What is a PEG tube
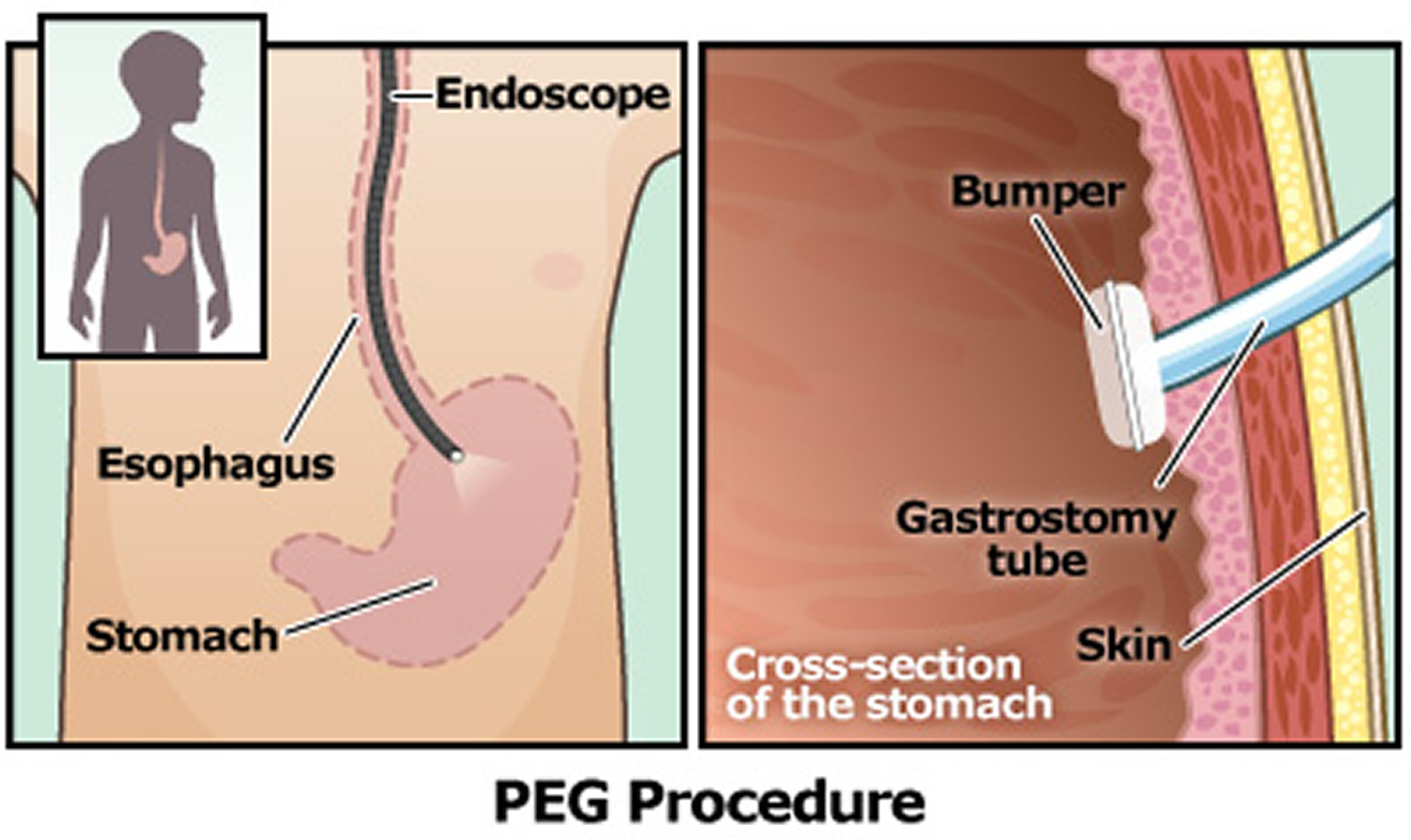
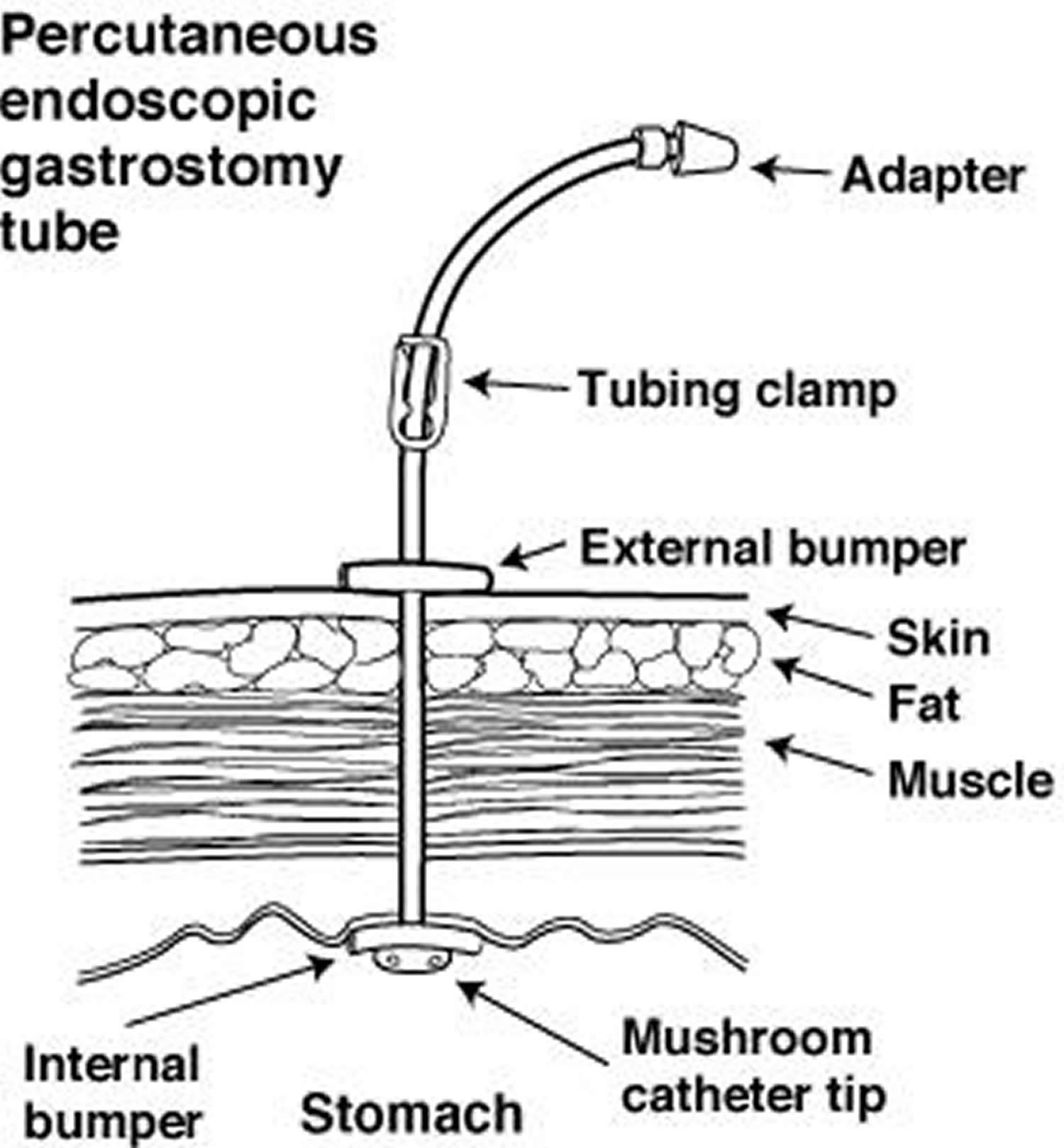
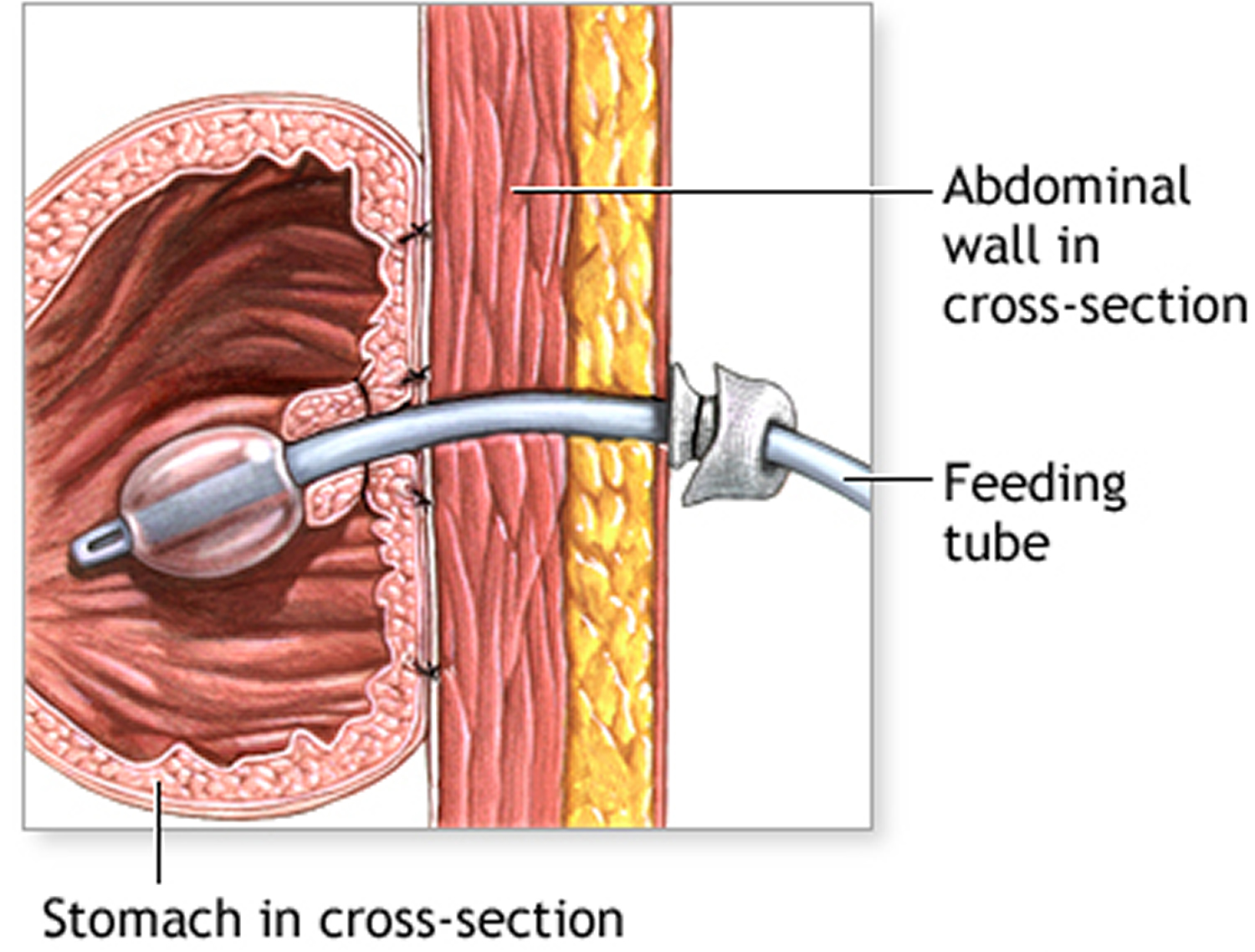
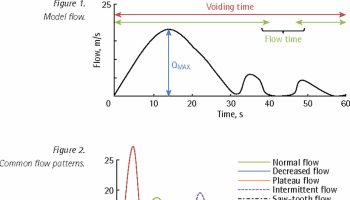
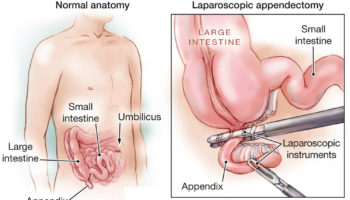
PEG tube stands for the abbreviation Percutaneous Endoscopic Gastrostomy (PEG) tube [Percutaneous (through the skin) – Endoscopic (using an endoscopic instrument) – Gastrostomy (means to the stomach)] is also called gastrostomy tube, which is a feeding tube that is a safe and effective way to provide food, liquids and medications (when appropriate) directly into the stomach. An endoscope is a long thin flexible tube with a small camera and light attached which allows the doctor to see the pictures of the inside of your gut on the video screen. The endoscope allows the doctor to choose the best location in the stomach to place the PEG tube. The PEG tube procedure is done for patients who are having trouble swallowing. PEG tube placement can generally be performed under local anesthesia rather than general anesthesia. The surgeon will give you an injection of local anaesthetic into the skin. An endoscope is passed into the mouth, down the esophagus, and into the stomach. Your stomach connects the esophagus to the small intestine, and acts as an important reservoir for food, prior to delivery to the small intestine (see Figure 1). Once the location is chosen and under direct visualization with the endoscope, a small opening is made on the outside of abdomen into the stomach. After the opening is made, the top part of the PEG tube is pulled up out of the stomach through the skin of the abdomen (abdominal wall). The top of the PEG tube rests on the skin and the bottom part of the PEG, which is shaped like bulb, remains inside the stomach. This bulb shape anchors the tube in the stomach and prevents it from coming out.
PEG gastrostomy tubes avoid the need for general anesthesia and a large incision. This procedure may or may not require a sedation anaesthetic.
However, if the PEG tube can’t be placed into your stomach, you may have a percutaneous endoscopic jejunostomy (PEJ) tube placed instead. A percutaneous endoscopic jejunostomy (PEJ) tube is placed in your jejunum, which is the second part of your small intestine.
PEG tube is prevented from coming out of the stomach by one of several methods. Some brands have a small wire within the tube, which after insertion is pulled from the exterior end of the tubing causing the portion within the stomach to curl up or “pigtail,” preventing it from being pulled out. Other systems employ a very small balloon at the end of the tube which is inflated within the stomach after insertion, serving the same purpose. Removal of the PEG tube simple involves cutting the wire which created the pigtail, or deflating the balloon section of the tube allowing it to slip easily from the stomach. About three inches of tubing will protrude from the incision area. Initially, there may be some discomfort while getting used to using the system, from gas or air, or from adjusting to the liquid foods themselves.
Your physician may recommend that you have PEG tube feeding tube procedure if you require long term nutritional support because you are unable to eat food normally, in order to make sure you are getting adequate nutrition.
PEG tube procedure can also be performed to shrink the stomach in cases of a bowel obstruction.
PEG tubes are inserted for other various reasons. They may be needed temporarily or permanently.
The PEG tube which is made of silicone, must stay in the stomach for about three months to allow the tract (hole) to heal between the abdomen and the stomach. The tract must be well healed so it is safe for the gastrostomy tube to be changed.
PEG tube might be recommended if you have difficulty eating, but your digestive system works normally. Examples include:
- Cancer, such as head and neck cancers, or cancer treatment that makes it difficult or painful to swallow
- Neurological problems, such as stroke and amyotrophic lateral sclerosis (ALS)
- Gastrointestinal problems, such as delayed gastric emptying (gastroparesis) and bowel obstruction
- Trauma, such as an injury to your digestive tract
- Birth defects of the mouth, esophagus, or stomach (esophageal atresia or tracheal esophageal fistula)
- Problems with sucking and/or swallowing, for example in patients debilitated by stroke or dementia
First introduced in 1980, today more than 200,000 patients every year receive PEG tube therapy.
What are possible complications of PEG tube
- Infection
- Chest infection
- Bleeding
- Blocked tube
- Peritonitis
- PEG tube falling out
- Damage to the liver or intestine
- Buried internal bolster
- Leaking
- Allergic reaction
- Breathing difficulties or heart irregularities
- Making a hole in the esophagus or stomach
- Damage to teeth or bridgework
- Death
PEG tube feeding
Your stomach and abdomen generally heals in 5 to 7 days. Moderate pain can be managed with medications. You will be fed intravenously (IV) for at least 24 hours. Feedings will begin when your bowel sounds are heard. Feedings will start slowly with clear liquids and gradually be increased.
You and your family will be taught:
- how to care for the skin around the tube
- signs and symptoms of infection
- what to do if the tube is pulled out
- signs and symptoms of tube blockage
- how to empty (decompress) the stomach through the tube
- how and what to feed through the gastrostomy tube
- how to conceal the tube under clothing
- what normal activities can be continued
Feeding through the PEG tube
Clear fluids, often water, will be given initially through the PEG tube 6-24 hours after its insertion. Once this is tolerated, then feeds and medications may be given through the tube. Medications can also be given through the PEG tube but care is needed as some medications can clog up the tubing. Your pharmacist will advise you with this.
What are the risks of a PEG tube?
Complications can occur with the PEG placement. Possible complications include pain at the PEG site, leakage of stomach contents around the tube site, and dislodgment or malfunction of the tube. Possible complications include infection of the PEG site, aspiration (inhalation of gastric contents into the lungs), bleeding and perforation (an unwanted hole in the bowel wall). Your doctor can describe for you symptoms that could indicate a possible complication.
When the PEG tube is used for feeding there are 2 major common risks:
- the feeding tube may become dislodged or blocked by medications or feeding fluid and
- you can get pneumonia if you aspirate any of the feeding fluid.
Chronic leakage around the site is NOT normal. If the PEG stoma is oozing blood, food, stomach acids, or any other substance, then you need to see your GI or visit the emergency room immediately.
How long does the PEG tube last?
This depends on the type of tube you have inserted, and how it is looked after.
A PEG tube can last up to a year but will need to be changed every so often due to the stomach acids. The PEG tubes can become blocked by food, residue or medications. It should be flushed well after each use.
If the PEG tube falls out, it is important to have another tube placed as soon as possible to prevent the hole closing over.
The PEG tube can be replaced by another tube or by a low profile device, also called a ‘button’. You should discuss this option with your doctor when your PEG tube is due to be changed.
If the PEG tube is no longer needed it can be simply removed and the exit hole will quickly close over. Sometimes it may require a small operation by a surgeon to repair the hole once the tube is removed.
How are feedings given? Can I still eat and drink?
Specialized liquid nutrition, as well as fluids, are given through the PEG tube. If the PEG tube is placed because of swallowing difficulty (e.g., after a stroke), there will still be restrictions on oral intake. Although a few PEG patients may continue to eat or drink after the procedure, this is a very important issue to discuss with your physician.
Are there any alternatives to a PEG tube?
Nutritional support is an important component of care for the critically ill. It is possible to be given nutrients and fluids through a naso-gastric tube.
The feeding tube can be placed directly into your stomach by an operation.
It is also possible to be given nutrients and fluids directly into your bloodstream (parenteral nutrition).
For patients with a functioning gastrointestinal (GI) tract, enteral nutrition is preferred to parenteral nutrition (into your bloodstream). Enteral nutrition is safer, more physiologic, and economical 1. In the intensive care unit (ICU) setting, enteral nutrition is associated with a decreased likelihood of developing infections when compared to parenteral nutrition. In patients with acute pancreatitis, use of enteral nutrition is also associated with a reduction in hospital length of stay and a trend toward reduced organ failure when compared to parenteral nutrition. Patients who have a functioning gastrointestinal (GI) tract but are unable to safely ingest oral intake are fed via enteral access. In patients in whom long-term enteral access is required, endoscopically placed enteral access is recommended. Percutaneous endoscopically placed gastrostomy (PEG) and jejunostomy (PEJ) tubes are utilized for long-term enteral nutrition.
What if the PEG tube comes out before the gastrostomy tract has healed?
It rarely happens with a PEG tube and sometimes happens with the Malecot® or balloon gastrostomy tubes. If the tube becomes accidentally dislodged call your doctor for instructions.
If you do not speak to a doctor or nurse after thirty (30) minutes, go to nearest emergency room in a hospital for tube reinsertion (make sure you bring your gastrostomy supplies with you). A tube will be placed into the gastrostomy tract to prevent closure and the need for another operation. If the emergency room doctors and nurses have questions, they can call your gastroenterologist, or surgeon who placed the tube.
If you do not have a replacement gastrostomy tube to take with you, a FOLEY® catheter of the same size or smaller can be inserted as a replacement tube. Often, a special x-ray called a “gastrostomy tube dye study” will need to be taken to make sure the newly placed tube is in the stomach. A FOLEY® catheter can be used for feeding and stomach decompression at home. Call your GI or surgical doctor or nurse if you required a visit to the emergency room for care of your gastrostomy tube.
Figure 1. Stomach
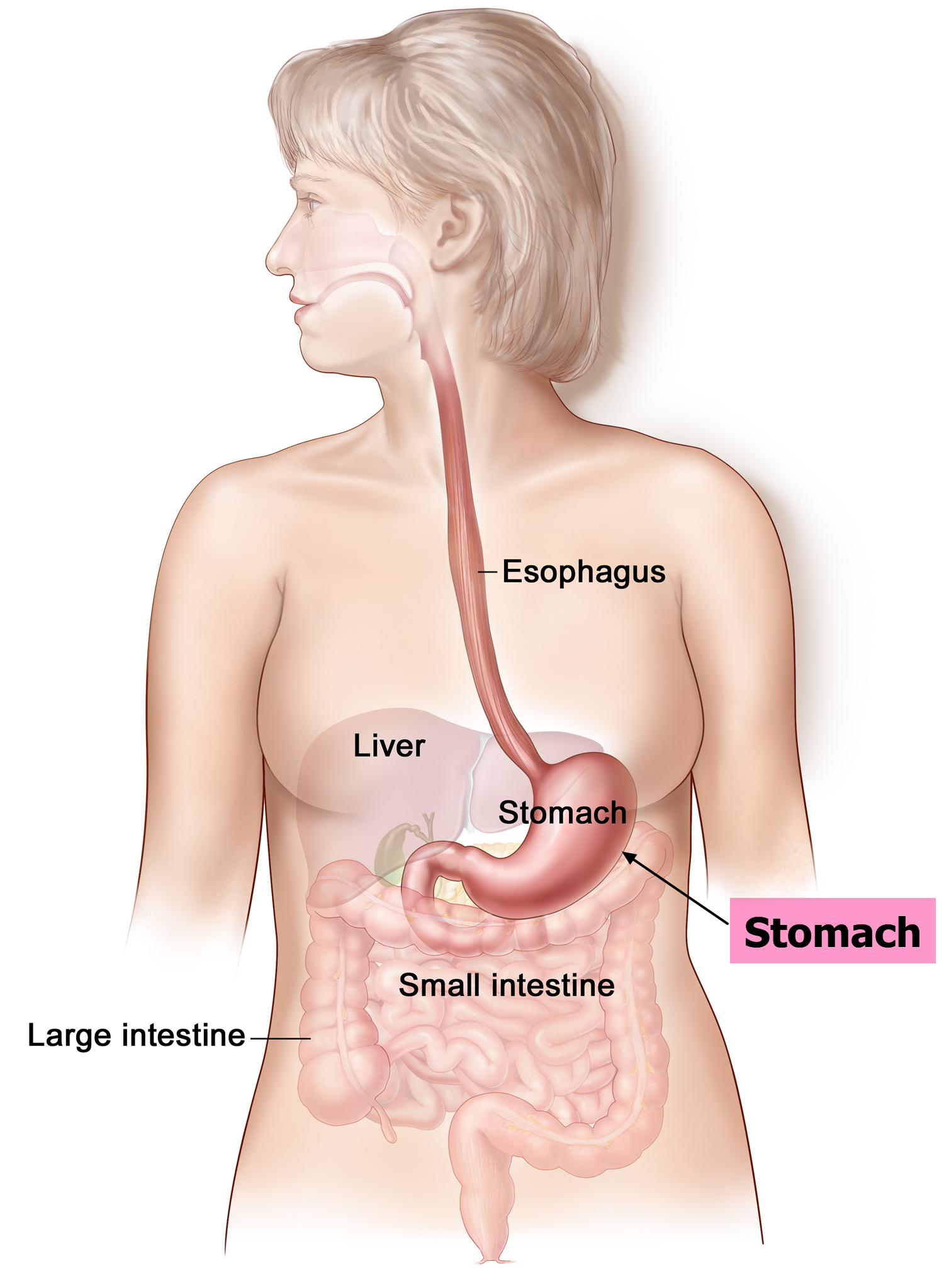 Figure 2. PEG tube – a small, flexible, hollow tube (catheter) with a balloon or flared tip is inserted into the stomach. The stomach is stitched closed around the tube and the incision is closed.
Figure 2. PEG tube – a small, flexible, hollow tube (catheter) with a balloon or flared tip is inserted into the stomach. The stomach is stitched closed around the tube and the incision is closed.PEG tube placement
During the PEG tube placement procedure, a physician places an endoscope (a long, thin, flexible instrument about 1/2 inch in diameter) into your mouth. The endoscope is then advanced through your esophagus (the “food pipe” leading from your mouth into your stomach) and into your stomach. The endoscope is used to ensure the correct positioning of the PEG tube (also called a feeding tube) in your stomach. The PEG tube rests in the stomach and comes out through the skin of the abdomen.
The percutaneous endoscopic gastrostomy (PEG) tube provides nutrition for patients who are having trouble swallowing. The internal bumper rests in the stomach, and the adapter comes out through the skin of the abdomen.
Before the PEG tube placement procedure
You will meet with a physician, dietitian and home care coordinator. They will review your history, discuss the procedure and answer any questions you might have.
Special conditions
Tell the physician if you have a lung or heart condition, a bleeding tendency or if you are allergic to any medications.
Medications
- If you have diabetes and use insulin, you may need to adjust the dosage of insulin the day of the test. Your primary physician will help you with this adjustment. Bring your diabetes medication with you so you can take it after the procedure.
- Tell your primary physician if you are taking blood thinning medications such as Coumadin (warfarin), dalteparin (Fragmin®), heparin, tinzaparin (Innohep®), enoxaparin (Lovenox®), clopidogrel (Plavix®), cilostazol (Pletal®), Persantine (dipyridamole) or Ticlid (ticlopidine hydrochloride). Your primary physician may prescribe an alternate method for thinning your blood before the procedure.
- Within 1 week before the PEG tube placement procedure, do NOT take aspirin, products containing aspirin or anti-inflammatory drugs (such as ibuprofen including Advil or Motrin; Naprosyn or Indocin).
- Please note: Do not discontinue any medication without first consulting with your primary or referring physician.
Eating and drinking
Do not eat or drink anything for 8 hours before the procedure.
Transportation
You will need to bring a responsible adult to accompany you after the procedure. You should not drive or operate machinery for 24 hours. The medication given during the procedure may cause drowsiness, making it unsafe for you to drive or operate machinery.
Overnight accommodations
You may be asked to stay overnight at a location that is within 30 minutes from where your procedure was performed.
On the day of the PEG tube placement procedure
You may need to stay overnight in the hospital after the procedure, so please pack any personal items that you may need.
You will meet with a physician who will explain the procedure in detail, including possible complications and side effects. The physician will also answer any questions you may have.
During the PEG tube placement procedure
- You will asked to wear a hospital gown and to remove your eyeglasses and/or dentures, if you have them.
- The procedure is performed by a physician with experience in the PEG procedure.
- You are given a pain reliever and sedative intravenously (in your vein). You will feel relaxed and drowsy.
- You are given a local anesthetic (pain-relieving medication) at the site where the PEG tube is placed.
- The endoscopy physician inserts an endoscope through your mouth and into your stomach. The endoscope does not interfere with your breathing.
- Through the endoscope, your physician will view the stomach lining to determine the PEG tube insertion site.
- A small incision is made in the abdominal wall where the PEG tube will exit.
- The PEG tube placement procedure lasts from 30 to 45 minutes.
After the PEG tube placement procedure
You will be taken to the Post Anesthesia Care Unit (PACU), where your nurse will monitor your temperature, heart rate, breathing, and blood pressure. They will also check the bandage around your tube. You will stay in the PACU until you’re fully awake.
- You will be observed closely for any complications.
- The PEG tube will be secured to your abdomen with tape.
- A responsible adult must accompany you after the procedure. Do not drive or operate machinery for 24 hours.
- You should expect to see some drainage around the PEG tube for the first 24 to 48 hours.
- A sterile gauze dressing will be placed around the incision. Your nurse will change the dressing as needed.
- Once the dressing has been removed and the area has healed, be sure to wash the area daily with soap and water.
- A dietitian will teach you how to use and care for your PEG tube, and you will be started on enteral tube feeding (feeding directly through the gastrointestinal tract).
- Your dietitian will help you choose a commercially prepared formula for the tube feeding.
- For a couple of days, you may have minor soreness in your abdomen where the PEG tube was inserted. This will feel like a pulled muscle. You will receive medication to help relieve this pain the first few days after the procedure.
- The amount of care needed for the PEG tube varies among patients. Generally, PEG tubes do not need to be replaced for several months, and may even function well for 2 or 3 years.
- If you are having difficulty with your PEG tube, please call your health care provider.
At home
- You may feel some soreness in your throat. This is normal and will get better in 1 or 2 days.
- You may have some discomfort at your incision site for the first 24 to 48 hours. If so, take your pain medication as instructed.
- You can shower 48 hours after your procedure. Don’t take tub baths or go swimming for 2 weeks after your procedure.
- You may see dark green or yellow drainage around your PEG or PEJ site. A small amount of green or yellow drainage is normal.
PEG tube care
Skin care with the PEG tube
Cleanse the area around the PEG tube with water for the first two days after placement. After this, daily bathing with soap and water is all that is necessary. Daily showers should be sufficient to keep the stoma site clean after it has healed from the initial surgery. To clean the skin around the PEG tube, lift up the flap, inspect the area; wash the skin with soap and water and dry the skin completely. Most PEG tubes do not need a dressing. A small amount of drainage is normal. Turn the tube with each feeding to prevent skin irritation.
Every day, inspect the skin around your feeding tube for any redness, swelling, or pus. Tell your doctor or nurse if you’re having any of these symptoms.
The PEG tube is marked at the point where it should be level with the incision and should be checked regularly to make sure it is still properly in place. Excessive tension on the tube may result in pressure necrosis (death of an area of tissue) of the interior abdominal wall. Excessive tension may also cause the tube to be pulled out prematurely.
If the tube becomes too loose, spacers, may be placed between the PEG and the skin to provide a better fit. If the tube gets too tight and there are spacers in place, these can be removed anytime, by your GI nurse or doctor.
Should the PEG tube accidentally come out, the original tube–or a replacement–needs to be placed back in the stoma as soon as possible or the incision will begin to heal, and new surgery may be required. Stomas could begin to close up in less than two hours. It is important you to have a spare, balloon tube (or a Foley Catheter, which also has a balloon) at home in case your tube comes out and you don’t have immediate access to an emergency room.
After three months you may choose to replace the PEG tube with the same type of tube or you may change to a balloon type gastrostomy tube. Talk with your nurse or doctor about the best tube for you. If the PEG tube is working well and does not need to be changed at 3 months, it may stay in for up to one year.
PEG tube rotation
You should regularly rotate your PEG tube, beginning a few days after initial placement. This makes sure the tissue and skin around the area haven’t stuck to the tube and will give you a good healthy stoma. It’s recommended that you rotate the PEG tube at least a quarter turn once a day. The best time is probably right after you bathe. If the tube feels tight and is difficult to turn, be sure not to force it. Make sure there is a little space in and out for the tube. If it’s too tight against the skin, slide the PEG-tube bumper up slightly. If your tube is held in place by a balloon, check to see if there is enough water in the balloon. It could be that the balloon has burst or eroded–this necessitates a tube change. If the feeding tube freely moves in and out and the balloon appears undamaged, try lubricating the stoma with a little water-based lubricant. If you don’t have lube, you could try using vegetable oil. Vaseline, or other petroleum-type lubricants, erode the plastic in the feeding tube over time so you should avoid using these. Once the PEG tube is lubricated, try rotating it again. Use as much gentle force as you’re comfortable with but note any pain or discomfort. Don’t panic if your tube won’t rotate. Stomas commonly get tight due to bloating, recent tube placement, or tube changes. However, if you’re unable to rotate your tube more than a few days, ask for medical advice.
PEG Tube Extension Sets
You will receive three types of extension sets. An extension set is a special tube that connects to the gastrostomy tube and allows formula, liquids and medicines to be given into the stomach. There is 1) a bolus set, 2) a right angle set and 3) a decompression tube. The bolus set is used for feedings given by gravity through a syringe. The right angle set is used for slow or continuous feedings given by a pump. The decompression tube (which has a long tip which opens a valve at the base of the tube) allows air and formula to be drained from the stomach, if needed. The decompression tube is used if you have too much gas (which can’t be burped up) or if you’re very uncomfortable and appears to have a bloated or full abdomen. The nurses taking care of you will show you how to attach and remove each extension tube.
PEG extension tubes must be the same size as the gastrostomy tube in order to fit. PEG tubes have two measurements, the diameter (width) measured in French (FR) size and the length measured in centimeters (CM). Catheters are also measured using this scale, where 1 Fr = .33mm. So, the bigger the French (Fr) number, the larger the diameter of your tube. Most adult PEG tubes run between 16 and 24 Fr.These numbers are printed on the inside flap of the PEG tube. The bolus set and the right angle set must be the same diameter (for example 14 Fr) as the PEG tube. The decompression tube must be the same diameter and the same length (for example 14 Fr and 1.7 cm) in order to fit. Doctors recommend that you write down the size of your PEG tube where you can find it when needed. This will help you when reordering supplies and talking with your doctors and nurses. Doctor’s office will also have a record of your PEG tube size.
How to check the water in your balloon
Your gastrostomy tube should have an access port for the balloon (the colored port on the tubes pictured at right). Insert a syringe into this port (the 60 cc syringe you use for feeding may have a special luer adapter for this purpose). Gently draw back on the syringe while making sure it is firmly attached to the port. Clear water should be drawn into the syringe–the same amount that was put into the balloon when placed. If the water is not clear, or there isn’t enough, or you’re not able to get any at all, then there is a problem with the balloon and you need to get your tube changed. If the water is fine, then you can slowly push it back into the balloon.
PEG Tube Care
To keep the PEG tube clean and unobstructed, you should flush the tube with clear water before and after feedings, or after medications have been administered through the tube. After the tube is placed, you should consult a registered dietitian or a nurse who specializes in nutrition to determine your nutritional needs, the amount of calories, protein, and fluids that will be necessary, as well as the most appropriate nutritional formula and how much of that formula will be needed each day. Nutritional products designed for tube feeding are formulated to provide all the nutrients you’ll require including proteins, carbohydrates, vitamins, and minerals. Some even contain dietary fiber and other non-nutritional elements. If you choose to blend food for your meals, you should consult your doctor or nutritionist to make sure you are meeting your nutritional needs.
When eating through a tube, it is imperative that you, or your caregiver thoroughly wash your hands with soap and water before preparing formula or having contact with the PEG system–much as you’ve always had to wash your hands before eating. The tube should be checked for patency, and the formula administered at room temperature. You should be upright, no less than thirty degrees, to minimize the risk of regurgitation and aspiration, and you should be kept upright for thirty to sixty minutes after feeding. In some cases, to prevent complications like abdominal cramping, nausea and vomiting, gastric distension, diarrhea, or aspiration, food should be infused slowly. It may take more than an hour to administer one feeding session, as the drip mechanism is kept at very slow settings. Sometimes continuous feeding is preferable. With this method, a feeding pump is set up and connected to the PEG tube. The formula is infused over a prescribed period of time into the patient. The risk for aspiration is decreased because less formula is given during a more prolonged period of infusion. Using an attached bag system to contain the liquid diet for feeding is a secondary method by which food is allowed to drip slowly into the tube though “gravity feeding.” With this technique, there is greater freedom in that feedings can be done anywhere, at any interval, and medications may be administered through the PEG tube utilizing this method. Under the drip-feeding method, feedings are usually performed every four to six hours. Clogging of tubes is regularly reported, especially in small-bore tubes. Tubes should be flushed with water before and after feeding during intermittent delivery, and every 4 to 8 hours during continuous feeding. This is done with a syringe full of water which is attached directly to the tube. Multiple flushings with the syringe will ensure a free flowing system. The patient may experience bloating either before or after feeding. If this occurs, the stomach and intestinal tract should be decompressed. Removing the adapter feeding cap from the tube and allowing the PEG to be open to air can easily accomplish this. Encouraging the patient to cough will also facilitate decompression.
The lifespan of the feeding tube is about six months. When the tubing begins to wear, it may pull away from the stomach wall and cause leakage near the insertion point. The replacement process is relatively simple, and usually does not involve another endoscopic procedure. Typically, the tubing is merely pulled out through the stomach site and then replaced with a new catheter.
Complications to this therapy may occur, but the likelihood is slight, with only a one percent chance of major problems (gastric hemorrhage, peristomal leakage) and an eight percent chance of minor ones (infection, stomal leaks, tube extrusion or migration, aspiration and fistula formation). Aspiration is perhaps the most common complication related to tube feeding. This occurs when food is actually inhaled into the lungs. Aspiration can lead to pneumonia, but if the patient is kept upright during feeding, the likelihood of developing this complication can be greatly minimized.
PEG tube clogs
The best way to deal with clogs in the feeding tube is to not get a clog in the first place. This is why it is always important to flush the tube with plenty of water before and after feeding. Also, make sure all medications are completely crushed. Tubies have frequent problems with reflux medicine like Prevacid or Nexium getting stuck in the tube. These meds are normally tiny balls packed in capsules and the balls often clump together in narrow passages like feeding tubes. The best way to take this type of medication is to suspend the tiny balls in something thicker than water. Applesauce works very well for this and can be pushed through the tube fairly easily. Another preventative measure for clogs is to make sure your food is well blended. Commercial formulas are designed to easily flow through feeding tubes, however blended meals need to be blended with a high-end blender, like a Vitamix or Blendtec, or strained before they are put into the tube.
If a clog does occur, there are simple steps you can take to try to clear out the obstruction. The first step is to pull the clog out. This may seem simple and obvious, yet when many tubies are confronted with a clog, their instinct is to just push harder to get the offending item in. This may just exacerbate the issue or lead to an explosive mess. The simplest solution is to take out your syringe, take a few deep breaths, push the plunger all the way into the syringe, reattach it to the feeding tube, and pull the plunger out to force the clog out the way it came.
Another way to clear clogs is to use warm water. Many tubies are firm believers in the idea that Coke, or other types of carbonated beverages, is the ideal way to remove a clog. In fact, there is no evidence that Coke is any more effective than water. While Coke has worked for some, it is just as likely that their clog would have been removed with time and water. Allowing the clog to soak in warm water gets it nice and wet and soft around the edges. The best way to do it is to load the syringe up with water, attach it to the tube and gently push it until it meets the clog. Next, lightly push and pull on the syringe and see if the clog moves at all. Be patient with the clog. After gently pushing and pulling with warm water around the clog, it should come lose and you can push it the rest of the way into your stomach. If the clog refuses to go in any further, but you can pull it out, make sure to draw it out completely into the syringe. Then you can clamp your tube, detach the syringe, and get rid of the clog.
Patience is key here. It could take 20 minutes to move the clog, but dealing with it at home is preferable to going to the ER. Just keep the warm water against the clog with a syringe and gently try pushing and pulling on it every few minutes. Eventually (hopefully) the clog will get mushy enough to move through the tube.
While Coke, or other carbonated drinks, have little or no effect on clogs, there are other liquids that may help break down the clog. Instead of warm water you can try meat tenderizer, papaya juice, mango juice, pineapple juice, or kiwi juice. There is also a product available online called Clog Zapper that is specifically made to unclog feeding tubes (one of the main ingredients is also found in meat tenderizer and papaya juice). All these will also take time (about 10-20 minutes) to work but the enzymes in these products should soften most clogs enough for you to clear them.
We hesitate to recommend this, but another possible way to get rid of clogs is to stick something down the tube. Be smart about this. Nothing unsanitary, or too long, or damaging to the tube. Actually, there are commercial tools called Enteral Feeding Tube DeCloggers that are designed to remove clogs, however they are for single-use only and are fairly expensive (around $25 for one). Other tubies have had success with knitting needles, bamboo skewers or pipe cleaners. Before using anything, be sure to measure the length of your feeding tube to prevent pushing the tool in too far.
If all else fails, then you should make a trip to the emergency room or contact your GI to get your feeding tube changed immediately.
Clogs are common for everyone who tube feeds, whether they blend their meals, or just eat formula. The most important thing, when dealing with a clog, is to have the right attitude. You’re not alone.
Feeding through a tube requires a catheter-tip syringe. This syringe has a tapered tip made for fitting into a catheter opening, extension set, or feed port (typical syringe with blue luer adapter pictured at right). There are also slip-tip syringes with a narrower tip offset from the barrel of the syringe. These could come in handy if you want to mix up your medications inside the syringe. A third type is the Luer-lock syringe. These syringes have a special tip designed to mate with a particular medicine port. The two sides lock together with a quarter-twist. Another example of a Luer-lock fitting is the button-end of the extension set.
Syringes need to be washed well after use (just like you’d wash your dishes after eating). The plunger on most syringes has a rubber tip. After repeated use, the rubber deteriorates and expands, making it much harder to push through the barrel. For this reason, syringes can’t really be used more than about a week before they need to be replaced. An alternative to the rubber-tipped plunger is the o-ring syringe. O-ring syringes (also known as ‘squirrel syringes’) have plungers with silicone o-rings on the end. They are a bit more expensive but can last much longer than other syringes. Many tubies have used the same o-ring syringe over a year–just washing after each use. These syringes are available from Real Food Blends or try asking your local veterinarian–they’re normally used to feed small animals.
Extension sets (used if you have a button) can be cared for much like syringes. They probably won’t get thoroughly cleaned in the dishwasher because it’s hard to flush water all the way through them. The best way to clean them is to run hot, soapy water–or just hot water–through them (you can push it through with a syringe), rinse them out, and air-dry. You can also soak them in a vinegar solution (50% vinegar and 50% water will do the trick) to kill most germs. Extension sets should last from one week to one month if they’re well cared for.
Feeding bags, used with pumps, are meant to be one-time-use only, but they can be washed and reused if necessary. As with syringes and extension sets, hand wash bags in hot, soapy water and/or soak them in a vinegar solution. Thorough cleaning is essential because formula has been sitting in the bag for a long period of time.
Flushing your PEG tube
Flush your PEG tube once a day or as directed by your doctor.
- Gather your supplies:
- 60 mL syringe, either one with catheter tip or an ENFit syringe
- 60 mL of water (room-temperature or warm, plain tap water) in a cup
- Paper towels
- Wash your hands with warm water and soap or use an alcohol based hand sanitizer.
- Draw up 60 mL of water into the syringe.
- Place the paper towels under the Y-port at the end of the tube to absorb any drainage.
- Clamp the tube.
- Insert the syringe into the Y-port of the PEG or PEJ tube.
- Unclamp the tube and gently push the plunger to inject the water.
- Re-clamp the tube.
- Remove the syringe from the Y-Port of the PEG or PEJ tube.
- You can reuse your syringe. Rinse it in warm water and dry it with clean paper towels after each time your flush your tube.
If you are having trouble flushing your tube, call your doctor or nurse.
Feeding Bag
PEG tube is very narrow, and commercial tube feeding formulas such as Ensure, are designed so that they will not clog the tube; they are not too thick and do not leave a residue. Most formulas are designed to have water added to them to ensure that the patient is receiving enough dietary water, and to further thin the formula for ease of use. To maintain patency, the patient should flush the tube with clear water before and after feedings, or after medications have been administered through the tube. The placement of noncommercial formulas or foods into the tube is highly discouraged, as there is a greater likelihood that they will contribute to clogging. After the tube is placed, a registered dietitian or a nurse who specializes in nutrition should assess the patient to determine their nutritional needs, the amount of calories, protein, and fluids that will be necessary, as well as the most appropriate nutritional formula and how much of that formula will be needed each day. Nutritional products designed for tube feeding are formulated to provide all the nutrients the patient will need including proteins, carbohydrates, vitamins, and minerals. Some even contain dietary fiber and other non-nutritional elements.
When feeding the patient, it is imperative that the caregiver or patient thoroughly washes their hands with soap and water before preparing formula or having contact with the PEG system. The tube should be checked for patency, and the formula administered at room temperature. The patient should be upright, no less than thirty degrees, to minimize the risk of regurgitation and aspiration, and they should be kept upright for thirty to sixty minutes after feeding. To prevent complications (abdominal cramping, nausea and vomiting, gastric distension, diarrhea, aspiration), food should be infused slowly. It may take more than an hour to administer one feeding session, as the drip mechanism is kept at very slow settings. Sometimes continuous feeding is preferable. With this method, a feeding pump is set up and connected to the PEG tube. The formula is infused over a prescribed period of time into the patient. The risk for aspiration is decreased because less formula is given during a more prolonged period of infusion. Using an attached bag system to contain the liquid diet for feeding is a secondary method by which food is allowed to drip slowly into the tube though “gravity feeding.” With this technique, there is greater freedom in that feedings can be done anywhere, at any interval, and medications may be administered through the PEG tube utilizing this method. Under the drip-feeding method, feedings are usually performed every four to six hours. Clogging of tubes is regularly reported, especially in small-bore tubes. Tubes should be flushed with water before and after feeding during intermittent delivery, and every 4 to 8 hours during continuous feeding. This is done with a syringe full of water which is attached directly to the tube. Multiple flushings with the syringe will ensure a free flowing system. The patient may experience bloating either before or after feeding. If this occurs, the stomach and intestinal tract should be decompressed. Removing the adapter feeding cap from the tube and allowing the PEG to be open to air can easily accomplish this. Encouraging the patient to cough will also facilitate decompression.
PEG Feeding Tube
Scrupulous oral care is imperative in preventing problems, and must be attended to frequently, especially in patients who are provided with total nutritional support through the PEG tube. Daily brushing of the patient’s teeth, gums and tongue must be performed. The patient’s lips should be routinely moistened, and if necessary, lubricated with petroleum jelly to prevent cracking. The incision area must be observed daily for redness, swelling, necrosis or purulent drainage, and the skin must also be cleaned daily. It helps to routinely apply an antibacterial ointment to the insertion site after cleaning to prevent infections such as Neosporin.
The lifespan of the feeding tube is about six months. When the tubing begins to wear, it may pull away from the stomach wall and cause leakage near the insertion point. The replacement process is relatively simple, and usually does not involve another endoscopic procedure. Typically, the tubing is merely pulled out through the stomach site and then replaced with a new catheter.
Complications to this therapy may occur, but the likelihood is slight, with only a one percent chance of major problems (gastric hemorrhage, peristomal leakage) and an eight percent chance of minor ones (infection, stomal leaks, tube extrusion or migration, aspiration and fistula formation). Aspiration is perhaps the most common complication related to tube feeding. This occurs when food is actually inhaled into the lungs. Aspiration can lead to pneumonia, but if the patient is kept upright during feeding, the likelihood of developing this complication can be greatly minimized.
For patients who are unable to chew and swallow food, tube feeding can safely and significantly increase the quality of life, maintaining appropriate weight levels and nutritional requirements.
General Feedings Guidelines
Give feedings and medications as directed by your nurse or doctor. Flush the gastrostomy tube with 60mL of warm water after every feeding or medication. This prevents clogging and keeps the tube as clean as possible. If you are giving continuous drip feeding into a PEG tube you may want to tape connections to prevent disconnection of the extension set from the tube and spillage of feedings. If you are using a balloon gastrostomy, such as an AMT mini-one tube, check the volume of water in the balloon every week and refill as necessary to maintain the amount of water prescribed by your child’s doctor or nurse (Do not perform this until at least 2 months after the tube was initially placed).
What should I do about the following problems?
Redness around the site
The skin may be slightly pink after initial insertion. You should see a decrease in this pink color over time. If the skin becomes tender, warm or red, call your child’s doctor or nurse.
Crusting
Drainage that dries on the skin is called crusting. Crusting and drainage is common around gastrostomy tubes. You can remove crusting and drainage with warm water.
Bleeding
If PEG tube gets bumped, or is rubbed, there may be a small amount of bleeding from around the tube. Apply pressure should stop the bleeding for up to ten minutes. If the bleeding does not stop, call your doctor or nurse. Blood coming through the tube is not normal. If this happens call your doctor or go to the nearest emergency room.
Granulation Tissue
Granulation tissue appears in most people at some time after the gastrostomy tube is placed. Granulomas are very common and are small areas of over granulation tissue that appear as fleshy protuberances like tiny beads of varying sizes. This tissue is common and not dangerous. On the other hand, if you see unnaturally swollen, red, lumpy, moist tissue or flesh around the stoma site, then it is most likely what’s known as hypergranulation tissue. This tissue could also exude yellow, sticky pus. It may be painful, bleed easy, and prevent your stoma from healing the way it should. Hypergranulation can occur for no apparent reason (friction, moisture or irritation may be contributing factors), especially during the first three months after the tube has been placed.
There are different methods for dealing with hypergranulation tissue. Initially, you should keep the site clean and dry in the hope that it will heal by itself. If this doesn’t work, silver nitrate may be an option. Silver nitrate is a caustic substance that burns the offending tissue. It will turn black as a result, scab up and eventually fall off. Note: you should spread petroleum jelly around the stoma before administering silver nitrate because it is extremely painful when it touches the skin. Other ointments have also proven to be effective at getting rid of hypergranulation. Creams intended for ear infections or skin issues (such as Kenacomb) may heal the site. Some G-tube patients report that 4-5 administrations of Kenacomb per day for five days clears up their hypergranulation. As a last resort, some doctors could choose to surgically remove the hypergranulation tissue. Wound care is extremely important after such a procedure to avoid infection or a reoccurrence.
Fever
If you have a fever, call your surgeon.
Vomiting and/or diarrhea
If you are having vomiting and/or diarrhea, call your surgeon or doctor for advice.
PEG tube replacement
Your doctor can easily remove or replace a PEG tube without sedatives or anesthesia, although your doctor might opt to use sedation and endoscopy in some cases. Your doctor will remove the PEG tube using firm traction and will either insert a new tube or let the opening close if no replacement is needed. PEG sites close quickly once the tube is removed, so accidental dislodgment requires immediate attention.
PEG tube removal
The majority of gastrostomy sites close spontaneously within 1–3 months 2, however, some of those that become chronic gastrocutaneous fistulae. Chronic gastrocutaneous fistulae are a difficult to manage complication following PEG tube removal, with an estimated incidence ranging from 4.5 to 45% 3, 4. Although complications related to the insertion of a PEG tube are well documented, complications following removal are not well described in the literature. The duration of gastrostomy use (>6 months duration) 5 and children <2 years of age 6 and resultant epithelialisation of the tract are critical factors in the development of chronic gastrocutaneous fistula, hence de-epithelialization may be important in treating refractory cases. It has been shown that epithelialization is a slow process and occurs at a rate of approximately 7 mm/day, over several weeks to months depending on the size of the wound and local conditions 7.
A study 3 identifies the following contributing factors for a persistent chronic gastrocutaneous fistula post-PEG tube removal:
- Younger patients less than 2 years of age
- Open Stamm gastrostomy technique
- Upsizing of PEG tube
- Change of a gastrostomy tube to a button
- Significant gastrostomy site infections
- Prolonged duration of PEG tube more than 2 years.
Based on the above findings, the authors 3 make the following recommendations to reduce the risk of developing a persistent GCF after removal of the PEG tube:
- Use of the percutaneous endoscopic technique, whenever feasible
- Use of the smallest size tube possible that meets patient requirements
- Avoid upsizing the PEG tube or changing the type of device unless absolutely necessary
- Antibiotic cover during the procedure and adequate and prompt treatment of gastrostomy site infections
- Remove PEG tube as soon as feasible and avoid tendency to keep it in place as a “safe measure” unless clinically indicated.
An increased incidence of chronic gastrocutaneous fistulae in younger children could be related to less subcutaneous tissue resulting in a shorter tract and early epithelialization. Chronic gastrocutaneous fistulae may respond to conservative measures to optimize healing including drugs such as proton pump inhibitors and somatostatin analogues to minimise gastric secretions, prokinetics to increase gastric emptying and postpyloric feeding 8. Defects that prove refractory to these measures and continue to discharge large volumes of gastric output can cause considerable morbidity to these patients, with recognized complications including cutaneous injury, risk of infection, dehydration, electrolyte disturbance and requirement for frequent dressings and stoma bags. Traditionally, prior to advances in gastrointestinal (GI) endoscopy, such patients would have ultimately required surgical closure via laparotomy with de-epithelialisation of the persistent gastrocutaneous fistula tract, gastric repair and fascial closure. However, given that many gastrostomy fed patients have multiple co-morbidities rendering them poor surgical candidates, the emergence of less-invasive endoscopic options has been an important development. Successful outcomes have been reported for persistent gastrocutaneous fistula with endoscopic clip closure 9 and endoscopically assisted suturing techniques 10. A combined approach to de-epithelialise the tract in addition to mechanical endoscopic closure has been advocated in the majority of published cases 10, thereby mimicking the surgical approach, with good results, albeit limited to small series and case reports. Given that endoscopic clip closure is less invasive than endoscopically assisted suturing, it is often the first-line approach. Whereas conventional endoscopic clips were limited in terms of the amount of persistent gastrocutaneous fistula tissue that can be entrapped and held, making the procedures technically difficult and cumbersome, over-the-scope clips with a ‘bear-claw’ design, which are now widely available, have been an advance and are felt to be superior in this regard 9. The Padlock clipis a novel over-the-scope clip that has been developed with a radial closure design to ensure greater ability to approximate and circumferentially entrap tissue for a more robust closure of perforations, surgical gastrostomies and fistulae 11. The Padlock clip has been shown to be effective for gastrostomy closure in preclinical animal model studies 12. Padlock clip for closure of a refractory gastrocutaneous fistula is easy to use in these circumstances, is less invasive than suturing approaches and could be considered as an alternative approach to this rare but troublesome complication of PEG tubes 11.
Figure 3. Padlock clip
PEG tube complications
There are risks and complications with this PEG tube procedure. They include but are not limited to the following.
Common risks and complications include:
- Nausea and vomiting.
- Faintness or dizziness, especially when you start to move around.
- Headache
- Pain, redness or bruising at the sedation injection (usually in the hand or arm).
- Muscle aches and pains.
- Allergy to medications given at time of the procedure.
- Failure of local anaesthetic. This may require a further injection of anaesthetic or a different method of anaesthetic to be used.
Uncommon risks and complications include:
- Infection at the stoma site. This will need antibiotics.
- Bleeding from the wound or with the abdomen.
- Damage to other organs within the abdomen during insertion of the PEG tube.
- Peritonitis from leakage of fluid from the stomach or from an infection
- Heart and lung problems such as heart attack or vomit in the lungs causing pneumonia. Emergency treatment may be necessary.
- Damage to your teeth or jaw due to the presence of instruments in your mouth.
- ‘Dead arm’ type feeling in any nerve, due to positioning with the procedure – usually temporary.
- An existing medical condition that you may have getting worse.
- The procedure may not be successful.
Rare risks and complications include:
- Bacteremia (infection of the blood). This will need antibiotics.
- Anaphylaxis (severe allergy) to medication given at the time of procedure.
- Death as a result of complications to this procedure is rare.
Notify the hospital or your surgeon straight away if you have:
- Chest pain or shortness of breath
- Severe abdominal (belly) pain, diarrhea, nausea, or vomiting
- A fever with temperature of 100.4° F (38° C) or higher
- Sharp chest or throat pain
- Have redness, tenderness or swelling for more than 48hours where you had the injection for sedation (either in the hand or arm).
- Any sign of redness, swelling, or pus around the tube
- Any dizziness or weakness
- Bleeding that doesn’t stop, such as bright red oozing from your insertion site
- Pain at your incision site that doesn’t get better with medication
- Trouble flushing your PEG or PEJ tube or button
- Drainage around your insertion site that soaks 5 or more gauze pads per day
If your PEG tube falls out contact the hospital straight away so that it can be replaced before your wound closes.
Nausea/Vomiting
Users are strongly advised to review with their healthcare provider, noting any differences in protocols/procedures, prior to taking any actions recommended here.
Symptoms:
- Nausea, vomiting
- Abdominal distress, distention, feeling bloated, cramping.
- Dry heaves/retching, cold sweat.
Immediate Action:
- Stop feeding.
- As per your doctor instruction, drain gastric contents through PEG-tube into a drainage bag/container or using a large syringe. If there is no return, flush with 10 cc water to make sure the tube is not blocked. Some tubes have valves (such as buttons) which make drainage difficult. If unable to vent button, call doctor.
- If vomiting persists, call doctor for appropriate intervention to avoid dehydration/fluid or electrolyte depletion.
Causes:
- Formula intolerance:
- High administration rate
- High formula concentration, allergy/intolerance of formula components
- Formula contaminated
- Mechanical problems:
- Tube displaced (Improper tube placement; tube migration)
- Patient improperly positioned feeding
- Side effect of medication or other treatments such as chemotherapy
- GI dysfunction:
- Poor gastric emptying, reflux, ulcer
- Bowel obstruction
- Constipation
- Psycho-social stressors:
- Anxiety concerning tube feeding procedure
- Offensive odors, sight and smell of food
- Coughing, post nasal drip, upper respiratory infection, sore throat
- Intolerance to oral diet (i.e. High sugar, lactose content)
Prevention:
- When feeding, build up rate and volume slowly. If nauseas develops, decrease rate of the home enteral nutrition (HEN) feeding until nausea subsides; gradually increase rate, then volume to previous level as tolerated, as per doctor instruction.
- Discuss with doctor the possibility of switching formulas
- Use good hand washing and clean technique when handling home enteral nutrition (HEN) formula/equipment. Wash all equipment with hot water after each use. It is generally recommended to use 1 bag for feedings within a 24 to 48 hour period. Before reusing, thoroughly clean bags with warm water and place in a clean container in fridge to retard bacterial growth. Do not store or wash equipment in the bathroom. Check expiration date of formula. Inspect can for bulging/evidence of contamination before opening. Cover and store any open formula in refrigerator and discard after 24 hours. Maximum hang time for formula at room temp. is 8 to 12 hours. If possible hand cold formula to slow bacterial growth.
- Examine tube for possible migration or dislodgment.
- Elevate head of bed or sit up with feedings. Position self onto right side after feedings.
- When starting new medications, check with doctor if nausea/vomiting is a possible side effect. If doctor prescribes anti-emetics, take at least 30-60 minutes prior to PEG feedings.
- Take dysmotility/antireflux/ulcer medications as prescribed.
- If bowel obstruction is suspected, seek medical attention.
- Constipation
- Use stress reduction/relaxation techniques/antianxiety medication prior to PEG feedings. Seek out support/encouragement.
- Remove offensive sights/smells (bedpan/commode/smell of cooking/food aversion)
- Notify doctor of persistent cough/nasal drip/infection/sore throat for evaluation.
- Review oral diet with a dietician to see if it contains elements that lead to nausea/vomiting. *Early morning nausea/vomiting can be common when first starting tube feeds as the body adjusts to feeding overnight and walking with a “full stomach”
Diarrhea
Symptoms
*Abdominal pain or cramping with frequent loose watery stool (color may vary)
Immediate Action:
- Decrease volume/administration rate of PEG formula.
- Call doctor if diarrhea is excessive (a noticeable increase in watery bowel movements for 24+ hours) to avoid fluid/electrolyte depletion
- Call doctor immediately if there is evidence of bleeding or if you are experiencing severe abdominal pain.
Causes:
- Formula intolerance:
- High administration rate
- High formula concentration, allergy/intolerance of formula components
- Formula contaminated
- GI Dysfunction:
- Short bowel syndrome
- Gastric Intestinal Colonization
- Bowel inflammation
- Advance side effects of medications, especially antibiotics
- Intolerance to oral diet (i.e. high sugar, lactose content)\
Prevention:
- Use appropriate feeding method (bolus, gravity or pump). Build up feeding rate and volume slowly until you reach prescribed rate. If diarrhea develops, decrease rate of home enteral nutrition (HEN) feeding until diarrhea subsides; gradually increase rate, then volume to previous level as tolerated, as per doctor instruction.
- Discuss with doctor the possibility of switching formula (such as to one with fiber), and the possible need for pancreatic enzyme replacement or lactase enzyme.
- Use clean technique when handling and storing PEG formula/equipment.
- Discuss with doctor the possible use of H2 blockers or bowel slowing medication.
- Report to doctor any recent course of antibiotics. A stool culture may be needed.
- C. Seek doctor input to controlling bowel inflammation.
- Evaluate prescribed medications with pharmacist for possible sorbitol, magnesium, or phosphorus content. Take proper amount of medication as prescribed. Inform doctor of any over the counter medications, herbals or supplements you may be taking.
- Review oral diet (if any) with dietician to see if it contains elements that lead to diarrhea (i.e. sugar, fat or lactose).
PEG Tube Obstruction/Blockage
Symptoms:
- Inability to flush with water, infuse tube feeding or administer medication.
- Bulging of tube when feeding bolus.
Immediate Action:
- Make sure tube clamp is open.
- Do not force feeding or medication into clogged tube.
- Try to flush tube with large syringe (60 ml if possible) filled with warm water. Pull plunger back on syringe; try flushing again with warm water. If flushing doesn’t work, call doctor re: trying Viokase (see below). Viokase may not be as effective with a PEJ tube.
Causes:
- Improper administration of medications or other non-formula additions with feeding. Medications not adequately crushed and dissolved before put into tube.
- Inadequate flushing of tube.
- Tube clamp is closed.
- Defective tubing (such as valves leaking with buttons)
- Infusion rate too low.
Prevention:
- Consult with pharmacist/doctor/nurse regarding proper administration of medications. (Medications like Prevacid may require special attention.) When possible use liquid medications and dilute in 30 cc water; otherwise dissolve crushed or powder medications in 30 cc water. Administer each medication separately from food, flushing before and after with water: ask doctor for appropriate volume to keep tube unclogged and meet your hydration needs. Never mix meds with formula.
- Flush tube with water (ask doctor for appropriate volume to keep tube unclogged and meet your hydration needs) after each feeding tube. Flush tube at least once a day if not in use.
- Open clamp when flushing, feeding or administering medications.
- Discuss tube replacement with doctor.
- Evaluate feeding rate and regimen with doctor. Flush tube with water (ask doctor for appropriate volume to keep tube unclogged and meet your hydration needs) every 6-8 hours with continuous feeds.
Suggested Protocol for Administering Viokase FOR DOCTOR USE ONLY:
Withdraw any enteral nutrition formula or medication from tube. Attempt to flush tube with warm water. If unable to flush:
- Write order to obtain one Viokase tab and one 300 mg sodium bicarbonate tablet for PEG tube unclogging.
- Crush Viokase tab and place in 15 ml warm water to dispense.
- Crush bicarbonate tablet and add to Viokase/water mixture.
- Instill water/Viokase/sodium bicarbonate mixture into tube.
- Allow to remain in tube for 30 minutes.
- Flush tube with 30 ml warm water.
- If tube is still clogged, consider repeating once.
- Sometimes carbonated beverages, can by syringed into the tube and are effective for unclogging it.
PEG Tube Displacement
Symptoms:
- Tube out of body or otherwise obviously dislodged/displaced.
- Choking/difficulty breathing.
- Nausea/vomiting abdominal pain
Immediate Action:
- Discontinue feeding.
- Do not remove percutaneously placed PEG/PEJ tube without doctor instruction: if one of these tubes falls out, reinsert if possible so the tract doesn’t close, and call doctor.
- Contact doctor for instructions.
Causes:
- Tube not adequately secured.
- Accidental or excessive pulling of tube. Tubes with gastric balloon may be treated by the stomach as a piece of food and be pulled into the small bowel.
- With PEG tube, persistent vomiting.
- Balloon deflates/bursts.
Prevention:
- Check external length of tube before each feeding. Mark feeding tube 1” from where it enters the body (so you can tell later if it’s moved). Use a tube attachment device (catheter/tube holder) or careful taping of external tube to nose/cheek/abdomen/clothing to avoid pulling or migration. Specially-designed under garments that helps secure tubes can be purchased for active consumers.
- See Complication “Nausea/Vomiting”
- Be sure balloon is intact (you should be able to aspirate a few cc’s of water or air). If balloon has burst, wash tube, reinsert, secure position with tape, and call doctor. If balloon is intact, deflate balloon, wash, reinsert and re-inflate. Report to doctor if problem persists.
Skin/Site Irritation and/or PEG Tube Leaking
Symptoms:
- Irritated skin, rash around tube; burning pain; foul odor; local infection.
- Leakage from the feeding tube itself (hole in tube, malfunctioning anit-reflux valve or cap) or from around the feeding tube.
- Need to change dressing more than once a day.
Immediate Action:
- If possible, clamp tube above defect.
- Stop feeding.
- Wash skin; apply day dressing.
- Call doctor.
Causes:
- Poorly fitting tube. (Tube is too small for tube tract, stem of button is too long or internal bumper is not snug against anterior stomach wall.)
- Tube tugging at exit site. (Excessive movement or tension at exit site causing enlargement of tube tract/irritation/ulceration.)
- Mechanical tube problem:
- Defective or deteriorated tubing or cap; or defective or clogged anit-reflux valve.
- Repeated clamping at the same site, accidental cutting of the tube.
Prevention:
- Discuss with doctor/nurse tube sizing, tips to keep tube fitting snuggly to avoid skin infection. Check tube for possible migration (see “Tube Displacement-Prevention”). Consult a doctor/nurse re: skin care. The nurse/doctor may apply/prescribe a steroid crème or silver nitrate if granulation tissue is a problem.
- Secure tube as directed with tape or tube holder (see “Tube Displacement-Prevention”).
- Discuss regarding tube/cap/button replacement with doctor. Move clamp to a different site daily. Avoid using scissors or sharp objects near tube.
Aspiration
Symptoms:
- Vomiting, heartburn
- Coughing or choking with difficulty breathing; chest pain
- Possible fever, shortness of breath, indicating pneumonia
Immediate Action:
- Stop feeding.
- As per doctor instruction, drain gastric contents through G-tube into a drainage bag/container or by a large syringe, if possible. Some tubes have valves (such as buttons) which make drainage difficult. If unable to vent button, call doctor.
- Call doctor for appropriate intervention.
Causes:
- Diminished gag reflex, gastro esophageal reflux (GER), swallowing disorder.
- Delayed gastric emptying
- Tube migration
More likely to occur in patients who are tube fed into their stomach (vs. small intestine)
Prevention:
- Put head of the bed on 6” blocks for night time feedings. Feeding while sitting up or using wedge pillows increases abdominal pressure and can aggravate gastro esophageal reflux.
- Position self on right side after feedings. Take medication for dysmotility as prescribed by doctor. Do not feed if stomach feels full or distended or if individual is vomiting.
- Anchor tube with tube holder/tape to avoid pulling or dislodging. Check tube for possible migration before feeding (See complication “Tube Displacement-Prevention”).
Constipation
Symptoms:
- Infrequent hard stool, stool impaction. (Liquid stool may leak around impacted stool.)
- Abdominal bloating, cramping/pain.
Immediate Action:
- Increase fluid intake, use stool softener or laxative as per doctor instruction.
- Call doctor if no bowel movement in several days and/or are experiencing vomiting, or severe abdominal distention or cramping.
Causes:
- Inadequate fluid or fiber intake
- Side effect of medications (i.e. narcotics, high dose calcium or antacids containing calcium)
- Inactivity
- Gastrointestinal dysmotility
- Bowel obstruction
Prevention:
- Discuss prophylactic bowel regimen with doctor/nurse (i.e. increasing fluid and fiber intake, and/or use of a stool softener of laxative).
- Discuss medications and possible side effects with doctor.
- Maintain regular exercise program, if able.
- Take medication for dysmotility as prescribed by doctor.
- Call doctor if you suspect bowel obstruction.
GI Bleeding
Symptoms:
- Bright red blood on outside of stool or per rectum
- Black, tarry stool or diarrhea
- Black/brown blood in vomit (looks like coffee grounds)
- Vomiting bright red blood
- Bright red blood coming from and/or around tube
Immediate Action:
Discuss all GI bleeding with doctor. If large amounts of blood are visible, seek treatment immediately.
Cause:
- Bright red blood on outside of stool or per rectum is likely caused by irritated hemorrhoids, fissure or an anal tear commonly linked to excessive diarrhea or constipation.
- Black, tarry stool or diarrhea; black/brown blood in vomit; or > 1 tablespoon bright red blood in vomit likely indicates upper GI bleeding.
- Vomiting small amounts (< 1 tablespoon) bright red blood when associated with frequent vomiting is likely caused by burst blood vessel in throat.
- Bright red blood coming from tube or around the tube may be caused by:
- Gastric ulcer/irritation
- Erosion of stomach lining from excessive tube movement.
- External granulation tissue.
Prevention:
- Reduce diarrhea (see complication “Diarrhea”) or avoid constipation ( see complication “Constipation”). Discuss symptoms with doctor.
- Discuss with doctor use of medications that block acid production.
- Reduce vomiting (see Complication #1 “Nausea/Vomiting”). Discuss symptoms with doctor.
- Discuss with doctor use of medications that block acid production.
- Secure tube as directed with tape or tube holder (see “Tube Displacement-Prevention”).
- Discuss granulation tissue with doctor/nurse. (May be related to tube leakage and/or improper skin care. See complication “Skin/Site Irritation.”)
Pump Power Failure
Symptoms:
- Unable to start pump.
- Repeated alarms without obvious cause.
Immediate Action:
- Check to see if pump is plugged into wall and that wall socket is functioning or check that battery is charged.
- Stop pump. Consult pump user manual “trouble shooting” section for possible cause. Call home care company for replacement.
- If pump will not work and replacement pump is not available, convert to gravity drip and administer at same or lower rate. If tube is located at the jejunum, flow should not exceed a constant drip to avoid dumping syndrome.
Causes:
- Power failure/low battery. Pump not plugged into wall outlet.
- Pump malfunction.
Prevention:
- Check electrical outlet. Notify local power company of durable medical equipment at home for emergency power outages. Keep pump plugged into electrical source whenever possible, even when infusing, if not ambulating to converse battery charge.
- Follow manufacturer/home care company recommendation for routine service/maintenance.
Rare Complications
Hyperglycemia
- Symptoms: Nausea, weakness, excessive thirst or hunger, headache, anxiety, nightmares, frequent urination; Glucose levels greater than ½% (or other level set by your doctor).
- Action: Call your doctor immediately for specific instructions.
- Causes: Diabetes body under a lot stress (due to illness, medications, steroids etc.)
- Prevention: Discuss diabetes management with doctor. Maintain prescribed volume and rate of home enteral nutrition (HEN) feedings.
Hypoglycemia
- Symptoms: Shaking, nausea, pale facial color, heart palpitations, sweating, anxiety, dizziness, blurred vision, weakness, fatigue, headache, blood sugar below 50-60 mg/dl.
- Action: Instill 2-4 ounces of orange juice, regular soda pop, or sugar water (1 tablespoon sugar to 4 ounces water) through feeding tube. (If you are unable to swallow, and if not contraindicated, place hard candy or cake decorating gel under tongue, or let 1-2 teaspoons of sugar dissolve in mouth. ) Then call your doctor immediately for specific instructions.
- Causes: Diabetes; body under a lot stress (due to illness, medications, steroids etc.)
- Prevention: Discuss diabetes management with doctor. Maintain prescribed volume and rate of PEG feedings.
Fluid or Electrolyte Imbalances
- Symptoms: Rapid weight loss or weight gain; thirst, weakness; edema, shortness of breath; shakiness; fine tremors; muscle cramping; numbness; tingling of hands or around mouth; palpitations; fatigue; taste changes; skin changes; loss of coordination
- Causes: Increased losses from vomiting, diarrhea, fistulae/ostomy output, urine output. Decreased urine output.
- Action: If you suspect a fluid overloaded or are extremely short of breath, stop PEG feedings and notify your doctor immediately. Call doctor regarding signs and symptoms and describe any change in weight, fluid intake or urine/stool output. doctor may recommend taking more or less fluid via feeding tube.
- Prevention: Take complete volume of PEG formula and fluids as ordered by doctor. Discuss with doctor indications for taking more or less fluid. Keep daily log of fluid intake, weight and urine/stool output — noting any significant fluctuations.
Hypoglycemia
- Symptoms: Shaking, nausea, pale facial color, heart palpitations, sweating, anxiety, dizziness, blurred vision, weakness, fatigue, headache, blood sugar below 50-60 mg/dl.
- Action: Instill 2-4 ounces of orange juice, regular soda pop, or sugar water (1 tablespoon sugar to 4 ounces water) through feeding tube. (If you are unable to swallow, and if not contraindicated, place hard candy or cake decorating gel under tongue, or let 1-2 teaspoons of sugar dissolve in mouth.) Then call doctor immediately for specific instructions.
- Causes: Diabetes, Stopping a feeding suddenly for patients on insulin.
- Prevention: Discuss diabetes management with doctor. Maintain prescribed volume and rate of PEG feedings.
- Chapter 98: Endoscopic Placement of Feeding Tubes. https://accessmedicine.mhmedical.com/content.aspx?bookid=1944§ionid=143522716
- El-Rifai N, Michaud L, Mention K et al. Persistence of gastrocutaneous fistula after removal of gastrostomy tubes in children: prevalence and associated factors. Endoscopy 2004;36:700–4. https://www.ncbi.nlm.nih.gov/pubmed/15280975
- Alshafei A, Deacy D, Antao B. Risk Factors for a Persistent Gastrocutaneous Fistula Following Gastrostomy Device Removal: A Tertiary Center Experience. Journal of Indian Association of Pediatric Surgeons. 2017;22(4):220-225. doi:10.4103/jiaps.JIAPS_205_16. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5615896/
- Bratu I, Bharmal A. Incidence and predictors of gastrocutaneous fistula in the pediatric patient. ISRN Gastroenterol 2011;2011:686803 doi:10.5402/2011/686803 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3168482/
- Papavramidis TS, Mantzoukis K, Michalopoulos N. Confronting gastrocutaneous fistulas. Ann Gastroenterol 2011;24:16–19. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3959466/
- Gastrostomies: evolution, techniques, indications, and complications. Gauderer MW, Stellato TA. Curr Probl Surg. 1986 Sep; 23(9):657-719. https://www.ncbi.nlm.nih.gov/pubmed/3095034/
- Almeleh R. Spontaneous accelerated epithelialization in deep dermal burns using an oxygen-delivering hydrogel: A report of two cases. Wounds. 2013;25:E18–25.
- Vasant DH, Lal S, Blackett BD et al. Closure of a large high-output gastrocutaneous fistula with combined postpyloric feeding and aggressive medical therapy. BMJ Case Rep 2012;2012:pii: bcr2012007267 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4544481/
- Kothari TH, Haber G, Sonpal N et al. The over-the-scope clip system—a novel technique for gastrocutaneous fistula closure: the first North American experience. Can J Gastroenterol 2012;26:193–5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3354887/
- Vasant DH, Abraham A, Paine PA. Endoscopically assisted suturing of a persistent gastrocutaneous fistula by using a site closure device. Gastrointest Endosc 2013;78:553–4. doi:10.1016/j.gie.2013.04.001 https://www.ncbi.nlm.nih.gov/pubmed/23948202
- Abraham A, Vasant DH, McLaughlin J, Paine PA. Endoscopic closure of a refractory gastrocutaneous fistula using a novel over-the-scope Padlock clip following de-epithelialisation of the fistula tract. BMJ Case Reports. 2015;2015:bcr2015211242. doi:10.1136/bcr-2015-211242. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4593293/
- Desilets DJ, Romanelli JR, Earle DB et al. Gastrotomy closure with the lock-it system and the Padlock-G clip: a survival study in a porcine model. J Laparoendosc Adv Surg Tech A 2010;20:671–6. doi:10.1089/lap.2010.0076