Polymicrogyria
Polymicrogyria is a condition characterized by abnormal development of the brain before birth. The surface of the brain normally has many ridges or folds, called gyri. In people with polymicrogyria, the brain develops too many folds, and the folds are unusually small. The name of polymicrogyria literally means too many (poly-) small (micro-) folds (-gyria) in the surface of the brain. Polymicrogyria, one of the most common brain malformations, accounts for approximately 20% of all malformations of cortical development 1.
Polymicrogyria can affect part of the brain or the whole brain. When the condition affects one side of the brain, researchers describe it as unilateral. When it affects both sides of the brain, it is described as bilateral. The signs and symptoms associated with polymicrogyria depend on how much of the brain, and which particular brain regions, are affected; however, affected people may experience recurrent seizures (epilepsy); delayed development; crossed eyes; problems with speech and swallowing; and muscle weakness or paralysis. Bilateral forms (affecting both sides of the brain) tend to cause more severe neurological problems. Polymicrogyria can result from both genetic and environmental causes. It may occur as an isolated finding or as part of a syndrome. Treatment is based on the signs and symptoms present in each person 2.
Researchers have identified multiple forms of polymicrogyria. The mildest form is known as unilateral focal polymicrogyria. This form of the condition affects a relatively small area on one side of the brain. It may cause minor neurological problems, such as mild seizures that can be easily controlled with medication. Some people with unilateral focal polymicrogyria do not have any problems associated with the condition.
Bilateral forms of polymicrogyria tend to cause more severe neurological problems. Signs and symptoms of these conditions can include recurrent seizures (epilepsy), delayed development, crossed eyes, problems with speech and swallowing, and muscle weakness or paralysis. The most severe form of the disorder, bilateral generalized polymicrogyria, affects the entire brain. This condition causes severe intellectual disability, problems with movement, and seizures that are difficult or impossible to control with medication.
Bilateral perisylvian polymicrogyria, the most common pattern of polymicrogyria, is associated with oromotor dysfunction and a seizure disorder. Other findings typically include difficulties with tongue movement, expressive speech, and sucking and swallowing, as well as excessive drooling and facial diplegia as seen in the Worster-Drought syndrome. Mild-moderate intellectual disability is seen in up to 75%. Motor dysfunction may include limb spasticity, which – if present – is rarely severe 3.
Polymicrogyria can result from both genetic and environmental causes. Polymicrogyria most often occurs as an isolated feature, although it can occur with other brain abnormalities. Polymicrogyria is also a feature of several genetic syndromes characterized by intellectual disability and multiple birth defects. These include 22q11.2 deletion syndrome, Adams-Oliver syndrome, Aicardi syndrome, Galloway-Mowat syndrome, Joubert syndrome, and Zellweger spectrum disorder.
The prevalence of isolated polymicrogyria is unknown 4. Researchers believe that it may be relatively common overall, although the individual forms of the disorder (such as bilateral generalized polymicrogyria) are probably rare.
Polymicrogyria treatment is based on the signs and symptoms present in each person 2.
Bilateral perisylvian polymicrogyria
Bilateral perisylvian polymicrogyria also called congenital bilateral perisylvian syndrome, is a rare neurological disorder that affects the cerebral cortex (the outer surface of the brain) 5. Bilateral perisylvian polymicrogyria is a subtype of a broader condition known as polymicrogyria. The cerebral cortex of the brain normally consists of several deep folds and grooves. In bilateral perisylvian polymicrogyria, the grooves that develop during embryonic growth form improperly on both sides of the brain near the Sylvian fissure, resulting in an increased number of folds that are unusually small 6. Signs and symptoms typically become apparent at birth, infancy, or later during childhood, and may include partial paralysis of the face, tongue, jaw, and throat; problems with speech and swallowing; excessive drooling; and seizures. Mild to severe intellectual disability often is also present. Some people with bilateral perisylvian polymicrogyria have other health problems or birth defects 2. Most cases of bilateral perisylvian polymicrogyria occur sporadically in people with no family history of bilateral perisylvian polymicrogyria. Rarely, more than one family member has bilateral perisylvian polymicrogyria, and the pattern of inheritance depends on the cause. Genetic causes may include mutations in single genes and contiguous gene disorders such as 22q11.2 deletion syndrome. bilateral perisylvian polymicrogyria has also been reported in association with twin pregnancy complications 7. The diagnosis of bilateral perisylvian polymicrogyria is based on the symptoms present and a thorough neurological evaluation including various imaging techniques. Treatment aims to address individual symptoms present in each person 2. For example, anti-seizure medications may help control seizures 6. The quality of life and life expectancy for people with bilateral perisylvian polymicrogyria are not well-described but may depend on severity of symptoms, whether complications develop, and whether other birth defects or an underlying syndrome are present 7.
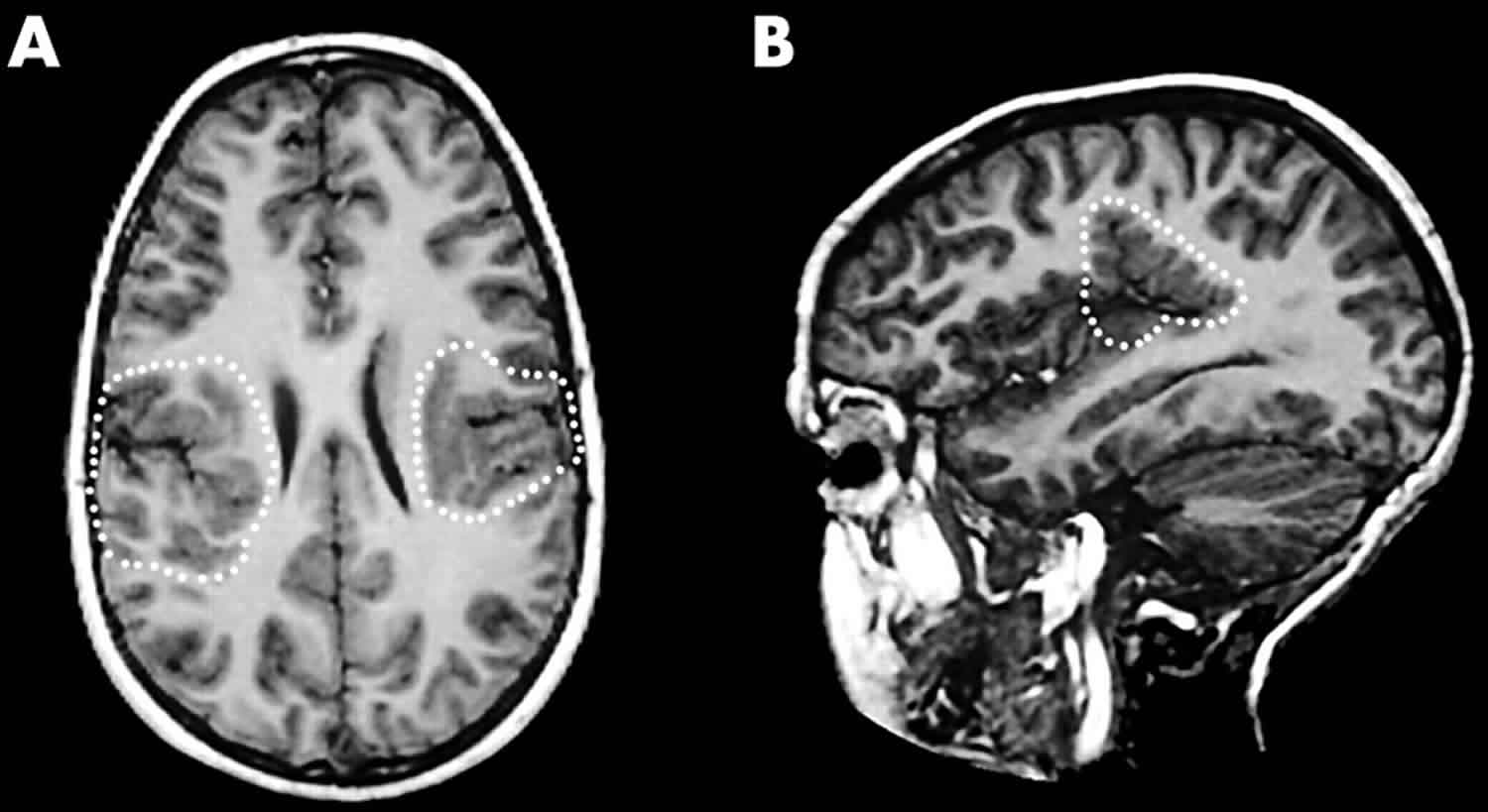
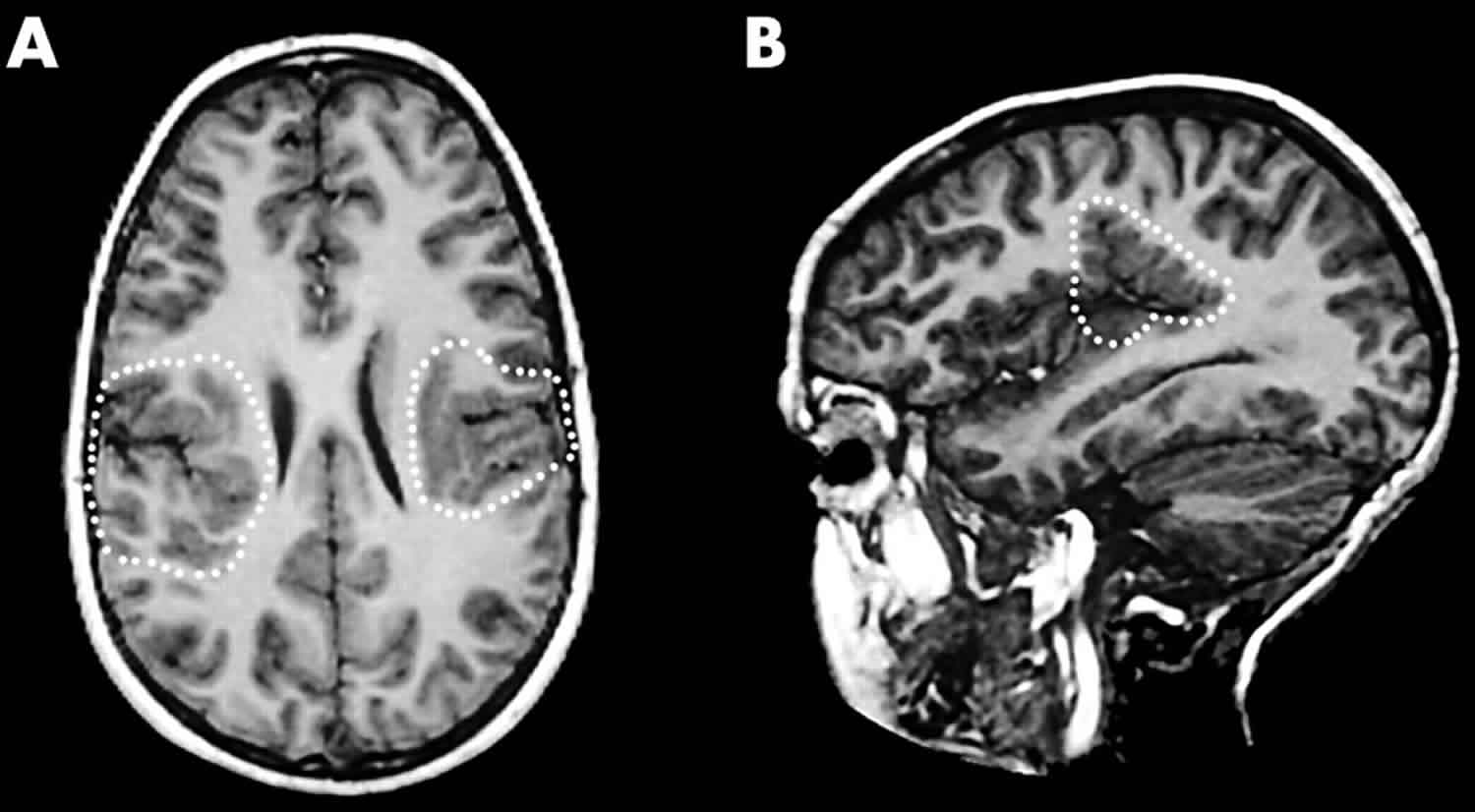
Figure 1. Bilateral perisylvian polymicrogyria
Footnote: Axial (A) and sagittal T1 weighted (B) magnetic resonance images showing bilateral perisylvian polymicrogyria. The axial slice displays bilateral inward folding of abnormal cortex in the posterior segments of the sylvian fissure bilaterally. The multiple small gyri are better demonstrated in the sagittal plane.
[Source 8 ]Bilateral perisylvian polymicrogyria causes
There are multiple possible causes of bilateral perisylvian polymicrogyria and the cause can vary from person to person. In some cases, the cause may not be known. Genetic causes may include a contiguous gene disorder (a disorder caused by the deletion of multiple adjacent genes) or a single gene disorder (a disorder caused by a mutation in one gene) 2. Bilateral perisylvian polymicrogyria may also have non-genetic causes. It has been reported in association with complications in twin pregnancies, including twin–twin transfusion syndrome and intrauterine death of a co‐twin. It has additionally been reported in association with amniotic band syndrome 9.
Contiguous gene disorders that have been associated with bilateral perisylvian polymicrogyria include 22q11.2 deletion syndrome and 1p36 deletion syndrome 2.
Single gene disorders that have been associated with bilateral perisylvian polymicrogyria include 2:
- MPPH syndrome – caused by a mutation in the AKT3, CCND2, or PIK3R2 genes
- Smith-Kingsmore syndrome – caused by a mutation in the MTOR gene
- MCAP syndrome – caused by mutations in the PIK3CA gene
- Lissencephaly – caused by a mutation in the TUBA1A gene
- Weaver syndrome – caused by a mutation in the EZH2 gene
Single genes in which mutations have been associated with bilateral perisylvian polymicrogyria (but not necessarily a defined disorder or syndrome) include the EOMES, NEDD4L, and ADGRG1 genes 10.
Inheritance pattern
In most cases, bilateral perisylvian polymicrogyria occurs sporadically in people with no family history of bilateral perisylvian polymicrogyria. Less commonly, bilateral perisylvian polymicrogyria is inherited, and more than one family member may have bilateral perisylvian polymicrogyria.[1] The inheritance in each of these cases depends on the underlying cause of bilateral perisylvian polymicrogyria and may be autosomal dominant, autosomal recessive, or X-linked.[4]
Bilateral perisylvian polymicrogyria symptoms
Signs and symptoms of bilateral perisylvian polymicrogyria usually are apparent at birth or become apparent during infancy or childhood. The signs and symptoms, and severity, vary from person to person but may include 2:
- Partial paralysis of muscles on both sides of the face, tongue, jaw, and throat
- Sudden, involuntary spasms of facial muscles
- Excessive drooling
- Difficulty with sucking, chewing, and/or swallowing (dysphagia)
- Difficulty with speech (dysarthria)
- Seizures
- Mild spasticity of the limbs (spastic tetraplegia)
- Developmental delay or learning impairments
- Mild to severe intellectual disability
- Contractures present from birth (congenital)
Various other health problems or birth defects may occur in people with bilateral perisylvian polymicrogyria, depending on whether an underlying genetic disorder with additional associated symptoms is present 11.
Bilateral perisylvian polymicrogyria diagnosis
A diagnosis of bilateral perisylvian polymicrogyria is typically based on a thorough physical examination, a detailed medical history, and a complete neurological evaluation, which may include tests such as 2:
- Magnetic resonance imaging (MRI) – a diagnosis of polymicrogyria is usually made by MRI because MRI typically can detect the small folds in the brain more effectively than other imaging techniques.
- Electroencephalography (EEG) – a test that measures electrical activity in the brain
- Computed tomography (CT) scanning
- Genetic testing – different types of genetic tests may be performed to determine if there is a genetic cause for the bilateral perisylvian polymicrogyria.
Bilateral perisylvian polymicrogyria treatment
The characteristics of the brain that define bilateral perisylvian polymicrogyria (bilateral perisylvian polymicrogyria) cannot be corrected, but there are treatments or therapies that aim to improve the signs and symptoms of bilateral perisylvian polymicrogyria. For example, anti-seizure medications may be prescribed to control seizures. People with bilateral perisylvian polymicrogyria may also benefit from physical therapy and/or speech therapy 6.
Bilateral frontoparietal polymicrogyria
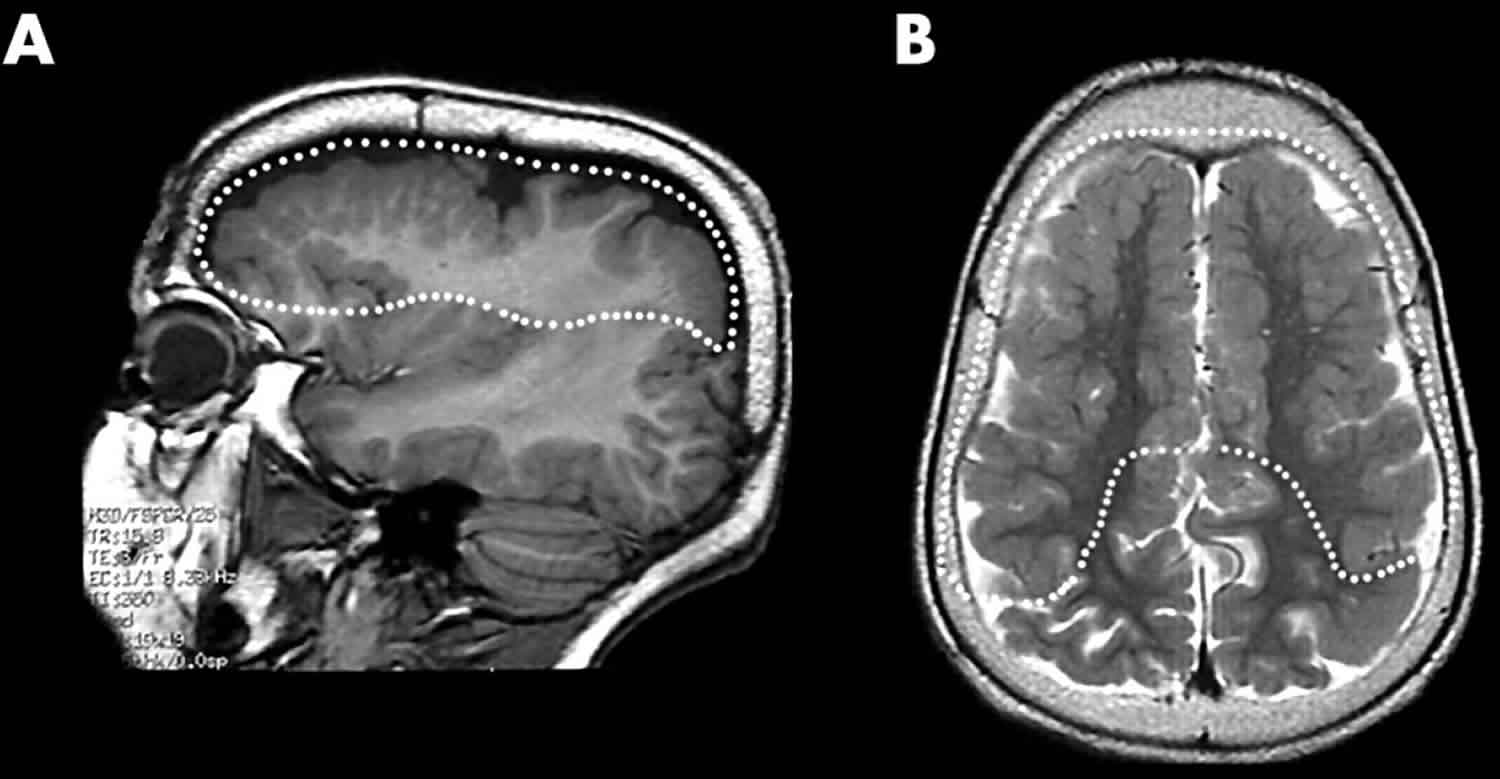
Bilateral frontoparietal polymicrogyria is a rare neurological disorder that affects the cerebral cortex (the outer surface of the brain). Bilateral frontoparietal polymicrogyria specifically affects the frontal and parietal lobes on both sides of the brain (bilateral). MRI in bilateral frontoparietal polymicrogyria patients shows bilateral white matter abnormalities and atrophy of the brain stem and cerebellum (Figure 2) 12. Signs and symptoms typically include moderate to severe intellectual disability, developmental delay, seizures, cerebellar ataxia, strabismus, and dysconjugate gaze (esotropia) (eyes that are not aligned). Seizures, which occur in 94% of patients and are mostly generalized seizures 12. Some cases are caused by mutations in the GPR56 gene and are inherited in an autosomal recessive manner. Treatment is based on the signs and symptoms present in each person 13.
Figure 2. Bilateral frontoparietal polymicrogyria
Footnote: Bilateral frontoparietal polymicrogyria. Sagittal T1 weighted (A) and axial T2 weighted (B) magnetic resonance images showing bilateral frontoparietal polymicrogyria. The sagittal image reveals thin white matter digitations within multiple small gyri of corrugated appearance in the frontal lobes, having a cauliflower-like aspect in the axial image. The posterior margins of abnormal cortex in the parietal lobes show cortical thickening, most probably reflecting histological heterogeneity with fusion of microsulci.
[Source 8 ]Bilateral frontoparietal polymicrogyria signs and symptoms
The signs and symptoms of bilateral frontoparietal polymicrogyria vary but may include 13:
- Moderate to severe intellectual disability
- Developmental delay
- Seizures
- Dysconjugate gaze (eyes that are not aligned)
- Ataxia
- Strabismus
- Increased muscle tone
- Finger dysmetria (difficulty controlling speed, distance and/or power of movements)
Polymicrogyria causes
In most people with polymicrogyria, the cause of the condition is unknown. However, researchers have identified several environmental and genetic factors that can be responsible for the disorder. Environmental causes of polymicrogyria include certain infections during pregnancy and a lack of oxygen to the fetus (intrauterine ischemia).
Researchers are investigating the genetic causes of polymicrogyria. The condition can result from deletions or rearrangements of genetic material from several different chromosomes.
Recent studies by experts have deemed the term “polymicrogyria” to refer to several different development disorders or birth defects of the brain that all have an irregular appearance of the brain surface in common. They have split “polymicrogyria” into different categories; classic polymicrogyria, Cobblestone Malformation, Tubulinopathy-associated dysgyria and other rare patterns. While all are rare, almost 50 genes have been associated with polymicrogyria or polymicrogyria-like malformations, which fall into several groups listed below:
- Polymicrogyria genes (all very rare) – PAX6, FOXP2, BICD2, EOMES (TBR2), WDR62, NDE1, CEP135, PI4KA
- Tubulinopathy genes – TUBA1A, TUBA8, TUBB2B, TUBB, TUBB3, DYNC1H1, KIF5C, KATNB1
- Warburg micro syndrome genes – RAB3GAP1, RAB3GAP2, RAB18, TBC1D20
- Cobblestone malformation genes with congenital muscular dystrophy plus – AG1, POMT1, POMT2, POMGnT1, FKTN, FKRP, LARGE, B3GALNT2, B3GNT1, GALNT2, GTDC2, ISPD, TMEM5
- Cobblestone malformation genes other – LAMA2, LAMB1, LAMC3, GPR56/ADGRG1, COL3A1, SRD5A3, ATP6V0A2, SNAP29
- Brain overgrowth and polymicrogyria genes – PIK3CA, PIK3R2, PTEN, AKT3, MTOR, CCND2
In addition, polymicrogyria has been seen with two relatively common chromosome deletion syndromes: deletion 1p36.3, also known as monosomy 1p36 and deletion 22q11.2, also known as DiGeorge syndrome.
Additionally, mutations in one gene, ADGRG1, have been found to cause a severe form of the condition called bilateral frontoparietal polymicrogyria. The ADGRG1 gene appears to be critical for the normal development of the outer layer of the brain. Researchers believe that many other genes are probably involved in the different forms of polymicrogyria.
Polymicrogyria is commonly associated with congenital cytomegalovirus 14. Cytomegalovirus (CMV) is a herpes type of virus that is very common and is typically harmless to the general population 15.
The National CMV Network at https://www.nationalcmv.org states the following information:
- According to the Centers for Disease Control and Prevention (CDC), out of every 100 Americans, 50- 80 people will have had a CMV infection by the time they are 40 years of age. A CMV infection causes cold-like symptoms, such as sore throat, fever, fatigue and swollen glands. These mild Cytomegalovirus symptoms last for only a few short weeks and is rarely a cause for concern for healthy kids or adults. The symptoms are sometimes so mild, only resembling a common cold, that most people do not even know they have it. These mild Cytomegalovirus symptoms last for only a few short weeks and is rarely a cause for concern for healthy kids or adults. Once the CMV virus is in the persons body, it stays there for life.
Polymicrogyria inheritance pattern
Isolated polymicrogyria can have different inheritance patterns. Several forms of the condition, including bilateral frontoparietal polymicrogyria (which is associated with mutations in the ADGRG1 gene), have an autosomal recessive pattern of inheritance. In autosomal recessive inheritance, both copies of the gene in each cell have mutations. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition.
Polymicrogyria can also have an autosomal dominant inheritance pattern, which means one copy of the altered gene in each cell is sufficient to cause the disorder. Other forms of polymicrogyria appear to have an X-linked pattern of inheritance. Genes associated with X-linked conditions are located on the X chromosome, which is one of the two sex chromosomes. A characteristic of X-linked inheritance is that fathers cannot pass X-linked traits to their sons.
Some people with polymicrogyria have relatives with the disorder, while other affected individuals have no family history of the condition. When an individual is the only affected person in his or her family, it can be difficult to determine the cause and possible inheritance pattern of the disorder.
Polymicrogyria symptoms
A wide variety of symptoms may be observed in people with polymicrogyria, depending on the areas of the brain implicated and whether or not it is part of a larger syndrome. Signs and symptoms may include 4:
- Developmental delay
- Crossed eyes
- Epilepsy
- Paralysis of the face, throat, and tongue
- Difficulty with speech and swallowing
- Drooling
Polymicrogyria diagnosis
The diagnosis of polymicrogyria is made by imaging brain structures using MRI since computed tomography (CT) and other imaging methods do not have high enough resolution or adequate contrast to identify the small folds that define polymicrogyria 2. It is important that optimal imaging techniques (including thin sections) and age-specific protocols be used to provide the best contrast between gray and white matter with good spatial resolution and adequate signal-to-noise ratio 16. Typical findings include areas of the cerebral cortex with a complex set of small gyri that appear fused to each other and separated by shallow sulci. These findings may be isolated to one side of the brain (unilateral) or may involve both sides of the brain (bilateral) 17.
With high-quality MRI, microgyri and microsulci may be appreciated and stippling of the gray-white junction (a specific feature of polymicrogyria not seen in other malformations of cortical development) may be observed 18. Of note, the Sylvian fissures (best seen on sagittal imaging) should be scrutinized in particular, as polymicrogyria often affects these areas preferentially.
While polymicrogyria is usually an isolated finding (i.e., occurring in the absence of other brain malformations), it can be seen in association with other brain malformations including gray matter heterotopia and ventriculomegaly, as well as abnormalities of the white matter, corpus callosum, brain stem, and cerebellum.
MRI – when interpreted by an expert – can reliably differentiate polymicrogyria from other malformations of cortical development.
Prenatal ultrasound examination. In 5% of cases, polymicrogyria is detected on prenatal ultrasound examination by the presence of abnormalities – usually microcephaly and/or associated brain malformations. Note: polymicrogyria is difficult to detect by ultrasound examination until late in gestation 18.
Polymicrogyria treatment
Polymicrogyria treatment is based on the signs and symptoms present in each person 2. Treatment may require the coordinated efforts of a team of specialists. Pediatricians, neurologists, surgeons, physical therapists, and others may need to systematically and comprehensively plan an affected child’s treatment. Commonly used, but not limited too, are physical therapy for gross motor impairment, orthotic devices and surgery for those with spastic motor impairment. Speech therapy is widely used for language and feeding impairment. Augmentative and alternative communication devices are also commonly used to aide in speech deficits. Occupational therapy is used for fine motor difficulties and antiepileptic drugs are used to treat and control seizure.
Treatment with anticonvulsant drugs may help prevent, reduce, or control various types of epilepsy associated with polymicrogyria. In affected infants who exhibit sudden, involuntary contractions of the head, neck, and trunk and/or uncontrolled extension of the legs and/or arms in the first six months of life (infantile spasms or West Syndrome), treatment with adrenocorticotropic hormone (ACTH or corticotropin) has resolved the seizures in some cases. In cases when drug therapy is ineffective in preventing or controlling seizures (intractable epilepsy), surgical removal of tissue in certain areas of the brain (focal corticectomy) or surgical division (callosotomy) of the fibers joining the two cerebral hemispheres (corpus callosum) may result in seizure improvement.
Early intervention is important in ensuring that children with polymicrogyria reach their potential. Special services that may be beneficial to affected children may include physical therapy, special remedial education, speech therapy, and other medical, social, and/or vocational services.
Genetic counseling will be of benefit for affected children and their families. Other treatment is symptomatic and supportive.
Polymicrogyria prognosis
It is difficult to make a predictable prognosis because each individual is very unique in their presentation of polymicrogyria.
References- Leventer RJ, Phelan EM, Coleman LT, Kean MJ, Jackson GD, Harvey AS. Clinical and imaging features of cortical malformations in childhood. Neurology. 1999;53:715–22.
- Stutterd CA, Dobyns WB, Jansen A, et al. Polymicrogyria Overview. 2005 Apr 18 [Updated 2018 Aug 16]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1329
- Kuzniecky R, Andermann F, Guerrini R. Congenital bilateral perisylvian syndrome: study of 31 patients. The CBPS Multicenter Collaborative Study. Lancet. 1993;341:608–12.
- Polymicrogyria. https://ghr.nlm.nih.gov/condition/polymicrogyria
- Bilateral perisylvian polymicrogyria. https://rarediseases.info.nih.gov/diseases/6011/bilateral-perisylvian-polymicrogyria
- Congenital Bilateral Perisylvian Syndrome. https://rarediseases.org/rare-diseases/congenital-bilateral-perisylvian-syndrome
- Stutterd CA, Leventer RJ. Polymicrogyria: a common and heterogeneous malformation of cortical development. Am J Med Genet C Semin Med Genet. June, 2014; 166C(2):227-239. https://onlinelibrary.wiley.com/doi/full/10.1002/ajmg.c.31399
- Jansen A, Andermann E. Genetics of the polymicrogyria syndromes. Journal of Medical Genetics 2005;42:369-378. http://dx.doi.org/10.1136/jmg.2004.023952
- Clark M, Neville BG. Familial and genetic associations in Worster-Drought syndrome and perisylvian disorders. Am J Med Genet A. January 1, 2008; 146A(1):35-42. https://www.ncbi.nlm.nih.gov/pubmed/17994559
- POLYMICROGYRIA, BILATERAL PERISYLVIAN, AUTOSOMAL RECESSIVE; BPPR. https://www.omim.org/entry/615752
- Kilinc O, Ekinci G, Demirkol E & Agan K. Bilateral agenesis of arcuate fasciculus demonstrated by fiber tractography in congenital bilateral perisylvian syndrome. Brain Dev. March 2015; 37(3):352-355. https://www.ncbi.nlm.nih.gov/pubmed/24852949
- Chang BS, Piao X, Bodell A, et al. Bilateral frontoparietal polymicrogyria: clinical and radiological features in 10 families with linkage to chromosome 16. Ann Neurol2003;53:596–606.
- POLYMICROGYRIA, BILATERAL FRONTOPARIETAL; BFPP. https://omim.org/entry/606854
- Kwak M, Yum MS, Yeh HR, Kim HJ, Ko TS. Brain magnetic resonance imaging findings of congenital cytomegalovirus infection as a prognostic factor for neurological outcome. Pediatr Neurol. 2018;83:14–18.
- CMV & PMG. https://pmgawareness.org/cmv-pmg
- Barkovich AJ. MRI analysis of sulcation morphology in polymicrogyria. Epilepsia. 2010;51 Suppl 1:17–22.
- Golden JA, Bonnemann CG. Developmental Structural Disorders. In: Goetz CG. Textbook of Clinical Neurology. Philadelphia, PA: Saunders; 2007
- Leventer RJ, Jansen A, Pilz DT, Stoodley N, Marini C, Dubeau F, Malone J, Mitchell LA, Mandelstam S, Scheffer IE, Berkovic SF, Andermann F, Andermann E, Guerrini R, Dobyns WB. Clinical and imaging heterogeneity of polymicrogyria: a study of 328 patients. Brain. 2010;133:1415–27.