What is prednisone
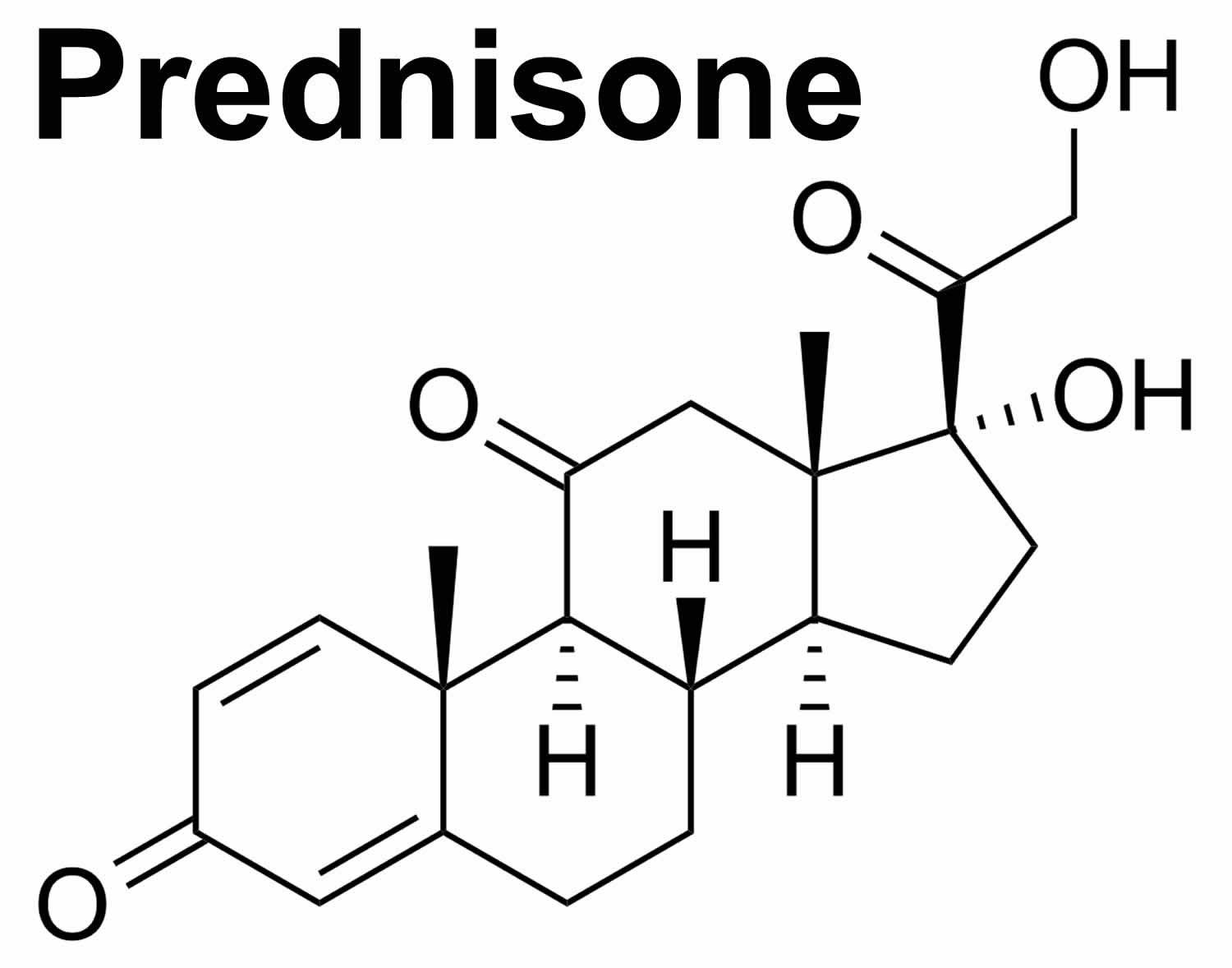
Prednisone is a man made anti-inflammatory with anti-inflammatory and immunomodulating properties derived from cortisone (corticosteroid). Corticosteroids are not the same as anabolic steroids. In contrast to anabolic steroids (used by “bodybuilders”), prednisone (corticosteroid) is used in inflammatory conditions for their anti–inflammatory effects. Prednisone has a rapid onset of action, and profoundly affect many parts of the immune system as well as most other body systems. Prednisone is biologically inert and converted to prednisolone in your liver. Prednisone is a glucocorticoid receptor agonist (activator). Prednisone is first metabolized in your liver to its active form, prednisolone. Prednisolone crosses cell membranes and binds with high affinity to specific cytoplasmic receptors. After cell surface receptor attachment and cell entry, prednisone enters the nucleus where it binds to and activates specific nuclear receptors, resulting in an altered gene expression and inhibition of proinflammatory cytokine production. The result includes inhibition of leukocyte (white blood cell) infiltration at the site of inflammation, interference in the function of mediators of inflammatory response, suppression of humoral immune responses, and reduction in edema or scar tissue. Prednisone agent also decreases the number of circulating lymphocytes, induces cell differentiation, and stimulates apoptosis in sensitive tumor cell populations. The antiinflammatory actions of corticosteroids are thought to involve phospholipase A2 inhibitory proteins, lipocortins, which control the biosynthesis of potent mediators of inflammation such as prostaglandins and leukotrienes.
Prednisone is used to treat a wide range of health problems including allergies, blood disorders, skin diseases, infections, certain cancers and to prevent organ rejection after a transplant.
Prednisone helps by reducing inflammation. Prednisone also damps down your immune system, which can help in autoimmune illnesses, like rheumatoid arthritis, where your immune system mistakenly attacks its own tissues.
Prednisone is available only on prescription as tablets and as a liquid to drink. It can also be given by injection but this is usually only done in hospital.
Key facts
- Take prednisone once a day in the morning so it doesn’t keep you awake.
- Taking prednisone can make you more likely to get infections. Tell your doctor if you’re exposed to infectious illnesses like chickenpox or shingles.
- The most common side effects of prednisone are weight gain, indigestion, insomnia and sweating a lot.
- Prednisone can cause withdrawal problems if you stop taking it suddenly. Do not stop the medicine suddenly if you’ve been on it for more than 3 weeks or have taken high doses (more than 40mg) for more than 1 week.
- Prednisone is also called by the brand names Prednisone Intensol, Sterapred, Sterapred DS, Deltacortril, Deltastab, Dilacort and Pevanti.
What does prednisone do?
Prednisone is in a class of medications called corticosteroids. It works to treat patients with low levels of corticosteroids by replacing steroids that are normally produced naturally by the body. Prednisone works to treat other conditions by reducing swelling and redness and by changing the way the immune system works.
Prednisone is used alone or with other medications to treat the symptoms of low corticosteroid levels (lack of certain substances that are usually produced by the body and are needed for normal body functioning). Prednisone is also used to treat other conditions in patients with normal corticosteroid levels. These conditions include certain types of arthritis; severe allergic reactions; multiple sclerosis (a disease in which the nerves do not function properly); lupus (a disease in which the body attacks many of its own organs); and certain conditions that affect the lungs, skin, eyes, kidneys blood, thyroid, stomach, and intestines. Prednisone is a cornerstone of treating most types of vasculitis, and are often used in combination with other immunosuppressive medications. Prednisone is also sometimes used to treat the symptoms of certain types of cancer.
Prednisone is also sometimes used with antibiotics to treat a certain type of pneumonia in patients with acquired immunodeficiency syndrome (AIDS). Talk to your doctor about the risks of using this drug for your condition.
Prednisone may be prescribed for other uses; ask your doctor or pharmacist for more information.
How does prednisone work?
In contrast to anabolic steroids (used by “bodybuilders”), glucocorticoids (corticosteroids) are used in inflammatory conditions for their anti–inflammatory effects. Prednisone has a rapid onset of action, and profoundly affect many parts of the immune system as well as most other body systems.
Corticosteroids mimic the effects of hormones your body naturally produces in your adrenal glands. The adrenal glands sit on top of your kidneys.
When prescribed in doses higher than your body’s usual levels, corticosteroids like prednisone dampen inflammation. This can reduce the symptoms of inflammatory conditions, such as arthritis and asthma.
Prednisone also damp down your immune system, which can help in autoimmune illnesses, like rheumatoid arthritis, where your immune system mistakenly attacks its own tissues.
Are there other steroids?
There are other corticosteroids available, including:
- deflazacort
- dexamethasone
- methylprednisone
- prednisolone
For most health problems, these steroids are very similar to prednisone in terms of how well they work and how safe they are.
Oral Prednisone Potency:
Prednisone 5 mg is approximately equivalent to:
- Betamethasone 0.75 mg;
- Cortisone 25 mg;
- Dexamethasone 0.75 mg;
- Hydrocortisone 20 mg;
- Methylprednisolone 4 mg;
- Prednisolone 5 mg;
- Triamcinolone 4 mg
When will I feel better?
This can vary. For some illnesses, you will feel better after a couple of days. Ask your doctor what to expect for your illness.
For other illnesses, you may not feel any better even though the medicine is helping you. This may be the case if you’re taking prednisone to stop your symptoms getting worse or to prevent a problem happening (for example after an organ transplant).
How long will I take prednisone for?
This depends on your health problem. You may only need a short course of prednisone for up to a week.
You may need to take it for longer – even for many years or the rest of your life.
Will I put on weight?
If you have to take prednisone for more than a few weeks, the chances are that you will put on weight. prednisone can make you hungrier and retain water so it can be quite challenging to avoid weight gain. Try to eat a healthy balanced diet without increasing your portion sizes. Regular exercise will also help to keep your weight stable.
Will it affect my mood?
You may notice mood changes and mental health problems while taking prednisone, including:
- feeling depressed (including thinking about suicide)
- feeling high or moods that go up and down
- feeling anxious, having problems sleeping, difficulty in thinking or being confused and losing your memory
- feeling, seeing or hearing things which do not exist
- having strange and frightening thoughts, changing how you act or having feelings of being alone
The higher the dose, the more intense the mood changes can be.
If this happens to you, talk to your doctor.
What will happen if I come off prednisone?
Don’t stop taking prednisone without talking to your doctor – you will need to reduce the dose gradually.
It can be dangerous to stop taking prednisone suddenly, especially if you have been on a high dose for a long time.
Your health condition may flare up again. You may also get withdrawal symptoms including:
- severe tiredness
- weakness
- body aches
- joint pain
Withdrawal problems are most likely to happen if you have taken prednisone for more than a few weeks or you take more than 40mg daily.
Your doctor will probably want to reduce your dose gradually over several weeks to prevent these side effects.
Can I take prednisone for a long time?
Taking prednisone for many months or years can have several harmful effects on your body. It can lead to:
- thinner bones (osteoporosis)
- poorly controlled diabetes
- eyesight problems
- slower growth in children and teenagers
If you have to take prednisone for a long time, there are steps you can take to stay as healthy as possible:
- Take regular exercise and make sure you get enough calcium in your diet to help strengthen your bones. Calcium-rich foods include milk, cheese and leafy greens. To check your bones, your doctor may arrange for you to have an occasional bone scan.
- If you have diabetes, you may need to check your blood glucose more often. Your doctor can advise you more about this.
- To reduce the chances of eyesight problems, visit an optometrist every 12 months to check for high pressure in your eye (glaucoma) and cataracts.
- Make sure that children and teenagers have their height monitored regularly by a doctor so that any stunting of growth can be picked up promptly.
Will prednisone affect my fertility?
No, prednisone does not reduce the fertility of men or women.
Will it affect my contraception?
For women, prednisone will not affect contraceptive pills or the morning after pill.
Can I drink alcohol with prednisone?
Yes, you can drink alcohol while taking prednisone.
Is there any food or drink I need to avoid?
Do not eat liquorice while taking prednisone.
It’s thought that real liquorice (licorice) increases the amount of prednisone in the body and also increases the risk of low potassium.
Do I need to be careful of infections?
Taking prednisone makes you more likely to catch infections such as flu, the common cold and chest infections, because prednisone suppresses your immune system.
Keep away from people with an infectious disease, especially chickenpox or shingles. If you have never had these illnesses they could make you very ill.
Tell your doctor straight away if you come into contact with someone who has an infectious disease such as chickenpox or shingles. Your doctor may be able to prescribe a medicine to protect you.
Can I have vaccinations?
Some vaccines are not suitable for you while you are taking prednisone.
Taking prednisone lowers your immune system. If you have a ‘live’ vaccine, like the shingles vaccine, while you are taking prednisone your immune system might not be able to handle it. This may lead to an infection. Inactive vaccinations, like the flu vaccine, are safe.
If you need any vaccinations, mention that you are taking a steroid.
How to take prednisone
Prednisone comes as a tablet, a solution (liquid), and a concentrated solution to take by mouth. Prednisone is usually taken with food one to four times a day or once every other day. Your doctor will probably tell you to take your dose(s) of prednisone at certain time(s) of day every day. Your personal dosing schedule will depend on your condition and on how you respond to treatment. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take prednisone exactly as directed. Do not take more or less of it or take it more often or for a longer period of time than prescribed by your doctor.
It’s important to take prednisone as your doctor has advised.
- The usual dose varies between 5mg and 60mg daily – 1ml of liquid prednisone is roughly equal to 10mg.
- It’s best to take prednisone as a single dose once a day straight after breakfast. For example, if your dose is 40mg daily, it’s usual to take 8 tablets (8 x 5mg) all at the same time.
- Take prednisone with breakfast so it doesn’t upset your stomach. Taking prednisone in the morning also means it’s less likely to affect your sleep.
- If you have enteric coated (red or brown) tablets, you can take these with or without food but make sure to swallow them whole. Do not take indigestion medicines 2 hours before or after taking enteric coated tablets.
- Sometimes, you may be advised to take prednisone on alternate days only.
Your doctor may instruct you to follow a low-salt, high potassium, or high calcium diet. Your doctor may also prescribe or recommend a calcium or potassium supplement. Follow these directions carefully.
Talk to your doctor about eating grapefruit and drinking grapefruit juice while you are taking prednisone.
If you are taking the concentrated solution, use the specially marked dropper that comes with the medication to measure your dose. You may mix the concentrated solution with juice, other flavored liquids, or soft foods such as applesauce.
Your doctor may change your dose of prednisone often during your treatment to be sure that you are always taking the lowest dose that works for you. Your doctor may also need to change your dose if you experience unusual stress on your body such as surgery, illness, infection, or a severe asthma attack. Tell your doctor if your symptoms improve or get worse or if you get sick or have any changes in your health during your treatment.
If you are taking prednisone to treat a long-lasting disease, the medication may help control your condition but will not cure it. Continue to take prednisone even if you feel well. Do not stop taking prednisone without talking to your doctor. If you suddenly stop taking prednisone, your body may not have enough natural steroids to function normally. This may cause symptoms such as extreme tiredness, weakness, slowed movements, upset stomach, weight loss, changes in skin color, sores in the mouth, and craving for salt. Call your doctor if you experience these or other unusual symptoms while you are taking decreasing doses of prednisone or after you stop taking the medication.
Who can and can’t take prednisone
Prednisone can be taken by adults and children.
Prednisone isn’t suitable for some people.
Tell your doctor before starting prednisone if you:
- have had an allergic reaction to prednisone or any other medicine
- have an infection (including eye infections)
- are trying to get pregnant, are already pregnant or you are breastfeeding
- have recently been in contact with someone with shingles, chickenpox or measles (unless you are sure you are immune to these infections)
- have recently had, or are about to have, any vaccinations
Make sure your doctor is aware if you have:
- had liver problems
- had mental health problems (either you or close family members)
- any unhealed wounds
- heart failure or have had a recent heart attack
- high blood pressure
- diabetes
- epilepsy
- glaucoma
- underactive thyroid
- osteoporosis (thinning bones)
- a stomach ulcer
Prednisone special precautions
Before taking prednisone:
- tell your doctor and pharmacist if you are allergic to prednisone, any other medications, or any of the inactive ingredients in prednisone tablets or solutions. Ask your doctor or pharmacist for a list of the inactive ingredients.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, and nutritional supplements you are taking or plan to take. Be sure to mention any of the following: amiodarone (Cordarone, Pacerone); anticoagulants (‘blood thinners’) such as warfarin (Coumadin); certain antifungals such as fluconazole (Diflucan), itraconazole (Sporanox), ketoconazole (Nizoral) and voriconazole (Vfend);aprepitant (Emend); aspirin; carbamazepine (Carbatrol, Epitol, Tegretol); cimetidine (Tagamet); clarithromycin (Biaxin, in Prevpak); cyclosporine (Neoral, Sandimmune); delavirdine (Rescriptor); diltiazem (Cardizem, Dilacor, Tiazac, others); dexamethasone (Decadron, Dexpak); diuretics (‘water pills’); efavirenz (Sustiva); fluoxetine (Prozac, Sarafem); fluvoxamine (Luvox); griseofulvin (Fulvicin, Grifulvin, Gris-PEG); HIV protease inhibitors including atazanavir (Reyataz), indinavir (Crixivan), lopinavir (in Kaletra), nelfinavir (Viracept), ritonavir (Norvir, in Kaletra), and saquinavir (Fortovase, Invirase); hormonal contraceptives (birth control pills, patches, rings, implants, and injections); lovastatin (Altocor, Mevacor); medications for diabetes; nefazodone; nevirapine (Viramune); phenobarbital; phenytoin (Dilantin, Phenytek); rifabutin (Mycobutin), rifampin (Rifadin, Rimactane, in Rifamate); sertraline (Zoloft); troleandomycin (TAO); verapamil (Calan, Covera, Isoptin, Verelan); and zafirlukast (Accolate).Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor what herbal products you are taking or plan to take, especially St. John’s wort.
- tell your doctor if you have an eye infection now or have ever had eye infections that come and go and if you have or have ever had threadworms (a type of worm that can live inside the body); diabetes; high blood pressure; emotional problems; mental illness; myasthenia gravis (a condition in which the muscles become weak); osteoporosis (condition in which the bones become weak and fragile and can break easily); seizures; tuberculosis (TB); ulcers; or liver, kidney, intestinal, heart, or thyroid disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breast-feeding. If you become pregnant while taking prednisone, call your doctor.
- if you are having surgery, including dental surgery, or need emergency medical treatment, tell the doctor, dentist, or medical staff that you are taking or have recently stopped taking prednisone. You should carry a card or wear a bracelet with this information in case you are unable to speak in a medical emergency.
- do not have any vaccinations (shots to prevent diseases) without talking to your doctor.
- you should know that prednisone may decrease your ability to fight infection and may prevent you from developing symptoms if you get an infection. Stay away from people who are sick and wash your hands often while you are taking this medication. Be sure to avoid people who have chicken pox or measles. Call your doctor immediately if you think you may have been around someone who had chicken pox or measles.
- If you are having any skin tests such as allergy tests or tuberculosis tests, tell the doctor or technician that you are taking prednisone.
Cautions with other medicines
There are many medicines that interfere with the way prednisone works, or that increase the risk of side effects. It’s very important you check a medicine is safe to take with prednisone before you start taking it.
This includes some medicines that you buy over the counter like aspirin and anti-inflammatory painkillers such as ibuprofen.
Tell your doctor or pharmacist if you take any other medicines, including herbal remedies, vitamins or supplements.
Pregnancy and breastfeeding
Prednisone isn’t usually recommended in pregnancy unless the potential benefits outweigh the risks.
Prednisone has occasionally been linked to problems in the first 12 weeks of pregnancy. High doses or long term use can also affect the unborn baby’s growth.
If you take prednisone in pregnancy, the baby’s growth will be checked often.
Prednisone and breastfeeding
You can usually take prednisone while you’re breastfeeding. However, prednisone can get into breast milk. If you’re taking a high dose of prednisone the baby may need to be monitored for side effects.
For safety, it’s usually recommended that you wait 3 to 4 hours after taking your dose of prednisone before feeding your baby or expressing milk.
I am taking prednisone or prednisolone during the first trimester of my pregnancy. Is there a chance for birth defects?
Probably not. There has been some conflicting information about the use of prednisone/prednisolone during the first trimester. Older studies suggested a small increased chance for having a baby with a cleft lip with or without a cleft palate. Newer studies and further review of the older studies do not support this. If there is a risk, it appears that it is small and most pregnancies would not be affected.
It is recommended that you speak with your health care provider before you stop or change any medication. The benefits of taking prednisone or prednisolone and treating your condition should be weighed against any possible risk to the developing pregnancy.
I have to take prednisone or prednisolone every day during my pregnancy. Will this cause any other harmful effects?
Probably not. Taking an oral corticosteroid like prednisone or prednisolone long-term during pregnancy has been associated with an increased chance for delivering a baby that is premature (born before 37 weeks of pregnancy) and/or has a lower birth weight than expected. However, corticosteroids are used to treat medical conditions that have a risk for prematurity and low birth weight. This suggests that the effects are likely related to the mothers’ illnesses and not the medicines alone. Also, other studies have shown that the use of prednisone or prednisolone might improve some pregnancy outcomes.
Can I take prednisone/prednisolone while breastfeeding?
Yes, as only small amounts of prednisone and prednisolone enter breast milk. Prednisone is very similar to the body’s natural hormones, which are needed for milk production and the health of infants. Since people produce these hormones naturally, it is unlikely that the amount of prednisone and prednisolone in the breast milk would cause harmful effects in the nursing infant or the mother’s milk production.
The amount of prednisone/prednisolone in breast milk might be higher if taking higher doses. Levels in breast milk are likely highest about one hour after taking your medicine. To limit the amount in the breast milk, you can wait four hours after taking prednisone/prednisolone before breastfeeding your baby. Keeping your dose as low as possible will also help to limit the amount of medicine in your breast milk. There are reports of women who safely breastfed infants while taking prednisone or prednisolone.
Prednisone uses
Prednisone and prednisolone are used to treat many conditions, such as: asthma, autoimmune diseases, ulcerative colitis, psoriasis, breathing disorders, allergic disorders, lupus and skin conditions. They help to prevent or suppress inflammation (swelling and irritation) and immune responses. Prednisone and prednisolone are prescribed in a wide range of doses, depending on what condition is being treated. These medications are taken by mouth (orally).
Prednisone is used alone or with other medications to treat the symptoms of low corticosteroid (cortisol) levels (lack of certain substances that are usually produced by the body and are needed for normal body functioning). Prednisone is also used to treat other conditions in patients with normal corticosteroid levels. These conditions include certain types of arthritis; severe allergic reactions; multiple sclerosis (a disease in which the nerves do not function properly); lupus (a disease in which the body attacks many of its own organs); and certain conditions that affect the lungs, skin, eyes, kidneys blood, thyroid, stomach, and intestines. Prednisone is a cornerstone of treating most types of vasculitis, and are often used in combination with other immunosuppressive medications. Prednisone is also sometimes used to treat the symptoms of certain types of cancer.
Prednisone is also sometimes used with antibiotics to treat a certain type of pneumonia in patients with acquired immunodeficiency syndrome (AIDS). Talk to your doctor about the risks of using this drug for your condition.
Prednisone may be prescribed for other uses; ask your doctor or pharmacist for more information.
What is prednisone used for
Prednisone tablets and solutions are indicated in the following conditions:
Endocrine Disorders
Primary or secondary adrenocortical insufficiency (hydrocortisone or cortisone is the first choice: synthetic analogs may be used in conjunction with mineralocorticoids where applicable; in infancy mineralocorticoid supplementation is of particular importance); congenital adrenal hyperplasia; hypercalcemia associated with cancer; nonsuppurative thyroiditis.
Rheumatic Disorders
As adjunctive therapy for short-term administration (to tide the patient over an acute episode or exacerbation) in: psoriatic arthritis, rheumatoid arthritis, including juvenile rheumatoid arthritis (selected cases may require low-dose maintenance therapy), ankylosing spondylitis, acute and subacute bursitis, acute nonspecific tenosynovitis, acute gouty arthritis, post-traumatic osteoarthritis, synovitis of osteoarthritis, epicondylitis.
Collagen Diseases
During an exacerbation or as maintenance therapy in selected cases of: systemic lupus erythematosus, systemic dermatomyositis (polymyositis), acute rheumatic carditis.
Dermatologic Diseases
Pemphigus; bullous dermatitis herpetiformis; severe erythema multiforme (Stevens-Johnson syndrome); exfoliative dermatitis; mycosis fungoides; severe psoriasis; severe seborrheic dermatitis.
Allergic States
Control of severe or incapacitating allergic conditions intractable to adequate trials of conventional treatment: seasonal or perennial allergic rhinitis; bronchial asthma; contact dermatitis; atopic dermatitis; serum sickness; drug hypersensitivity reactions.
Ophthalmic Diseases
Severe acute and chronic allergic and inflammatory processes involving the eye and its adnexa such as: allergic corneal marginal ulcers, herpes zoster ophthalmicus, anterior segment inflammation, diffuse posterior uveitis and choroiditis, sympathetic ophthalmia, allergic conjunctivitis, keratitis, chorioretinitis, optic neuritis, iritis and iridocyclitis.
Respiratory Diseases
Symptomatic sarcoidosis; Loeffler’s syndrome not manageable by other means; berylliosis; fulminating or disseminated pulmonary tuberculosis when used concurrently with appropriate antituberculous chemotherapy; aspiration pneumonitis.
Hematologic Disorders
Idiopathic thrombocytopenic purpura in adults; secondary thrombocytopenia in adults; acquired (autoimmune) hemolytic anemia; erythroblastopenia (RBC anemia); congenital (erythroid) hypoplastic anemia.
Neoplastic Diseases
For palliative management of: leukemias and lymphomas in adults, acute leukemia of childhood.
Edematous States
To induce a diuresis or remission of proteinuria in the nephrotic syndrome, without uremia, of the idiopathic type or that due to lupus erythematosus.
Gastrointestinal Diseases
To tide the patient over a critical period of the disease in: ulcerative colitis, regional enteritis.
Miscellaneous
Tuberculous meningitis with subarachnoid block or impending block when used concurrently with appropriate antituberculous chemotherapy; trichinosis with neurologic or myocardial involvement.
Prednisone dosage
The dose depends on your illness and whether you are taking prednisone as a short course or for longer.
In children, the dose may be lower than for an adult with the same illness because it is calculated according to their height and weight.
Your dose may go up or down.
Once your illness starts to get better, it’s likely that your dose will go down.
Your doctor will probably reduce your dose before you stop treatment completely.
Your dose may go up if your illness gets worse.
Dose Adjustments
Elderly: Dose selection should be cautious generally starting at the low end of the dose range.
Prednisone Discontinuation:
- Abrupt discontinuation after high-dose or long-term therapy should be avoided.
- Prednisone-induced adrenocortical insufficiency may persist for months after drug discontinuation.
- Recommendations:
- To reduce the effect of drug-induced adrenocortical insufficiency, gradual dose reduction is recommended.
- In situation of stress, this drug may need to be restarted or doses increased during dose reduction or for up to 12 months after discontinuation to account for drug-induced adrenocortical insufficiency.
Alternate Day Therapy:
- Alternate day therapy may be considered for long term oral glucocorticoid therapy to help minimize adrenal suppression, and other glucocorticoid-related side effects.
- In the event of an acute flare-up, it may be necessary to return to the full suppressive daily dose for control; once control is established; alternate day therapy may be reinstituted.
Dose adjustments of antidiabetic agents may be necessary as corticosteroids may increase blood glucose concentrations.
Changes in thyroid status may require corticosteroid dose adjustment
Routine administration of vaccines or toxoids should be deferred until corticosteroid therapy is discontinued if possible.
Switching from Immediate-release to Delayed-release:
- Patients on immediate-release prednisone, prednisolone, or methylprednisolone may be switched to delayed-release prednisone at an equivalent dose based on relative potency
What should I do if I forget a dose?
If you miss a dose of prednisone, take it as soon as you remember. If you don’t remember until the following day, skip the missed dose.
Do not take a double dose to make up for a forgotten one.
If you forget doses often, it may help to set an alarm to remind you. You could also ask your pharmacist for advice on other ways to help you remember to take your medicine.
What if I take too much?
Taking too many prednisone tablets by accident is unlikely to harm you.
If you’re worried, talk to your doctor or pharmacist.
Prednisone side effects
Many of the side–effects of steroids are predictable. All are related to:
- The amount of steroid a patient takes in his/her daily dose, and
- The length of time the patient remains on the medication. Not all side–effects occur in all patients.
The higher the dose of prednisone/prednisolone that you take, the greater the chance of side effects. You are less likely to get side effects if you take a relatively low dose of less than 20mg prednisone daily.
Some side effects, such as stomach upset or mood changes, can happen straight away. Others, such as getting a rounder face, happen after weeks or months.
Prednisone side effects short term
Common side effects
Common side effects happen in more than 1 in 100 people. Keep taking the medicine, but tell your doctor if they bother you or don’t go away:
- weight gain
- indigestion
- not able to sleep
- restlessness
- increased sweating
Also tell your doctor if any of these symptoms are severe or do not go away:
- headache
- dizziness
- difficulty falling asleep or staying asleep
- inappropriate happiness
- extreme changes in mood
- changes in personality
- bulging eyes
- acne
- thin, fragile skin
- red or purple blotches or lines under the skin
- slowed healing of cuts and bruises
- increased hair growth
- changes in the way fat is spread around the body
- extreme tiredness
- weak muscles
- irregular or absent menstrual periods
- decreased sexual desire
- heartburn
One of the numerous potential side–effects of prednisone and other forms of corticosteroid treatment is hirsutism — excessive growth of body hair. Patients vary in the degree to which this side–effect of steroids occurs. Although some experience minimal hirsutism, the patient depicted here developed this side effect after taking 10 milligrams of prednisone for a few months.
Weight Gain
Weight gain is usually the most dreaded side–effects of steroid use, incurred to some degree by nearly all patients who take them. The amount of weight gain varies from individual to individual. In addition to causing weight gain, prednisone leads to a redistribution of body fat to places that are undesirable, particularly the face, back of the neck, and abdomen. Accumulation of fat in the back of the neck is sometimes referred to as a “buffalo hump”. Supraclavical “fat pads” are collections of fat at the base of the neck, just above the collarbones, which are common in patients on steroids. They sometimes cause concern among patients if mistaken for lymph nodes or other causes for worry, but will gradually subside as the prednisone dose is tapered to below 10 milligrams/day.
Glucose Intolerance
High blood sugar, or steroid–induced diabetes. This usually resolves when the steroids are decreased or discontinued.
Hypertension
High blood pressure. This usually improves as the corticosteroid dose is reduced.
Increased Susceptibility to Infections
Patients are at increased risk for many types of infections, from minor fungal infections in the mouth (“thrush”, caused by Candida) to life–threatening infections such as Pneumocystis carinii pneumonia. The higher the steroid dose and the longer the duration of therapy, the greater the risk of infection. The risk is also increased when patients receive combinations of immunosuppressive medications, such as cyclophosphamide (cytoxan) and prednisone. The risk of some infections can be greatly reduced by taking specific types of antibiotics prophylactically.
Bone Thinning (Osteoporosis)
Prednisone may cause thinning of the bones even in people who are not usually at high risk for osteoporosis (for example: males, young people). In people susceptible to osteoporosis, prednisone may accelerate the process of bone loss. Fortunately, in the past few years, excellent treatments and preventive measures have become available for osteoporosis. All patients on prednisone for prolonged periods are candidates for these medicines.
Easy Bruising
Prednisone also causes “thin skin”. Patients on moderate to high doses of prednisone often notice that they bruise easily, even with only slight trauma.
Mood Swings/Insomnia
Many patients find it difficult to sleep when taking high doses of steroids. Many also find that they are more irritable than usual. Steroids sometimes even induce depression, which improves when the drug is decreased or discontinued.
Avascular Necrosis of Bone
For reasons that are not known, high dose prednisone (for example, greater than 20 milligrams a day) predisposes some patients to joint damage, most often of the hips. In avascular necrosis (or osteonecrosis, meaning “bone death”) of the hip, the part of the leg bone that inserts into the pelvis dies, resulting in pain with weight–bearing and some loss of joint function. Many patients with avascular necrosis require joint replacements.
Abdominal striae (“stripes”).
Cataracts
Long–term steroid use may lead to cataract development in the eyes, which frequently require surgical removal.
Acne
High dose prednisone predisposes some patients to acne, especially facial acne.
Serious side effects
You are more likely to have a serious side effect if you take a higher dose (more than 20mg daily) of prednisolone or if you have been taking it for more than a few weeks.
Tell a doctor straight away if you get:
- fever, chills, a very sore throat, ear or sinus pain, a cough, more saliva or a change in colour of saliva, pain with passing urine, mouth sores or a wound that will not heal – these can be signs of an infection
- sleepy or confused, feeling very thirsty or hungry, passing urine more often, flushing, breathing quickly or breath that smells like fruit – these can be signs of high blood sugar
- weight gain in the upper back or belly, moon face, very bad headaches and slow wound healing – these can be signs of Cushing’s syndrome
- a very upset stomach or vomiting, very bad dizziness or passing out, muscle weakness, feeling very tired, mood changes, loss of appetite and weight loss – these can be signs of adrenal gland problems
- muscle pain or weakness, muscle cramps, or a heartbeat that does not feel normal – these can be signs of low potassium levels
- severe stomach pain, severe back pain, severe upset stomach or vomiting – these can be signs of pancreas problems
You should also tell a doctor straight away if you get:
- breathless
- swelling in your arms or legs
- changes in your eyesight
- any bruising or bleeding that isn’t normal
- black poop
- black or dark brown vomit or vomiting blood
Serious allergic reaction
In rare cases, it’s possible to have a serious allergic reaction to prednisone. A serious allergic reaction is an emergency. Contact a doctor straight away if you think you or someone around you is having a serious allergic reaction.
The warning signs of a serious allergic reaction are:
- getting a skin rash that may include itchy, red, swollen, blistered or peeling skin
- wheezing
- tightness in the chest or throat
- having trouble breathing or talking
- swelling of the mouth, face, lips, tongue, or throat
These are not all the side effects of prednisone. For a full list see the leaflet inside your medicines packet.
Some side effects can be serious. If you experience any of the following symptoms, call your doctor immediately:
- vision problems
- eye pain, redness, or tearing
- sore throat, fever, chills, cough, or other signs of infection
- seizures
- depression
- loss of contact with reality
- confusion
- muscle twitching or tightening
- shaking of the hands that you cannot control
- numbness, burning, or tingling in the face, arms, legs, feet, or hands
- upset stomach
- vomiting
- lightheadedness
- irregular heartbeat
- sudden weight gain
- shortness of breath, especially during the night
- dry, hacking cough
- swelling or pain in the stomach
- swelling of the eyes, face, lips, tongue, throat, arms, hands, feet, ankles, or lower legs
- difficulty breathing or swallowing
- rash
- hives
- itching
Prednisone long term side effects
Taking prednisone for many months or years can have several harmful effects on your body. It can lead to:
- thinner bones (osteoporosis)
- poorly controlled diabetes
- eyesight problems
- slower growth in children and teenagers
If you have to take prednisone for a long time, there are steps you can take to stay as healthy as possible:
- Take regular exercise and make sure you get enough calcium in your diet to help strengthen your bones. Calcium-rich foods include milk, cheese and leafy greens. To check your bones, your doctor may arrange for you to have an occasional bone scan.
- If you have diabetes, you may need to check your blood glucose more often. Your doctor can advise you more about this.
- To reduce the chances of eyesight problems, visit an optometrist every 12 months to check for high pressure in your eye (glaucoma) and cataracts.
- Make sure that children and teenagers have their height monitored regularly by a doctor so that any stunting of growth can be picked up promptly.
Prednisone may slow growth and development in children. Your child’s doctor will watch his or her growth carefully. Talk to your child’s doctor about the risks of giving prednisone to your child.
Prednisone may increase the risk that you will develop osteoporosis. Talk to your doctor about the risks of taking prednisone and about things that you can do to decrease the chance that you will develop osteoporosis.
Some patients who took prednisone or similar medications developed a type of cancer called Kaposi’s sarcoma. Talk to your doctor about the risks of taking prednisone.
Prednisone may cause other side effects. Call your doctor if you have any unusual problems while you are taking this medication.
Stunted growth in children
Long periods of prednisone treatment can slow down the normal growth of children and teenagers.
Your child’s doctor will watch their growth carefully while they are taking steroids. That way any slowing of growth can be picked up promptly and treatment changed if necessary.
Talk to your doctor about the risks of giving prednisone to your child if you are concerned.
How to cope with side effects
What to do about:
- weight gain – try to eat a healthy balanced diet without increasing your portion sizes so you don’t gain too much weight. Regular exercise will also help to keep your weight stable.
- indigestion – take prednisone with food to reduce the chances of stomach problems. It may also help if you avoid rich or spicy food while you’re taking prednisone. If symptoms continue, ask your doctor if you may benefit from taking an additional medicine to protect your stomach.
Prednisone withdrawal
Don’t stop taking prednisone without talking to your doctor – you will need to reduce the dose gradually.
It can be dangerous to stop taking prednisone suddenly, especially if you have been on a high dose for a long time.
Your health condition may flare up again. You may also get withdrawal symptoms including:
- severe tiredness
- weakness
- body aches
- joint pain
Withdrawal problems are most likely to happen if you have taken prednisone for more than a few weeks or you take more than 40mg daily.
Your doctor will probably want to reduce your dose gradually over several weeks to prevent these side effects.