Postural orthostatic tachycardia syndrome
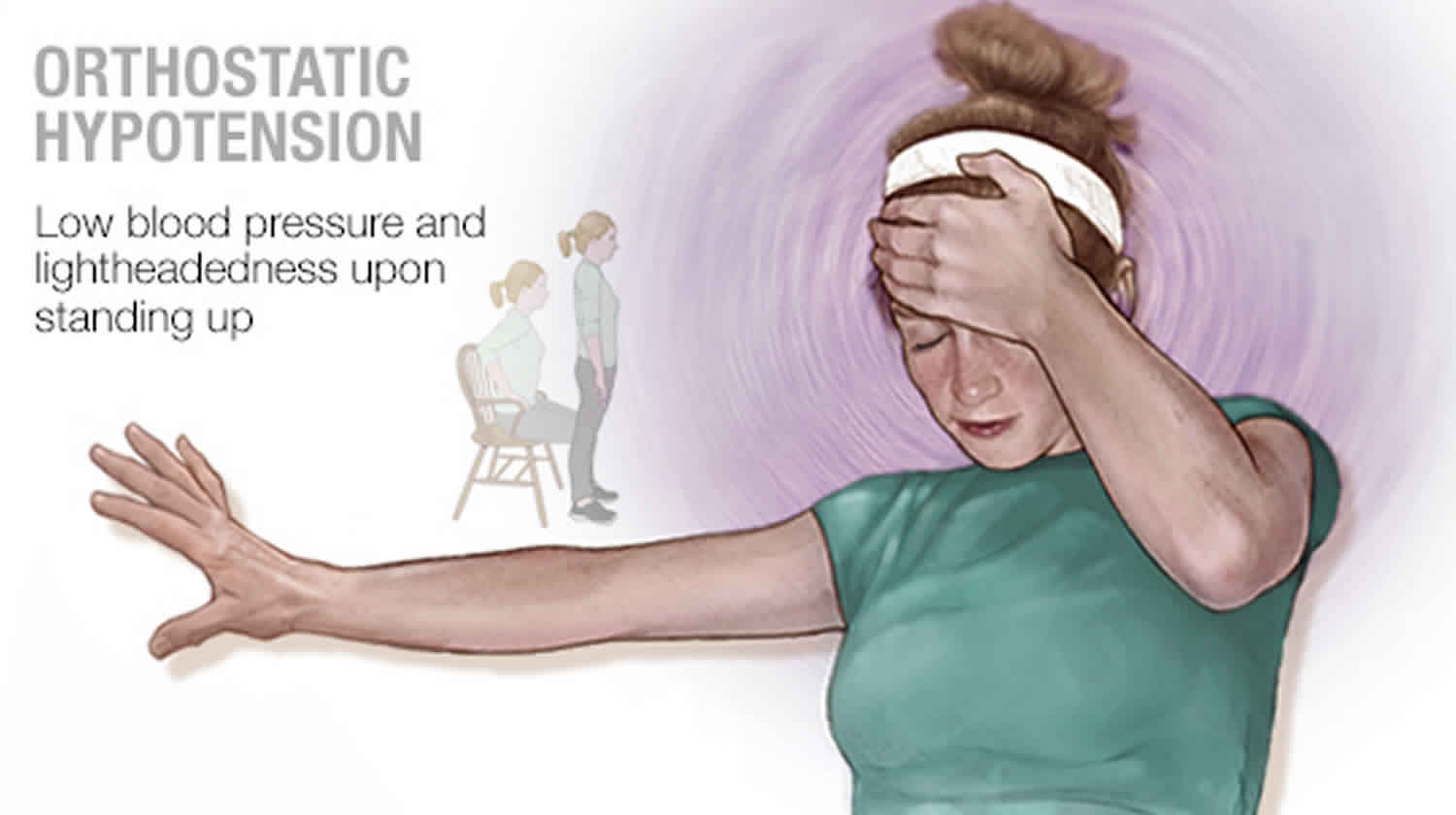
Postural orthostatic tachycardia syndrome (POTS) is a condition characterized by too little blood returning to the heart when moving from a lying down to a standing up position (orthostatic intolerance). Orthostatic intolerance describes a condition in which an excessively reduced volume of blood returns to the heart after an individual stands up from a lying down position. Orthostatic intolerance causes lightheadedness or fainting that can be eased by lying back down. In people with POTS, the lightheadedness or fainting are also accompanied by a rapid increase in heart rate of more than 30 beats per minute or a heart rate that exceeds 120 beats per minute, within 10 minutes of rising 1. The increase in heart rate may be a sign that the cardiovascular system is working hard to maintain blood pressure and blood flow to the brain. Although POTS can affect men and women of all ages, most cases (between 75 and 80 percent) are diagnosed in women between the ages of 15 and 50 1. Some women report an increase in episodes of POTS right before their menstrual periods.
Postural orthostatic tachycardia syndrome (POTS) is one of the most common forms of orthostatic intolerance globally and is estimated to affect over 500,000 patients in the United States alone 2. Worldwide prevalence has not been well-established, although previous study populations have estimated ranges between 0.2 to 1% in developed countries 3. The overwhelmingly demographic of POTS patients are young, premenopausal Caucasian females (4.5 to 1) between the ages of 15 and 45 years old 4, with the majority presenting between the ages of 15 and 25 years 5. There is a significant overlap between POTS, chronic fatigue syndrome and across a spectrum of autoimmune disorders 6.
Doctors aren’t sure yet what causes the reduced return of blood to the heart that occurs in orthostatic intolerance or why the heart begins to beat so rapidly in POTS. Current thinking is that there are a number of mechanisms. Some individuals have peripheral denervation (neuropathic POTS); some have symptoms that are due to sustained or parosyxmal overactivity of the sympathetic nervous system (hyperadrenergic POTS); and many individuals with POTS have significant deconditioning. However, POTS often begins after a pregnancy, major surgery, trauma, or a viral illness. It may make individuals unable to exercise because the activity brings on fainting spells or dizziness 7.
Therapies for POTS are targeted at relieving low blood volume or regulating circulatory problems that could be causing the disorder 8. No single treatment has been found to be effect for all. A number of drugs seem to be effective in the short term. Whether they help in long term is uncertain. Simple interventions such as adding extra salt to the diet and attention to adequate fluid intake are often effective. The drugs fludrocortisone (for those on a high salt diet) and midodrine in low doses are often used to increase blood volume and narrow blood vessels. Drinking 16 ounces of water (2 glassfuls) before getting up can also help raise blood pressure. Some individuals are helped by beta receptor blocking agents. There is some evidence that an exercise program can gradually improve orthostatic tolerance.
Positional orthostatic tachycardia syndrome key facts
- Postural orthostatic tachycardia syndrome (POTS) is a common form of autonomic dysregulation predominantly affecting young White females characterized by excessive tachycardia upon standing in the presence of orthostatic intolerance.
- Adult diagnostic criteria require a heart rate increase of greater than or equal to 30 bpm within the first 10 minutes of standing or head-up tilt (HUT) in the absence of orthostatic hypotension.
- The complex heterogeneous etiologies of POTS generally classify as neuropathic, hyperadrenergic, hypovolemic, autoimmune, and physical deconditioning with significant overlap between the various etiologies.
- Symptoms are often chronic and non-specific and may include chronic fatigue, dizziness, sleep disturbance, headache, tremors, tachycardia, anxiety, depression, gastrointestinal disturbances, syncope, and vision changes.
- Management and treatment require an emphasis on patient education, and a progressive monitored exercise regimen with second-line pharmacologic approaches aimed at increasing fluid volume and controlling excessive sympathetic drive (fludrocortisone, midodrine, clonidine, propranolol).
- Prognosis is favorable especially with younger age at onset, with more than half of patients no longer meeting POTS criteria within 5 years.
Postural orthostatic tachycardia syndrome causes
The cause of POTS is unknown. A variety of proposed causes have led to the characterization of specific postural orthostatic tachycardia syndrome subtypes as described below, with a general consensus of excessive tachycardia in the setting of cardiovascular deconditioning as the final common pathway 9.
Neuropathic POTS
Neuropathic postural orthostatic tachycardia syndrome is a length-dependent autonomic neuropathy characterized by predominantly lower limb sympathetic denervation leading to reduced venoconstriction and venous pooling 10. One study observed 50% of POTS patients exhibited peripheral sudomotor denervation correlated with a distal pattern of anhidrosis demonstrated by thermoregulatory sweat testing 11. POTS patients have been observed to have decreased norepinephrine spillover in the lower extremities despite normal systemic norepinephrine spillover implicating dysfunctional norepinephrine reuptake due to injured terminal nerves 12. Peripheral venous pooling evidenced by dependent acrocyanosis has also been observed 5. Thus, an excessive cardiovascular response is necessary to maintain adequate mean arterial pressures.
Hyperadrenergic POTS
An estimated 30 to 60% of postural orthostatic tachycardia syndrome patients fall under the hyperadrenergic subtype, characterized by elevated standing plasma norepinephrine levels of greater than or equal to 600 pg/mL with predominant symptoms of increased sympathetic tone including palpitations, tremors, hypertension, anxiety, and tachycardia 13. A norepinephrine transporter (NET) loss of function gene mutation (SLC6A2) resulting in deficient norepinephrine transport contributing to an increased mean supine heart rate was a feature in one case 14. Norepinephrine transporter (NET) block is more frequently seen in the setting of pharmacologic inhibition by medications including tricyclic antidepressants, sympathomimetics (i.e., methylphenidate), and norepinephrine reuptake inhibitors (i.e., bupropion) 13. These medications are often useful in treating the associated cognitive effects of POTS such as depression, anxiety, and concentration difficulties. Therefore it is prudent to ensure patients are systemically clear of possible pharmacologic causes of elevated catecholamine levels and tachycardia throughout diagnostic evaluations.
Hypovolemic POTS
Up to 70% of patients with postural orthostatic tachycardia syndrome exhibit decreased plasma, red blood cell, and total blood volumes, although the degree of hypovolemia varies between studies 15. In POTS patients, this physiologic low volume state persists in association with a paradoxically low level of renin and aldosterone levels, suggesting a possible impairment of the renin-angiotensin-aldosterone axis that is crucial to maintaining adequate plasma volume 16. Secondary hypovolemic states present in patients with co-existing gastrointestinal conditions culminating in excessive fluid loss and poor volume intake (nausea, vomiting, diarrhea) 13.
Autoimmune POTS
An autoimmunity hypothesis is one proposal for postural orthostatic tachycardia syndrome given the significant overlapping commonalities (female predominance, post-viral onset, elevated autoimmune markers) seen in other systemic autoimmune disorders such as rheumatoid arthritis, lupus, and Sjogren’s syndrome 13. Previous studies have demonstrated increased autoantibodies in POTS. Positive antinuclear antibodies were present in up to 25% of patients, with Hashimoto thyroiditis being the most prevalent 3. One study demonstrated increased proinflammatory IL-6 levels in POTS patients associated with increased sympathetic drive, perhaps driven by chronic systemic immune activation 17. Additionally, other autoimmune markers including ganglionic AChR, G-protein coupled receptor, and various nonspecific autoantibodies have presented in the POTS population 6.
Deconditioning POTS
Physical and cardiovascular deconditioning is often evident in patients with postural orthostatic tachycardia syndrome, although its presence as either a cause or effect is unclear 5. Moreover, it appears the severity of deconditioning does not necessarily correlate with objective laboratory or autonomic findings 18. Similar POTS-like symptoms have been observed in otherwise healthy individuals placed in microgravity environments such as space flight, further implicating the physical and gravity dependent roles underlying POTS 9. Decreased cardiac size and mass have been demonstrated in POTS patients compared to healthy controls, with an average decreased left ventricular mass of 16% and reduced plasma volume of 20% 19. The well documented chronic fatigue, autonomic instability, and overall functional impairment give way to reduced physical activity and prolonged bed rest states, resulting in an unfavorable feedback cycle that exacerbates already prominent existing symptoms.
POTS pathophysiology
The pathophysiology underlying postural orthostatic tachycardia syndrome is heterogeneous, encompassing excess sympathetic tone, impaired peripheral autonomic function, volume dysregulation, cardiovascular deconditioning, and autoimmune dysfunction 13. In normal healthy subjects, a shift of the intravascular volume to the interstitial space reduces the total effective circulating blood volume, reflecting the gravity-dependent physiology seen in orthostatic-related pathologies. As expected, a subsequent reduction in stroke volume results in a compensatory increased sympathetic drive augmenting cardiac contractility, heart rate, and systemic vascular resistance. POTS patients exhibit persistent decreased stroke volume despite an exaggerated sympathetic response with postural changes such as standing, culminating in a final common pathway of tachycardia in the presence of orthostatic intolerance on standing 13.
The mechanisms as mentioned earlier are not mutually exclusive but instead overlap in a complex interaction of cause and effect. Affected physiologic systems include neuropathic, cardiovascular, renal, immune, and hematologic; this widespread implication of complex systems have added a certain degree of difficulty in constructing a comprehensive framework in the understanding of POTS. Common symptoms include chronic fatigue, dizziness, sleep disturbance, headache, tremors, tachycardia, anxiety, depression, gastrointestinal disturbances, syncope, and vision changes 3.
Postural orthostatic tachycardia syndrome symptoms
POTS symptoms and signs (for at least 6 months):
- Lightheadedness, palpitations and tremulousness during standing
- Other upright posture symptoms may include:
- Visual changes
- Discomfort in the head and neck
- Throbbing of the head
- Poor concentration
- Tiredness
- Weakness
- Occasionally fainting
- Nausea
- Chest discomfort
- Shortness of breath
The typical POTS patient is a young female between 15 and 25 years old presenting with multiple often chronic symptoms such as fatigue, lightheadedness, palpitations, cognitive impairment, and less commonly syncope 3. Autonomic dysfunction often manifests as gastrointestinal symptoms (nausea, abdominal pain) and bladder complaints (suprapubic pain, frequency) 5. Additionally, stressors including viral infections, trauma, surgery, and pregnancy have been noted to precipitate symptom onset 5. Family history is not well correlated due to the generalized and chronic nature of the syndrome. It is important to elucidate possible contributing factors such as physical fitness level, sleep hygiene, fluid intake, and current medication or supplement usage.
The physical exam may reveal peripheral edema, acrocyanosis, clammy skin, joint hypermobility, and changes in peripheral sensation 3. The absence of discrete findings on the physical exam does not preclude the presence of POTS.
Postural orthostatic tachycardia syndrome diagnosis
The initial evaluation of suspected postural orthostatic tachycardia syndrome should focus on excluding primary cardiovascular etiologies such as structural heart defects or tachyarrhythmias, underlying systemic causes including endocrine dysfunction, establishing chronicity of autonomic complaints, medication review, and assessing associated co-morbidities including gastrointestinal, neurological, and psychiatric signs and symptoms 10.
In addition to a complete history and physical, basic labs and a thorough cardiac evaluation (electrocardiogram, echocardiogram, Holter monitor) should be initiated. The predominance of specific states such as physical deconditioning, gastrointestinal, urologic, and hyperadrenergic symptoms may necessitate additional testing including VO2 max exercise testing, thyroid function panel and autoimmune studies, plasma, and urinary metanephrines, and specialist consultation 3.
An active stand test consists of having the patient lying supine for 10 minutes with measurement of supine baseline blood pressure and heart rate; the patient then stands and with re-measurement of BP and HR at timed intervals (1, 3, 5, and 10 minutes) 13. The head-up tilt table (HUT) with non-invasive hemodynamic monitoring is the accepted gold standard for assessing orthostatic intolerance in POTS 3. Current adult diagnostic criterion requires a heart rate increment greater than or equal to 30 bpm within the first 10 minutes of standing or head-up tilt table (HUT) in the absence of orthostatic hypotension 13.
Postural orthostatic tachycardia syndrome treatment
The management of postural orthostatic tachycardia syndrome divides into non-pharmacologic and pharmacologic approaches and contingent on accurate diagnosis, patient education, and therapy adherence.
Patient education and management of expectations are crucial to the overall successful management of POTS given its often non-specific and chronic debilitating nature. It is important to assess the patient’s understanding, answer and follow-up on questions and concerns, and emphasize the need for a multi-pronged therapeutic approach to treatment to improve quality of life. There is no current class I recommendations for POTS management 3. Regardless of treatment, each approach should be tailored individually to predominating subtypes (e.g., hyperadrenergic, hypovolemic).
A recent study 2016 study evaluating 33 adolescents with confirmed POTS who underwent a 3-week an interprofessional rehabilitation program consisting of physicians, physical and occupational therapists, psychologists, and nurses saw significant reductions in psychological stress and functional impairment 20.
Exercise conditioning is a fundamental aspect of postural orthostatic tachycardia syndrome treatment 3 and it is a recommendation for all patients to start on a gradual physical exercise regimen 21. Given the high probability of symptom exacerbation with activity, beginning with a supervised low-intensity program focused on avoiding upright positioning (rowing, swimming) with incremental progression over 3 months has been demonstrated to improve symptoms 13. A previous progressive 3-month exercise regimen was found to increase maximal oxygen intake 11%, left ventricular mass 12%, end-diastolic volume 8%; at the conclusion, 53% (10/19 patients) no longer met POTS criteria 22. Other conservative non-pharmacologic interventions include physical counter maneuvers (muscle contraction, leg crossing, forward bending) 10, compression garments, increased fluid (2-3 liters) and salt (slowly up to 10 grams) intake 9 and avoidance of symptom exacerbation (caffeine, alcohol, prolonged heat exposure).
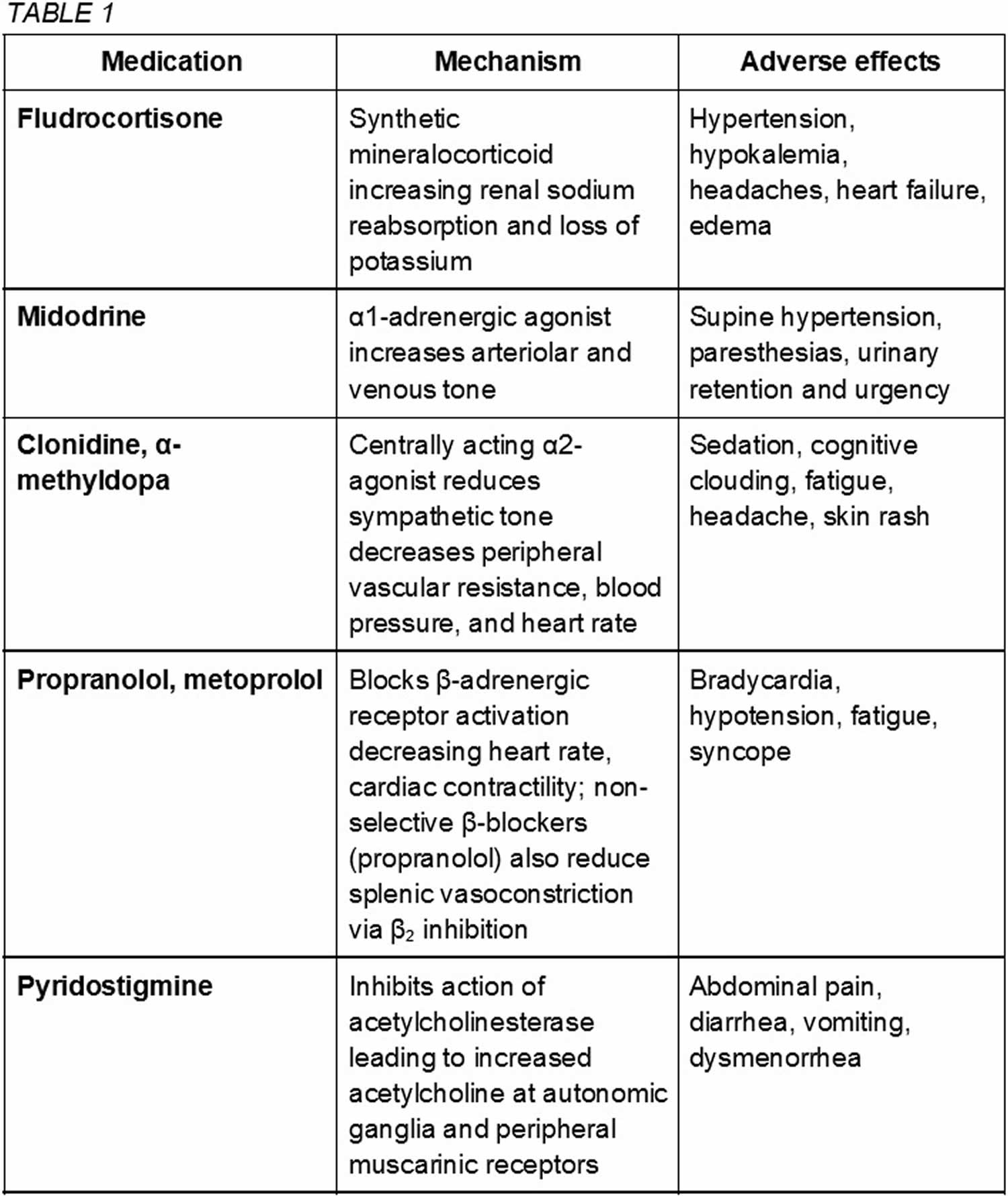
Pharmacologic therapies are not considered first-line treatment for POTS and enter the clinical picture in severe or refractory cases with the goal of stabilization for continued physical reconditioning 5. POTS medications are not proven to be more effective than non-pharmacologic approaches and should be utilized with caution given potential adverse interactions and side effects. The US Food and Drug Administration (FDA) has not approved any drug for POTS treatment. The following medications are used off label 13. Some common medications are described here and summarized in table 1.
- Fludrocortisone, a synthetic mineralocorticoid aldosterone analog, increases salt retention and plasma volume. Adverse hypertension, hypokalemia, and headaches may be present.
- The alpha-1-adrenergic agonist midodrine causes systemic vasoconstriction leading to an increase in venous return that may be effective in hypotensive phenotypes. Limitations include frequent dosing, urinary retention, and supine hypertension 15.
- Clonidine and alpha-methyldopa are central-acting alpha-2 agonist sympatholytics that may be beneficial in hyperadrenergic subtypes with hypertension as a predominant symptom. May cause adverse sedation, cognitive clouding, and fatigue.
- Beta-blockers (propranolol, metoprolol) may reduce upright tachycardia without significant hemodynamic changes. However, worsening fatigue is a concern.
- Pyridostigmine is an acetylcholinesterase inhibitor that increases acetylcholine levels in the autonomic ganglia 5. In turn, this may reduce tachycardia with minimal hemodynamic effects; however worsening cramps, vomiting, and urinary symptoms often limit continued use.
Generally medications exacerbating specific symptoms such as tachycardia (sympathomimetics including amphetamines, selective serotonin and/or norepinephrine reuptake inhibitors, droxidopa) or worsening orthostatic intolerance (diuretics, calcium channel blockers, nitrates, opiates, tricyclic antidepressants) should be avoided; in specific cases it may be beneficial in accordance with the patient’s history and presentation 13.
Postural orthostatic tachycardia syndrome prognosis
POTS may follow a relapsing-remitting course, in which symptoms come and go, for years. In most cases (approximately 80 percent), an individual with POTS improves to some degree and becomes functional, although some residual symptoms are common.
Over half of patients do not meet criteria for POTS within 5 years, most within the first 1 to 2 years, characterized as the absence of orthostatic symptoms with minimal functional impairment 3. Younger patients generally experience more favorable outcomes 21, with only a sporadic few cases of POTS developing in those over 50 years old 15. There have no deaths attributed directly to POTS 4.
Postural orthostatic tachycardia syndrome complications
There is limited data regarding specific complications arising from postural orthostatic tachycardia syndrome; however, the impact on the quality of life and daily function may be quite significant. Worsening physical and cardiovascular deconditioning may predispose some individuals to increased rates of infection, thromboembolism in addition to detrimental maladaptive psychological and cognitive processes. Anxiety, depression, and fatigue often persist despite treatment, perhaps revealing a therapeutic avenue for cognitive and behavioral approaches.
References- Postural Tachycardia Syndrome Information Page. https://www.ninds.nih.gov/Disorders/All-Disorders/Postural-Tachycardia-Syndrome-Information-Page
- Zhao S, Tran VH. Postural Orthostatic Tachycardia Syndrome (POTS) [Updated 2019 Apr 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541074
- Fedorowski A. Postural orthostatic tachycardia syndrome: clinical presentation, aetiology and management. J. Intern. Med. 2019 Apr;285(4):352-366.
- Jones PK, Shaw BH, Raj SR. Clinical challenges in the diagnosis and management of postural tachycardia syndrome. Pract Neurol. 2016 Dec;16(6):431-438.
- Zadourian A, Doherty TA, Swiatkiewicz I, Taub PR. Postural Orthostatic Tachycardia Syndrome: Prevalence, Pathophysiology, and Management. Drugs. 2018 Jul;78(10):983-994.
- Vernino S, Stiles LE. Autoimmunity in postural orthostatic tachycardia syndrome: Current understanding. Auton Neurosci. 2018 Dec;215:78-82.
- What is hypovolemic postural tachycardia syndrome (POTS)? https://www.rarediseasesnetwork.org/cms/autonomic/Learn-More/Disorder-Definitions
- Idiopathic Orthostatic Hypotension and other Autonomic Failure Syndromes. https://emedicine.medscape.com/article/1154266-overview
- Fu Q, Levine BD. Exercise and non-pharmacological treatment of POTS. Auton Neurosci. 2018 Dec;215:20-27.
- Benarroch EE. Postural tachycardia syndrome: a heterogeneous and multifactorial disorder. Mayo Clin. Proc. 2012 Dec;87(12):1214-25.
- Thieben MJ, Sandroni P, Sletten DM, Benrud-Larson LM, Fealey RD, Vernino S, Lennon VA, Shen WK, Low PA. Postural orthostatic tachycardia syndrome: the Mayo clinic experience. Mayo Clin. Proc. 2007 Mar;82(3):308-13.
- Jacob G, Costa F, Shannon JR, Robertson RM, Wathen M, Stein M, Biaggioni I, Ertl A, Black B, Robertson D. The neuropathic postural tachycardia syndrome. N. Engl. J. Med. 2000 Oct 05;343(14):1008-14.
- Bryarly M, Phillips LT, Fu Q, Vernino S, Levine BD. Postural Orthostatic Tachycardia Syndrome: JACC Focus Seminar. J. Am. Coll. Cardiol. 2019 Mar 19;73(10):1207-1228.
- Shannon JR, Flattem NL, Jordan J, Jacob G, Black BK, Biaggioni I, Blakely RD, Robertson D. Orthostatic intolerance and tachycardia associated with norepinephrine-transporter deficiency. N. Engl. J. Med. 2000 Feb 24;342(8):541-9.
- Sheldon RS, Grubb BP, Olshansky B, Shen WK, Calkins H, Brignole M, Raj SR, Krahn AD, Morillo CA, Stewart JM, Sutton R, Sandroni P, Friday KJ, Hachul DT, Cohen MI, Lau DH, Mayuga KA, Moak JP, Sandhu RK, Kanjwal K. 2015 heart rhythm society expert consensus statement on the diagnosis and treatment of postural tachycardia syndrome, inappropriate sinus tachycardia, and vasovagal syncope. Heart Rhythm. 2015 Jun;12(6):e41-63.
- Raj SR, Biaggioni I, Yamhure PC, Black BK, Paranjape SY, Byrne DW, Robertson D. Renin-aldosterone paradox and perturbed blood volume regulation underlying postural tachycardia syndrome. Circulation. 2005 Apr 05;111(13):1574-82.
- Okamoto LE, Raj SR, Gamboa A, Shibao CA, Arnold AC, Garland EM, Black BK, Farley G, Diedrich A, Biaggioni I. Sympathetic activation is associated with increased IL-6, but not CRP in the absence of obesity: lessons from postural tachycardia syndrome and obesity. Am. J. Physiol. Heart Circ. Physiol. 2015 Dec 15;309(12):H2098-107.
- Parsaik A, Allison TG, Singer W, Sletten DM, Joyner MJ, Benarroch EE, Low PA, Sandroni P. Deconditioning in patients with orthostatic intolerance. Neurology. 2012 Oct 02;79(14):1435-9.
- Miwa K, Fujita M. Small heart with low cardiac output for orthostatic intolerance in patients with chronic fatigue syndrome. Clin Cardiol. 2011 Dec;34(12):782-6.
- Bruce BK, Harrison TE, Bee SM, Luedtke CA, Porter CJ, Fischer PR, Hayes SE, Allman DA, Ale CM, Weiss KE. Improvement in Functioning and Psychological Distress in Adolescents With Postural Orthostatic Tachycardia Syndrome Following Interdisciplinary Treatment. Clin Pediatr (Phila). 2016 Dec;55(14):1300-1304.
- Grubb BP. Postural tachycardia syndrome. Circulation. 2008 May 27;117(21):2814-7.
- Fu Q, Vangundy TB, Galbreath MM, Shibata S, Jain M, Hastings JL, Bhella PS, Levine BD. Cardiac origins of the postural orthostatic tachycardia syndrome. J. Am. Coll. Cardiol. 2010 Jun 22;55(25):2858-68.