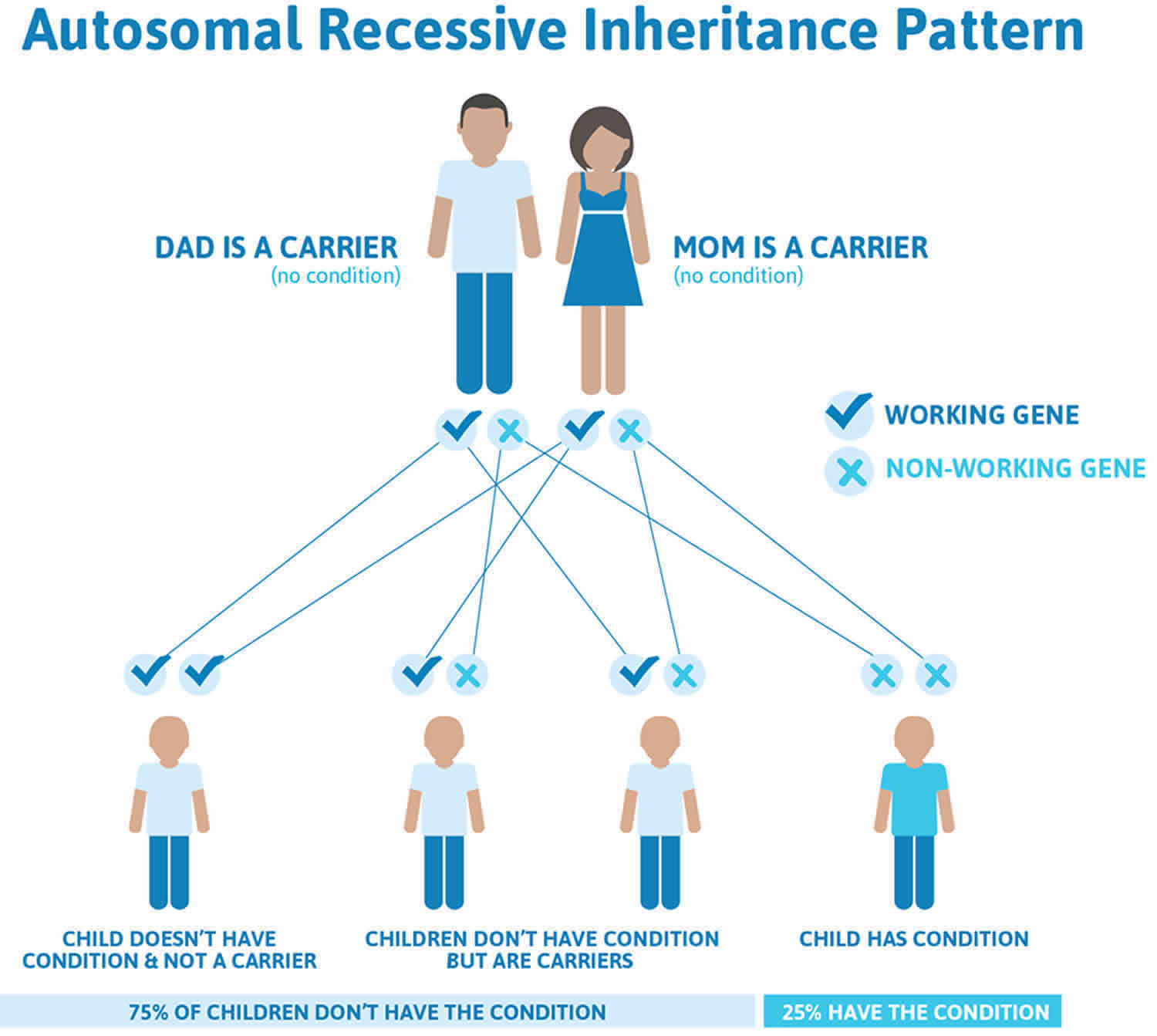
Acral peeling skin syndrome is inherited in an autosomal recessive pattern, which means both copies of the gene in each cell have mutations 11. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition.
It is rare to see any history of autosomal recessive conditions within a family because if someone is a carrier for one of these conditions, they would have to have a child with someone who is also a carrier for the same condition. Autosomal recessive conditions are individually pretty rare, so the chance that you and your partner are carriers for the same recessive genetic condition are likely low. Even if both partners are a carrier for the same condition, there is only a 25% chance that they will both pass down the non-working copy of the gene to the baby, thus causing a genetic condition. This chance is the same with each pregnancy, no matter how many children they have with or without the condition.
- If both partners are carriers of the same abnormal gene, they may pass on either their normal gene or their abnormal gene to their child. This occurs randomly.
- Each child of parents who both carry the same abnormal gene therefore has a 25% (1 in 4) chance of inheriting a abnormal gene from both parents and being affected by the condition.
- This also means that there is a 75% ( 3 in 4) chance that a child will not be affected by the condition. This chance remains the same in every pregnancy and is the same for boys or girls.
- There is also a 50% (2 in 4) chance that the child will inherit just one copy of the abnormal gene from a parent. If this happens, then they will be healthy carriers like their parents.
- Lastly, there is a 25% (1 in 4) chance that the child will inherit both normal copies of the gene. In this case the child will not have the condition, and will not be a carrier.
These possible outcomes occur randomly. The chance remains the same in every pregnancy and is the same for boys and girls.
Figure 3 illustrates autosomal recessive inheritance. The example below shows what happens when both dad and mum is a carrier of the abnormal gene, there is only a 25% chance that they will both pass down the abnormal gene to the baby, thus causing a genetic condition.
Figure 3. Acral peeling skin syndrome autosomal recessive inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Acral peeling skin syndrome symptoms
Acral peeling skin syndrome is considered a subtype of peeling skin syndrome in which the peeling of the skin is limited to the dorsa of the hands and the feet 12. The skin peeling is due to separation of the stratum corneum from the stratum granulosum 13.
Clinically, acral peeling skin syndrome is asymptomatic peeling with residual erythema for a few days that later heal spontaneously without scaring 14. The onset of acral peeling skin syndrome is variable, but in the majority of the cases reported, the disease developed shortly after birth. Acral peeling skin syndrome has been described to affect predominantly the dorsal aspects of the hands and the feet 12. However, Hashimoto et al. 15 described a 34 year old patient with peeling of the plantar and the dorsal of the feet. The variability in the phenotypic expression of acral peeling skin syndrome indicates that the heterogeneity of clinical findings is not only between families, but also within family members.
The symptoms of acral peeling skin syndrome are aggravated by hot temperatures, high humidity and friction 14.
Hashimoto et al. 15 and Wakade et al. 16 demonstrated that skin hydration by soaking in water for 5-10 minutes induced blistering in their patients Hyperhidrosis produces a similar effect as soaking the limbs in water.
Acral peeling skin syndrome diagnosis
History and physical examination are only suggestive, and diagnosis of acral peeling skin syndrome is only confirmed by histology of skin biopsy and genetic studies 7. Histology typically shows hyperkeratosis, psoriasiform hyperplasia, hypergranulosis with keratinohyalin granules and cleavage of the stratum corneum from the stratum granulosum – a key histological feature of peeling skin syndrome.
Genetic studies and testing show an autosomal recessive pattern and are important for identifying mutations and for profiling risks of transmitting mutant genes to future generations. This is especially crucial in populations where consanguineous marriages are practiced. Genetic mutations in the TGM5 or CSTA genes are implicated in acral peeling skin syndrome, while of the 2 generalized variants, only the type B, inflammatory generalized type, has been associated with a homozygous non-sense mutation in the CSDN gene (which encodes corneodesmosin) 17.
Acral peeling skin syndrome treatment
There is no effective treatment for acral peeling skin syndrome reported. Management of this condition is largely symptomatic and preventative. Emollients are useful to some patients while the use of keratolytics may enhance the shedding. Topical tretinoin was found to be ineffective in this patient. Similarly, Phototherapy, oral corticosteroids and methotrexate were found to be in effective 18. Calcipotriol was reported to be effective in one case report 19.
References- Singhal AK, Yadav DK, Soni B, Arya S. A Case of Peeling Skin Syndrome. Indian Dermatol Online J. 2017;8(3):208–210. doi:10.4103/idoj.IDOJ_118_16 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5447344
- Cassidy AJ, van Steensel MA, Steijlen PM, van Geel M, van der Velden J, Morley SM, et al. A homozygous missense mutation in TGM5 abolishes epidermal transglutaminase 5 activity and causes acral peeling skin syndrome. Am J Hum Genet. 2005;77:909–17.
- Cabral RM, Kurban M, Wajid M, Shimomura Y, Petukhova L, Christiano AM. Whole-exome sequencing in a single proband reveals a mutation in the CHST8 gene in autosomal recessive peeling skin syndrome. Genomics. 2012;99:202–8.
- Sárdy M, Fáy A, Kárpáti S, Horváth A. Comel–Netherton syndrome and peeling skin syndrome type B: Overlapping syndrome or one entity? Int J Dermatol. 2002;41:264–8.
- Peeling skin syndrome. https://www.orpha.net/consor/cgi-bin/OC_Exp.php?lng=EN&Expert=817
- Acral peeling skin syndrome resulting from a homozygous nonsense mutation in the CSTA gene encoding cystatin A. Pediatr Dermatol. 2013 Sep-Oct;30(5):e87-8. doi: 10.1111/pde.12092. Epub 2013 Mar 28. https://doi.org/10.1111/pde.12092
- Mathew R, Omole OB, Rigby J, Grayson W. Adult-onset acral peeling skin syndrome in a non-identical twin: a case report in South Africa. Am J Case Rep. 2014;15:589–592. Published 2014 Dec 31. doi:10.12659/AJCR.892110 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4319446
- Acral peeling skin syndrome. https://ghr.nlm.nih.gov/condition/acral-peeling-skin-syndrome
- Kiprono SK, Chaula BM, Naafs B, Masenga JE. Acral peeling skin syndrome in two East-African siblings: case report. BMC Dermatol. 2012;12:2. Published 2012 Mar 19. doi:10.1186/1471-5945-12-2 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3341202
- Al-Mohaimeed AA, Sharaf FK. Breaking bad news issues: A survey among physicians. Oman Med J. 2013;28:20–25.
- Kavaklieva S, Yordanova I, Bruckner-Tuderman L, Has C. Acral peeling skin syndrome resembling epidermolysis bullosa simplex in a 10-month old boy. Case Rep Dermatol. 2013;5:210–14.
- Cassidy AJ, van Steensel MAM, Steijlen P, van Geel M, van der Velden J, Morley SM, Terrinoni A, Melino G, Candi E, McLean WHI. A homozygous missense mutation in TGM abolishes epidermal transglutaminase 5 activity and causes acral peeling skin syndrome. Am J Hum Genet. 2005;77:909–917. doi: 10.1086/497707
- Garcia EG, Carreno RG, Gonzalez MA, Reyes JJ. A crap peeling skin syndrome: a report of two cases. Ultrastruct Pathol. 2005;29:65–70. doi: 10.1080/01913120590909867
- Kharfi M, El Fekih N, Ammar D, Jaafoura H, Schwonbeck S, van Steensel MA, Fazaa B, Kamoun MR, Fischer J. A missense mutation in TGM causes acral peeling skin syndrome in a Tunisian family. J Invest Dermatol. 2009;129:2512–2515. doi: 10.1038/jid.2009.118
- Hashimoto K, Hamzavi I, Tanaka K, Shwayder T. Acral peeling skin syndrome. J Am Acad Dermatol. 2000;43:1112–1119. doi: 10.1067/mjd.2000.103645
- Wakade O, Adams B, Shwayder T. Acral peeling skin syndrome: a case of two brothers. Pediatr Dermatol. 2009;26(3):328–330. doi: 10.1111/j.1525-1470.2009.00917.x
- Krunic AL, Stone KL, Simpson MA, McGrath JA. Acral peeling skin syndrome resulting from a homozygous nonsense mutation in the CSTA gene encoding cystatin A. Pediatr Dermatol. 2013;30:e87–88.
- Levy S, Goldsmith L. The peeling skin syndrome. J Am Acad Dermatol. 1982;7:909–917.
- Mizuno Y, Suga Y, Hasegawa T, Haruna K, Kohroh K, Ogawa H, Ikeda S, Shimizu T, Komatsu N. A case of peeling skin syndrome succesfully treated with topical calcipotriol. J Dermatol. 2006;33:430–432. doi: 10.1111/j.1346-8138.2006.00102.x