What is pruritus
Pruritus is a medical term for itch or itching. Pruritus (itching) refers to a unpleasant sensation of your skin that provokes the desire for you to rub or scratch the area to obtain relief. Pruritus can cause discomfort and frustration; in severe cases it can lead to disturbed sleep, anxiety and depression. Constant scratching to obtain relief can damage the skin (excoriation, lichenification) and reduce its effectiveness as a major protective barrier.
Itching is a normal body response to protect you from harmful external substances or parasites such as insect bites. However, pruritus (or itch) is a common and distressing symptom of many skin diseases, systemic illnesses and psychological disorders.
Pruritus is perhaps the commonest presenting symptom of skin disorders. In any two week period, 8-9% of the population suffer from significant pruritus. Pruritus lasting more than 6 weeks is called chronic pruritus. Pruritus may be localized to one area or generalized all over the skin.
Pruritus is often a symptom of an underlying disease process such as a skin problem, a systemic disease, or abnormal nerve impulses.
There are many possible causes of pruritus, but for some people with pruritus no obvious cause can be found.
Generalized pruritus without rash (especially in people over 65 years of age) is most commonly caused by dry skin.
Pruritus may also be caused by medicines or by internal diseases affecting the body.
Causes of pruritus of skin include:
- Skin conditions. Many skin conditions itch, including dry skin (xerosis), eczema (dermatitis), psoriasis, scabies, burns, scars, insect bites and hives.
- Internal diseases. Itchy skin can be a symptom of an underlying illness. These include liver disease, kidney failure, iron deficiency anemia, thyroid problems and certain cancers, including multiple myeloma and lymphoma.
- Nerve disorders. Conditions that affect the nervous system — such as multiple sclerosis, diabetes, pinched nerves and shingles (herpes zoster) — can cause itching.
- Psychiatric diseases. Examples of psychiatric diseases that can cause itchy skin are anxiety, obsessive-compulsive disorder and depression.
- Irritation and allergic reactions. Wool, chemicals, soaps and other substances can irritate the skin and cause itching. Sometimes the substance, such as poison ivy, parasites or cosmetics, causes an allergic reaction. Also, reactions to certain drugs, such as narcotic pain medications (opioids) can cause itchy skin.
- Pregnancy. During pregnancy, some women experience itchy skin.
There remain a small number of individuals with itch and no apparent underlying cause or rash. This is more common in the elderly. It is always important to look for an underlying causative condition, as the most effective management of pruritus without rash depends on the treatment of any underlying disease. The management of itch appears to be situation specific (e.g. iron deficiency), even if the underlying cause cannot be treated. The management of true pruritus of unknown cause is different again.
The epidemiology of pruritus depends on its underlying cause or causes. However, in general, the incidence of chronic pruritus increases with age, it is more common in women, and in those of Asian background.
The treatment of pruritus relies on establishing the cause and then either removing or treating the cause to prevent further itching. In many cases, tests are necessary to determine the cause; while these are in progress, treatment to provide symptomatic relief of pruritus may be given.
- Standard topical antipruritic agents: menthol and camphor (e.g., Sarna lotion), oatmeal baths (e.g., Aveeno), pramoxine (e.g., PrameGel), calamine lotion (Caladryl; use only on weeping lesions, not on dry skin), doxepin 5% cream (Zonalon)
- Topical antipruritic agents for refractory pruritus (e.g., severe atopic dermatitis): Burrow’s solution (wet dressings), Unna’s boot, tar emulsion
See your doctor or a skin disease specialist (dermatologist) if the itching:
- Lasts more than two weeks and doesn’t improve with self-care measures
- Is severe and distracts you from your daily routines or prevents you from sleeping
- Comes on suddenly and can’t be easily explained
- Affects your whole body
- Is accompanied by other signs and symptoms, such as extreme tiredness, weight loss, changes in bowel habits, or urinary frequency, fever or redness of the skin
If the condition persists for three months despite treatment, see a dermatologist to be evaluated for skin disease and an internist to be evaluated for other diseases.
Can pruritus be cured?
When pruritus is a symptom of an internal disorder, treatment of this will sometimes lead to resolution of itch. Stopping a causative drug can lead to resolution of pruritus. Treating dry skin can improve pruritus but the treatment will need to be ongoing.
Pruritus ani
Pruritus ani is itching around the opening of the back passage (the anus). It is a symptom with many causes, but sometimes no obvious cause can be found. Pruritus ani is common and occurs more often in men than women. It is seldom due to an underlying serious condition and those who have pruritus ani are usually otherwise well.
Can pruritus ani be cured?
As there are so many different causes of pruritus ani, there is no one treatment that can cure all cases. It is important to have a correct diagnosis to ensure the right treatment can be implemented to relieve the symptom of itching.
Is pruritus ani hereditary?
No.
Pruritus ani causes
Pruritus ani has many possible causes, so it is sensible to seek the advice of your doctor if you experience itching around the anus.
Some of the more common causes pruritus ani are:
- Anal disease. The contents of the bowel contain digestive enzymes that can irritate the skin and cause itching. Minor leakages of bowel motions, and a failure to remove them completely from the skin around the anus when wiping, can lead to pruritus ani. One contributory factor may be the presence of piles (hemorrhoids), which are the result of build-up of pressure on the blood vessels of the anal area. Constipation (not opening the bowels regularly) can make the piles and pruritus ani worse. Skin tags (small skin growths) in the anal area can also contribute to itching.
- Skin disease around the back passage. Examples of this include psoriasis, eczema, dermatitis, thrush (a Candida yeast infection), and fungal infections.
- Threadworms or pinworms (Enterobius vermicularis) are small roundworms that live in the lower digestive tract of humans. In children, itching around the back passage is often due to threadworms, which can cause pruritus ani in adults too. The itching is usually worse at night.
- Allergy. Pruritus ani may be due to an allergy to something in contact with the skin, for instance to fragrance in toilet paper, or to local anesthetics or preservatives in creams used for piles.
- Skin irritation. The skin of the bottom is sensitive and can easily be irritated by moist tissue wipes, soaps, perfumes, antiseptics (for example, Dettol). These make the skin sore and itchy, and contribute to pruritus ani.
- Sweating. The skin around the back passage is often moist with sweat. If long periods pass without ventilation to the area, for instance if you sit down for a long time or wear tight underwear, the skin can be irritated further and become itchy.
The anal skin is exposed to irritating digestive products which may result in a rash (irritant dermatitis). The rash is made worse by:
- Frequent stools (diarrhea)
- Straining at stool (constipation)
- Scratching
- Vigorous use of toilet tissue
- Scrubbing with soap and water
- Acidic or spicy foods.
Pruritus ani symptoms
Itching is the main symptom, often occurring after the bowels have opened. Itching may be experienced during the night interfering with sleep. Sometimes the skin becomes sore and can crack or ‘fissure’ after scratching, making it uncomfortable to open your bowels.
What does pruritus ani look like?
The skin around the anus may look inflamed and thickened, and show scratch marks. Small fissures may occur and these may feel painful and sensitive, and bleed.
Pruritus ani diagnosis
It is usually possible to make a diagnosis of pruritus ani by hearing your story and examining the affected skin. Your doctor will want to find out why you have pruritus ani, and may need to examine you for threadworms, allergies etc. The tests selected will depend on the clues offered by your story and the examination of the skin around the anus.
Pruritus ani treatment
The first step will be to find out if any of the causes listed above are playing a part in causing your pruritus ani. If they are, then your doctor will treat them appropriately.
If no obvious cause can be found, your doctor may suggest a variety of ways of helping your pruritus ani such as:
- A short course of a steroid ointment or cream to be applied every day to the area to reduce the itching. This can then be used as and when needed should pruritus ani return.
- A course of antihistamine may be prescribed by your doctor to relieve itching.
- It is important to remove all irritants such as bowel motions or soap from the skin creases. An emollient cream, such as aqueous cream, should be used instead of soap for washing the area to avoid the irritating effect of soap and detergents. Cotton wool balls with warm water are gentler than toilet paper and more effective in cleaning fissures and skin creases. It is important to ensure no little bits of toilet paper or cotton wool are left in the area as this will cause more irritation. The area also should be rinsed thoroughly after you have opened your bowels.
- If you have troublesome constipation, you should see your doctor for advice.
Pruritus ani self care
- You should avoid any of the things listed above that might be contributing to your pruritus ani. If you notice that a particular food makes the itching worse, avoid it.
- Scratch as little as possible, as scratching keeps the itch going.
- Open your bowels regularly. Try not to delay going to the toilet when you have the urge to do so.
- Keep your stools soft so you do not have to strain to open your bowels. Eat plenty of fruit, vegetables and other roughage, and drink plenty of water.
- The use of a bidet or a shower jet helps to remove particles of bowel motion that have become trapped near the anus. Always dry the skin gently, without rubbing it.
- Keep the area as well ventilated as possible. Underwear should be loose and made of cotton not synthetic materials. Avoid prolonged sitting.
- Avoid getting too hot in bed at night and avoid wearing underwear in bed.
Pruritus causes
Causes of pruritus can be classified under 5 main headings.
Localized pruritus
Localized pruritus is pruritus that is confined to a certain part of your body. It can occur in association with a primary rash (e.g. dermatitis) or may occur because of hypersensitive nerves in the skin (neuropathic pruritus). Neuropathic pruritus is due to compression or degeneration of nerves in the skin, on route to the spine or in the spine itself. Neuropathic itch is sometimes associated with reduced or absent sweating in the affected area of skin.
Typical causes of localized itchy rashes:
- Scalp: seborrheic dermatitis, head lice
- Back: Grover disease
- Hands: pompholyx, irritant and/or allergic contact dermatitis
- Genitals: vulvovaginal Candida albicans infection, lichen sclerosus
- Legs: venous eczema
- Feet: tinea pedis
Neuropathic causes of localized pruritus without primary rash:
- Face: trigeminal trophic syndrome
- Hand: cheiralgia paraesthetica
- Arm: brachioradial pruritus
- Back: notalgia paraesthetica
- Genital: pruritus vulvae, pruritus ani
- Dermatomal: herpes zoster (shingles) during recovery phase
Scratching a localized itch may lead to lichen simplex, prurigo or prurigo nodularis.
Systemic causes of pruritus
Sytemic diseases may cause generalized pruritus. There is nothing wrong with the skin itself, at least until it’s been scratched. Pruritus can be an important dermatologic clue to the presence of significant underlying disease in 10 to 50 percent of older adults 1. This is sometimes called metabolic itch. Systemic causes must be considered, especially in elderly patients in whom pruritus is persistent and refractory to xerosis management and other nonspecific therapies 2.
In up to 30 percent of patients, the diagnosis of Hodgkin’s lymphoma is preceded by intense, chronic, generalized pruritus 3. Pruritus also may be a presenting feature in patients with cutaneous T-cell lymphoma 4. Patients with human immunodeficiency virus (HIV) infection commonly have itching, which is most often considered secondary to comorbid dermatologic conditions such as xerosis, seborrheic dermatitis, candidiasis, psoriasis, scabies, or eosinophilic folliculitis 5. Uremia causes severe paroxysms of pruritus (especially during the summer) in 25 percent of patients with chronic renal failure and 86 percent of patients who are receiving hemodialysis 6.
Along with uremia, cholestasis is responsible for some of the most intense itching. Cholestasis-related pruritus is most severe at night, with a predilection for the hands and feet. Hyperpigmentation may result in areas of heavy scratching. In patients with hyperpigmentation, the middle of the back is spared, resulting in a classic butterfly-shaped dermatitis 7. Cholestasis may be caused by numerous medications, including oral contraceptive pills, erythromycin, amoxicillin–clavulanate potassium (Augmentin), phenothiazines, and anabolic steroids.
Cholestasis affects as many as 0.5 percent of pregnant women, particularly during the third trimester. Overall, itching is common in pregnancy, occurring in up to 14 percent of women 8. Pregnancy-specific causes of pruritus are listed in Table 1.
Metabolic disorders include chronic renal failure (dialysis) and liver disease (with or without cholestasis):
- Uremic pruritus arises in patients undergoing dialysis is due to a combination of xerosis (dry skin), secondary hyperparathyroidism, peripheral neuropathy (nerve changes) and inflammation.
- Secondary hyperparathyroidism which also occurs in dialysis patients leads to microprecipitation (deposition) of calcium and magnesium salts in the skin, triggering mast cell degeneration, releasing serotonin and histamine.
- Once chronic pruritus has occurred, there may be secondary changes in the nerves in the skin and central nervous system which heighten the sensation of itch.
- Severe paroxysms of generalized itching, worse in summer.
- Hepatogenic pruritus is more common in intrahepatic than extrahepatic cholestasis. Examples of intrahepatic cholestasis is associated with chronic viral hepatitis, primary biliary cirrhosis, pregnancy-related cholestasis. Extra-hepatic cholestasis is associated with pressure on the bile ducts, e.g. from pancreatic tumors or pseudocysts.
- Cholestasis is thought to release toxic substances from the liver, which stimulates neural itch fibers in the skin 9. Intense itching (hands, feet, pressure sites) that becomes worse at night. Reactive hyperpigmentation that spares the middle of the back (butterfly-shaped dermatitis).
- Characteristically, cholestatic pruritus is most severe at night; it tends to affect the hands, feet and areas where clothes are rubbing on the skin.
Hematological disorders include iron deficiency anemia and polycythemia vera:
- Generalized pruritus along with glossitis (tongue inflammation) and angular cheilitis (inflammation of mouth corners) are seen in iron deficiency anemia 10.
- In polycythaemia vera, itch is usually precipitated by contact with water (aquagenic pruritus), e.g. after a shower 11. Pricking-type itch persisting for hours after hot shower or bath. This is thought to be mediated by the effect of platelets, serotonin and prostaglandins.
Endocrine disorders include thyroid disease and diabetes mellitus:
- In Graves’ disease (thyrotoxicosis or hyperthyroidism), increased blood flow, skin temperature and decreased itch threshold mediated by the increase in thyroid hormones, lead to the itch 12. Warm, moist skin; possibly, pretibial edema. Associated conditions: onycholysis, hyperpigmentation, vitiligo. Pruritus associated with myxoedema and hypothyroidism is rare, and if present, is more likely the result of xerosis (dry skin).
- In diabetes mellitus, localized itch tends to occur in the perianal/genital region usually due to Candida albicans or dermatophyte infections. It is unclear if metabolic abnormalities such as renal impairment, autonomic failure or diabetic neuropathy contribute to this.
Paraneoplastic itch is associated with lymphoma, especially Hodgkin lymphoma, leukemia or a solid organ tumor (e.g., lung, colon, brain):
- In Hodgkin lymphoma, pruritus is thought to be caused by histamine release, which may be related to eosinophilia 3. Prolonged generalized pruritus often preceding diagnosis.
- Malignant carcinoid. Intermittent head and neck flushing with explosive diarrhea.
- Multiple myeloma: In elderly patients: bone pain, headache, cachexia, anemia, renal failure.
Infections causing itch include human immunodeficiency virus infection (HIV) and hepatitis C virus:
- Patients with HIV (human immunodeficiency virus) commonly complain of itch 5. A common presenting symptom resulting from secondary causes (eczema, drug reaction, eosinophilic folliculitis, seborrhea). This may be associated with skin infections/infestations, dry skin, drug reactions, hyperoesinophilia (increased eosinophil levels) and cutaneous T cell lymphoma. There is a possible correlation between intractable pruritus and increased HIV viral load.
- In chronic hepatitis C infection, the mechanisms responsible for itch remain unclear. In the absence of cholestasis, pruritus may be related to antiviral therapy; it has been noted to occur in patients treated with combination therapy (interferon alfa and ribavirin).
Neurodermatitis or neurotic excoriations 13: Bouts of intense itching that may awaken patients from sound sleep. Involvement of scalp, neck, wrist, extensor elbow, outer leg, ankle, and perineum.
Delusions of parasitosis: Focal erosions on exposed areas of arms and legs.
Parasitic infections: Usually in returning travelers or immigrants
- Filariasis: Tropical parasite responsible for lymphedema
- Schistosomiasis: Freshwater exposure in Africa, the Mediterranean area, or South America
- Onchocerciasis: Transmitted by black fly in Africa or Latin America
- Trichinosis: Ingestion of undercooked pork, bear, wild boar, or walrus meat
Parvovirus B19 infection: “Slapped cheek” appearance in children; arthritis in some adults.
Peripheral neuropathy
- Brachioradial pruritus: Involvement of lateral arm in white patients who have traveled to the tropics 14
- Herpes zoster: Pruritus accompanying painful prodrome two days before appearance of rash
- Notalgia paresthetica: Pruritus in middle of back with hyperpigmented patch 7
Scleroderma: Nonpitting extremity edema, erythema, and intense pruritus. Edema phase with pruritus occurring before fibrosis of skin
Urticaria: Response to allergen, cold, heat, exercise, sunlight, or direct pressure
Weight loss (rapid) in eating disorders 15: Signs in addition to pruritus: hair loss, fine lanugo hair on back and cheeks, yellow skin discoloration, petechiae.
Table 1. Causes of Pruritus in Pregnancy
| Cause | Features |
|---|---|
Pruritic urticarial papules and plaques of pregnancy (common in third trimester) | Intense pruritus involving abdomen, with spread to thighs, buttocks, breasts, and arms |
Prurigo of pregnancy (common in second half of pregnancy) | Associated with atopic dermatitis |
Excoriated papules and nodules on extensor arms and abdomen | |
Herpes gestationis or pemphigoid gestationis (uncommon) | Autoimmune condition associated with Graves’ disease |
Vesicles and bullae on abdomen and extremities in second half of pregnancy | |
Responsive to prednisone (dosage: 20 to 40 mg per day) 16 | |
Intrahepatic cholestasis of pregnancy (uncommon) | Trunk and extremity itching without rash in late pregnancy |
No jaundice in mild form | |
Responsive to cholestyramine (Questran) and vitamin K1 17 | |
Pruritic folliculitis of pregnancy (uncommon, occurs in second half of pregnancy) | Erythematous follicular papules over trunk, with spread to extremities |
Possibly a variant of prurigo of pregnancy | |
Other common pruritic conditions exacerbated in pregnancy | Atopic dermatitis, allergic contact dermatitis |
Pruritic skin diseases
Pruritus is most frequently a symptom of many skin diseases. Some of these are included in the following list.
- Allergic contact dermatitis: Sharply demarcated erythematous lesion with overlying vesicles. Reaction within two to seven days of exposure.
- Dry skin (xerosis or asteatotic eczema) is common in older adults. The itch of dry skin, otherwise known as xerosis or asteatotic eczema, is common in older adults 19. Xerosis occurs most often during the winter in northern climates.
- Urticaria
- Psoriasis: Plaques on extensor extremities, low back, palms, soles, and scalp.
- Atopic dermatitis: “Itch that rashes (when scratched)” in patients with atopic conditions (e.g., allergic rhinitis, asthma). Involvement of flexor wrists and ankles, as well as antecubital and popliteal fossae
- Folliculitis: Pruritus out of proportion to appearance of dermatitis. Papules and pustules at follicular sites on chest, back, or thigh.
- Dermatitis herpetiformis: Rare vesicular dermatitis affecting lumbosacral spine, elbows, or knees.
- Lichen simplex
- Lichen planus: Lesions often located on the flexor wrists “6Ps”: pruritus, polygonal, planar, purple papules, and plaques.
- Bullous pemphigoid: Initially pruritic urticarial lesions, often in intertriginous areas. Formation of tense blisters after urticaria.
- Pediculosis (lice infestation): Occiput of school-aged children; genitalia in adults (sexually transmitted disease).
- Scabies: Burrows in hand web spaces, axillae, and genitalia. Hyperkeratotic plaques, pruritic papules, or scales. Face and scalp affected in children but not in adults.
- Miliaria
- Sunburn teroidal: Possible photosensitizing cause (e.g., nonsteroidal anti-inflammatory drugs, cosmetics).
- Pityriasis rosea
- Mycosis fungoides (cutaneous T-cell lymphomas): Oval eczematous patch on skin with no sun exposure (e.g., buttocks). Possible presentation as new eczematous dermatitis in older adults. Possible presentation as erythroderma (exfoliative dermatitis).
- Xerotic eczema: Intense itching in elderly patients (often during winter months in northern climates). Involvement of back, flank, abdomen, waist, and distal extremities.
Atopic dermatitis can result in severe pruritus and is often described as “the itch that rashes (when scratched).” Atopic dermatitis affects 10 percent of children and often develops before six months of age 20. Atopic dermatitis often persists into adulthood and may be exacerbated during pregnancy. Patients with atopic dermatitis usually have a family history of asthma and allergic rhinitis.
In infants with atopic dermatitis, eczema usually involves the face, scalp, trunk, extensor arms, and legs. Older children and adults experience “hot and sweaty fossae and folds” involving flexor surfaces such as the antecubital and popliteal fossae, as well as the flexor wrists and ankles 21. Adults also may develop atopic dermatitis of the hands, upper eyelids, and anogenital region.
Pruritus may arise as a result of exposure to certain external factors.
- Allergens or irritants:
- Cosmetics, black hair dye
- Latex
- Laundry detergents, fabric softeners
- Nickel
- Ointments that are highly concentrated in inert oil
- Paint-on tattoos (paraphenylenediamine), tattoo dye (cadmium yellow, mercuric sulfide [red])
- Rhus oil (e.g., poison ivy)
- Topical medications: benzocaine (Americaine), neomycin
- Cold, which can cause ‘winter itch’
- Heat exposure 8:
- Cholinergic urticaria (response to hot bath, fever, exercise)
- Miliaria rubra (prickly heat)
- Occupational exposure 22:
- Fiberglass
- Glyceryl monothioglycolate (in permanent-wave solution)
- Methyl methacrylate (e.g., Plexiglas)
- Potassium dichromate in cements and dyes
- Rosins or epoxy resins in adhesives
- Rubber
- A physical urticaria, such as dermographism
- Aquagenic pruritus (itch on exposure to water). Aquagenic pruritus (associated with polycythemia vera, itching within 15 minutes of any water contact) 23:
- Cholinergic urticaria (response to warm water)
- Polycythemia vera
- Swimmer’s itch (seven-day eruption after freshwater swimming)
- Insects and infestations, e.g. scabies
- Medications (topical or systemic) 8:
- Antifungal agents: fluconazole (Diflucan), itraconazole (Sporanox), ketoconazole (Nizoral)
- Aspirin
- B vitamins, including niacinamide
- Drug hypersensitivity: rifampin (Rifadin), vancomycin (Vancocin)
- Nitrates (food preservatives)
- Opioids
- Quinidine
- Spinal narcotics (pruritus affecting face, neck, and upper chest)
Allergic contact dermatitis
A careful history is important in patients with allergic contact dermatitis, another common cause of pruritus. Allergic contact dermatitis may be caused by exposure to substances such as nickel, latex, cosmetics, rhus oils (e.g., poison ivy), and topical medications such as benzocaine (Americaine) and neomycin 22. Like xerosis and atopic dermatitis, allergic contact dermatitis is an eczematous reaction, but the reaction is localized to allergen-exposed areas. It can be difficult to distinguish allergic contact dermatitis from irritant contact dermatitis, which is often a reaction to the frequent use of concentrated organic solvent or soap. However, allergic contact dermatitis tends to develop rapidly, and the lesions have more distinct borders than those of irritant contact dermatitis.
Hormonal reasons for pruritus
About 2% of pregnant women have pruritus without any obvious dermatological cause. In some cases the itch is due to cholestasis (pooling of bile in the gall bladder and liver). It usually occurs in the 3rd trimester and is relieved after giving birth.
Generalized itch is also a common symptom of menopause.
Mechanisms underlying pruritus
Pruritus or itch, like pain, can originate anywhere along the neural itch pathway, from the central nervous system (brain and spinal cord) to the peripheral nervous system and the skin. The way scratching stops itching has been explained by an interaction with pain pathways within the dorsal horn of the spinal cord.
Mechanisms underlying pruritus are complex:
- The itch signal is transmitted mainly through small, itch-selective C-fibres in the skin in addition to histamine-triggered and non-histaminergic neurons.
- These connect with secondary neurons which cross the opposite side of the spinothalamic tract and ascend to parts of the brain involved in sensation, emotion, reward and memory. These areas overlap with those activated by pain.
- Patients with chronic pruritus usually have both peripheral and central hypersensitization (heightened reaction) which means they tend to overreact to noxious stimuli which normally inhibit itch (such as heat and scratching) and also misinterpret non-noxious stimuli as an itch (e.g., light touch)
Pruritus originates within the skin’s free nerve endings, which are most heavily concentrated in the wrists and ankles. The sensation of pruritus is transmitted through C fibers to the dorsal horn of the spinal cord and then to the cerebral cortex via the spinothalamic tract 24. Pruritus generates a spinal reflex response, the scratch, which is as innate as a deep tendon reflex 7. Regardless of the cause, pruritus often is exacerbated by skin inflammation, dry or hot ambient conditions, skin vasodilation, and psychologic stressors 25.
A single mechanism cannot explain all causes of pruritus. Histamine, which is released by mast cells in persons with urticaria and other allergic reactions, classically is associated with pruritus. However, with the exception of allergic conditions, histamine must be considered only one of several chemical mediators of itch.
Serotonin appears to be a key component of the pruritus that occurs with several diseases, including polycythemia vera, uremia, cholestasis and lymphoma, and of morphine-associated pruritus. Serotonin inhibitors such as cyproheptadine (Periactin), pizotifen, paroxetine (Paxil), and ondansetron (Zofran) have proved effective in treating several of these pruritic conditions 7.
Opioids trigger pruritus in as many as 90 percent of patients receiving intraspinal injections of narcotics. Intravenous and intradermal opioid injections also may induce itching.2 Narcotic antagonists have been used successfully to relieve pruritus in patients with cholestasis 26.
The pruritus that occurs in herpes zoster prodrome may be a model for pruritus with a neuropathic cause. Certain idiopathic types of localized pruritus have been attributed to peripheral neuropathy. Brachioradial pruritus is an uncommon condition that presents as lateral arm pruritus and has been associated with spinal disease. Similarly, notalgia paresthetica is thought to be of neuropathic origin, with pruritus limited to the middle of the back. Severe pruritus also has been observed in patients with spinal tumors and multiple sclerosis 7.
Atopic dermatitis appears to involve an immune-mediated release of cytokines and other pro-inflammatory agents, a mechanism analogous to airway hyperreactivity in patients with asthma 20. Superimposed on this hyperreactivity is a distorted touch sensation. Although patients without atopic dermatitis perceive mild mechanical stimulation as touch, patients with the condition perceive it as pruritus 21.
Pruritus symptoms
You may have itchy skin over certain small areas, such as on an arm or leg, or over your whole body. Itchy skin can occur without any other noticeable changes on the skin. Or it may be associated with:
- Redness
- Bumps, spots or blisters
- Dry, cracked skin
- Leathery or scaly skin
Sometimes itchiness lasts a long time and can be intense. As you rub or scratch the area, it gets itchier. And the more it itches, the more you scratch. Breaking this itch-scratch cycle can be difficult.
Persistent scratching over a period of time may lead to:
- Lichenification (thickened skin, lichen simplex)
- Prurigo papules and nodules.
There are no specific skin signs associated with pruritus, apart from scratch marks (excoriations) and signs of the underlying condition.
Pruritus complications
Itchy skin that lasts more than six weeks (chronic pruritus) can affect the quality of your life, for example, by interrupting your sleep and causing anxiety or depression. Insomnia, which is a common concern for many older adults, is further exacerbated by pruritus. Lack of sleep may significantly affect quality of life; it can also increase the risk of accidents and injuries, and result in a worsening of comorbid conditions 27.
Complications arise when pruritus is accompanied by intense scratching. Lichen simplex chronicus is a localized skin thickening, often appearing over the posterior neck, extremities, scrotum, vulva, anus, and buttocks. In prurigo nodularis, a variant of lichen simplex chronicus, 10- to 20-mm nodules develop over areas within easy scratching reach, such as the extensor arms and legs 8. Prurigo nodularis has been successfully treated with a cream containing 0.025 percent capsaicin (Zostrix) applied topically four to six times per day for two to eight weeks) 28. Impetigo may result from superinfected excoriations, as commonly occur in patients with atopic dermatitis 29.
Pruritus diagnosis
The first steps of evaluation of an itchy patient are medical history and examination.
A thorough history can identify constitutional symptoms that may point towards an underlying systemic disease. Drug triggers such as opioids may be identified, especially if the commencement of the drug relates to the itch.
A careful examination can identify dermatological causes for the itch (eg scabies, lichen simplex, pemphigoid) or evidence of chronic skin changes related to the itch. In dermatological causes of pruritus, primary skin lesions will usually suggest the diagnosis. Patients without primary skin lesions and little evidence of chronic scratching should be investigated for systemic, neuropathic and psychogenic causes.
The panel of investigations could include:
- Full/complete blood count. A complete blood count can provide evidence of an internal condition causing your itch, such as iron deficiency.
- Creatinine and renal function tests
- Liver function tests
- Thyroid function tests. Thyroid abnormalities such as hyperthyroidism, may cause pruritus.
- Erythrocyte sedimentation rate (ESR)
- Chest radiography. A chest X-ray can show if you have enlarged lymph nodes, which can go along with pruritus of skin.
- HIV serology.
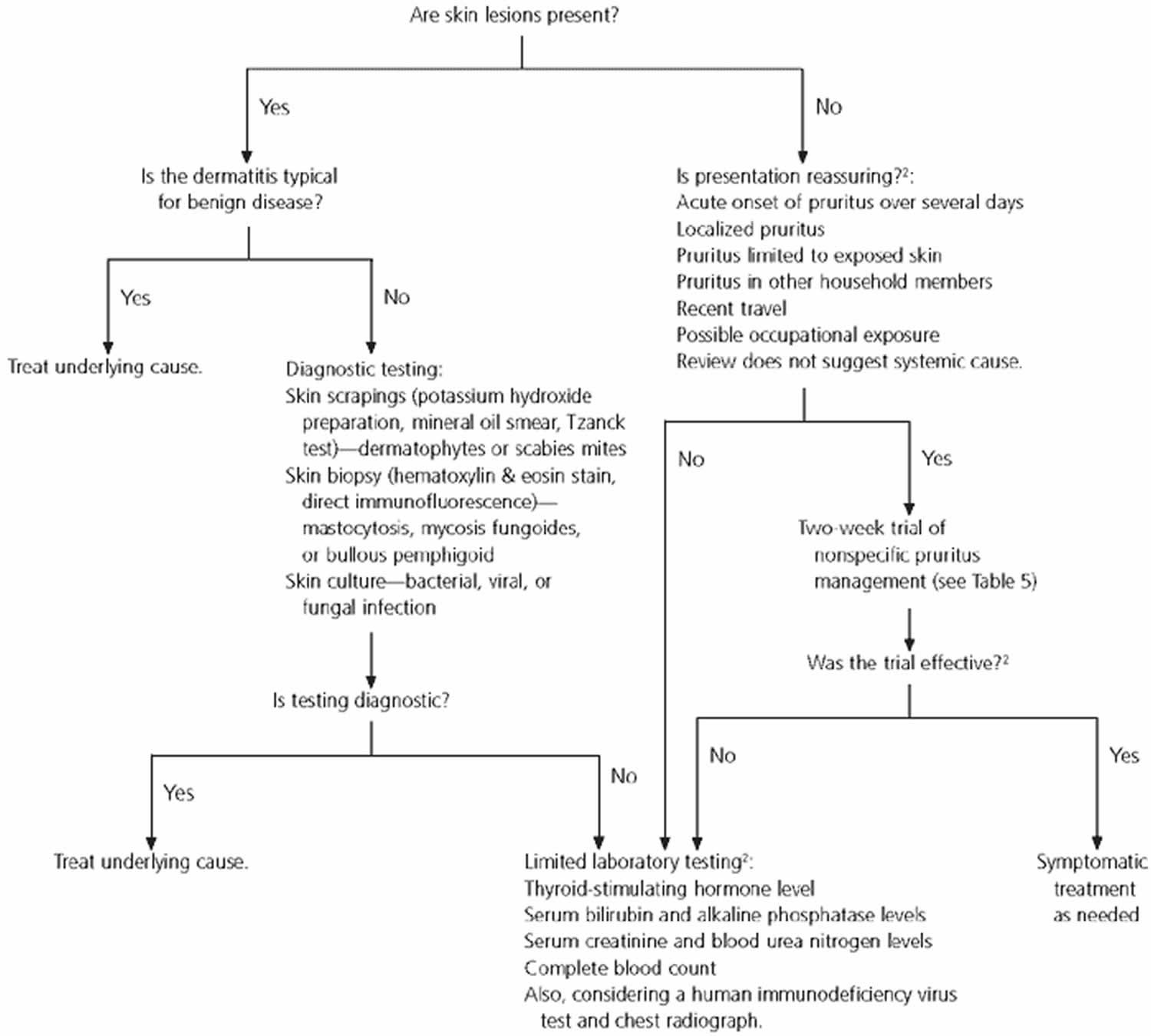
Figure 1. Algorithm for the evaluation of pruritus
[Source 18 ]Pruritus treatment
The management of pruritus relies on establishing the cause and then either removing or treating the cause to prevent further itching. In many cases, tests are necessary to determine the cause; while these are in progress, treatment to provide symptomatic relief of pruritus may be given.
Topical treatments
In addition to specific therapy for any underlying skin or internal disease, topical treatment may include:
- Wet dressings or tepid shower to cool the skin
- Calamine lotion (contains phenol, which cools the skin): avoid on dry skin and limit use to a few days
- Menthol/camphor lotion: gives a chilling sensation
- Local anesthetics, such as pramoxine (also called pramocaine), applied to small itchy spots such as insect bites
- Regular use of emollients, especially if skin is dry
- Mild topical corticosteroids for short periods
- Topical calcineurin inhibitors are also used to reduce itch associated with inflammatory skin conditions
- Topical doxepin, a tricyclic antidepressant and antihistamine, is an antipruritic used in eczema.
Other measures that can be useful in preventing pruritus include avoiding precipitating factors such as rough clothing or fabrics, overheating, and vasodilators if they provoke itching (eg, caffeine, alcohol, spices). Fingernails should be kept short and clean. If the urge to scratch is irresistible then rub the area with your palm.
Topical antihistamines should not be used for chronic itch, as they may sensitise the skin and result in allergic contact dermatitis.
Moisturizers (emollients)
These should be applied several times every day to help the outer layer of your skin function better as a barrier to the outside world. The drier your skin, the more frequently you should apply a moisturizer. There are many different types of moisturizers varying in their degree of greasiness, and it is important that you choose one you like to use. The best one to use is the greasiest one you are prepared to apply.
Aqueous cream was originally developed as a soap substitute. It is often used as a moisturizer but can irritate the skin in some people and make itching worse.
Anti-itch creams
Some creams containing anti-itch agents in addition to their moisturizing effect can be bought over the counter, such as creams containing crotamiton or lauromacrogols). Your doctor may prescribe other creams such as doxepin cream, which has antihistamine action when applied in cream form.
Topical steroid creams or ointments
These will usually settle the redness and itching when there is an active inflammatory skin condition.
Systemic therapy
If pruritus is severe and sleep is disturbed, then treatment with oral medication may be necessary. Some drugs may help to relieve the itch whilst others are given solely for their sedative effects.
- Antihistamines are most useful in urticaria, in which histamine is released. Use for other pruritic conditions is not supported by randomised control trials. Sedating antihistamines may be used for their sedative effects.
- Systemic antipruritic agents (used in allergic and urticarial disease) such as doxepin and amitriptyline are tricyclic antidepressants have antipruritic action and act on the central and peripheral nervous systems. Doxepin (Sinequan), 10 to 25 mg at bedtime4; hydroxyzine (Atarax), 25 to 100 mg at bedtime; nonsedating antihistamines (e.g., fexofenadine [Allegra]) 30
- Tetracyclic antidepressants such as mirtazepine and selective serotonin reuptake inhibitors (paroxetine, sertraline, fluoxetine) may also help some patients with severe itch including when it is caused by cholestasis, T-cell lymphoma, malignancy or a neuropathic condition.
- Anti-epileptic drugs such as sodium valproate, gabapentin and pregabalin may also be of benefit to some patients, e.g., those with itch associated with renal failure or neuropathic itch. The mechanism of action is uncertain.
- Opioid antagonists such as butorphanol intranasal spray, naltrexone tablets, and naloxone have been effective in patients suffering from intractable pruritus in association with liver disease, atopic eczema and chronic urticaria. Nalfurafine, which is a kappa-opioid agonist has also been studied and shown to reduce itch associated with chronic renal impairment, however it is not widely available.
- Aspirin is sometimes effective if pruritus is mediated by kinins or prostaglandins and is noted to be effective in patients with pruritus due to polycythaemia vera. Note: aspirin may cause or aggravate itch in some patients.
- Thalidomide has been successful in treating nodular prurigo and chronic pruritus of various kinds but is rarely used because of serious adverse effects and expense.
- Rifampicin is effective for patients with pruritus associated with cholestasis (some forms of liver disease).
- Isolated case reports in severe itch associated with malignancy have reported success with the NKR1 antagonist, aprepitant (normally used short-term for postoperative or chemotherapy-induced nausea). This is under investigation for neuropathic itch and nodular prurigo.
Antihistamines
An antihistamine tablet or syrup can help to improve some causes of pruritus. Non-sedating antihistamines may be of help in some patients. Sedating antihistamines (those that make you drowsy) are no longer generally recommended in managing itch or pruritus; this includes those that can be purchased without prescription, such as chlorpheniramine.
Some antidepressant tablets, prescribed by your doctor, taken at night can help you sleep if it is disturbed by itching.
Phototherapy
Ultraviolet light treatment, given in the hospital can help to reduce pruritus or the itch/scratch cycle. Broadband ultraviolet B or narrow-band UVB phototherapy alone, or in conjunction with UVA, has been shown to be helpful for pruritus associated with chronic kidney disease, psoriasis, atopic eczema and cutaneous T-cell lymphoma.
Behavioral therapy
Behavioural therapy may be used in conjunction with pharmacotherapy to modify behaviors such as coping mechanisms and stress reduction, which help interrupt the itch-scratch cycle. One randomized controlled trial showed short-term benefits in reduction in itch frequency and scratching as well as improvement in coping mechanisms.
Reversing habits
Pruritus can lead to a cycle of itching and scratching that can develop into a habit and be very hard to break. Identifying the times of day and the activities when scratching occurs most, may help you change your behavior.
Self care
Anything you can do to take your mind off the itching will help to reduce or stop the scratching.
- Humidify dry indoor environment, especially in winter.
- Try to avoid situations where you tend to scratch by changing your habits.
- Try patting the skin instead of scratching.
- Avoid soaking in baths for long periods as hot water may remove the natural oils from your skin.
- Decrease frequency of bathing and limit bathing to brief exposure to tepid water; after bathing, briefly pat skin dry and immediately apply skin lubricant. Bathe or shower quickly in tepid (not hot) water no more than once daily.
- Avoid using soaps or foaming body washes even if they claim to be good for dry itchy skin. Many of these contain detergents which remove natural oil from the skin.
- Use mild, unscented, hypoallergenic soap two to three times per week; limit daily use of soap to groin and axillae (spare legs, arms, and torso).
- You may find that laying a cool flannel soaked in moisturizing cream on the skin can reduce the feeling of itch. A cooled emollient (moisturizer) which has been kept in the refrigerator may also help.
- Keep your bedroom cool and do not sleep with heavy or heat retaining bedclothes. If you are hot and itchy during the day a fan can help to cool the skin down.
- Emollients (moisturizers). Use skin lubricants liberally. People with pruritus usually have dry skin, and therefore emollients may help to moisturize dry skin. They ease itching, reduce scaling, soften cracked areas and help the penetration of other topical treatments. There is a wide range of moisturizers available from pharmacists and supermarkets. There is usually no advantage in buying expensive moisturizers. Petrolatum or lubricant cream at bedtime; alcohol-free, hypoallergenic lotions frequently during the day.
- Choose clothing that does not irritate the skin (preferably made of doubly rinsed cotton or silk); avoid clothing made of wool, smooth-textured cotton, or heat-retaining material (synthetic fabrics); when washing sheets, add bath oil (e.g., Alpha Keri) to rinse cycle.
- Avoid use of vasodilators (caffeine, alcohol, spices, hot water) and excessive sweating.
- Avoid use of provocative topical medications, such as corticosteroids for prolonged periods (risk of skin atrophy) and topical anesthetics and antihistamines (may sensitize exposed skin and increase risk of allergic contact dermatitis).
- Prevent complications of scratching by keeping fingernails short and clean, and by rubbing skin with the palms of the hands if urge to scratch is irresistible.
Treatment of systemic causes
Management of pruritus should be directed at the underlying cause. In patients with pruritus that has a systemic cause (e.g., hyperthyroidism, iron deficiency anemia, Hodgkin’s lymphoma, HIV infection), itching gradually recedes as the primary condition improves. Although a full discussion of treatment is beyond the scope of this article, specific management strategies for uremic and cholestatic pruritus, as well as other systemic pruritic conditions, are included in Table 2.
Table 2. Specific Management of Pruritic Conditions
Cholestasis |
Cholestyramine (Questran), 4 to 6 g orally 30 minutes before meals |
Ursodiol acid (Actigall), 13 to 15 mg per kg per day orally |
Ondansetron (Zofran), 4 to 8 mg IV, then 4 mg orally every eight hours |
Opiate receptor antagonist such as nalmefene (Revex), 20 mg orally two times per day |
Rifampin (Rifadin), 300 mg orally twice daily |
Bile duct stenting for extrahepatic cholestasis |
Bright-light therapy |
Neurotic excoriation |
Pimozide (Orap) orally for delusions of parasitosis |
Selective serotonin reuptake inhibitor (e.g., fluvoxamine [Luvox], fluoxetine [Prozac], paroxetine [Paxil]) |
Notalgia paresthetica |
Capsaicin 0.025% cream (Zostrix) applied to localized areas four to six times daily for several weeks |
Polycythemia vera |
Aspirin, 500 mg orally every eight to 24 hours |
Paroxetine (Paxil), 10 to 20 mg orally per day |
Interferon alfa, 3 to 35 million IU per week |
Spinal opioid–induced pruritus |
Ondansetron, 8 mg IV, concurrent with opioid |
Nalbuphine (Nubain), 5 mg IV, concurrent with opioid |
Uremia* |
Ultraviolet B phototherapy two times per week for one month |
Activated charcoal, 6 g per day orally |
Capsaicin 0.025% cream applied to localized areas four to six times daily for several weeks |
Footnote:
*—Ondansetron and naltrexone (Trexan) are not effective in treating pruritus caused by uremia.
IV = intravenously.
[Source 18 ]Pruritus prognosis
The management of chronic pruritus is difficult and often requires the use of combination therapy over a long period of time. Identification and treatment of underlying conditions causing pruritus may help in this process. The symptom may quickly disappear or persist for long periods of time.
References- Zirwas MJ, Seraly MP. Pruritus of unknown origin: a retrospective study. J Am Acad Dermatol. 2001;45:892–6.
- Braverman IM. Skin manifestations of internal malignancy. Clin Geriatr Med. 2002;18:1–19.
- Callen JP, Bernardi DM, Clark RA, Weber DA. Adult-onset recalcitrant eczema: a marker of noncutaneous lymphoma or leukemia. J Am Acad Dermatol. 2000;43(2 pt 1):207–10.
- Elmer KB, George RM. Cutaneous T-cell lymphoma presenting as benign dermatoses. Am Fam Physician. 1999;59:2809–13.
- Gelfand JM, Rudikoff D. Evaluation and treatment of itching in HIV-infected patients. Mt Sinai J Med. 2001;68:298–308.
- Robinson-Bostom L, DiGiovanna JJ. Cutaneous manifestations of end-stage renal disease. J Am Acad Dermatol. 2000;43:975–86.
- Krajnik M, Zylicz Z. Understanding pruritus in systemic disease. J Pain Symptom Manage. 2001;21:151–68.
- Habif TP. Clinical dermatology: a color guide to diagnosis and therapy. 3d ed. St. Louis: Mosby, 1996.
- Jones EA, Bergasa NV. The pruritus of cholestasis. Hepatology. 1999;29:1003–6.
- Valsecchi R, Cainelli T. Generalized pruritus: a manifestation of iron deficiency [Letter]. Arch Dermatol. 1983;119:630.
- Diehn F, Tefferi A. Pruritus in polycythaemia vera: prevalence, laboratory correlates and management. Br J Haematol. 2001;115:619–21.
- Heymann WR. Chronic urticaria and angioedema associated with thyroid autoimmunity: review and therapeutic implications. J Am Acad Dermatol. 1999;40(2 pt 1):229–32.
- Cyr PR, Dreher GK. Neurotic excoriations. Am Fam Physician. 2001;64:1981–4.
- Veien NK, Hattel T, Laurberg G, Spaun E. Brachioradial pruritus. J Am Acad Dermatol. 2001;44:704–5.
- Gupta MA, Gupta AK, Voorhees JJ. Starvation-associated pruritus: a clinical feature of eating disorders. J Am Acad Dermatol. 1992;27:118–20.
- Kroumpouzos G, Cohen LM. Dermatoses of pregnancy. J Am Acad Dermatol. 2001;45:1–19.
- Fagan EA. Intrahepatic cholestasis of pregnancy. Clin Liver Dis. 1999;3:603–32.
- Pruritus. Am Fam Physician. 2003 Sep 15;68(6):1135-1142. https://www.aafp.org/afp/2003/0915/p1135.html
- Shellow WV. Evaluation of pruritus. In: Goroll AH, Mulley AG Jr, eds. Primary care medicine: office evaluation and management of the adult patient. 4th ed. Philadelphia: Lippincott Williams & Wilkins, 2000:1001–4.
- Correale CE, Walker C, Murphy L, Craig TJ. Atopic dermatitis: a review of diagnosis and treatment. Am Fam Physician. 1999;60:1191–8,1209–10.
- Beltrani VS. The clinical spectrum of atopic dermatitis. J Allergy Clin Immunol. 1999;104(3 pt 2):S87–98.
- Belsito DV. The diagnostic evaluation, treatment, and prevention of allergic contact dermatitis in the new millennium. J Allergy Clin Immunol. 2000;105:409–20.
- Fisher AA. Aquagenic pruritus. Cutis. 1993;51:146–7.
- Parker F. Structure and function of skin. In: Goldman L, Bennett JC, eds. Cecil Textbook of medicine. 21st ed. Philadelphia: Saunders, 2000:2266.
- Shellow WV. Evaluation of pruritus. In: Goroll AH, Mulley AG Jr, eds. Primary care medicine: office evaluation and management of the adult patient. 4th ed. Philadelphia: Lippincott Williams & Wilkins, 2000:1001–4
- Tennyson H, Levine N. Neurotropic and psychotropic drugs in dermatology. Dermatol Clin. 2001;19:179–97.
- Berger R, Gilchrest BA. Skin disorders. In: Duthie EH, Katz PR, eds. Practice of geriatrics. 3d ed. Philadelphia: Saunders, 1998:467–72.
- Leibsohn E. Treatment of notalgia paresthetica with capsaicin. Cutis. 1992;49:335–6.
- Harrigan E, Rabinowitz LG. Atopic dermatitis. Immunol Allergy Clin North Am. 1999;19:383–96.
- Finn AF Jr, Kaplan AP, Fretwell R, Qu R, Long J. A double-blind, placebo-controlled trial of fexofenadine HCl in the treatment of chronic idiopathic urticaria. J Allergy Clin Immunol. 1999;104:1071–8.