Phymatous rosacea
Phymatous rosacea also known as rhinophyma, is a stage of rosacea in which rosacea can thicken the skin on the nose, causing the nose to appear bulbous (rhinophyma), but phymatous rosacea may also occur in other locations 1. Rhinophyma predominantly affects male patients. The male-to-female ratio in patients with rhinophyma ranges from 5:1 to 30:1. This is possibly due to androgens (male hormones) 2. Other forms of rosacea may or may not be present 3. Occasionally, rhinophyma is preceded by acne.
Rhinophyma is a skin condition affecting the nose in which the skin is thickened and the sebaceous (oil) glands are enlarged. The skin appears skin colored or red and often has prominent blood vessels, which may be thin and red (telangiectasia) or larger and purplish in hue (venulectasia). The affected skin may be bulbous, pitted due to prominent pores (which may ooze sebum or contain a scaly plug), and scarred.
Typically, rhinophyma affects the tip of the nose, although the sides and skin on the top of the nose can also be involved. Rhinophyma can be cosmetically unsightly as skin thickening may result in irregular nodular growth and deformity of the nose.
Phymatous rosacea can also affect the following sites:
- Chin (gnathophyma)
- Ears (otophyma)
- Eyelids (blepharophyma)
- Forehead (metophyma).
Rhinophyma, along with other forms of phymatous rosacea, is graded on a clinical scale of severity from 1 to 3 3:
- Grade 1: prominent follicular openings with no skin thickening
- Grade 2: prominent follicular openings with mild skin thickening
- Grade 3: prominent follicular openings, skin thickening and overactive sebaceous glands and nodular nasal contour
Rosacea is a common, chronic inflammatory skin disease that affects primarily the central face (the cheeks, nose, chin, and forehead) that most often starts between the age of 30 and 60 years and is characterized by episodes of exacerbation and remission 4. It often begins as a tendency to flush and blush frequently. In time, persistent areas of redness appear on the cheeks and nose. The chin, forehead and neck can also be affected. Rosacea is common in those with fair skin, blue eyes and Celtic origins. Rosacea may be transient, recurrent or persistent and is characterized by its color, red. Women are more commonly affected than men 4. The prevalence of rosacea across populations has been reported to range from less than 1% to 22% 5.
Rosacea frequently presents as facial redness and there may be inflamed, red bumps and pimples (papules and pustules) on the cheeks, chin or forehead; tiny blood vessels may be visible on the cheeks and nose (telangiectasia), and recurrent flushing. Less commonly, it can lead to skin thickening due to hypertrophy of the sebaceous glands and fibrosis and swelling, particularly at the nose also called rhinophyma (bulbous nose) 6. The skin is often very sensitive and may feel dry, rough or swollen.
Involvement of the eyes (ocular rosacea) is estimated to occur in up to three quarters of patients with rosacea and frequently includes foreign-body sensation, dryness, burning, itching, redness, photophobia, tearing, and blurred vision 7. Sight-threatening
keratitis is rare.
The red, pimply facial rash can cause embarrassment, low self-esteem, and anxiety and may lead to feelings of depression and stigmatization, with a marked negative effect on quality of life 8.
Typically, rosacea is a multistage disease. The stages are the flushing stage, or transitory congestive redness; the erythrosis stage, of persistent telangiectatic redness; the papulopustular stage; and the phymatous stage.
Rosacea has been classified by the National Rosacea Society Expert Committee 9 into four subtypes:
- Erythematotelangiectatic
- Papulopustular
- Phymatous
- Ocular.
According to this classification, the presence of at least one of the following primary features in a central distribution on the face is diagnostic of rosacea: flushing (transient erythema), nontransient erythema, papules and pustules, and telangiectasia.
Secondary features, which can appear concurrently or independently, include a burning or stinging sensation, plaque, a dry appearance of the skin, edema, ocular manifestations, occurrence in a location other than the face, and phymatous changes 10. Given that rosacea often spans more than one subtype, that it can progress between subtypes, and that certain findings are pathognomonic (such as phymatous changes), the international Rosacea Consensus panel recently proposed a different classification strategy — one that is based on phenotype and that more adequately covers the diversity of clinical presentations. However, this strategy has not yet been widely adopted 11.
Rosacea key points
- Rosacea is a common, chronic facial skin disease that can have an adverse effect on quality of life; it affects more women than men.
- Rosacea diagnosis is made clinically, and management consists of education, the avoidance of triggers that can exacerbate the condition, skin care measures, and various treatment options.
- Erythema can be treated with topical brimonidine, topical oxymetazoline, laser therapy, or other lightbased therapies.
- For inflammatory lesions, first-line therapies include topical ivermectin, topical azelaic acid, or topical metronidazole. Treatment with modified-release oral doxycycline at a dose of 40 mg, oral tetracycline, or low-dose oral isotretinoin is recommended for moderate-to-severe inflammatory lesions and for inflamed phymas; fibrotic phymas can be treated with surgical therapies or ablative laser therapy.
- For ocular rosacea, eyelid hygiene and the use of artificial tears are recommended. More severe forms of ocular rosacea can be treated with cyclosporine eyedrops, fusidic acid gel or metronidazole gel applied to the eyelids, or oral doxycycline. Referral to an ophthalmologist may be warranted.
- Maintenance therapy is recommended, preferably with the use of a topical treatment.
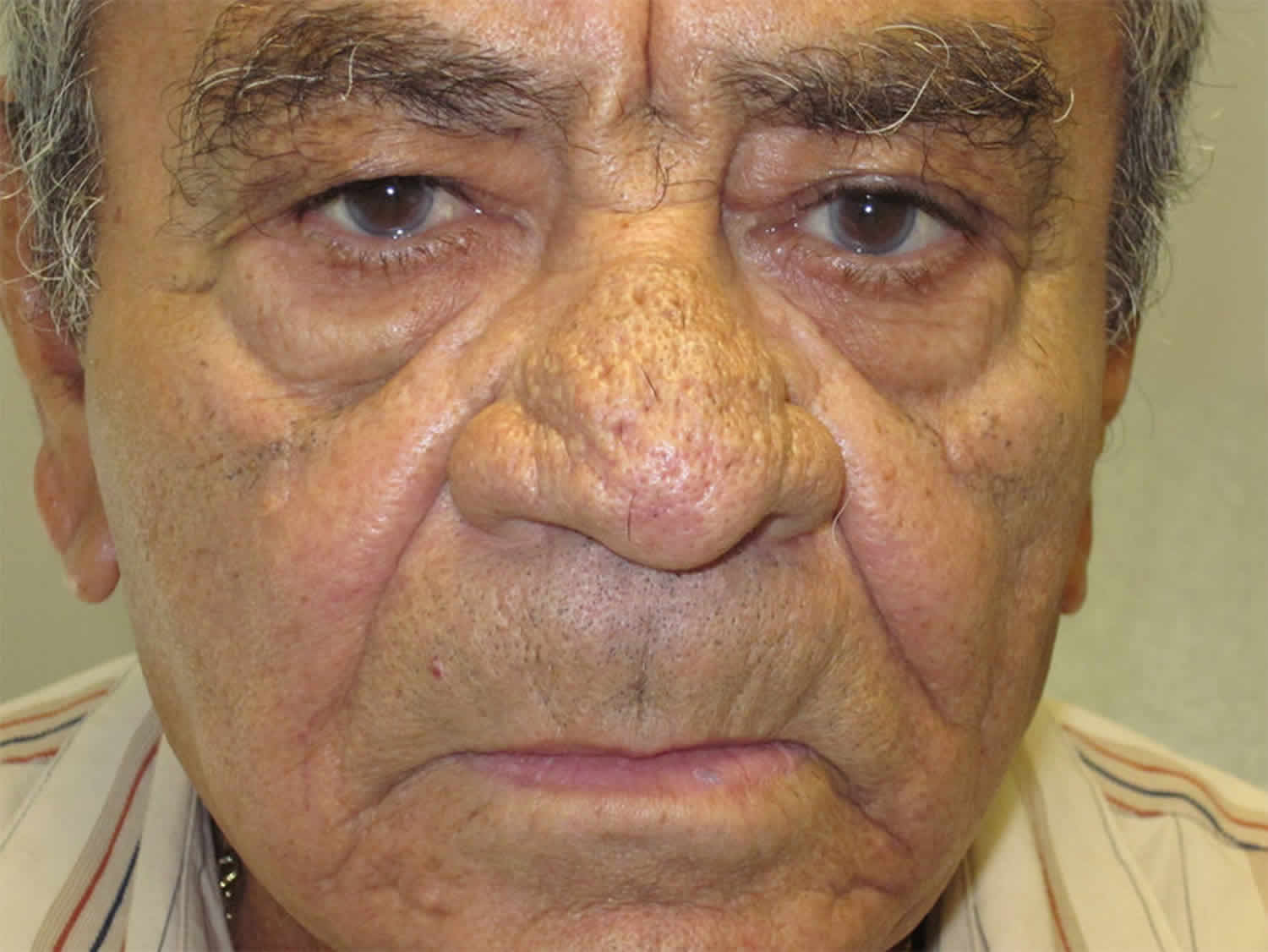
Figure 1. Phymatous rosacea
Footnote: Phymatous rosacea. Note: Thickened, glandular skin of the nose, creating a cosmetic deformity.
[Source 12 ]Papulopustular rosacea causes
The cause of rosacea remains uncertain. There are several theories regarding the cause of rosacea, including genetic, dysregulation of the innate and adaptive immune system, environmental, vascular, neuronal dysfunction, and inflammatory factors. Skin damage due to chronic exposure to ultraviolet radiation plays a part.
Rosacea is associated with impairment of the skin barrier, which results in excess transepidermal water loss, making the skin dry, prone to scaling and peeling, and sensitive to burning and stinging 13.
The skin’s innate immune response appears to be important, as high concentrations of antimicrobial peptides such as cathelicidins have been observed in rosacea 14.
- Cathelicidins are part of the skin’s normal defence against microbes.
- Cathelicidins promote infiltration of neutrophils in the dermis and dilation of blood vessels.
- Neutrophils release nitric acid also promoting vasodilation.
- Fluid leaks out of these dilated blood vessels causing swelling (oedema); and proinflammatory cytokines leak into the dermis, increasing the inflammation.
Matrix metalloproteinases such as collagenase and elastase also appear important in rosacea.
- These enzymes remodel normal tissue and help in wound healing and production of blood vessels (angiogenesis).
- In rosacea, they are in high concentration and may contribute to cutaneous inflammation and thickened, hardened skin.
- Matrix metalloproteinases may also activate cathelicidins contributing to inflammation.
Hair follicle mites (Demodex folliculorum) are sometimes observed within rosacea papules but their role is unclear.
An increased incidence of rosacea has been reported in those who carry the stomach bacterium Helicobacter pylori, but most dermatologists do not believe it to be the cause of rosacea.
Rosacea may be aggravated by facial creams or oils, and especially by topical steroids (steroid rosacea).
Triggers such as heat, stress, ultraviolet light, spicy food, hot beverages, smoking, and alcohol may exacerbate symptoms 15.
Phymatous rosacea signs and symptoms
Phymatous rosacea is characterized by thickened skin with irregular contours overlying the ears, cheeks, chin (gnathophyma), forehead (metophyma), and nose (rhinophyma).
Phymatous rosacea symptoms include changes in the nose, such as:
- Bulb-like (bulbous) shape
- Many oil glands
- Reddish color (possible)
- Thickening of the skin
- Waxy, yellow surface.
Phymatous rosacea can also affect the following sites:
- Chin (gnathophyma)
- Ears (otophyma)
- Eyelids (blepharophyma)
- Forehead (metophyma).
Rosacea results in red spots (papules) and sometimes pustules. They are dome-shaped rather than pointed and unlike acne, there are no blackheads, whiteheads or nodules. Rosacea may also result in red areas (erythematotelangiectatic rosacea), scaling (rosacea dermatitis) and swelling (phymatous rosacea).
Characteristics of rosacea 16:
- Frequent blushing or flushing
- A red face due to persistent redness and/or prominent blood vessels – telangiectasia (the first stage or erythematotelangiectatic rosacea)
- Red papules and pustules on the nose, forehead, cheeks and chin often follow (inflammatory or papulopustular rosacea); rarely, the trunk and upper limbs may also be affected
- Dry and flaky facial skin
- Aggravation by sun exposure and hot and spicy food or drink (anything that reddens the face)
- Sensitive skin: burning and stinging, especially in reaction to make-up, sunscreens and other facial creams
- Red, sore or gritty eyelid margins including papules and styes (posterior blepharitis), and sore or tired eyes (conjunctivitis, keratitis, episcleritis) – ocular rosacea
- Enlarged unshapely nose with prominent pores (sebaceous hyperplasia) and fibrous thickening – rhinophyma
- Firm swelling of other facial areas including the eyelids – blepharophyma
- Persistent redness and swelling or solid oedema of the upper face due to lymphatic obstruction – Morbihan disease
- Persistent yellow-brown papules and nodules due to granulomatous rosacea.
Phymatous rosacea possible complications
Basal cell carcinoma is a common form of skin cancer that has been reported to arise in rhinophyma. However, rhinophyma is not considered a precursor for malignancy 3.
Papulopustular rosacea diagnosis
In most cases, no investigations are required and the diagnosis of rosacea is made clinically. Occasionally a skin biopsy is performed only to rule out other diagnoses, since the histopathological features of rosacea are typically not specific to rosacea 17.
The Global Rosacea Consensus Panel recommends classification using diagnostic, major and minor phenotypes. One diagnostic or two major phenotypes are required for diagnosis.
Diagnostic phenotypes
- Fixed centrofacial erythema in a characteristic pattern that may periodically intensify
- Phymatous changes
Major phenotypes
- Papules and pustules
- Flushing
- Telangiectasia
- Ocular rosacea (lid margin telangiectases, interpalpebral conjunctival injection, spade-shaped infiltrates in cornea, scleritis, sclerokeratitis)
Minor phenotypes
- Burning or stinging
- Edema
- Dry appearance
Papulopustular rosacea treatment
Management of rosacea usually starts with educating patients about the skin condition and potential exacerbating factors to help patients identify triggers and improve their coping mechanisms 18. Although randomized trial data are lacking, clinical experience supports several general measures for skin care 18. Maintaining a diary is a useful means of identifying stimuli and triggers that can exacerbate rosacea (see below). Given the impairment of the skinbarrier function, irritant cosmetic products should be avoided. Ultraviolet light is a well-known trigger for rosacea; therefore, the daily use of sunscreens is recommended 13.
Inflamed phymatous rosacea
- Tretinoin (0.025% cream or 0.01% lotion): Once or twice daily for 8 to 12 weeks 19. Side effects include redness, dryness, itching, scaling and mild burning.
- Oral doxycycline 100 mg once daily for 8 to 12 weeks 19. Side effects include gastrointestinal discomfort, photosensitivity and candidiasis.
- Oral tetracycline 250 to 500 mg (tapering) twice daily for 8 to 12 weeks 19. Side effects include gastrointestinal discomfort, photosensitivity and candidiasis.
- Oral isotretinoin 0.25 to 0.30 mg per kilogram per day for 3 to 4 months 19. Side effects include cheilitis, dry mouth and lips, epistaxis, myalgia, increased triglyceride level, increased alanine aminotransferase level and birth defects.
The most effective medical treatment appears to be systemic isotretinoin, which can reduce the bulk of rhinophyma 20.
Noninflamed phymatous rosacea
Surgical interventions or ablative laser therapy: One or two treatments (electrosurgery, excision). Side effects include pain, crusts and scarring.
Techniques used to improve the cosmetic appearance of rhinophyma include:
- Dermaplaning (excision of thickened skin by shaving off the surface)
- Dermabrasion (scraping the surface skin)
- Cryotherapy (freezing)
- Laser resurfacing (CO2 , Argon, Nd:YAG, Er:YAG)
- Electrosurgery
General measures and skin care
- Keep a diary to identify stimuli and triggers that can exacerbate rosacea (e.g., cosmetics, weather conditions, exercise, drugs, spicy food, beverages, alcohol, and stress).
- Avoid the identified triggers.
- Daily use of sunscreens that protect against exposure to ultraviolet A and ultraviolet B radiation, have a sun protection factor of 30 or greater (SPF 30+), and preferably contain dimethicone, cyclomethicone, or both to mitigate facial irritation. Sunscreens containing zinc oxide or titanium are generally associated with few unacceptable side effects.
- Use of soap-free cleansers and non-oily moisturizers. Many moisturizers have been developed for the sensitive and easily irritated skin of patients with rosacea; sometimes these products contain green pigment to neutralize facial redness.
- Use of oil-free foundation and concealer when the use of these products is desired.
- Generally avoid the following skin care products:
- Waterproof make-up, which can be difficult to remove.
- Skin tonics, toners, and astringents (i.e., products that contain alcohol, menthol, peppermint, camphor, witch hazel, or eucalyptus oil).
- Cosmetics containing sodium lauryl sulphate, strong fragrances, fruit acids, or glycolic acids.
- Exfoliating scrub cream.
- Avoid oil-based facial creams. Use water-based make-up.
- Never apply a topical steroid to the rosacea as although short-term improvement may be observed (vasoconstriction and anti-inflammatory effect), it makes the rosacea more severe over the next weeks (possibly by increased production of nitric oxide).
- Keep your face cool to reduce flushing: minimise your exposure to hot or spicy foods, alcohol, hot showers and baths and warm rooms.
- Some people find they can reduce facial redness for short periods by holding an ice block in their mouth, between the gum and cheek.
Oral antibiotics for rosacea
Tetracycline antibiotics including doxycycline and minocycline are commonly used to treat rosacea:
- They reduce the redness, papules, pustules and eye symptoms.
- The antibiotics are usually prescribed for 6–12 weeks, with the duration and dose depending on the severity of the rosacea.
- Further courses are often needed from time to time, as antibiotics don’t cure the disorder.
Sometimes other oral antibiotics such as cotrimoxazole or metronidazole are prescribed for resistant cases.
Anti-inflammatory effects of antibiotics are under investigation.
- They have been shown to inhibit matrix metalloproteinases function and in turn reduce cathelicidins and inflammation.
- The effective dose of tetracyclines in rosacea is lower than that required to kill bacteria, so they are not working through their antimicrobial function.
Disadvantages of longterm antibiotics include development of bacterial resistance, so low doses that do not have antimicrobial effects are preferable (eg, 40–50 mg doxycycline daily).
Topical treatment of rosacea
- Metronidazole cream or gel can be used intermittently or long-term on its own for mild inflammatory rosacea and in combination with oral antibiotics for more severe cases.
- Azelaic acid cream or lotion is also effective for mild inflammatory rosacea, applied twice daily to affected areas.
- Brimonidine gel, an alpha-2 adrenergic agonist, and oxymetazoline hydrochloride cream, an alpha1A adrenoceptor agonist, reduce facial redness temporarily.
- Ivermectin cream can be used in the treatment of papulopustular rosacea. It controls demodex mites and is anti-inflammatory.
Isotretinoin
When antibiotics are ineffective or poorly tolerated, oral isotretinoin may be very effective. Although isotretinoin is often curative for acne, it may be needed in low dose long-term for rosacea, sometimes for years. It has important side effects and is not suitable for everyone.
Medications to reduce flushing
Nutraceuticals targeting flushing, facial redness and inflammation may be beneficial.
Certain medications such as clonidine (an alpha2-receptor agonist) and carvedilol (a non-selective beta blockers with some alpha-blocking activity) may reduce the vascular dilatation (widening of blood vessels) that results in flushing. They are generally well tolerated. Side effects may include low blood pressure, gastrointestinal symptoms, dry eyes, blurred vision and low heart rate.
Anti-inflammatory agents used for rosacea
Oral non-steroidal anti-inflammatory agents such as diclofenac may reduce the discomfort and redness of affected skin. Although these are uncommon, serious potential adverse effects to these agents include peptic ulceration, renal toxicity and hypersensitivity reactions.
Calcineurin inhibitors such as tacrolimus ointment and pimecrolimus cream are reported to help some patients with rosacea.
Vascular laser
Persistent telangiectasia can be successfully improved with vascular laser or intense pulsed light treatment. Where these are unavailable, cautery, diathermy (electrosurgery) or sclerotherapy (strong saline injections) may be helpful. Papulopustular rosacea may also improve with laser treatment or radiofrequency.
Phymatous rosacea prognosis
Rhinophyma can be corrected with surgery. The condition may return.
References- Rhinophyma Treated with Options Today. https://www.rosacea.org/rosacea-review/2012/spring/rhinophyma-treated-with-options-today
- Rohrich RJ, Griffin JR, Adams WP Jr. Rhinophyma: review and update. Plast Reconstr Surg. 2002;110(3):860–870. doi:10.1097/00006534-200209010-00023
- Chapter 7: Rosacea and Related Disorders. Bologna Dermatology 3rd Edition.
- Elewski BE, Draelos Z, Dréno B, Jansen T, Layton A, Picardo M. Rosacea — global diversity and optimized outcome: proposed international consensus from the Rosacea International Expert Group. J Eur Acad Dermatol Venereol 2011; 25:188-200.
- Tan J, Berg M. Rosacea: current state of epidemiology. J Am Acad Dermatol 2013; 69: Suppl 1: S27-S35.
- van Zuuren EJ, Fedorowicz Z, Carter B, van der Linden MM, Charland L. Interventions for rosacea. Cochrane Database Syst Rev 2015; 4: CD003262
- Vieira AC, Mannis MJ. Ocular rosacea: common and commonly missed. J Am Acad Dermatol 2013; 69: Suppl 1: S36-S41.
- Halioua B, Cribier B, Frey M, Tan J. Feelings of stigmatization in patients with rosacea. J Eur Acad Dermatol Venereol 2017; 31: 163-8.
- Standard grading system for rosacea: Report of the National Rosacea Society Expert Committee on the Classification and Staging of Rosacea. https://www.rosacea.org/physicians/grading-system-for-rosacea/view-online#toc16
- Wilkin J, Dahl M, Detmar M, et al. Standard classification of rosacea: report of the National Rosacea Society Expert Committee on the classification and staging of rosacea. J Am Acad Dermatol 2002; 46: 584-7.
- Tan J, Almeida LM, Bewley A, et al. Updating the diagnosis, classification and assessment of rosacea: recommendations from the global ROSacea COnsensus (ROSCO) panel. Br J Dermatol 2017; 176: 431-8.
- Emer, Jason & Weinkle, Allison & Doktor, Vladyslava. (2015). Update on the Management of Rosacea. Clinical, Cosmetic and Investigational Dermatology. 8. 159. 10.2147/CCID.S58940
- Two AM, Wu W, Gallo RL, Hata TR. Rosacea: part II. Topical and systemic therapies in the treatment of rosacea. J Am Acad Dermatol 2015; 72: 761-70.
- Rosacea. https://dermnetnz.org/topics/rosacea
- Picardo M, Eichenfield LF, Tan J. Acne and rosacea. Dermatol Ther (Heidelb) 2017; 7: Suppl 1: 43-52.
- Rosacea. https://dermnetnz.org/topics/rosacea/
- Two AM, Wu W, Gallo RL, Hata TR. Rosacea: part I. Introduction, categorization, histology, pathogenesis, and risk factors. J Am Acad Dermatol 2015; 72: 749-58.
- Schaller M, Almeida LM, Bewley A, et al. Rosacea treatment update: recommendations from the global ROSacea COnsensus (ROSCO) panel. Br J Dermatol 2017; 176: 465-71.
- Asai Y, Tan J, Baibergenova A, et al. Canadian clinical practice guidelines for rosacea. J Cutan Med Surg 2016; 20: 432-45.
- Chapter 43.9: Rhinophyma and other phymas. Rook’s Dermatology 8th Edition.